Back to Journals » Cancer Management and Research » Volume 17
A Case Report of Pulmonary Malignant Melanoma with Multiple Intracranial Hemorrhagic Metastases
Authors Zhang J, Yang G, Peng S, Fang Y
Received 10 January 2025
Accepted for publication 11 April 2025
Published 17 April 2025 Volume 2025:17 Pages 829—833
DOI https://doi.org/10.2147/CMAR.S516880
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Seema Singh
Jian Zhang,1,2,* Guangming Yang,3,* Shaopeng Peng,1 Yuan Fang4
1Department of Neurosurgery, Gusu Provincial Hospital, Lanzhou, 730000, People’s Republic of China; 2NHC Key Laboratory of Diagnosis and Therapy of Gastrointestinal Tumor, Lanzhou, 730000, People’s Republic of China; 3The First Clinical School of Medicine, Gansu University of Traditional Chinese Medicine, Lanzhou, 730000, People’s Republic of China; 4Department of Ultrasonography, Gusu Provincial Hospital, Lanzhou, 730000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yuan Fang, Email [email protected]
Abstract: Primary pulmonary malignant melanoma is a very rare non-epithelial tumour with a high degree of malignancy, susceptibility to early haematogenous metastasis and poor prognosis. Lung malignant melanoma with multiple intracranial metastases is highly susceptible to misdiagnosis or underdiagnosis in clinical practice. This article reports a case of pulmonary malignant melanoma with multiple intracranial hemorrhagic metastases, aiming to improve clinicians’ understanding of this disease through this case analysis. Especially for patients over 60 years old with intracranial multiple hemorrhage, it is necessary to broaden the diagnostic and therapeutic thinking, and to exclude rare malignant tumors in the whole body through multi-systematic examination, so as to avoid misdiagnosis or omission of the diagnosis, which may cause delays in the condition.
Keywords: malignant melanoma of the lung, metastases, malignant tumours, haemorrhagic stroke
Introduction
Malignant melanoma (MM) typically originates from embryonic neural crest melanocytes and is characterized as a highly aggressive tumor with a poor prognosis and a tendency for metastasis.1 It is recognized as one of the most challenging cancers to treat due to its resistance to traditional therapeutic approaches and unfavorable clinical outcomes. This aggressive tumor can metastasize systemically even in the early stages of the disease. While primary lesions are frequently found on the skin or mucosal surfaces, they can also occur in other tissues and organs, such as the respiratory tract, oral cavity, liver, esophagus, larynx, and cervix.2 Given that the majority of patients with respiratory-derived MM have already metastasized at the time of diagnosis, early detection and treatment are crucial. Primary malignant melanoma of the lung (PMML) is an extremely rare non-epithelial tumor, accounting for only 0.01% of all primary lung tumors and 0.4% of all malignant melanomas.3 We report a case of a male patient who initially presented with spontaneous intracranial hemorrhage without initial pulmonary symptoms such as cough or sputum. The clinical diagnosis was initially misinterpreted as “hemorrhagic stroke”. After comprehensive examinations and multidisciplinary team (MDT) discussions, the final diagnosis was confirmed as PMML with multiple intracranial hemorrhagic metastases. Through this case report, we aim to enhance the awareness of neurologists regarding the differential diagnosis of multifocal intracranial hemorrhagic diseases. For atypical intracranial hemorrhages, it is essential to broaden the diagnostic approach, thoroughly investigate the medical history, and conduct extensive examinations to avoid clinical misdiagnosis or missed diagnosis, thereby preventing delayed treatment.
Case
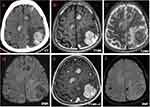
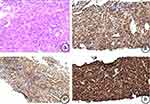
This report presents the case of a male patient over 50 years of age who presented to the doctor with intermittent headache, dizziness, and weakness of the right side of the limbs, which had lasted for 2 weeks. One week prior to admission, the patient experienced sudden weakness in his right hand while playing chess, accompanied by pain in the top of his head and dizziness, followed by weakness and instability in his right leg upon standing. He was conscious, without nausea or vomiting, and the symptoms resolved after a brief rest, without further medical evaluation. Three days before admission, the symptoms recurred and did not resolve with rest, leading to symptomatic treatment at a nearby hospital without neurological examination. Upon admission, the patient’s main symptoms were progressively worsening right-sided limb weakness, intermittent headaches, and dizziness. Neurological examination revealed clear consciousness, slightly slurred speech, normal orientation and memory, mildly reduced calculation and comprehension abilities, right-sided limb muscle strength of 3/5, and normal left-sided limb muscle strength. Cranial CT showed multiple nodular high-density shadows in both cerebral hemispheres with surrounding brain edema, suggestive of hemorrhage (Figure 1). MRI revealed multiple nodular mass-like lesions in bilateral parietal lobes, exhibiting heterogeneous enhancement on contrast imaging (Figure 1b-e). Susceptibility-weighted imaging (SWI) revealed multiple nodular lesions in the bilateral parietal lobes, exhibiting characteristic patchy hypointense signals within the mass lesions (Figure 1f). Chest CT showed multiple nodules and mass shadows of varying sizes in both lungs, with enlarged right hilar lymph nodes (Figure 2). Whole-body PET-CT suggested multiple intracranial metastases from pulmonary malignant tumor. CT-guided lung lesion biopsy confirmed the diagnosis of primary pulmonary malignant melanoma, with immunohistochemical staining positive for CK7, S-100, HMB-45, Melan-A, and a Ki-67 index of 70% (Figure 3), and no mutations in BRAF, NRAS, or KRAS detected. After multidisciplinary team discussion, the diagnosis was established as primary pulmonary malignant melanoma with multiple intracranial hemorrhagic metastases. The patient was transferred to the oncology centre 1 month after admission and received one cycle of temozolomide, cisplatin and bevacizumab and was discharged with clinical improvement. However, the patient did not adhere to further treatment after discharge and died approximately 6 months later.
Discussion
Primary malignant melanoma of the lung (PMML) is an extremely rare malignant tumor, with only a limited number of reports in both domestic and international literature. It is characterized by high malignancy, strong invasive ability, a high recurrence rate, and a poor prognosis.4,5 Cases of PMML with multiple pulmonary and intracranial hemorrhagic metastases are very rare. The pathogenesis of PMML remains controversial; most scholars believe that melanocytes are a type of neuroendocrine cell, present in various parts of the body, which migrate to the respiratory tract during embryonic development and subsequently transform into cancer cells.6,7 Other reports indicate that pulmonary melanoma cells may originate from submucosal bronchial glands or pluripotent stem cells in the lower respiratory tract.8 Literature statistics show that approximately 5–10% of metastatic malignant melanoma has an unknown primary source, potentially due to the primary lesion being typically concealed or resulting from the deterioration and metastasis of ectopic melanocyte cells from other body parts.9,10 Due to the nonspecific clinical manifestations of PMML, considering the presence of multiple nodules, it is often misdiagnosed as pulmonary tuberculosis or lung metastases. Pulmonary malignant melanoma with multiple hemorrhagic intracranial metastases requires differentiation from glioblastoma, other metastatic tumors (eg, lung/kidney cancer), brain abscess, and hypertensive hemorrhage. Key diagnostic methods include MRI (T1WI hyperintensity, thick-ring enhancement) and immunohistochemistry (HMB45/S-100/Melan-A positivity). In this case, the patient showed no cough, sputum production, or history of melanoma in the skin or eyes, although there was a history of hemoptysis. The initial symptoms included headaches and dizziness, accompanied by limb weakness, and were initially misdiagnosed as multiple intracranial hemorrhagic lesions. After admission, further investigations including chest CT, cranial MRI, CT-guided percutaneous biopsy of bilateral lung masses, and immunophenotyping were performed, followed by comprehensive whole-body PET-CT and ECT scans, leading to a definitive diagnosis of primary malignant melanoma of the lung with multiple pulmonary and intracranial hemorrhagic metastases. Unlike lung cancer, the chest CT scan of this patient showed a nodular tumor with clear margins, accompanied by enlargement of the tracheobronchial lymph nodes. The cranial MRI revealed multiple hemorrhagic metastatic lesions located at the cortex and at cortical and subcortical transition. HMB-45 is a specific marker detectable in 50–75% of melanocytic lesions and its reactivity is considered to be directly proportional to the proliferation status of melanocytes.11 In this case, the immunohistochemical staining of the lung mass indicated high expression of HMB-45, Melan-A, and S-100, with no expression of CK, CgA, Syn, HMW-CK, or TTF-1, providing significant diagnostic value for primary malignant melanoma of the lung.
With the widespread application of cancer gene diagnostics, traditional pathological diagnosis and staging have been supplemented by various cytogenetic and molecular genetic tools.12 Gene-assisted diagnostics have been shown to be crucial in revealing cancer-specific clonal gene abnormalities, which are vital for disease diagnosis, prognosis, and the development of personalized treatment plans.12 Studies have found that BRAF gene mutations serve as important biomarkers for predicting responses to novel targeted therapies (eg, Dabrafenib, Vemurafenib) and significantly impact tumor prognostic assessments. As a result, BRAF gene testing has been widely integrated into clinical practice.13 In malignant melanoma of the skin, approximately 50% of cases exhibit detectable BRAF mutations, whereas other types of malignant melanoma (such as pulmonary and intracranial) show a relatively low positive detection rate.14 In the case presented in this report, the BRAF gene test result was negative, and no mutations were found in NRAS or KRAS gene testing.
Currently, the optimal treatment strategy for primary malignant melanoma of the lung with multiple pulmonary and intracranial metastases remains a topic of discussion. Studies have shown that patients who undergo surgical resection tend to have a better prognosis compared to those receiving conservative treatment.15 Additionally, there is a viewpoint suggesting that a combined approach of radiotherapy and chemotherapy with targeted and immunotherapy can help relieve suffering and prolong survival in patients with multiple metastases of pulmonary malignant melanoma. Based on recent advances in research regarding primary pulmonary melanoma with secondary intracranial multiple metastases, we believe that for solitary pulmonary or intracranial lesions causing symptoms such as respiratory distress or neurological deficits, surgical treatment should be prioritized after excluding any surgical contraindications. Following the surgery, combining pathological examination and genetic testing results with a comprehensive regimen of radiotherapy, molecular targeted therapy, and immunotherapy could yield favorable prognoses. In the case reported in this study, the patient presented with multiple metastatic lesions in both the lungs and the brain, and it was recommended that the patient continue with radiotherapy and targeted treatment. However, the patient and family did not adhere to these medical recommendations and opted to forgo further treatment.
Conclusion
PMML is extremely rare and is often misdiagnosed as lung cancer or pulmonary tuberculosis; a definitive diagnosis relies on pathological examination of tissue. Due to the variability in tissue morphology and immunophenotype, the diagnosis is quite challenging and must be differentiated from other lung malignancies. Immunohistochemical staining can aid in this differentiation. Currently, there is a lack of standardized treatment guidelines for PMML with multiple intracranial metastases, but research into targeted immunotherapy is advancing. Combination therapy with PD-1/PD-L1 inhibitors is expected to become a mainstream approach. We hope this case can provide further insights into the diagnosis and treatment of PMML.
Ethical Statement
The research does not require the approval of the ethics committee.
Consent to Publish
Written informed consent was obtained from the patient’s next of kin for publication of any potentially identifiable images or data included in this article.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Science and Technology Plan Project of Lanzhou (2023-2-104); NHC Key Laboratory of Diagnosis and Therapy of Gastrointestinal Tumor, PhD/post-doctoral research projects (NHCDP2022013).
Disclosure
All authors declare no conflicts of interest in this work.
References
1. Pitcovski J, Shahar E, Aizenshtein E, et al. Melanoma antigens and related immunological markers. Crit Rev Oncol Hematol. 2017;115:36–49. doi:10.1016/j.critrevonc.2017.05.001
2. Karimkhani C, Green AC, Nijsten T, et al. The global burden of melanoma: results from the global burden of disease study 2015. Br J Dermatol. 2017;177(1):134–140. doi:10.1111/bjd.15510
3. Wilson RW, Moran CA. Primary melanoma of the lung: a clinicopathologic and immunohistochemical study of eight cases. Am J Surg Pathol. 1997;21(10):1196–1202. doi:10.1097/00000478-199710000-00010
4. Gong L, Liu X-Y, Zhang W-D, et al. Primary pulmonary malignant melanoma: a clinicopathologic study of two cases. Diagn Pathol. 2012;7(1):123. doi:10.1186/1746-1596-7-123
5. Pan X-D, Zhang B, Guo L-C, et al. Primary malignant melanoma of the lung in the elderly: case report and literature review. Chin Med J. 2010;123(13):1815–1817. doi:10.3760/cma.j.issn.0366-6999.2010.13.040
6. Shi Y, Bing Z, Xiaohui X, et al. Primary pulmonary malignant melanoma: case report and literature review. Thorac Cancer. 2018;9(9):1185–1189. doi:10.1111/1759-7714.12798
7. Peng J, Han F, Yang T, et al. Primary malignant melanoma of the lung: a case report and literature review. Medicine. 2017;96(46):e8772. doi:10.1097/MD.0000000000008772
8. Maeda R, Isowa N, Onuma H, et al. Primary malignant melanoma of the lung with rapid progression. Gen Thorac Cardiovasc Surg. 2009;57(12):671–674. doi:10.1007/s11748-009-0454-9
9. Chang AE, Karnell LH, Menck HR. The national cancer data base report on cutaneous and noncutaneous melanoma: a summary of 84,836 cases from the past decade. The American college of surgeons commission on cancer and the American cancer society. Cancer. 1998;83(8):1664–1678. doi:10.1002/(SICI)1097-0142(19981015)83:8<1664::AID-CNCR23>3.0.CO;2-G
10. Katz KA, Eric Jonasch FSH, Hodi FS, et al. Melanoma of unknown primary: experience at Massachusetts General Hospital and Dana-Farber Cancer Institute. Melanoma Res. 2005;15(1):77–82. doi:10.1097/00008390-200502000-00013
11. Brito AB, Rogerio F, Reis F, et al. Primary meningeal melanocytoma mimicking a nonfunctioning pituitary adenoma. Clin Neuropathol. 2016;35(3):158–161. doi:10.5414/NP300885
12. Korf BR, Mikhail FM. Overview of genetic diagnosis in cancer. Curr Protoc Hum Genet. 2017;93:
13. Colombino M, Sini M, Lissia A, et al. Discrepant alterations in main candidate genes among multiple primary melanomas. J Transl Med. 2014;12(1):117. doi:10.1186/1479-5876-12-117
14. Cristina Sini M, Doneddu V, Paliogiannis P, et al. Genetic alterations in main candidate genes during melanoma progression. Oncotarget. 2018;9(9):8531–8541. doi:10.18632/oncotarget.23989
15. Seitelman E, Donenfeld P, Kay K, et al. Successful treatment of primary pulmonary melanoma. J Thorac Dis. 2011;3(3):207–208. doi:10.3978/j.issn.2072-1439.2011.04.02
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.