Back to Journals » Journal of Pain Research » Volume 18
A Cost Effectiveness Analysis of Spinal Cord Stimulation versus Conventional Medical Management for the Treatment of Low Back Pain Using Data from DISTINCT RCT and Medical Claims from a U.S. Commercial Payer Database
Authors Deer T , Heros R , Scarfo K, Gilligan C , Jameson J, Pilitsis JG , Desai MJ , Panchalingam T, Goates S, Benison AM, Okaro U, Falowski S
Received 8 November 2024
Accepted for publication 15 March 2025
Published 7 June 2025 Volume 2025:18 Pages 2823—2838
DOI https://doi.org/10.2147/JPR.S486759
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Robert Twillman
Timothy Deer,1,* Robert Heros,2,* Keith Scarfo,3 Christopher Gilligan,4 Jessica Jameson,5 Julie G Pilitsis,6 Mehul J Desai,7 Thadchaigeni Panchalingam,8 Scott Goates,8 Alexander M Benison,8 Udoka Okaro,8 Steven Falowski9
1The Spine and Nerve Center of the Virginias, Charleston, WV, USA; 2Spinal Diagnostics, Tualatin, OR, USA; 3Norman Prince Spine Institute, Brown University Health, Rhode Island Hospital, Providence, RI, USA; 4Robert Wood Johnson University Hospital, New Brunswick, NJ, USA; 5Axis Spine Center, Coeur d’Alene, ID, USA; 6Department of Neurosurgery, The University of Arizona, Tucson, AZ, USA; 7International Spine, Pain & Performance Center, Washington, DC, USA; 8Neuromodulation, Abbott Labs, Austin, TX, USA; 9Neurosurgical Associates of Lancaster, Lancaster, PA, USA
*These authors contributed equally to this work
Correspondence: Steven Falowski, Neurosurgical Associates of Lancaster, Lancaster, PA, USA, Email [email protected]
Purpose: To compare the healthcare utilization (HCU) and costs for passive recharge burst Spinal Cord Stimulation (SCS) and conventional medical management (CMM) cohorts in patients with chronic low back pain (LBP) to a matched real-world cohort of similar indication. The null hypothesis is that SCS is equally or less cost-effective than CMM in treating LBP.
Patients and Methods: DISTINCT is a prospective, multi-center, randomized study. Data was collected during in-clinic visits at baseline, one, three, and six months. The DISTINCT “completer cohort” included 79 DISTINCT SCS patients and 55 DISTINCT CMM patients who completed the six-month visit. An external real-world cohort (n = 71) with similar characteristics to DISTINCT CMM patients was identified from a claims database (Optum’s de-identified Market Clarity Data). Accessed data included healthcare resource utilization (HCU), pain-related medication usage, pain scale, and quality of life. HCU data covered physical therapy, chiropractic therapy, massage therapy, occupational therapy, acupuncture, injection treatments, radiofrequency ablation procedures, and opioid and anticonvulsant usage.
Results: The DISTINCT study demonstrated superior outcomes in pain relief, function, and other symptoms with SCS compared to CMM in the treatment of persistent (at least 6 months) low back pain. DISTINCT SCS patients utilized fewer healthcare resources and incurred lower costs than DISTINCT CMM patients. Real-world CMM patients exhibited higher utilization of certain therapies, suggesting potential pre-crossover bias. SCS resulted in significant cost savings and improved quality of life compared to CMM. Including device costs, cost-effectiveness could be achieved within 2.7 years based on DISTINCT data. The real-world CMM arm used more high-priced interventional therapies, suggesting a pre-crossover bias in the CMM cohort.
Conclusion: This analysis supports the long-term benefits and cost-effectiveness of SCS in managing chronic LBP compared to CMM.
Keywords: non-surgical back pain, low back pain, spinal cord stimulation, cost effectiveness, cost savings, BurstDR™
Introduction
Low back pain (LBP) is a complex condition influenced by various factors including psychological factors, social factors, biophysical factors, comorbidities, and pain-processing mechanisms.1 It is a prevalent chronic pain condition and a leading cause of global disability.2,3 The economic impact encompasses high healthcare costs, lost productivity, and disability payments — impacting individuals, families, employers, healthcare systems, communities, and society at large.1,2,4,5 Chronic LBP, persisting for 12 weeks or more, is an expensive condition to treat, estimated to cost 12.2–90.6 billion dollars annually in the US, with a lifetime prevalence of 60–85% globally.6–8
Chronic LBP may involve both nociceptive and/or neuropathic pain (NP). Nociceptive pain arises from tissues damaged by physical or chemical agents such as trauma, surgery, or chemical burns.9 Neuropathic back pain originates from nerve root injury, disease, or pathological innervation of damaged lumbar discs, often posing challenges to detection and management.2,3
The primary treatment goals of chronic LBP are pain reduction, functional improvement, and prevention of future exacerbation.10 Guidelines recommend a multimodal approach combining pharmacological therapies for symptomatic relief with nonpharmacological interventions, such as physical activity and psychosocial/behavioral approaches.11–16 Pharmacotherapy options include acetaminophen, nonsteroidal anti‐inflammatory drugs, muscle relaxants, antidepressants, anticonvulsants, opioids, and topical treatments. However, oral medications have limited efficacy and are associated with risks including tolerance and addiction with long-term opioid use.3 Non-pharmacological options like Transcutaneous Electrical Nerve Stimulation (TENS), physiotherapy, interventional procedures (eg, epidural steroid injections (ESIs), radiofrequency ablations and spinal cord stimulation (SCS)) are also considered efficacious.17–21
SCS, particularly passive recharge burst, has emerged as an option for LBP patients unresponsive to conventional medical management.22 SCS is a form of neurostimulation therapy where electrodes transmit electrical impulses to targeted regions of the spinal cord, altering the way pain signals are processed. SCS has been shown to be effective in treating many chronic and neuropathic pain conditions.23 Clinical studies show that SCS provides a sustained, long-term, reduction of 50% or greater in over 70% of patients leading to decreased pain medication usage, improved functional status, enabling return to work.22,24–27
The DISTINCT study is a prospective, randomized, controlled study comparing passive recharge burst to conventional medical management (CMM) in patients with chronic LBP who have not undergone lumbar spine surgery and for whom corrective surgery is not an option. In the reimbursement landscape of the US, patients must try various conservative treatments, such as, physical therapy and medication including opioids, before implantable technologies and surgery are covered. Many commercial payers require a failed spine surgery before approving a spinal cord stimulator trial. This can lead to prolonged suboptimal pain control, worsened functional capacity and psychological conditions like depression and anxiety, diminished effectiveness due to treatment delays for patients, and significant economic burden to payers and the US healthcare system in general.28–31 While previous research has shown that SCS is cost-effective, many of these studies were either small and retrospective or relied heavily on models using estimates from published literature for costs and treatment outcomes, rather than data collected prospectively or sometimes only compared costs with no value placed on quality of life outcomes.32–35 This study contributes to the literature by providing new evidence on the cost-effectiveness of SCS over CMM to treat chronic LBP using a unique combination of prospectively collected patient healthcare utilization data and commercial health insurance claims data. Further, by creating an external CMM arm with closely matching real-world patients, this study provides evidence of potential bias created by postponement of costlier interventional treatments in anticipation of the cross-over after six months in the CMM group of the DISTINCT study.
This analysis focuses on assessing the cost-effectiveness of the DISTINCT SCS cohort compared to the DISTINCT CMM cohort. Additionally, we compare the cost difference with a matched real-world cohort of patients with similar chronic low back pain diagnoses without surgical interventions. This analysis compares healthcare resource utilization and associated costs between DISTINCT SCS and CMM arms from a payer perspective. A matched real-world cohort of similar chronic low back pain patients with no evidence of lumbar spine surgery was used to impute the unit costs of therapies used by both arms.
Materials and Methods
DISTINCT Patient Selection and Data Source
All study documents received institutional review board (IRB) approval of the respective investigational sites prior to subject enrollment. The study was conducted in accordance with the US Code of Federal Regulations and the World Medical Association Declaration of Helsinki. The study was registered on ClinicalTrials.gov (NCT04479787). All patients were informed about the purpose and procedures of the study and provided written informed consent prior to study enrollment. A total of 270 patients were enrolled at 30 study sites in the United States (US). Enrollment criteria are discussed in Deer 2023.24 An independent, board-certified spine surgeon reviewed and confirmed the absence of appropriate corrective surgical options. Health economic outcomes between the CMM and SCS cohorts were compared using data collected at baseline and during one-, three-, and six-month in-clinic visits. These data included patient-level healthcare resource utilization (HCU), pain-related medication usage, pain Numeric Rating Scale (NRS), and quality of life (Patient-Reported Outcome Measure Information System [PROMIS-29+2]).24 The analysis focused on the “completer cohort” comprising of 79 DISTINCT SCS patients (out of 126) and 55 DISTINCT CMM patients (out of 74) from the phase-I trial who completed their six-month visits, including the HCU and PROMIS-29+2 Profile v2.1 forms. The HCU data reported physical, chiropractic, massage, and occupational therapies, acupuncture, injection treatments, and radiofrequency ablation procedures. Data on the use of short- and long-acting opioids and anticonvulsants were collected.
After the six months primary endpoint assessment, patients could crossover to an alternate treatment arm. To address potential bias due to the crossover option, a real-world cohort of 71 patients, similar to patients enrolled in DISTINCT, was identified from the Optum’s de-identified Market Clarity Data (Market Clarity) multi-payer claims database spanning from 2016 to 2022. Permission to access and utilize Market Clarity data for the current study has been obtained from Optum via a data sharing agreement. Real-world cohort’s HCU data was extracted to supplement that of the trial CMM patients.36,37 Diagnoses of interest were identified using International Classification of Diseases, Tenth Revision (ICD-10) codes, and the pain diagnoses categories of the DISTINCT patients as listed in the baseline data (Supplemental Table 1). Procedures were identified using Current Procedural Terminology (CPT) (Supplemental Table 2), Healthcare Common Procedure Coding System (HCPCS), and ICD-10 Procedure Coding System (PCS) codes.
External Cohort Selection and Matching
The DISTINCT Inclusion /Exclusion criteria were applied to the Market Clarity to match the DISTINCT patients and ensure a comparable cohort. Eligible patients were required to be 18 years or older, have a diagnosis of refractory axial low back pain (LBP) with a neuropathic component, along with claims related to the diagnosis spanning a minimum of six months from the cohort entry.38 The cohort entry date was defined as the first outpatient or inpatient service with a diagnosis of LBP where the patient’s encounter was with a physician from one of the following as defined by the National Uniform Claim Committee (NUCC): pain medicine, neurosurgery, physical medicine and rehabilitation, or orthopedic surgery (Supplemental Table 3). The index date was defined as the second outpatient or inpatient service for the treatment of LBP.
To match the DISTINCT trial, patients with a history of lumbar spine surgery, including failed back surgery syndrome, were excluded, as were those who underwent lumbar spine surgery within one year of cohort entry. Patients treated with neuromodulation devices or those receiving an intrathecal pump within one year of cohort entry were also excluded. Patients diagnosed with cancer or other conditions listed in the exclusion criteria in the year before or after cohort entry were excluded, as were those experiencing or planning pregnancy in the nine months before or three months after cohort entry. Patients with a daily morphine milligram equivalent (MME) dose exceeding 50 MME in the 30 days before cohort entry were excluded. Additionally, patients with less than six months of data pre-cohort entry or less than one year of data post-cohort entry without continuous enrollment and patients who did not use at least one non-pharmacologic therapy within six months of the index date were excluded.
Matching between the real-world CMM patients and the DISTINCT patients was conducted using Mahalanobis distance-based nearest neighbor matching with a 1:1 ratio.39 Matching was based on baseline patient characteristics, including age, sex, race, pain diagnosis, and the number of years of pain calculated as the number of years a patient was observed in the claims data actively seeking back pain care. Post-matching balance was assessed using standardized mean differences. For the matched real-world CMM patients, their use of treatments, procedures (Supplemental Table 2), and prescription medication (Supplemental Table 4), along with the associated costs, was obtained for six months following the index visit. Device acquisition costs for the SCS implant were obtained from recent literature.40
Statistical Analysis
Baseline patient characteristics, including pain diagnoses and duration, are summarized. We quantified healthcare utilization and associated average costs per patient between (1) DISTINCT SCS vs DISTINCT CMM; and (2) DISTINCT SCS vs matched real-world CMM. Quality of life (QoL) statistics, incremental cost-effectiveness ratios between SCS and CMM therapies, and the disparity in cost per patient achieving treatment target between SCS and CMM groups at six months were estimated.41 Patients achieving a ≥50% reduction in LBP, measured by NRS were considered as achieving treatment target in the DISTINCT trial.
Therapy-specific costs were estimated from the claims data of matched real-world CMM patients and used to compute costs for the trial patients. A bootstrapped, therapy-specific average cost per visit per patient was estimated and used to impute average costs for the trial patients. To account for parameter uncertainty, a 95% confidence interval (95% CI) was estimated using the Bias-Corrected Accelerated (BCA) bootstrap method with 10,000 replications.42 For medications, costs based on specific drugs, dosage, and quantity were taken directly from the medication costs of the matched real-world CMM patients.
The primary HCU analyses focused on the proportion of patients using each therapy and associated costs, including physical therapy, chiropractic therapy, injection treatments, ablation procedures, and usage of opioids and anticonvulsants. Differences in average costs, along with their 95% CIs, were calculated using the BCA bootstrap method with 10,000 replications. All costs were reported in 2021 US dollars (U.S.$).
The average costs per patient achieving a ≥50% reduction in LBP with SCS vs CMM were calculated for DISTINCT patients by dividing the total average cost per patient at six months by the proportion of patients who experienced a 50% reduction. The PROMIS-29+2 Profile v2.1 (PROPr) was used to calculate Health-Related Quality of Life (HRQoL). Finally, using the PROPr scores and the derived total average cost per patient at six months, the Incremental Cost Effectiveness Ratio (ICER) between the SCS and CMM therapies was estimated.
Results
Patient Characteristics
Table 1 summarizes the patient demographics and pain-related characteristics of the completer cohort of the DISTINCT patients and matched real-world CMM patients. The reported summary statistics of demographics and pain-related diagnoses were limited to those used as matching criteria. The mean (standard deviation, SD) age of the DISTINCT Patients at enrollment was 58.8 (12.9) years, with majority being female (55.22%). Most (67.91%) had been experiencing chronic pain for more than 5 years, with a mean (SD) duration of 12.4 (12.9) years. The most common diagnosis was lumbar spondylosis (62.69%), followed by lumbar radiculopathy (42.54%). Between-group mean tests of DISTINCT CMM and matched real-world CMM groups were conducted and reported p-values indicated the close match between the patients.
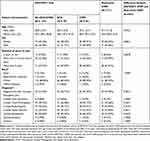 |
Table 1 Baseline Characteristics of Completer Cohort of DISTINCT Randomized Control Trial and Matched Real-World CMM Patients |
A suitable real-world cohort consisting of 163,006 patients was identified in Market Clarity data between January 2016 and December 2022. After applying the inclusion and exclusion criteria from the trial, 5064 patients remained in the final real-world cohort for matching (Figure 1). The standardized mean differences between the matched cohorts are presented in Figure 2. The baseline characteristics of the matched real-world CMM patients were similar and not statistically significantly different from that of DISTINCT trial patients (Table 1).
 |
Figure 1 Cohort Selection from Real-World Health Insurance Claims Data. |
Health Care Resource Utilization (HCU)
Figure 3 details HCU related to the primary therapies and pain medication use at six months. At six months, 25% of the patients from the DISTINCT CMM (14/55) received physical therapy; 9% (5/55) received chiropractic therapy; 31% (17/55) underwent injection treatments, 15% (8/55) had ablation procedures, and 38% (21/55) used opioids. In contrast, lower proportions of the DISTINCT SCS patients utilized the same therapies or procedures; physical therapy-11% (9/79), chiropractic therapy or ablation procedures 3% (2/79), injection treatments 9% (7/79), and opioids 35% (28/79). A higher proportion of patients in DISTINCT SCS (31%) used anticonvulsants compared to DISTINCT CMM (18%). Likewise, a higher proportion of patients in the real-world CMM cohort utilized chiropractic therapy, injections, and ablation during the six months following the index diagnosis, suggesting that some patients receiving CMM treatment in the trial may have postponed certain treatments in anticipation of the cross-over after six months. Opioid and anticonvulsant use among real-world CMM patients were 39% (20/51) and 33% (17/51), respectively.
A comprehensive breakdown of the HCU for other treatments and procedures used by real-world and trial CMM patients can be found in Supplemental Table 5. In addition to the listed therapies, 9% (12/134) of the trial patients had used massage therapy, and another 3% (4/134) had used acupuncture, services not commonly covered by commercial payers hence, not compared in the real-world CMM cohort.
Table 2 presents treatment-specific average per-patient costs, including the cost differences between CMM and SCS treatment arms for the primary therapies during the six-month follow-up. The medication and the total average costs of the real-world CMM cohort were calculated using 51 (out of 71) real-world patients who had both medical and prescription drug coverage during their enrollment period. Real-world CMM patients incurred a higher average cost of $3,502 per patient for six months compared to $1,754 for DISTINCT CMM patients and $760 for DISTINCT SCS. On average, injection treatments were the costliest, followed by ablation procedures. Other back-pain-related treatment and procedure costs for real-world patients are reported in Supplemental Table 6.
 |
Table 2 Average Cost per Patient (2021 US $) by Primary Therapy During the 6-month Follow-up |
Using the matched real-world CMM patients’ HCU and costs, the total average costs per patient across all healthcare use six-months from index visit are presented in Supplemental Table 7. Total costs (the summation of any treatment/procedure and medication costs incurred during the first six months) and total back-pain-related costs (summation of treatment/procedure costs from claims that listed at least one of the LBP diagnosis codes as the primary reason for the treatment/procedure) are reported. Real-world CMM patients incurred a total service cost of $10,165, (outpatient cost of $8,035, and a medication cost of $1,968) with 42% related to back pain. Total back-pain-related costs for real-world CMM patients accounted for 42% of total service costs, 45% of total outpatient service costs, and 42% of medication costs. The DISTINCT trial data did not include every type of healthcare utilization, like the real-world data; therefore, the total average costs for the DISTINCT patients only accounted for the primary therapies and pain medications.
The HRQoL scores (Table 3) show a significant difference in the quality-of-life metric between patients in SCS vs CMM therapies of the DISTINCT trial at six-months, with SCS patients expressing higher HRQoL (0.343–0.162 = 0.181; p<=0.001). In trial Incremental Cost-Effectiveness Ratio (ICER) were estimated based on HRQoL scores converted to quality-adjusted life years (QALY) and total average costs from Table 2. QALYs were calculated using HRQoL sores and adjusting for the length of the trial in years. The in-trial ICERs are calculated as the difference in costs between DISTINCT SCS and DISTINCT CMM [real-world CMM], divided by the difference quality of life, measured as QALYs.43 The derived ICER was compared with the cost-effectiveness threshold (willingness-to-pay), which has been fixed at ICER < $50,000 per quality-adjusted-life-year (QALY).44
 |
Table 3 Summary of Health-Related Quality of Life (HRQoL) Scores (PROMIS Preference, PROPr) of DISTINCT CMM and SCS Treatments at Six months |
SCS resulted in lower costs and greater QALYs compared to CMM for the treatment of chronic LBP. The ICER for SCS ($10,923) was below the willingness-to-pay threshold, indicating cost-effectiveness. If the costs of the matched real-world CMM patients were used in place of DISTINCT CMM costs, SCS treatment costs $30,132 less compared to CMM to gain one more QALY. Including SCS device acquisition $30,000 based on the average reimbursement for the initial SCS device and procedure cost, the ICER for SCS reached $318,747/QALY based on DISTINCT costs.40 Note that ICERs assume no additional costs/benefits beyond the six months.
With initial device costs included, assuming that the HCU remains constant over time and the HRQoL is maintained, cost-effectiveness can be achieved in 2.7 years (Figure 4A) based on the DISTINCT-CMM and SCS cost estimates, the time to cost-effectiveness reduces to 2.0 years (Figure 4B), and further to 1.9 years (Figure 4C) when costs from the matched real-world CMM patients are used in place of trial CMM costs which are prone to cross-over bias.
Figure 4B includes the costs of opioids and anticonvulsants only whereas Figure 4C includes costs of all pain medications used by real-world CMM patients.
The primary endpoint of the DISTINCT was the proportion of patients achieving at least a 50% reduction on the NRS in six months between SCS and CMM. Following the trial endpoint, the average cost per patient to achieve a 50% reduction in LBP was calculated. With SCS treatment 84.8% (95% CI: 73.4– 91.1%) achieved the treatment target compared to a 7.3% (95% CI: 1.8–14.6%) with CMM (Supplemental Table 8). On average, excluding the initial device costs, achieving a 50% reduction in pain with SCS costs $896 per patient, whereas with CMM, it costs $24,127 per patient. When initial device costs are factored in, the cost of achieving a 50% reduction in pain with SCS is $36,269 per patient.
Figure 5 demonstrates the cost per patient achieving treatment target with SCS versus CMM with the treatment target being at least a 50% reduction in pain. Despite the higher initial cost, SCS treatment costs less per patient achieving treatment target starting around nine months compared to CMM treatment and the relative increase in the cost per patient achieving treatment target with CMM treatment is far greater compared to SCS after nine months.
 |
Figure 5 Cost (2021 US $) per patient achieving treatment target with SCS versus CMM therapies for the treatment of chronic low back pain. |
Discussion
The primary objective of this study was to evaluate the cost-effectiveness of SCS versus CMM therapies for the treatment of chronic LBP in patient’s ineligible for lumbar spine surgery and for whom corrective surgery is not an option. DISTINCT CMM patients had an option to cross over after six months potentially influencing their therapy choices and introducing a pre-crossover bias. To mitigate this bias, a real-world matched cohort (real-world CMM cohort) was selected using a commercial based payer database, closely mirroring the DISTINCT study eligibility criteria. Cost-effectiveness and cost per patient achieving treatment target were also compared between the two treatments.
The DISTINCT-SCS patients previously reported significant improvements in pain reduction, disability improvement and improved quality of life after six months of therapy.24 In this analysis, we show that DISTINCT SCS patients utilized fewer healthcare resources within six months of their implant compared to the DISTINCT CMM and real-world CMM cohorts. Interestingly, the real-world CMM arm utilized more of both high-priced, interventional therapies (injections and radiofrequency ablation) suggesting a pre-cross-over bias in CMM cohort. The reduction in HCU in SCS led to a significant decrease in total average HCU cost per patient in the six-month follow-up. Additionally, SCS was associated with a reduction opioid usage aligning with previous studies that demonstrated the role of SCS in reducing opioid-related abuse, morbidity, mortality, and associated costs.45–48 The total cost of medication was higher for DISTINCT SCS compared to DISTINCT CMM due to a higher proportion of patients using anticonvulsants ($319 higher with DISTINCT SCS vs DISTINCT CMM), but similar usage compared to real-world CMM patients resulting in cost saving ($143 lower with real-world CMM Vs DISTINCT SCS). This aligns with a previous finding from Adil (2020) which reported that within 1 year of SCS, 60.4% (out of 8497) of patients had some reduction in their opioid use, 34.2% moved to a clinically important lower dosage group, and 17.0% weaned off opioids entirely.45
DISTINCT SCS patients report significant improvements in quality of life at lower costs compared to CMM patients. The overall economic value as determined by cost-effectiveness and cost per patient achieving treatment target favored SCS over CMM. When considering upfront device costs, SCS treatment becomes cost effective (at the standard threshold of $50,000 per QALY) within 2.7 years with a lower cost per patient achieving treatment target from nine months.
Since our analysis focused on the in-trial experience of DISTINCT patients we did not explicitly consider costs that could be associated with device failure or revision beyond six months, which may increase long term costs for the SCS treatment group. However, despite this limitation, our findings are consistent with previous analyses which found economic advantages to SCS. For example, a 2008 multicenter, prospective RCT reported that despite the initial higher health cost in the SCS group, subsequent years demonstrated lower costs compared to the CMM group with significant savings at 5-years (Costs of the CMM cohort -$33,722) vs SCS cohort-$24,799).49 Another retrospective study affirmed that although SCS patients incurred greater median annual total cost ($13,216) compared to the CMM patients at initial implantation ($5,934), the median annual cost for patients who underwent SCS consistently decreased over time becoming less than half of the annualized costs for the non-SCS group at 9 years.35
Furthermore, a Cleveland Clinic study reported substantial savings in healthcare ($18,000) over 3-years for patients with SCS when compared to 6-years pre-implant.50 Per a previous study, the average time to even out up-front device cost was 3.1 years among patients who discontinued opioids or observed a ≥50% reduction in average daily dose and 4.2 years for patients who did not reduce or discontinue opioids.51
Chronic low back pain and its associated disability impose a significant financial burden on families, healthcare systems, and the broader economy. Existing studies consistently support the effectiveness and superiority of SCS to CMM with patients experiencing improved performance outcomes, higher satisfaction rates, and fewer complications.24,26,27,52
Overall, SCS emerges as a superior therapy for patients diagnosed with chronic LBP delivering substantial cost savings and improved quality of life and long-term cost effectiveness when compared to CMM. Spinal cord stimulation ought to be considered earlier in the treatment continuum and not as a salvage therapy.
This study has limitations. First, long term follow-up of healthcare utilization of chronic LBP patients is limited in insurance claims data due to interruptions in continuity of enrollment and coverage. This makes it challenging to identify patients with chronic LBP in real-world data for at least 12 years, which is the average duration of pain among the trial patients. However, the demographics of the matched real-world CMM cohort were consistent with the literature and DISTINCT patients, showing that patients with chronic LBP are more likely to be female and older than 50 years. Further studies should incorporate long-term follow-up of patients, including prospective methods of data collections. Further, this analysis does not include costs associated with complications or annual maintenance of the device after implantation. These aspects are beyond the scope of this analysis, as the primary focus is on comparing the in-trial experience of patients and the cost-effectiveness of the treatments in the DISTINCT trial. Future studies with long-term follow-up can address this limitation given that complications, device replacements are better captured in data with long-term follow-up. Second, HCU costs were not collected in the trial and therefore were imputed using the cost estimates of the real-world patients, which may have introduced some uncertainty. We partially accounted for the uncertainty around the cost estimates by reporting bias-corrected bootstrapped 95% CIs. Future trials should try to collect data on costs data along with data on healthcare visits and procedures. Third, only a subset of the HCU data were collected during the trial, therefore, our HCU did not capture all distinct types of therapies, procedures, and costs of care. Further, a therapy, procedure, or a medication that did not have a health insurance claim associated with it (eg, out-of-pocket healthcare costs) was not available to the researcher, which means the total average costs were likely underestimated. This is evident from the higher estimated total average cost of real-world CMM patients when all claims related to back-pain diagnosis as opposed to only a subset of therapies and medications reflecting the trial HCU were included (US $ 4,517 vs 3,502) (Supplemental Table 7).
Conclusion
SCS emerges as a superior therapy, delivering substantial cost savings and improved quality of life for chronic LBP patients. The evidence suggests that despite the upfront cost, SCS is a more cost effective and beneficial therapy for patients with chronic LBP when compared to CMM.
Abbreviations
BCA, Bias-Corrected Accelerated; CI, Confidence Interval; CMM, Conventional Medical Management; CPT, Current Procedural Terminology; ESI, Epidural Steroid Injections; HCPCS, Healthcare Common Procedure Coding System; HCU, Healthcare Utilization; HRQoL, Health-Related Quality of Life; ICD-10, International Classification of Diseases, Tenth Revision; ICER, Incremental Cost Effectiveness Ratio; IRB, Institutional Review Board; LBP, Low Back Pain; MME, Morphine Milligram Equivalent; NP, Neuropathic Pain; NRS, Numeric Rating Scale; NUCC, National Uniform Claim Committee; PCS, ICD-10 Procedure Coding System; PROMIS, Patient-Reported Outcome Measure Information System; PROPr, PROMIS-29+2 Profile v2.1; QALY, Quality Adjusted Life Year; QoL, Quality of Life; RCT, Randomized Control Trial; SCS, Spinal Cord Stimulation; SD, Standard Deviation; TENS, Transcutaneous Electrical Nerve Stimulation; US, United States.
Data Sharing Statement
All relevant data are included in the article or available in Supplementary Information. To gain access to Optum’s de-identified Market Clarity Data, a request can be made to Optum (https://www.optum.com), but costs may be incurred, a data sharing agreement would be necessary, and no patient identifiable information can be obtained.
Ethics Approval and Informed Consent
All study documents received institutional review board (IRB) approval prior to patient enrollment. The study was registered on ClinicalTrials.gov (NCT04479787), and the registration was first submitted on 07/17/2020. All study documents received institutional review board (IRB) approval of the respective investigational sites. Therefore, the dates of these approvals vary from site to site. The earliest approval was on 6/18/2020 and the latest approval was on 5/28/2021. All patients were informed about the purpose and procedures of the study and provided written informed consent prior to study enrollment. Ethics committee approval was not required for Optum’s Market Clarity Data as the data available for analysis were de-identified and not traceable back to an individual. Optum’s de-identified Market Clarity Data was used with permission under the data use agreement between Abbott and Optum.
Acknowledgments
The authors acknowledge the DISTINCT investigator and clinical group: James Yue MD, Edward Tavel MD, Sayed Wahezi MD, Robert Funk MD, Patrick Buchanan MD, Jacqueline Weisbein M, Anne Christopher MD, Denis Patterson MD, Mohab Ibrahim MD, Ajay Antony MD, Nathan Miller MD, Keith Scarfo MD, Michael Fishell MD, Derron Wilson MD, Scott Kreiner MD, Chi Lim MD, Edward Braun MD, Levy Roberts, MD, PhD, David Dickerson MD, Susan Moeschler, MD, Jonathan Duncan MD, Jijun Xu MD, Andras Laufer, MD, Kenneth Candido MD and Alex Chieu PhD. This study was funded by Abbott Labs, (Plano, TX).
Funding
This study was funded by Abbott Laboratories, TX, USA.
Disclosure
Timothy Deer has consulting agreements with Abbott, Saluda, SpineThera, CornerLoc, Boston Scientific, Pain Teq, Spinal Simplicity, Biotronik, Aurora, Nevronik and SPR Therapeutics and is an investigator with Abbott, Saluda, Boston Scientific, Pain Teq,and SPR Therapeutics. Timothy Deer has stocks or stock options with Saluda, SpineThera, Pain Teq, Aurora, Nevronik, and has a patent pending with Abbott.Robert Heros reports consulting fees from Abbott, Mainstay Medical, Saluda Medical, and Biotronik, and support for attending meetings from Mainstay Medical and participated on a data safety monitoring board/advisory board for Biotronik. He is an investigator with Abbott, Mainstay, and Saluda. Keith-Austin Scarfo reported a consultant agreement with Abbott. Chris Gilligan reports consulting fees from Mainstay Medical, Persica, Saluda, and Iliad Lifesciences and stock or stock options from Mainstay Medical. Jessica Jameson reports consulting fees from Boston Scientific, Nevro, SPR, Abbott, and Nevro and payment or honoraria from Nevro, Boston Scientific, Saluda, Abbott, and Medtronic. Julie Pilitsis is a medical advisor and has investments or stock options in for Aim Medical Robotics. She has received grant support from Medtronic, Boston Scientific, Abbott, Focused Ultrasound Foundation, NIH-NeuroBlueprint MedTech 5U54EB033650 and NIH R18EB036591. Mehul Desai reports consulting fees from Medtronic, SPR Therapeutics, and Nalu Medical and stock or stock options from SPR Therapeutics, Synerfuse, Virdio Health, and HypreVention. Thadchaigeni Panchalingam, Scott Goates, Alexander M Benison, and Udoka Okaro are employees of Abbott. Steven Falowski has consulting agreements with Medtronic, Abbott, and Shiratronics. teven Falowski is a research investigator with Abbott, Medtronic, CornerLoc, Aurora, and Saluda.He also has stocks or stock options with SPR Therapeutics, Saluda, Aurora, SurgenTec, Synerfuse, BackStop Neural, PainTeq, and is an owner of CornerLoc. The authors report no other conflicts of interest in this work.
References
1. Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356–2367. doi:10.1016/s0140-6736(18)30480-x
2. Hoy D, Bain C, Williams G, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028–2037. doi:10.1002/art.34347
3. Baron R, Binder A, Attal N, Casale R, Dickenson AH, Treede RD. Neuropathic low back pain in clinical practice. Eur J Pain. 2016;20(6):861–873. doi:10.1002/ejp.838
4. Vos T, Barber R, Bell B, et al; Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743–800. doi:10.1016/s0140-6736(15)60692-4
5. Morlion B. Chronic low back pain: pharmacological, interventional and surgical strategies. Nat Rev Neurol. 2013;9(8):462–473. doi:10.1038/nrneurol.2013.130
6. Schmidt CO, Raspe H, Pfingsten M, et al. Back pain in the German adult population: prevalence, severity, and sociodemographic correlates in a multiregional survey. Spine. 2007;32(18):2005–2011. doi:10.1097/BRS.0b013e318133fad8
7. Patel AT, Ogle AA. Diagnosis and management of acute low back pain. Am Family Phys. 2000;61(6):1779–86,1789–90.
8. Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8(1):8–20. doi:10.1016/j.spinee.2007.10.005
9. Armstrong SA, Herr MJ. Physiology, Nociception. In: StatPearls. StatPearls Publishing LLC; 2024.
10. Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478–491. doi:10.7326/0003-4819-147-7-200710020-00006
11. Excellence NIfHaC. Early management of persistent non 2010 specific low back pain. 2009.
12. Centre for Clinical Practice at N. National Institute for Health and Clinical Excellence: guidance. In: Neuropathic Pain: The Pharmacological Management of Neuropathic Pain in Adults in Non-Specialist Settings. National Institute for Health and Clinical Excellence (UK); 2010.
13. Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J. 2010;19(12):2075–2094. doi:10.1007/s00586-010-1502-y
14. Attal N, Cruccu G, Baron R, et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010;17(9):1113–e88. doi:10.1111/j.1468-1331.2010.02999.x
15. Dworkin RH, Turk DC, McDermott MP, et al. Interpreting the clinical importance of group differences in chronic pain clinical trials: IMMPACT recommendations. Pain. 2009;146(3):238–244. doi:10.1016/j.pain.2009.08.019
16. Clark JD, Bair MJ, Belitskaya-Lévy I, et al. Sequential and Comparative Evaluation of Pain Treatment Effectiveness Response (SCEPTER), a pragmatic trial for conservative chronic low back pain treatment. Contemp Clin Trials. 2023;125:107041. doi:10.1016/j.cct.2022.107041
17. Martinez V, Attal N, Vanzo B, et al. Adherence of French GPs to chronic neuropathic pain clinical guidelines: results of a cross-sectional, randomized, “e” case-vignette survey. PLoS One. 2014;9(4):e93855. doi:10.1371/journal.pone.0093855
18. Kumar A, Felderhof C, Eljamel MS. Spinal cord stimulation for the treatment of refractory unilateral limb pain syndromes. Stereotact Funct Neurosurg. 2003;81(1–4):70–74. doi:10.1159/000075107
19. Kumar S, Rampp T, Kessler C, et al. Effectiveness of Ayurvedic Massage (Sahacharadi Taila) in patients with chronic low back pain: a randomized controlled trial. J Altern Complement Med. 2017;23(2):109–115. doi:10.1089/acm.2015.0272
20. D’Souza RS, ElSaban M, Martinez Alvarez GA, Jin MY, Kubrova E, Hassett LC. Treatment of pain in length-dependent peripheral neuropathy with the use of spinal cord stimulation: a systematic review. Pain Med. 2023;24(Supplement_2):S24–S32. doi:10.1093/pm/pnad091
21. Manchikanti L, Sanapati MR, Soin A, et al. An updated analysis of utilization of epidural procedures in managing chronic pain in the Medicare population from 2000 to 2018. Pain Physician. 2020;23(2):111. doi:10.36076/ppj.2020/23/111
22. Van Buyten JP. Neurostimulation for chronic neuropathic back pain in failed back surgery syndrome. J Pain Sympt Manage. 2006;31(4 Suppl):S25–9. doi:10.1016/j.jpainsymman.2005.12.012
23. Ahmed S, Yearwood T, De Ridder D, Vanneste S. Burst and high frequency stimulation: underlying mechanism of action. Expert Rev Med Devices. 2018;15(1):61–70. doi:10.1080/17434440.2018.1418662
24. Deer T, Gilligan C, Falowski S, et al. Treatment of refractory low back pain using passive recharge burst in patients without options for corrective surgery: findings and results from the DISTINCT Study, a prospective randomized multicenter controlled trial. Neuromodulation. 2023;26(7):1387–1399. doi:10.1016/j.neurom.2023.07.009
25. Kapural L, Yu C, Doust MW, et al. Novel 10-kHz high-frequency therapy (HF10 therapy) is superior to traditional low-frequency Spinal cord stimulation for the treatment of chronic back and leg pain: the SENZA-RCT randomized controlled trial. Anesthesiology. 2015;123(4):851–860. doi:10.1097/ALN.0000000000000774
26. Al-Kaisy A, Royds J, Palmisani S, et al. Multicentre, double-blind, randomised, sham-controlled trial of 10 khz high-frequency spinal cord stimulation for chronic neuropathic low back pain (MODULATE-LBP): a trial protocol. Trials. 2020;21(1):111. doi:10.1186/s13063-019-3831-4
27. Bell GK, Kidd D, North RB. Cost-effectiveness analysis of spinal cord stimulation in treatment of failed back surgery syndrome. J Pain Sympt Manage. 1997;13(5):286–295. doi:10.1016/s0885-3924(96)00323-5
28. Lad SP, Petraglia III FW, Kent AR, et al. Longer delay from chronic pain to spinal cord stimulation results in higher healthcare resource utilization. Neuromodulation. 2016;19(5):469–476. doi:10.1111/ner.12389
29. North R, Shipley J. Practice parameters for the use of spinal cord stimulation in the treatment of chronic neuropathic pain. Pain Med. 2007;8:S200–S275.
30. Hoelscher C, Riley J, Wu C, Sharan A. Cost-effectiveness data regarding spinal cord stimulation for low back pain. Spine. 2017;42(Suppl 14):S72–S79. doi:10.1097/BRS.0000000000002194
31. Kumar K, Wilson J. Factors Affecting Spinal Cord Stimulation Outcome in Chronic Benign Pain With Suggestions to Improve Success Rate. Springer; 2007.
32. Mekhail N, Deer TR, Poree L, et al. Cost-effectiveness of dorsal root ganglion stimulation or spinal cord stimulation for complex regional pain syndrome. Neuromodulation. 2021;24(4):708–718. doi:10.1111/ner.13134
33. Rojo E, Pérez Hernández C, Sánchez Martínez N, et al. Real-world cost-effectiveness analysis of spinal cord stimulation vs conventional therapy in the management of failed back surgery syndrome. J Pain Res. 2021;14:3025–3032. doi:10.2147/JPR.S326092
34. Taylor RS, Lad SP, White JL, et al. Health care resource utilization and costs in patients with painful diabetic neuropathy treated with 10 kHz spinal cord stimulation therapy. J Manag Care Specialty Pharm. 2023;29(9):1021–1029. doi:10.18553/jmcp.2023.29.9.1021
35. Farber SH, Han JL, Elsamadicy AA, et al. Long-term cost utility of spinal cord stimulation in patients with failed back surgery syndrome. Pain Physician. 2017;20(6):E797–e805.
36. Braun E, Khatri N, Kim B, et al. A prospective, randomized single-blind crossover study comparing high-frequency 10,000 hz and burst spinal cord stimulation. Neuromodulation. 2023;26(5):1023–1029. doi:10.1016/j.neurom.2022.10.054
37. Duarte RV, Nevitt S, McNicol E, et al. Systematic review and meta-analysis of placebo/sham controlled randomised trials of spinal cord stimulation for neuropathic pain. Pain. 2020;161(1):24–35. doi:10.1097/j.pain.0000000000001689
38. Spears CA, Hodges SE, Kiyani M, et al. Health care resource utilization and management of chronic, refractory low back pain in the United States. Spine. 2020;45(20):E1333–E1341. doi:10.1097/BRS.0000000000003572
39. Rubin DB. Matching to remove bias in observational studies. Biometrics. 1973;29(1):159–183. doi:10.2307/2529684
40. Patel NP, Wu C, Lad SP, et al. Cost-effectiveness of 10-kHz spinal cord stimulation therapy compared with conventional medical management over the first 12 months of therapy for patients with nonsurgical back pain: randomized controlled trial. J Neurosurg Spine. 2023;38(2):249–257. doi:10.3171/2022.9.Spine22416
41. Mody RR, Meyer KL, Ward JM, O’Day KB. Cost per patient achieving treatment targets and number needed to treat with Tirzepatide Versus Semaglutide 1 mg in patients with type 2 diabetes in the United States. Diabet Ther. 2023;14(12):2045–2055. doi:10.1007/s13300-023-01470-w
42. Martin M. An introduction to bootstrap methods with applications to R by M.R. Chernick and R.A. LaBudde. Aust NZ J Stat. 2012;54:253–255. doi:10.1111/j.1467-842X.2012.00663.x
43. Neumann PJ, Ganiats TG, Russell LB, Sanders GD, Siegel JE. Cost-Effectiveness in Health and Medicine.
44. Dubois RW. Cost-effectiveness thresholds in the USA: are they coming? Are they already here? J Comp Eff Res. 2016;5(1):9–11. doi:10.2217/cer.15.50
45. Adil SM, Charalambous LT, Spears CA, et al. Impact of spinal cord stimulation on opioid dose reduction: a nationwide analysis. Neurosurgery. 2020;88(1):193–201. doi:10.1093/neuros/nyaa353
46. Hatcher S, Jacobs D, Air EL. 203 opioid reduction after SCS. Neurosurgery. 2022;68(Supplement_1):62. doi:10.1227/NEU.0000000000001880_203
47. Gupta M, Abd-Elsayed A, Knezevic NN. Improving care of chronic pain patients with spinal cord stimulator therapy amidst the opioid epidemic. Neurol Sci. 2020;41(10):2703–2710. doi:10.1007/s10072-020-04435-0
48. Hunter CW, Carlson J, Yang A, et al. BURST(able): a retrospective, multicenter study examining the impact of Spinal cord stimulation with burst on pain and opioid consumption in the setting of salvage treatment and “upgrade”. Pain Physician. 2020;23(6):E643–e658.
49. Kumar K, Taylor RS, Jacques L, et al. Spinal cord stimulation versus conventional medical management for neuropathic pain: a multicentre randomised controlled trial in patients with failed back surgery syndrome. Pain. 2007;132(1–2):179–188. doi:10.1016/j.pain.2007.07.028
50. Mekhail NA, Aeschbach A, Stanton-Hicks M. Cost benefit analysis of neurostimulation for chronic pain. Clin J Pain. 2004;20(6):462–468. doi:10.1097/00002508-200411000-00012
51. Fraifeld EM, Hatheway JA, Ricker CN. Systemic opioid prescribing patterns and total cost of care in patients initiating spinal cord stimulation therapy: a retrospective analysis. Pain Med. 2021;22(4):784–799. doi:10.1093/pm/pnab033
52. Deer T, Slavin KV, Amirdelfan K, et al. Success using neuromodulation with BURST (SUNBURST) study: results from a prospective, randomized controlled trial using a novel burst waveform. Neuromodulation. 2018;21(1):56–66. doi:10.1111/ner.12698
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




