Back to Journals » Journal of Multidisciplinary Healthcare » Volume 18
A Multidisciplinary and Longitudinal Framework for Enhancing Innovation Efficiency in Healthcare Systems
Authors Szentpeteri JL , Szabo P, Liber N, Pandur E, Deak M , Csutak A, Sik A
Received 28 November 2024
Accepted for publication 25 February 2025
Published 8 April 2025 Volume 2025:18 Pages 1969—1984
DOI https://doi.org/10.2147/JMDH.S497613
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Jozsef L Szentpeteri,1 Peter Szabo,1 Noemi Liber,1 Eva Pandur,1 Mate Deak,1 Adrienne Csutak,2 Attila Sik1,3,4
1Institute of Transdisciplinary Discoveries, Medical School, University of Pecs, Pecs, Hungary; 2Department of Ophthalmology, Medical School, University of Pecs, Pecs, Hungary; 3Institute of Physiology, Medical School, University of Pecs, Pecs, Hungary; 4Obuda University, University Research and Innovation Center, Budapest, Hungary
Correspondence: Attila Sik, Institute of Physiology, Medical School, University of Pecs, Szigeti ut 12, Pecs, 7622, Hungary, Tel +36 70 551 5252, Email [email protected]
Introduction: Healthcare spending constitutes a significant portion of the GDP. Innovation in healthcare lowers healthcare costs, improves outcomes, and increases service quality. Several obstacles hinder most innovative efforts in hospitals. Often, supposed innovative solutions fail to address existing problems, which do not translate into market-ready solutions and lack economic or social value. Improvement in healthcare innovation efficiency saves a considerable amount of money and lives. Drawing on multidisciplinary frameworks of concepts and practices, this study develops a comprehensive methodology to change hospital innovation organizational culture and improve innovation efficiency.
Methods: We designed a comprehensive framework from problem identification through to product development involving university students, clinical staff, medical doctors, and researchers working in a non-medical field. Two novel elements were introduced: the Champion Network (medical doctors) and the Discovery Team (members working in non-medical fields). Coaching and mentoring the clinical staff, innovation courses, and hackathon events for students were also part of the framework.
Results: The involvement of clinical staff and the number of intellectual product disclosures increased by an average of 10% in 3 years despite the COVID-19 challenge. Out of many identified problems, IT and process management stood out as a general problem in all eight analyzed clinics. Hardware and software solutions were created during the program.
Discussion: Introducing various layers of participants in the innovation process, including non-medical professionals and students, changes the attitude of healthcare professionals towards innovation and can result in a product or service development addressing real-life needs. Our research shows that a holistic approach involving healthcare professionals and non-medical experts from various levels in their careers, ranging from undergraduate students to senior leaders, changes innovation culture and generates solutions for existing real-life problems.
Keywords: organizational culture, framework, multidisciplinary innovation, mentoring and coaching, clinics
Introduction
Healthcare spending constitutes a significant portion of GDP in every country. In 2015, for instance, the US allocated 16.9% of its GDP to healthcare, while the UK spent 9.8%. Other advanced nations had healthcare expenditures ranging from 8.9% to 11.5% of their GDP. This equates to per capita spending of $9451 in the US and $4003 in the UK.1 In Central Europe, the healthcare expenditure relative to GDP in 2020 varied between 6.3% (Romania) and 9.2% (Czechia).2 Healthcare spending in Hungary in the same year was 7.2%, equating to $1160 per capita. Most of the expenditures are financed by public resources (5%) in contrast to private ones (2.7% in 2011).3 Unfortunately, substantial expenditures on healthcare do not necessarily lead to improved services. Approximately one-third of the financial resources are wasted on unnecessary treatments, poor care coordination, administrative complexities, overpriced medications, and other inefficiencies.4 Therefore, optimization of procedures and workflows with the potential to save healthcare expenditures is one of the primary goals of the healthcare system in every country.4 Innovation may lower healthcare costs, improve outcomes, and elevate service quality. Traditionally, cost-saving innovations encompass new drugs, medical devices, process improvements, and alternatives such as using ambulatory surgery centers instead of hospital outpatient departments.5 However, several obstacles hinder most innovative efforts in hospitals and many other organizations. Often, supposed innovative solutions fail to address existing problems instead of targeting trivial issues. These ideas might be inventive, presenting new solutions to specific problems, but they often do not translate into market-ready solutions and lack economic or social value. Universities and hospitals have numerous such inventions, managed by Technology Transfer Officers, that never achieve success despite being patented due to limited market interest. Innovating within an existing healthcare system is challenging, as disruptive innovations are hard to achieve internally due to the system’s complexity and established path dependencies.6 Despite the challenges, methods to improve innovation efficiency in the healthcare arena have been developed in the past. Innovation funds were set up worldwide,7–9 and hackathons (rapid innovation challenge games) were run in many countries, focusing on a given challenge.10 Uncovering, however, the focus areas and potential processes to promote innovation within an organization have only been recently addressed. Mentoring interested clinical staff, including the unit leaders, is the focus of the HealthIL network (www.healthil.org) with headquarters in Israel. In addition to mentoring the clinical staff, obtaining an outsider’s view of the day-to-day running of the clinical unit can provide additional and unforeseen aspects of the activity and uncover hidden inefficiencies that are hidden from the healthcare workforce. Using this approach, more value using fewer resources can be achieved, termed frugal innovation.11,12 Although the concept has originated in resource-constrained contexts, it is now being practiced and implemented by global multinationals such as Sony and GE Healthcare and was proposed to be used in the healthcare environment.13 Resources are usually scarce in the healthcare system; thus approaches that improve efficiency without using resources are much sought after. Multidisciplinary teams, consisting of professionals from the organization, are launched in various organizations to address multifaceted and complex problems.14 Our novel approach, detailed below, takes a different approach and deploys non-medical professionals and university students acting as an observation team. When real-life problems are identified, ideas are generated using various platforms, and products are developed and validated in the clinical environment. The combination of mentoring and a multidisciplinary team proved to be a valuable strategy for improving innovation efficiency in hospital clinics in Hungary.
Theory
Multidisciplinary theory involves combining knowledge and techniques from multiple disciplines to tackle complex issues, comprehend phenomena, or devise solutions. This approach highlights the importance of collaboration among different fields, each contributing its unique perspectives, tools, and expertise. A multidisciplinary approach to address scientific and healthcare-related questions has been successfully used extensively.15,16 It has been proven to be a promising tool when complex cases require designing interventions in hospital settings17 or researching social issues such as bereavement.18 Innovation is the process of creating new ideas, products, services, or methods that provide significant value or improvement over existing solutions. Since it is a complex procedure, we hypothesized that combining expertise from diverse disciplines and using a multi-stakeholder approach will improve innovation efficiency in hospitals in the short term and pave the path to change organizational culture.
The study was conducted in Hungary as the research group had access to various clinics and medical professionals locally. We, however, believe that the framework we present here can be used in other countries with success.
Materials and Methods
Problem Identification and Mentoring
The Champion Network
We pioneered the Champion Network in 2020, starting with three pilot hospital clinics and expanding to 8 by 2022. Our affiliated clinics included 1) Internal Medicine and Nephrology Dental and Oral Surgery, 3) Otorhinolaryngology, 4) Surgery, 5) Rheumatology and Immunology, 6) Ophthalmology, 7) Neurology, and 8) Oncotherapy. To understand clinic issues and barriers to innovation and engage with the community, we asked clinic managers to nominate “Champions” (practicing doctors) who are well-established, open-minded, and influential but not burdened with middle management. Champions participated in EIT (European Institute of Innovation and Technologies) Health Project Plan trainings, informed colleagues about opportunities, helped present our activities, and contributed to policy proposals for promoting innovation. The Innovation Staff (below) organized workshops to enhance their skills in motivating innovation, identifying clinical challenges, and understanding success factors for innovative projects.
The Discovery Team
We established a 10-member Discovery Team to identify and assess organizational challenges. Recruited via faculty contacts and social media, members worked in interdisciplinary pairs (humanities, arts, computer science, education) to monitor clinical processes. Importantly, none of the members were medical doctors. Team members observed daily routines in pilot clinics to pinpoint and address challenges, aiming to enhance efficiency for both staff and patients. The reason for choosing non-clinical members or medical staff is that, without a particular bias, they might be able to see a more general picture of the day-to-day operation of hospital clinics. Their responsibilities included participating in online meetings, visiting designated clinics, documenting issues, proposing solutions, and attending closing meetings for evaluation and implementation planning. To discover potential problems hindering healthcare efficiency in clinics, we developed a methodology and template to facilitate the Discovery Team’s work, requiring them to document challenges based on predefined criteria. Champions in the clinics assisted by enabling interactions with patients, staff, and managers. Team members then individually submitted detailed reports of their findings and suggestions. These reports were evaluated, categorized, and prioritized using a modified methodology from the Israeli center (HealthIL, see below). A report was presented to the leaders of the hospital clinics, followed by personal discussions to determine the next steps.
HealthIL-Based Mentoring
Using the methodology provided by HealthIL (www.healthil.org), we developed our innovation process with the clinical leaders involved in the project through a process of identifying challenges and organizational support mechanisms. We also created our scoring sheet to assess and prioritize the challenges identified by the Discovery Team using the criteria bank provided by the mentors. Informed consent was obtained from all participants of the study.
Data Analysis
The completed survey measuring motivation for innovation was analyzed for qualitative assessment (Supplementary Material 1). The completed template was scored based on the scoring criteria (Supplementary Material 2). Scores were then normalized to get a number between 0 and 1. Where enough data was available, the average and standard deviation were calculated.
Concept Development
To find solutions to the identified and highly ranked problems, we have used various platforms, including hackathons, innovation lectures, and seminars.
Hackathons
The identified problems were presented to students in hackathon events. Groups of students representing various disciplines (engineering, health and medicine, social sciences, and humanities) were formed. Two weeks before the hackathon event, challenges were introduced, providing time for internet searches and brainstorming. During the actual hackathon, which lasted 8–10 hours, assigned mentors (university staff from various departments) provided feedback and help to each team.
Innovation Course
The Innovative Healthcare Technologies course introduced students to innovative technologies in the clinical field and taught the steps of project development and launching start-ups. The theoretical sessions of the course were complemented by practical work, where students had to participate in hackathon events. In the competition, they worked on the challenges identified by the Discovery Team using the knowledge and methods acquired during the course. Innovation projects were set up to develop and implement solutions to the challenges, which require a larger budget, the involvement of experts, and possibly a tender or an external product or service developer partner. The ethical permit number for the study is 10033-PTE/2024 issued by the University of Pecs, Clinical Center, Regional Research Ethics Committee.
Product Development
Hardware Development
The objective was to develop a prototype for improving hand movement in patients suffering from arthritis. An external company was responsible for the product development.
Software Development
The results of the Discovery Team’s surveys showed that IT problems are the second most serious barrier for clinics. The aim was to develop an application with an external company to make digital patient records more manageable, focusing on patient self-management, particularly for long-term treatments.
Results
This study embarked on a longitudinal journey from 2020 to 2022 to explore and enhance clinic efficiency across a broad spectrum of healthcare services. It aimed at evolving the clinic’s operational, technical, and innovation capacities through a blend of methodologies and strategic engagements. The study grew in scope and depth, indicating a successful engagement and operational evolution within the participating clinics.
Building Blocks of the Framework
The framework consisted of separate blocks, shown in Figure 1 and detailed below. The participation of each team is indicated in Table 1. The description of the participants of the study is as follows:
 |
Table 1 Participation of Key Players of the Framework. X Indicates Participation O Represents the Lack of the Particular Player |
Leaders
Those clinical leaders who were invited and selected to the program, who already had an innovative project, were involved in a co-development project with an industrial partner or at least were open to learning innovative approaches and changing the mindset of co-workers. The leaders nominated the Champions, participated in skills development workshops, and were active in meetings to develop solutions to the challenges identified by the Discovery Team.
Champions
Selection criteria, role, and required work are detailed in the Methods section.
Innovation Staff
They designed and implemented the Clinical Innovation Program and analyzed and evaluated the results of surveys and interviews. They also liaised with the Champion Network and Discovery Team members, providing professional guidance and operational support. The Innovation Staff had legal, business, communications, and other knowledge, skills, and experience to support the innovation process.
Healthcare Staff
Physicians, nurses, and residents from the pilot clinics and other university-affiliated clinics comprised the Healthcare Staff involved in the innovation program. Their role was to identify real clinical needs and challenges that could be addressed through project development that had the potential to become a marketable product or service at the end of the process. These individuals did not have access to information and opportunities, had innovation skills gaps, and their environment did not necessarily motivate and inspire them to innovate and engage in innovation.
External Support
An external service provider ran workshops for the Champion Network members, Staff and Leaders, and other clinical managers. The experts were either EIT Health staff, affiliated with EIT Health, or suggested by EIT Health. The main aim of the sessions was to provide tools and methods used in innovation and shape their mindset toward finding new, preferably marketable, solutions for existing problems. The workshops focused on these objectives and explored the problems and challenges with the active participation of the clinical staff.
Discovery Team
The composition, selection criteria, role, and required work to be expected from the Discovery Team members are detailed in the Methods section.
Problem Identification
We have developed a challenge identification and assessment template (see Supplementary Material 3) to be used by the members of the Discovery Team. The template was required to describe the identified challenge and the stakeholders involved in the challenge. It also probed how it is currently being addressed, and finally, proposed solutions, if any, and described the impact if the problem is solved. Within each category, there were further clarification questions.
The challenges received in the completed template were reviewed and grouped by the Innovation Staff. The grouping was based on two main principles. Firstly, by the stakeholders (doctors or patients) and, secondly, by the problem area (process management, infrastructure, communication/language issues, IT/digital solutions). From this list of challenges, only those that could be addressed with an innovative solution were taken forward. In other words, issues such as the lack of parking or the lack of a canteen in the clinic. We then surveyed the challenges to assess if they could be addressed by the teams and the design thinking methodology used by the students in the Innovation Course or Hackathons. For those challenges where this was not possible because, for example, to be a very specific problem, we proposed the creation of an innovation project. In the latter case, a scoring system based on the methodology learned during the HealthIL mentoring was used to establish a priority ranking, which was then reported back to the Leaders of clinics. The priority template had four main aspects: organizational/strategic assessment, clinical and patient-related impact assessment, organizational attention, and ability to adapt and scale. A higher score (between 1 and 5) indicated a higher ranking for a given challenge or project proposal.
Five main problem categories were identified: IT, Communication, Process Management, Infrastructure, and Other (miscellaneous that could not be categorized in the four main categories). Two out of 3 years were analyzed since the Discovery Team started in year 2 of the project (2021). The highest-ranking problem category across clinics was Process Management (0.42 ±0.15), followed by IT, Other, Infrastructure, and Communication (Table 2). There was a difference between specific clinics: Surgery (0.41 ±0.15 in 2021) and Rheumatology (0.41 ±0.15 in 2022) scored the highest, while Ophthalmology had the lowest score (0.24 ±0.01 in 2021 and 0.25 ±0.01 in 2022, Table 3), suggesting clinic-specific challenges.
Mentoring and Skill Development
The EIT Health organization provided individual mentoring sessions for hospital clinic managers, followed by joint workshops. The focus of the project was to identify the strengths and weaknesses in the innovation process, address real-world challenges, and promote innovation within the organization. It also provided an opportunity for the managers to learn methods and techniques for conducting innovation projects. Before the mentoring sessions, an assessment was made of ongoing and completed innovation activities and processes (Supplementary Material 2). The status of the motivation to engage in innovation activities was assessed by motivational questionnaires (Survey column, Table 4). It enabled us to refine the future clinical innovation agenda and scope of activities based on the number of completions and the answers to each question. The Champions helped recruit participants to various workshops held either by the Innovation Staff or by External mentors (Workshops column in Table 4). The questionnaire was completed by 58 clinical staff from 6 clinics. More than half (55.2%) rarely experienced support for new solutions. Nevertheless, close to half (41.4%) worked in teams to find solutions, and the spirit of teamwork and support in teams was also high (53.4%). The responses to the question about the need for a collaborative project development environment were evenly divided: 49% welcomed it, while 40% were indifferent. Only a small minority (11%) would be against such a workplace. Close to half (49%) would take the opportunity that may not pay off in the short term but give one a chance to excel. The same questionnaire asked the clinical staff which phase of the innovation process they found the most difficult (Engagement column in Table 4, Supplementary Material 2, Question 7). The following innovation stages were available to choose from: 1) Problem identification, 2) Brainstorming, 3) Screening and selection, 4) Creating a concept, 5) Creating a prototype, 6) Testing and refining the prototype, 7) Creating the final product, 8) Launching and marketing the product. The answers showed that as a project progresses from needs assessment through prototyping to launching a product, the difficulty of understanding how to do it increases, reaching 62.1%. The stage in the innovation process where projects most likely fail was prototyping, according to the respondents (25.9%) (Supplementary Material 2, Question 8). Only a small proportion of the respondents (19%) have already been involved in an innovation project. The three main reasons why they were not involved were 1) they did not encounter such an opportunity (29.3%), they worked at the clinic for a short time (25.9%), and 3) they did not have the right academic qualification (19%). Almost none of the respondents received a request from a startup for cooperation (3.4%), but most would be open to such collaboration if they get paid (43.1%) (Supplementary Material 2, Question 13). After analyzing the answers, tailored mentoring and workshops took place. The workshops provided Champions and participants with methodological knowledge and tools to find solutions to challenges and clinical needs (Skills column in Table 4). Participation in innovation projects to develop and implement solutions to the challenges was also measured as the outcome of the Clinical Innovation Program (Project column in Table 4). The change in innovation skills was measured by quantitative online motivation surveys and qualitative structured interviews (Table 5). The increased aptitude for innovation and change was also demonstrated by, for example, action plans. For example, the Otorhinolaryngology Clinic devised a problem-solution path consisting of 42 actions.
 |
Table 5 Performed Analyses Over the years in Each Clinic. X Indicates a Completed Analysis or Survey, While O Represents No Completed Analysis or Survey |
Increased Intellectual Product (IP) Disclosures
Despite the large number of university hospitals and the number of professionals covering all fields of medicine, the proportion of IP applications and developments based on real clinical needs was low. Before the launch of the Clinical Innovation Program (2015–2019), the percentage of life sciences/healthcare-related IP disclosures out of all disclosures was 39%. The percentage of IP submitted by a clinician or jointly with another non-clinician applicant was 21%. This number has changed from 2020, reaching the maximum of 50% of applications submitted by clinicians in 2022 (Table 6).
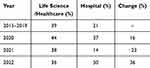 |
Table 6 Change in Intellectual Product Disclosures by Clinical Staff Over the years |
Concept Generation and Screening
Hackathons
Four events were held in Hungarian and English, requiring a physical or online presence, organized every semester by various units of the University, typically with the participation of student teams of 4–5 people. The identified clinical problems were delivered to the students via the university’s electronic (website) or social media interfaces and were implemented as part of courses as a condition for completion. Applications of ready-made teams or individual participants were expected. In the latter case, the organizers created the team by randomly mixing disciplines and nationalities. A priority goal for the organization was for as many university faculties and disciplines as possible to appear on each team. The performance of the teams was evaluated by a jury of experts in each case based on a predetermined set of criteria.
Innovation Course
The theoretical sessions of the course were complemented by practical work. In the competition, they worked on the challenges identified by the Discovery Team using the knowledge and methods acquired during the course.
Product Development
Through the Clinical Innovation Program, two clinical needs were identified jointly by the Innovation Staff, Leaders, and Champions, with high-priority and minimal budget needs. The first was the need for a device that could improve arthritic patients’ hand movement playfully.
Hardware Development
An external company created three distinct prototypes to improve the hand movement of arthritic patients. Structural drawings were also produced, showing the working principle and mechanics of the prototype. The Numberball was designed for preventative and rehabilitative purposes for those who suffer from rheumatic problems of the hand (Figure 2A). It is primarily intended as a playful tool for rehabilitating hand and finger movement limitations caused by muscle weakness or disease. The speed of manipulating the device can be measured, and conclusions about motor skills can be drawn, opening up further possibilities for use. The Octopus (Figure 2B) helps to strengthen the muscles of the hand and wrist playfully. It can be used to strengthen muscles after injuries or in arthritic patients. The main purpose of this device is to be used as a medical aid that allows the lateral and rotational movement of the fingers and the hands in a playful way. Gripping it with the ends of the fingers concentrates the load on the fingers while placing the whole palm can spread the load over the entire hand. Frog force (Figure 2C) is a hand movement-enhancing device that helps develop the circular movement of the fingers. The resistance of the device can be changed, and the device can be adapted to the rehabilitation needs of the individual. The special design allows users with different hand geometries to easily use it.
 |
Figure 2 The developed prototypes for improving hand mobility for rheumatic patients. Three devices are shown, each tested by patients for usability. (A) Numberball, (B) Octopus, (C) Frog Force. |
Software Development: Patient Pathway Management’s Digital Solution
As the survey showed, process management and IT classified problems remained consistently over the years as the two most serious issues for all participating clinics. Scheduling patients’ appointments and communicating with patients with the existing software was particularly difficult and slowed down patient care. Thus, the aim was to develop an application for patients and clinicians that makes digital patient records more manageable and transparent, with a focus on patient self-management. The product would be of particular benefit to clinicians in clinics where the patient is not undergoing a one-off or short-term treatment but is receiving care over a longer period, such as for certain rheumatological diseases, diabetes, or neurological conditions. The product could be interconnected with other mandatory hospital digital tools required by national legislation, enabling two-way, input-output information exchange and, thus, digital patient documentation at the same time. A seed fund covered the first phase of the project, during which we were able to create a minimal viable product with a reduced feature set. The development was guided by the suggestions of the participating clinics and their staff. Concrete steps that have been taken: 1) a user flow, ie a visual representation, was created to provide a digital path for users at different levels, 2) the information architecture included a visual representation of the product infrastructure, features, and hierarchy, 3) during the specification phase the technical documentation was prepared, detailing the exact technological conditions and the implementation process, 4) based on the specification, the overall design and the exact time and cost schedule for the development were also defined. Three main blocks were created with details: the Administration Block (Figure 3), the web-based Medical Block (Figure 4), and the Patient Block (Figure 5) that can be used on mobile devices.
Longitudinal Observations
First Year: Establishing Foundations
Initially, three clinics (Internal Medicine, Dentistry, and Otorhinolaryngology) actively participated, establishing a foundational year focused on leadership and innovation readiness. Leaders, Champions, and Innovative Staff were actively involved across all clinics, with three instances each, highlighting a phase focused on identifying and empowering key innovation drivers. The first year emphasized Quantitative Analysis and Online Motivation Surveys alongside the screening of IP Portfolios, marking the initial data-gathering phase to oversee where the developmental process may begin and what challenges are faced by both the Innovation Staff team and the clinics. Mandatory workshops for champions and continuous information sharing through champions were implemented to expand their knowledge and provide tools for improving the efficiency of the innovation process and start changing the organizational culture for innovation. No significant problems were documented in this phase, indicating a preliminary assessment period.
Second Year: Expanding Engagement and Deepening Insights
The project expanded to include additional clinics, maintaining consistent data from key participants. Leaders, Innovative Staff, and Staff were involved in clinics six instances each, with Champions slightly less prevalent. One may observe the marked participation of the Discovery Team, indicating a shift towards active exploration and external knowledge integration as preparation and building the foundation of our intervention. We pivoted towards extensive Qualitative Analysis and Structured Interviews, reflecting a deeper dive into the clinics’ operational contexts. As proposed solutions, we introduced hackathons, lectures, and university innovation projects, indicating an expansion of strategies to foster innovation. We also identified more problems, especially in Process Management, Other, and Infrastructure, indicating escalating concerns over problems and the need for innovation.
Third Year: Refining Strategies and Fostering Innovation
The project maintained its momentum with continuous participation from initial clinics. Leaders, the Champion Network, Innovation Staff, and the Discovery Team remained active in the third year, but due to lack of funds and administrative issues, External mentors, hackathon events, and the Innovation Course were absent. We also balanced our methodological approach evenly, with both qualitative and quantitative methodologies. Our focus shifted towards motivation surveys and maintaining the university innovation project, emphasizing sustained engagement and motivational assessment. The discovered problems reflected similar IT and operational challenges.
Discussion
The Need for Change
Most previous studies have suggested links between hospital organizational culture and hospital performance metrics,19–22 though there are some exceptions.23,24 A novel program in the USA (Leadership Saves Lives), using a longitudinal mixed methods approach, showed that hospital organizational culture change has a prominent effect on the quality of patient care and can actually save lives.25 Our mission in this study was not directed to saving lives immediately but to influencing organizational culture in hospitals to improve innovation frequency and quality. Although the participating students in the Innovation Course, mainly medics, were not part of the current clinical staff, their involvement in innovation projects can lead to organizational cultural change, improve outcomes for patients, and save lives in the long run.
Hackathon: A Tool to Educate Students and to Promote Innovation
Hackathons are a cutting-edge approach to innovation and teaching that encourages collaboration, imagination, and problem-solving. The existing (relevant) problem and the intention to solve it together result in the person who appears to be instead of “the person living with the problem” the “person who wants to solve the problem”. The first step in the change of attitude is a consciously observant person with appropriate observation techniques and a critical way of thinking, who not only perceives the problems surrounding him/her but also becomes aware of the points where he/she can intervene.26 We used this tool for three reasons in our program. First, to provide methods for the next generation of doctors that they can use to solve real-life problems. The second is to change the mindset of the young generation to be open to innovation. Third, to encourage students, especially medical students, to harness the value of different disciplines and work in a multidisciplinary team.27,28
Clinical Innovation Program
We started our Clinical Innovation Program in 2020, building on two complementary initiatives: the Champion Network and the Discovery Team. The university has 29 clinics covering the whole spectrum of healthcare, yet few innovative projects, developments, or patents have come to light due to the everyday, standard issues faced by healthcare workers, especially doctors and researchers. Our multidisciplinary approach showed several vital accomplishments and identified future research directions. First, we uncovered the current attitude toward healthcare innovation in hospital clinics and identified the reason for the lack of motivation. Work overload, lack of opportunity, and knowledge gaps in innovation were the most common and, fortunately, could be addressed with relative ease. Second, using the mutual effort of the Campion Network and the Discovery Team, we identified sets of common problems that can be addressed with minimal financial help. Most issues were process management-related across the investigated clinics. One proposed solution was a patient pathway management application that was already being developed already. The Champion Network has successfully built a culture of innovation by incorporating doctors as Champions, thus increasing the awareness and motivation of the clinical workforce to solve problems with the potential of developing commercially viable products and services. The multidisciplinary approach of the Discovery Team was successful in identifying and responding to clinic-specific challenges, showing that external perspectives can be valuable. Our study grew over three years in scope, with success demonstrated by the engagement and operational involvement seen in participating clinics.
Dynamic data collection and analysis guaranteed the relevance and efficacy of our interventions. All these were practical solutions developed during hackathons and innovation courses, such as the digital application for managing patient records and rehabilitative devices, which finally met the identified problems and offered the students experiential innovation practice. The identification of IT problems consistently reflects the way advanced technologies should be integrated into healthcare. The structured multidisciplinary approach through the Champion Network and Discovery Team enhanced clinic efficiency, indicated by the solution-seeking attitude and the increased number of participations in IP submissions. It contributed to the culture of innovations, thus demonstrating the potential for broader application for improvements in healthcare services.
Hospitals were overwhelmed by the workload during the COVID-19 pandemic, and medical professionals were restricted from meeting our research team. After the pandemic, however, clinicians were enthusiastic to continue the project, indicating the motivation of medical staff to improve innovation efficiency.
Limitations of the Study
Although our Clinical Innovation Program is a multidisciplinary holistic approach, it lacks a robust number of observations to draw a general conclusion. Expanding the framework to additional clinics and hospitals, preferably at the international level, would fine-tune the process to improve the innovation culture in the healthcare sector. Questionnaires before, during, and after the program would also prove or disprove its value. It also needs to be noted that the project was carried out during the COVID-19 pandemic, creating difficult circumstances for hospitals.
Conclusions
Although innovation is not typically the primary focus of healthcare team research, there is increasing recognition of the significance of innovation generated within healthcare organizations.29 It is recognized that such innovations enhance performance, and research focused on improving areas such as patient safety acknowledges that these outcomes depend on innovation.30,31 Our research shows that a holistic approach involving healthcare professionals and non-medical experts from various levels in their careers, ranging from undergraduate students to senior leaders, changes innovation culture and generates solutions for existing real-life problems. The success of the proposed framework to improve innovation efficiency depends on the willingness and motivation of the healthcare professionals, especially of the leadership. Therefore, great attention must be paid to the initial phase of the project when the objectives and potential benefits are outlined to the leaders. Identifying opinion leaders using the Organizational Network Analysis method and finding their motivation would further increase the chance to change the organizational innovation culture. This approach also helps expand the use of the framework in other healthcare units. Moreover, the comprehensive framework we detailed in this study contains general methods and tools that are not specific to countries and, hence, can be adopted in any country irrespective of the geographic location. We believe that the key to improving innovation efficiency in healthcare depends mainly on the organizational culture that, with a comprehensive approach, can be changed and improved globally.
Acknowledgment
This work was supported by the European Institute of Innovation and Technology (EIT Health), the Cooperative Doctorate Scholarship of the Ministry of Innovation and Technology financed by the National Research Development and Innovation Fund for AS, and the Tandem fund of the Medical School, University of Pecs for AC and AS.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Keane MP, McCormick B, Popławska G. Health care spending in the US vs UK: the roles of medical education costs, malpractice risk and defensive medicine. European Econ Rev. 2020;124:103401.
2. Eurostat. Healthcare expenditure statistics. 2022. Available from: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Healthcare_expenditure_statistics.
3. Gulácsi L, Rotar AM, Niewada M, et al. Health technology assessment in Poland, the Czech Republic, Hungary, Romania and Bulgaria. Eur J Health Econ. 2014;15(Suppl 1):S13–S25. doi:10.1007/s10198-014-0590-8
4. Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307(14):1513–1516. doi:10.1001/jama.2012.362
5. Robinson JC, Smith MD. Cost-reducing innovation in health care. Health Affairs. 2008;27(5):1353–1356. doi:10.1377/hlthaff.27.5.1353
6. Sydow J, Schreyögg G, Koch J. Organizational path dependence: opening the black box. Acad Manag Rev. 2009;34(4):689–709.
7. Berghöfer A, Göckler DG, Sydow J, et al. The German health care innovation Fund – an incentive for innovations to promote the integration of health care. J Health Organiz Manage. 2020;34(8):915–923. doi:10.1108/JHOM-05-2020-0180
8. Shieber J. techcrunch.com. A healthcare investment fund has become one of Israel’s largest with a $660 million close; 2019. Available from: https://techcrunch.com/2019/03/06/a-healthcare-investment-fund-has-become-one-of-israels-largest-with-a-660-million-close/.
9. Alpert JL, Lin ZL, Ahmed W, et al. Annual primary care 2030 convening: creating an enabling ecosystem for person-centered primary healthcare models to achieve universal health coverage in low-and middle-income countries. Ann Global Health. 2020;86(1):1–6. doi:10.5334/aogh.2526
10. Angelidis P, Berman L, Casas-Perez MDLL, et al. The hackathon model to spur innovation around global mHealth. J Med Eng Technol. 2016;40(7–8):392–399. doi:10.1080/03091902.2016.1213903
11. Nari Kahle H, Dubiel A, Ernst H, et al. The democratizing effects of frugal innovation. J Indian Business Res. 2013;5(4):220–234. doi:10.1108/JIBR-01-2013-0008
12. Soni P, Krishnan RT. Frugal innovation: aligning theory, practice, and public policy. J Indian Business Res. 2014;6(1):29–47.
13. Bianchi C, Bianco M, Ardanche M, Schenck M. Healthcare frugal innovation: a solving problem rationale under scarcity conditions. Technol Soc. 2017;51:74–80.
14. Mitchell R, Boyle B. Understanding the role of profession in multidisciplinary team innovation: professional identity, minority dissent and team innovation. British J Manage. 2021;32(2):512–528. doi:10.1111/1467-8551.12419
15. Bezemer GFG, Garssen J. TLR9 and COVID-19: a multidisciplinary theory of a multifaceted therapeutic target. Front Pharmacol. 2021;11:601685. doi:10.3389/fphar.2020.601685
16. Paton R, McNamara LA. Multidisciplinary Approaches to Theory in Medicine. Amsterdam, Boston: Elsevier; 2006.
17. Sun K, Goodfellow H, Konstantara E, et al. The multidisciplinary, theory-based co-design of a new digital health intervention supporting the care of oesophageal cancer patients. Digit Health. 2021;7:20552076211038410. doi:10.1177/20552076211038410
18. Green L, Grant V. Gagged grief and beleaguered bereavements?’ an analysis of multidisciplinary theory and research relating to same sex partnership bereavement. Sexualities. 2008;11(3):275–300. doi:10.1177/1363460708089421
19. Shwartz M, Cramer IE, Holmes SK, et al. Survey-assessed quality and organizational factors related to quality in pursuing perfection hospitals. Qual Manag Health Care. 2010;19(4):349–363. doi:10.1097/QMH.0b013e3181f9ef02
20. Gittell JH, Fairfield KM, Bierbaum B, et al. Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay: a nine-hospital study of surgical patients. Med Care. 2000;38(8):807–819. doi:10.1097/00005650-200008000-00005
21. VanDeusen Lukas C, Holmes SK, Cohen AB, et al. Transformational change in health care systems: an organizational model. Health Care Manage Rev. 2007;32(4):309–320. doi:10.1097/01.HMR.0000296785.29718.5d
22. Meterko M, David CM, Young GJ. Teamwork culture and patient satisfaction in hospitals. Med Care. 2004;42(5):492–498. doi:10.1097/01.mlr.0000124389.58422.b2
23. Davenport DLP, Henderson WG, Mosca CL, et al. Risk-adjusted morbidity in teaching hospitals correlates with reported levels of communication and collaboration on surgical teams but not with scale measures of teamwork climate, safety climate, or working conditions. J Am Coll Surg. 2007;205(6):778–784. doi:10.1016/j.jamcollsurg.2007.07.039
24. Shortell SM, Jones RH, Rademaker AW, et al. Assessing the impact of total quality management and organizational culture on multiple outcomes of care for coronary artery bypass graft surgery patients. Med Care. 2000;38(2):207–217. doi:10.1097/00005650-200002000-00010
25. Curry LA, Linnander EL, Brewster AL, et al. Organizational culture change in U.S. hospitals: a mixed methods longitudinal intervention study. Implement Sci. 2015;10(1):29. doi:10.1186/s13012-015-0218-0
26. Schulten C, Chounta I-A. How do we learn in and from Hackathons? A systematic literature review. Educat Inform Technol. 2024;29(15):20103–20134. doi:10.1007/s10639-024-12668-1
27. Falk J, Nolte A, Huppenkothen D, et al., The future of hackathon research and practice. arxiv.org, 2022.
28. Falk J, Kannabiran G, Hansen NB. What do hackathons do? Understanding participation in hackathons through program theory analysis. 2021. New York, NY, USA: ACM.
29. Mitchell R, Boyle B. Professional diversity, identity salience and team innovation: the moderating role of openmindedness norms. J Organiz Behav. 2015;36(6):873–894. doi:10.1002/job.2009
30. Dias C EA. Improvement of hospital performance through innovation: toward the value of hospital care. Health Care Manager. 2013;32(2):129–140.
31. Tartari E, Pires D, Bellissimo-Rodrigues F, et al. The global hand-sanitizing relay: promoting hand hygiene through innovation. J Hosp Infect. 2017;95(2):189–193. doi:10.1016/j.jhin.2016.11.003
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.








