Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 17
A Mixture of Water-Soluble Polysaccharides Reduces Caspase-1 and IL-1β Inflammatory Responses by Cutibacterium acnes in vitro in Reconstructed Human Epidermis (RHE)
Authors Gruber JV , Terpak N , Massard S, Chen X, Kim Y
Received 20 July 2024
Accepted for publication 30 October 2024
Published 21 November 2024 Volume 2024:17 Pages 2627—2633
DOI https://doi.org/10.2147/CCID.S487881
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Monica K. Li
James V Gruber,1 Nicole Terpak,2 Sebastien Massard,2 Xiang Chen,2 Yurah Kim2
1Research, Vantage, Fairfield, NJ, USA; 2Research, Vantage, Warren, NJ, USA
Correspondence: James V Gruber, Email [email protected]
Introduction: It is well established that Cutibacterium acnes (C. acnes) is a common skin commensal microorganism that has been linked to acne. In acne flare-ups, C. acnes can be found in abundant levels within the inflammatory lesions (called comedones) associated with the skin disease. Recently, it was reported that 3D reconstructed human epidermis (RHE) treated with viable cultures of C. acnes can elicit β-defensin antimicrobial peptide responses in the skin and can weaken the skin barrier of the RHE after three days of exposure to C. acnes.
Methods: Employing a modification of this in vitro assay, RHE was pretreated with C. acnes for 48 hours, then further treated with a mixture of water-soluble polysaccharides (STRATAPHIX™ POLY, “Polysaccharide Blend”) previously shown to reduce inflammasome-mediated inflammatory responses in normal human epidermal keratinocytes (NHEK). Two inflammasome-mediated inflammation markers were tested, including caspase-1, a potent protease enzyme activated by NOD-like receptor protein (NLRP)-induced inflammasome activation, and interleukin-1β (IL-1β), a cytokine which is activated from inactive pro-IL-1β by caspase-1.
Results: The treatment of the RHE tissues with C. acnes for 48 hours elicited an inflammatory response measured with both markers compared against untreated tissues. Treatment of the tissues with 1% and 2% salicylic acid for 24 hours after C. acnes treatment increased the inflammatory response measured with both markers. Application of the water-soluble polysaccharides in combination with 1% and 2% of salicylic acid significantly reduces expression of both active caspase-1 and IL-1β compared against the tissues treated with C. acnes and salicylic acid alone.
Discussion: The results lend further support to previously reported work which was done on NHEKs treated with ultraviolet B (UVB) light and adenosine triphosphate (ATP) and demonstrate that the same mixture of polysaccharides can have a modulating effect against bacterial and chemical induced inflammation in RHE.
Keywords: Cutibacterium acnes, In vitro, tissues, inflammation, caspase-1, IL-1β, topical
Introduction
Acne is a skin condition that affects individuals throughout their lives. The causes of acne are complex and are principally based on a person’s genetics, while a person’s age, eating habits, hygiene, and hormonal changes among other etiologies can also play a significant role in the progress of the disease.1 However, emerging now is a more nuanced understanding of the causes of acne that appear to be linked to the skin’s innate immunity and the communication between the skin’s living cells, including epithelial and immune cells, and Cutibacterium acnes (C. acnes), a known skin commensal that is associated with acne.2,3 More profoundly, it now appears that acne may have a relationship to various acneic strains of C. acnes, so-called bad C. acnes, against strains that are known to be less pathogenic.4 Acne inflammation has also been directly linked to inflammasome-mediated inflammation cascades.5–7 It has been reported that NOD-like receptor protein (NLRP) inflammasome-mediated release of inflammatory markers can occur in sebocytes, the cells responsible for formation of sebum, including sebocytes treated with C. acnes.8,9
Presently, there are five topical active ingredients that are approved by the US FDA for the treatment of acne, including salicylic acid, benzoyl peroxide, sulfur, resorcinol, and resorcinol monoacetate and combinations of resorcinol and resorcinol monoacetate with sulfur.10 Regardless of the complexity of the source of the disease, it has been found that if the increase in C. acnes is controlled either by antibiotics, retinoids, topical antimicrobials like benzoyl peroxide or salicylic acid, or combinations of treatments that control the growth of the C. acnes, the condition can be made to improve.11,12 As noted in the work by Monteiro and Fernandes, the overabundant use of antibiotics is frowned upon as it facilitates the growth of bacteria that possess antimicrobial resistance.13
It was previously reported by Gruber and Holtz that normal human epidermal keratinocytes pretreated with either UVB or ATP demonstrated an upregulation of NLRP inflammasome-mediated release of caspase-1, a potent protease enzyme that can elicit further downstream inflammatory responses through the activation of IL-1β and IL-18.14 Reconstructed human epidermis (RHE) models colonized with skin microorganisms have begun to emerge, showing a good relevance and pertinency. The challenge with trying to grow skin commensals or potentially other probiotics on such in vitro tissue models is that they can overwhelm the tissue growth and thus simply become a contaminant in the model. However, recently Gruber and colleagues reported on the topical treatment of RHE models with a probiotic treatment containing viable Lactobacillus plantarum cultures that demonstrated an ability to upregulate elastin in these tissue models.15,16 In a recent study run by Khmaladze et al, it was noted that topical treatment of skin equivalents with a formulation containing living Lactobacillus reuteri DSM 17938 can contribute to antiaging benefits on the skin.17 Another interesting finding in that study demonstrated that living probiotics behave differently on RHE models than non-living bacterial lysates of the same probiotic. This work provides a cautionary note that living and dead probiotics can behave quite differently on skin. Meloni and Balzaretti have described an in vitro testing model in which the skin commensal microbes C. acnes and Malassesia restricta are grown on RHE.18 The model assayed the influence of skin commensals on skin barrier structure, cellular proliferation and differentiation, and expression of anti-microbial defenses.
In the present work, the model described by Meloni et al was modified to examine the influence of C. acnes to modulate skin inflammatory responses including effects on caspase-1 and IL-1β. Both inflammatory markers are known to be expressed in epidermal keratinocytes which make up the epidermal layer of the RHE models.14 By demonstrating that the topical application of C. acnes could upregulate these two critical skin inflammatory markers associated with inflammatory acne lesions, it was possible to then investigate the influence of a monographed acne treatment, salicylic acid, alone and in combination with the water-soluble polysaccharide blend described earlier by Gruber and Holtz.14
Materials and Methods
Reconstructed Human Epidermis
The 3D human epidermis full thickness EpiDermFT (EFT-400, MatTek Company; production site: Bratislava, Slovakia) consists of a fully differentiated epidermis with cornified epidermal layers: keratin 5 expressed in basal cells, and involucrin and keratin 10 expressed in the spinous and granular layers. The dermal compartment is composed of a collagen matrix containing viable normal human dermal fibroblasts (NHDF). The epidermal and dermal layers are mitotically and metabolically active and exhibit in vivo-like morphological and growth characteristics which are uniform and highly reproducible. A well-developed basement membrane is present at the dermal/epidermal junction. The tissues are cultured on specially prepared cell culture inserts (surface 1.0 cm²) where all biological components of the epidermis and the culture medium are tested by the manufacturer for viral, bacterial, fungal, and mycoplasma contamination. The tissues are shipped at 4°C in 24-well plates containing a nutrient agarose gel and may be stored at 2–8°C for up to 6 days prior to use. Cultures can be continued for up to 2 weeks with good retention of normal epidermal morphology.
Immediately after arrival of the test system in the laboratory, data sheets enclosed with the batch, shipment integrity, color, and temperature of the agar medium used for transport were checked. The tissues were then removed from the agarose nutrient solution under a sterile air flow cabin. The inserts were rapidly transferred to 12-well plate previously filled with culture medium without antibiotics and incubated at 37°C, 5% CO2, saturated humidity. On the day of the test, the medium was replaced with fresh growth medium without antibiotics.
Test Materials
All test materials were provided by Vantage [Warren, NJ] and are summarized in Box 1. STRATAPHIX™ POLY [INCI: Water (and) Glycerin (and) Laminaria Digitata Extract (and) Opuntia Ficus Indica Stem Extract (and) Galactoarabinan (and) Schizophyllan], referred to in this work as the “Polysaccharide Blend”, was previously shown to influence the expression of caspase-1 in UVB and ATP-treated normal human epidermal keratinocytes.14
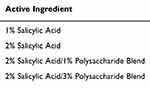 |
Box 1 Summary of Active Ingredients Tested |
Growth of Bacterial Suspension and Tissue Treatments
The testing procedures employed in the present study were modified from early procedures developed by Meloni and Balzaretti with the following changes.18 Before the assay, the test strain C. acnes ATCC 11827 was sown on agar culture medium, starting from glycerinate culture stored at <-70°C and incubated at 37°C, for 1–2 days in anaerobic conditions to check its normal colony morphology. A second subculture was performed that used fresh culture.
Preparation of Microbial Suspension and Colonization Procedure
On the day of the test, the bacterial suspension was resuspended in sterile saline solution, adjusting the concentration level to 107–108 CFU/mL by optical density (OD) reading (via spectrophotometer), considering an application volume of 60 μL. The bacterial suspension was then used for the FT skin colonization procedure: 6 μL of lipid mix (olive oil and neutral TAG mixed 1:1) on the tissue surface added with 60 μL of C. acnes ATCC 11827, 107–108 CFU/mL for 72 h at 37°C, 5% CO2 and 90% RH. A viable count on agar plates was performed to check the starting inoculum concentration. After 48 h of colonization, the inoculum excess was removed before treatment with 5 μL of the test item that was applied on the epidermal surface for each dedicated series for 24 h. At the end of the treatment period, media were collected and stored at −20°C for the ELISA assay. The entire assay procedure is shown schematically in Figure 1.
 |
Figure 1 Assay protocol schematic. |
ELISA Assay
Culture media collected at 72 h were analyzed for caspase-1 and TNF-α by ELISA test using biological triplicate quantified in technical duplicate. Each inflammatory marker in the culture media has been quantified with a commercially available kit and according to internal procedures.
• Human Caspase-1/ICE Immunoassay (Catalog Number DCA100, R&D Systems, Minneapolis, MN)
• Human IL-1β (Catalog Number DLB50, R&D Systems, Minneapolis, MN)
Optical density (OD) was read at 450 nm using the TECAN INFINITE M-200 spectrophotometer, and readings at 570 nm were subtracted from the readings at 450 nm. This subtraction corrects for optical imperfections in the plate.
Statistical Analysis
The OD data were analyzed using the paired Student’s T-test with statistical significance set at p≤0.05. In all instances examined, the data for the negative control were not reported as all values discussed below in the studies were statistically significant against the negative control.
Results and Discussion
Caspase-1 Results
Results from the treatment of RHE tissues with C. acnes followed by treatments of 1% and 2% salicylic acid and 2% salicylic acid combined with 1% and 3% of the polysaccharide blend are shown in Figure 2. The data from the caspase-1 expression demonstrate that the treatment of the RHE tissue with C. acnes causes an initial increase in expression of caspase-1 compared against untreated controls (data not shown). This result is consistent with known literature that demonstrates that C. acnes can elicit an NLPR inflammasome-driven response via release of active caspase-1 from skin, principally from the keratinocytes in the epidermis, but also from the sebocytes and immune cells known to reside in the skin.12 When the tissues treated with C. acnes were then treated with 1% (p=0.00008) and 2% (p=0.001) of salicylic acid after treatment with the C. acnes, there was an additional statistically significant increase in the expression of caspase-1 in the tissues. However, there was no statistically significant difference between the 1% and 2% treatment with salicylic acid, 2% salicylic acid being the highest level allowed by the FDA for leave-on acne treatments in the US.10
When the 2% salicylic acid was blended with 1% (p=0.002) and 3% (p=0.02) of the polysaccharide blend, it was found that the level of caspase-1 expression dropped significantly below the levels noted for 2% salicylic acid alone, and at the 3% levels of the polysaccharide blend the levels of caspase-1 expression drop significantly compared to the C. acnes-treated tissue control (p=0.02). The data further support the results found in earlier studies with the same polysaccharide blend that demonstrated reduction in caspase-1 expression in keratinocytes after elicitation of an inflammatory response by UVB and ATP.14
IL-1β Results
Examination of the release of IL-1β from the RHE tissues demonstrated a somewhat similar effect compared to the caspase-1 expression, Figure 3. IL-1β exists in cells in a non-active pro-cytokine form which must be activated by caspase-1 to become active IL-1β.12,14 At this point, the IL-1β can be released extracellularly and thus is able to spread the inflammatory response to other cells in the tissue. Data shown in Figure 3 demonstrate that treatment of the RHE tissues with C. acnes increases the expression of IL-1β compared to untreated controls (data not shown). Further treatment with 1% (p=0.002) and 2% (p=0.0003) salicylic acid increased expression of IL-1β above the levels noted for the C. acnes treatment alone. Addition of 1% (p=0.05) and 3% (p=0.02) of the polysaccharide blend demonstrated a statistically significant decrease of IL-1β expression compared to the salicylic acid treatments alone. The levels of IL-1β never dropped below the levels of the C. acnes-treated tissues as was noted above for caspase-1 expression.
Conclusions
Acne can be a serious problem for many people, causing not only physical impairments but also psychological concerns as well. The use of antibiotics and retinoids has been beneficial at helping individuals overcome acne, but, particularly in the case of antibiotics, the potential for the development of antimicrobial-resistant microbes is a serious concern. In this respect, topical treatments are considered an excellent primary treatment regimen for mild acne and as a combination for more serious acne where antibiotics and retinoids are used as well. In the pantheon of topical actives that can treat acne in the US, the FDA’s list of approved ingredients is not lengthy.
Previous work by Gruber and Holtz examined the influence of the polysaccharide blend on NHEKs activated with UVB and ATP.14 In the present study, the work extends the external threats that activate the inflammasomes to topically applied C. acnes and salicylic acid. The testing demonstrates an emerging in vitro testing model in which C. acnes is allowed to interact with RHE tissues prior to application of active ingredients and shows that C. acnes influences the expression of NLRP inflammasome-mediated expression of caspase-1 and IL-1β. The current work extends the findings from previous work reported by Gruber and Holtz, in which NHEKs were tested solely for the release of NLRP inflammasome-mediated caspase-1. The testing reported here extends the skin inflammatory targets to caspase-1 and to a further downstream inflammatory target, IL-1β, known to be activated by the release of active caspase-1. The two inflammatory markers are further activated by topical application of 1% and 2% salicylic acid. In examining the maximum FDA allowable leave-on levels of salicylic acid allowed for acne treatments, ie 2%, in combination with 1% and 3% of the polysaccharide blend, it was found that the polysaccharides can significantly reduce the expression of the inflammation markers. This further demonstrates benefits from the polysaccharide blend that had previously been shown to influence NLRP inflammasome-mediated expression of caspase-1 driven by UVB and ATP in NHEKs. The data support the ability to modulate skin inflammatory responses in vitro in a new C. acnes tissue testing assay.
Clinically, the ability to combine a non-therapeutic treatment with an approved topical acne treatment, ie salicylic acid, may allow for improved efficacy of salicylic acid. Known primarily for its ability to control the growth of C. acnes, and for its keratolytic effects on acne comedones, salicylic acid combined with ingredients that can also help modulate the inflammatory response associated with acne flare-ups may extend the benefits of the approved acne treatment. In addition, by reducing inflammatory response driven by the skin’s innate immune response, it may also be possible to help improve post-inflammatory erythema (PIE) and post-inflammatory hyperpigmentation (PIH) in skin afflicted with acne lesions. Studies on these benefits are ongoing and will be reported in later work.
Acknowledgment
The studies reported here were done in collaboration with VitroScreen Srl [Milano, IT].
Disclosure
The authors report no conflicts of interest in this work.
References
1. Mias C, Mengeaud V, Pessou-Touya S, Dupaln H. Recent advances in understanding acne: deciphering the relationship between Cutibacterium acnes and TH17 inflammatory pathway. Eur Acad Dermatol Venereol. 2023;37(Suppl. 2):3–11. doi:10.1111/jdv.18794
2. Kurokawa I, Nakase K. Recent advances in understanding and managing acne. F1000Research. 2020;9:792–800. doi:10.12688/f1000research.25588.1
3. Schachner LA, Alexis AF, Andriessen A, et al. Insights into acne and skin barrier: optimizing treatment regimens with ceramide-containing skincare. J Cosmet Dermatol. 2023;22:2902–2908. doi:10.1111/jocd.15946
4. Borrel V, Gaannesen AV, Barreau M, et al. Adaptation of acneic and non acenic strains of Cutibacterium acnes to sebum-like environment. MicrobiolgyOpen. 2019;8:e841. doi:10.1002/mbo3.841
5. Contassot E, French LE. New insights into acne pathogenesis: Propionibacterium acnes activates the inflammasomes. J Invest Dermatol. 2014;134:310–313. doi:10.1038/jid.2013.505
6. Thiboutot DM. Inflammasome activation by Propionibacterium acnes: the story of IL-1 in acne continues to unfold. J Invest Dermatol. 2014;134:595–597. doi:10.1038/jid.2013.528
7. Kistowska M, Gehrke S, Jankovic D, et al. IL-1β drives inflammatory responses to Propionibacterium acnes in vitro and in vivo. J Invest Dermatol. 2014;134:677–685 doi:10.1058/jid.2013.438.
8. Jung YR, Shi JM, Kim CH, et al. Activation of NLRP3 inflammasomes by palmitic acid in human sebocytes. Ann Dermatol. 2021;33:541–548. doi:10.5021/ad.2021.33.6.541
9. Li ZJ, Choi DK, Sohn KC, et al. Propionibacterium acnes activates the NLRP3 inflammasomes in human sebocytes. J Invest Dermatol. 2014;134:2747–2756. doi:10.1038/jid.2014.221
10. U.S. Food and Drug Administration. Availabe from: 21CFR333: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=333&showFR=1&subpartNode=21:5.0.1.1.14.4.
11. Firlej E, Kowalska W, Szymaszek K, Rolinski J, Bartosinski J. The role of skin immune system in acne. J Clin Med. 2022;11:1579. doi:10.3390/jcm11061579
12. Zhu W, Wang HL, Bu XL, Zhang JB, Lu YG. A narrative review of research progress on the role of NLRP3 inflammasome in acne vulgaris. Ann Transl Med. 2022;10:645. doi:10.21037/atm-21-5924
13. Monteiro RC, Fernandes M. Are antibiotics still relevant in acne? A review of the therapeutic conundrum. Int J Dermatol. 2024;63:306–310. doi:10.1111/ijd.16854
14. Gruber JV, Holtz R. In vitro expression of NLRP inflammasome-induced active caspase-1 expression in normal human epidermal keratinocytes (NHEK) by various exogenous threats and subsequent inhibition by naturally derived ingredient blends. J Inflamm Res. 2019;12:219–230. doi:10.2147/JIR.S215776
15. Gruber JV, Holtz R. Living, quiescent Lactobacillus plantarum Lp90 probiotic, delivered topically to full thickness tissues in vitro via a just-add-water cream delivery system, stimulates the expression of elastin protein. J Cosmet Dermatol. 2023;22:2852–2860. doi:10.1111/jocd.15927
16. Gruber JV, Holtz R. Examining the Genomic Influence of Topically Applied Probiotics In Vitro. Int J Cosmet Sci. 2024. doi:10.1111/ics.12999
17. Khmaladze I, Butler E, Fabre S, Gillbro JM. Lactobacillus reuteri DSM 17938-A comparative study on the effect of probiotics and lysates on human skin. Exp Dermatol. 2019;28:822–828. doi:10.1111/exd.13950
18. Meloni M, Balzaretti S. Skin Microbiome Handbook: from Basic Research to Product Development. In: Dayan N, editor. In: Three-Dimensional Human Skin Models to Investigate Skin Innate and Immune-Mediated Responses to Microorganisms. Beverly, MA: Scrivener Publishing; 2020:277–288.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Toll-like Interleukin -1 Receptor Regulator (TILRR) Protein, a Major Modulator of Inflammation, is Expressed in Normal Human and Macaque Tissues and PBMCs
Kashem MA, Li L, Yuan XY, Plummer FA, Luo M
Journal of Inflammation Research 2022, 15:2925-2937
Published Date: 12 May 2022
VRT-043198 Ameliorates Surgery-Induced Neurocognitive Disorders by Restoring the NGF and BNDF Expression in Aged Mice
Tang Q, Guo Q, Li K, Fei F
Neuropsychiatric Disease and Treatment 2022, 18:1027-1037
Published Date: 16 May 2022
Cannabidiol Inhibits Inflammation Induced by Cutibacterium acnes-Derived Extracellular Vesicles via Activation of CB2 Receptor in Keratinocytes
Jiang Z, Jin S, Fan X, Cao K, Liu Y, Wang X, Ma Y, Xiang L
Journal of Inflammation Research 2022, 15:4573-4583
Published Date: 11 August 2022
Special Focus on the Cellular Anti-Inflammatory Effects of Several Micro-Immunotherapy Formulations: Considerations Regarding Intestinal-, Immune-Axis-Related- and Neuronal-Inflammation Contexts
Jacques C, Floris I
Journal of Inflammation Research 2022, 15:6695-6717
Published Date: 13 December 2022
The Mechanism of Pyroptosis and Its Application Prospect in Diabetic Wound Healing
Al Mamun A, Shao C, Geng P, Wang S, Xiao J
Journal of Inflammation Research 2024, 17:1481-1501
Published Date: 6 March 2024



