Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 17
A New Heterozygous Variant of c.1225_1227delTTC (p.Phe409del) in Insulin Receptor Gene Associated with Severe Insulin Resistance and Hyperandrogenemia in an Adolescent Female with Type A Severe Insulin Resistance Syndrome
Authors Song Y, Lei W, Huang Q, Zhang J, Zhang Q, Chen L, Li H, Liu L, Zeng T , Hu X
Received 30 July 2024
Accepted for publication 23 October 2024
Published 25 November 2024 Volume 2024:17 Pages 4389—4396
DOI https://doi.org/10.2147/DMSO.S481745
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Juei-Tang Cheng
Yuqing Song,1,2,* Wenjie Lei,1– 3,* Qianqian Huang,1,2 Jiehan Zhang,1,2 Qiao Zhang,4 Lulu Chen,1,2 Huiqing Li,1,2 Li Liu,5 Tianshu Zeng,1,2 Xiang Hu1,2
1Department of Endocrinology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430022, People’s Republic of China; 2Hubei Provincial Clinical Research Center for Diabetes and Metabolic Disorders, Wuhan, 430022, People’s Republic of China; 3People’s Hospital of Luotian County, Huanggang, 438600, People’s Republic of China; 4Department of Cardiovascular Surgery, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430022, People’s Republic of China; 5The People’s Hospital of Maojian, Shiyan, 442000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Tianshu Zeng; Xiang Hu, Email [email protected]; [email protected]
Background: Functional defects caused by mutations in the insulin receptor (INSR) gene often lead to severe hereditary insulin resistance syndromes, including but not limited to type A insulin resistance syndrome.
Method and Result: Here, we report a case of a 12-year-old girl with elevated fasting blood glucose detected by opportunistic testing, associated with severe insulin resistance and hyperandrogenemia. She had axillary hair, acne, clitoral hypertrophy, prominent labia minora hypertrophy and thickened voice with BMI 20.57kg/m2, and ultrasound imaging showed that she had multiple follicles in both ovaries. Insulin was initially administered, but the glycemic control was poor. Accordingly, the prescription was later switched to metformin, maintaining euglycemic blood glucose level. The whole exome sequencing from peripheral blood revealed that the patient carries NM_000208.2:c.1225_1227delTTC (p.Phe409del) heterozygous mutation in the INSR gene. She was tentatively diagnosed as type A insulin resistance syndrome based on her clinical features and heterozygous mutation in the INSR gene.
Conclusion: Our results demonstrated that type A insulin resistance syndrome in patients presenting with severe insulin resistance and hyperandrogenemia was associated with a heterozygous variant of c.1225_1227delTTC (p.Phe409del), suggesting that exon sequencing would be beneficial to detect the potential mutations in the INSR gene of these patients for precise diagnosis and intervention in clinical practice.
Keywords: insulin receptor gene, heterozygous mutation, severe insulin resistance, hyperandrogenemia, type A insulin resistance syndrome, female
Introduction
Insulin resistance is widely defined as a state of reduced responsiveness of insulin-sensitive tissues to physiological levels of insulin. It is usually associated with hyperinsulinemia and plays a critical role in the development of a cluster of insulin resistance-related diseases such as type 2 diabetes mellitus (T2DM) and metabolic syndrome (MS).1,2 Insulin resistance is characterized by defective insulin signaling in insulin-responsive tissues, and its mechanism is closely related to the structure and function of insulin receptor and/or insulin receptor gene (INSR), although ectopic lipid deposition, abnormalities in secretion or action of endocrine mediators such as leptin, mitochondrial dysfunction and oxidative stress, dysregulation of intestinal microbiota and chronic inflammation are also considered to be important causative factors of insulin resistance.3,4 Hyperandrogenemia (HA) in female refers to a condition of androgen excess, with variable clinical manifestations, including accelerated growth, advancement of bone age, hirsutism, acne, enlarged clitoris in pre-pubertal stage,5 and abnormal menstruation periods, infertility and androgenic alopecia in adults. Hyperandrogenemia occurs in many disorders, including but not restricted to polycystic ovarian syndrome, which is closely related to insulin resistance in female.6 Here, we report a case of a girl with severe insulin resistance and hyperandrogenemia, with NM_000208.2:c.1225_1227delTTC (p.Phe409del) heterozygous mutation in the INSR gene, who was tentatively diagnosed as type A insulin resistance syndrome based on her clinical features and INSR gene mutation.
Materials and Methods
Laboratory Examination
Blood glucose and lipid profile, sex hormones, ACTH, cortisol, thyroid hormones, growth hormone, serum electrolytes, and diabetes-related antibodies were determined, and liver and kidney function tests were performed using commercial reagent kits.
Oral Glucose Tolerance Test (OGTT)
OGTT was performed with the administration of a 75g glucose oral solution after overnight fasting. Blood samples were collected before and at 30, 60, 120 and 180 minutes after glucose administration for the determination of plasma glucose, insulin and C-peptide.
Doppler Echocardiography and Bone Stage Assessment
Doppler echocardiography was employed to evaluate the liver, gallbladder, pancreas, heart, uterus and adnexa, while Tanner Whitehouse (TW3) Methods were used to assess the bone age of the patient.
Gene Sequencing
In view of that, the patient may harbor gene mutations contributing to insulin resistance, including but not restricted to the most common causes of INSR and PIK3R1 gene variants. Whole-exome sequencing of DNA from peripheral blood was performed on the patient and her parents, which includes all coding exons of nuclear genes together with mitochondrial genome in the human genome as described previously and is cost-effective in clinical practice in China. In brief, the genomic DNA was fragmented, and exome capture was performed using the Roche KAPA HyperExome chip, and the sequencing was performed using the MGISEO-2000 platform.7 Additionally, we conducted validation of the identified INSR mutation in both the patient and the parents to confirm its presence and inheritance pattern.
Results
Case Presentation
The girl was 12 years old, with weight 52kg, height 159cm, waist circumference 70 cm and hip circumference 74 cm. She was characterized by voice deepening, absence of menarche, increases in pubic and axillary hair, clitoral enlargement and prominent labia minora, and her pubertal development was rated Tanner stage 3. Neither the patient nor her parents showed obvious acanthosis nigricans. Her father and mother, who both suffered diabetes mellitus with insulin resistance, had the height of 170 cm and 156 cm and weight of 75 kg and 52 kg, respectively. Her parents were non-consanguineously married. However, her paternal grandfather and maternal grandmother had diabetes mellitus, with no reported family history of other metabolic disorders.
It was detected by opportunistic testing in the regular examination at school that her fasting plasma glucose (FPG) was as high as 12.1mmol/L. Further testing indicated that glycated hemoglobin (HbA1c) was 9.5% and postprandial blood glucose was 23.5mmol/L, associated with increases in fasting insulin of 158.17µIU/mL, 2-hour postprandial insulin of 178.39 µIU/m L, and testosterone of 4.13 ng/mL (reference range 0.087–0.82 in Tanner stage 3), and she was diagnosed with diabetes mellitus (type unspecified).
Initially, insulin was prescribed to the patient. However, she was not able to achieve a good blood glucose control, with fasting glucose ranging from 6 to 9mmol/l and postprandial glucose ranging from 8 to 15mmol/l. Three months later, metformin 1500 mg daily was administered to the patient and the insulin administration was discontinued after our consultation. Remarkably, she had much better glycemic control, with fasting blood glucose (4.8–6.1 mmol/L), postprandial blood glucose (4.8–7.9 mmol/L) and HbA1c (5.8%).
Laboratory Examination
The testosterone level is 4.13ng/mL, suggesting severe hyperandrogenemia in this girl. No obvious abnormality was observed in ACTH, cortisol circadian rhythm, thyroid hormone (Table 1), liver and kidney function, lipid profile and diabetes-related autoantibodies (Table 2).
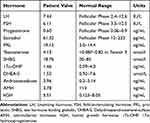 |
Table 1 Hormone Analysis |
 |
Table 2 Diabetes-Related Autoantibodies |
OGTT
Remarkable increases in plasma glucose and insulin level were observed in the patient, suggesting severe insulin resistance (Table 3).
 |
Table 3 Results of OGTT |
Doppler Ultrasound Evaluation and Bone Stage Assessment
Ultrasound of the uterus and both adnexa showed bilaterally enlarged ovaries with tens of small ovarian follicles and the endometrial thickness was 3mm. No significant abnormalities were observed in important organs such as the liver, kidneys, and heart on ultrasonography. Her bone age is 14 years 4 months, and 11 years 2 months according to TW3-RUS and TW3-Carpal, respectively.
Genetic Sequencing
The whole-exome sequencing testing results indicated that a heterozygous variant of NM_000208.2 (INSR):c.1225_1227delTTC (p.Phe409del) was detected in the patient and her father, but not in her mother (Figure 1). Actually, her father had diabetes for a couple of years with significant insulin resistance and the blood glucose control seemed good using metformin. Her mother also had mild type 2 diabetes using lifestyle interventions. Based on the American College of Medical Genetics and Genomics (ACMG) standards and guidelines, it was interpreted as a variant of uncertain significance (VUS).
Discussion
We reported a 12-year-old female patient with severe insulin resistance, hyperandrogenemia and polycystic ovaries caused by a heterozygous mutation NM_000208.2:c.1225_1227delTTC (p.Phe409del) in the INSR gene, which has not been reported previously to our best knowledge. It is reported that the INSR localized at 19p13.2–13.3 (OMIM147670), with a total length of more than 170 kb, containing 22 exons and 21 introns, in which the exons 1–11 encode the α-subunit, and the exons 12–22 encode the β subunit. The human INSR is a heterotetramer consisting of two α (insulin binding) and two β (tyrosine kinase) subunits that are linked via disulfide bonds.8 INSR signals in response to insulin, enhances cellular glucose transport, increases glycogen synthase enzymatic activity, and subsequently regulates metabolic processes such as protein or lipid synthesis, as well as growth. Defects in insulin receptor structures and function, including α-subunit and β subunit, can lead to complicated disorders, including but not limited to insulin resistance syndromes.9,10
Insulin resistance syndromes are usually categorized into type A, caused by abnormalities in the INSR gene, and type B, caused by autoantibodies to the INSR.11,12 Type A insulin resistance syndrome (TAIRS) is an autosomal recessive or dominant genetic disease, due to mutations in the INSR gene affecting the binding of insulin to the INSR and consequently causing insulin signaling impairment and insulin resistance, which is more common in adolescent females.13 TAIRS is characterized by severe insulin resistance, hyperandrogenemia and acanthosis nigricans, which are often associated with polycystic ovary syndrome.14 It is reported by Sanderson, E. E that an 11-year-old girl with severe insulin resistance and hyperglycemia, who was diagnosed with Type A Insulin Resistance Syndrome (TAIRS) and showed a significant response to metformin treatment, was associated with a heterozygous missense variant His1157Arg in exon 19 of the INSR gene.15 Donohue syndrome (leprechaunism) and Rabson-Mendenhall syndrome are two rare autosomal recessive disorders caused by mutations in the INSR gene. Donohue syndrome is the most severe form of inherited insulin resistance syndromes, which is characterized by intrauterine growth retardation, dysmorphic features, acanthosis nigricans, hirsutism and severe insulin resistance with early demise within the first year of age. Rabson-Mendenhall syndrome is somewhat less severe, with progressive hyperglycemia and eventual development of refractory ketoacidosis, together with somatic anomalies and survival up to the third decade.16 Actually, Donohue syndrome and Rabson-Mendenhall syndrome are increasingly considered severe forms of type A insulin resistance syndrome.17 In general, patients with typical type A insulin resistance syndrome have INSR heterozygote abnormalities, whereas patients with Donohue syndrome or Rashon-Mendenhall syndrome often have homozygous or compound and/or severe heterozygote abnormalities.18 This patient we reported was presented with severe hyperinsulinemia, accompanied by a mutation in the INSR gene, hyperandrogenemia and polycystic ovaries. The whole exome testing results of the patient showed a heterozygous mutation of c.1225_1227delTTC (p.Phe409del) in exon 19 of the INSR gene, which is considered to cause a deletion of phenylalanine (Phe) at position 409 in the amino acid sequence of the INSR (β subunit). Thus, we tentatively diagnosed this girl as type A insulin resistance syndrome according to the article published by Japanese scholar Wataru Ogawa in 202219 and postulated that the INSR mutation in this patient might decrease subunit tyrosine kinase activity and/or insulin-receptor binding capacity, leading to impairment of insulin signaling and insulin resistance-related disorders.20 Insulin resistance and hyperandrogenemia are common features of type A insulin resistance syndrome (TAIRS).21 More and more studies indicate that while many peripheral tissues develop insulin resistance, the theca cells in the ovaries remain sensitive to insulin. Therefore, stimulation of the insulin receptors by hyperinsulinemia results in an excess of androgen in female. In addition, insulin stimulates the secretion of Gonadotropin-releasing hormone (GnRH) in the hypothalamus, resulting in pulsatile LH release and excessive secretion of testosterone in women. Moreover, androgen excess can facilitate insulin resistance, hyperinsulinemia and diabetes.22 These may be important explanations for the development of hyperandrogenemia associated with insulin resistance in the patient we reported as well as in TAIRS.
Currently, lifestyle modifications, oral and injectable antihyperglycemic medications, and insulin, along with therapies targeted to reverse or attenuate insulin resistance in patients of severe insulin resistance, constitute our modern treatment armamentarium.17 In the patient we reported, insulin injection was administered initially as key elements of the therapeutic approach. However, the glycemic control was poor by insulin injection in combination with diet and exercise. Additionally, it is reported that IGF-1 can mediate their effects through similar tyrosine kinase receptors as a possible therapeutic agent against insulin resistance. Furthermore, recombinant human IGF-1 (rhIGF-1) can improve metabolic control in INSR-related severe insulin resistance syndromes and increase life span in patients with Donohue syndrome.23 Moreover, metformin and thiazolidinediones play a crucial role in severe insulin resistance, improving glucose homeostasis, in part by enhancing insulin sensitivity. In view of the fact that metformin is considered the first-line medication for improving insulin sensitivity in patients,17 recombinant human IGF-1 is inaccessible for this patient and thiazolidinediones is not recommended in individuals younger than 18 years old, metformin is prescribed for this patient and the blood glucose control became better and better with the insulin injection discontinued accordingly, suggesting that metformin administration based on diet and exercise could be sufficient in glycemic control in some patient of severe insulin resistance with INSR gene mutations.
It is reported that the prognosis is closely related to the location or number of mutations in the INSR gene, and genetic testing is crucial in these patients.24 Moreover, the patient we reported carrying a heterozygous variant of c.1225_1227delTTC (p.Phe409del) in exon 19 of the INSR gene was characterized by severe insulin resistance and hyperandrogenemia, which is similar to polycystic ovary syndrome and significantly different from Donohue syndrome and Rabson-Mendenhall syndrome. These findings suggest that genetic testing should not only be recommend in those with suspected Donohue syndrome and Rabson-Mendenhall syndrome but also be worth considering in female with severe insulin resistance and hyperandrogenemia, especially in young girls, which would be of great help for early detection, precise diagnosis and treatment, as well as prenatal genetic counseling in these patients.
Noteworthy, the heterozygous variant of NM_000208.2 (INSR):c.1225_1227delTTC (p.Phe409del) was detected in the patient’s father, who had diabetes for a couple of years with significant insulin resistance with blood good glycemic control using metformin, and looked like a patient with typical type 2 diabetes. It is reported by Zhu, A. N. that INSR plays a role in the susceptibility to type 2 diabetes in the Han Chinese population,25 which seems consistent with our findings in this patient. Therefore, we tentatively put forward that INSR variants might occur in male patients with seemingly typical type 2 diabetes and genetic testing could be meaningful in them for early detection, precise diagnosis and treatment, as well as prenatal genetic counseling in these patients.
It should be noted that we were not able to confirm the causative relationship between the detected heterozygous variant of c.1225_1227delTTC (p.Phe409del) in exon 19 of the INSR gene and her severe insulin resistance and hyperandrogenemia in the reported patient by performing cellular and/or animal experiments, although the mutation is considered to cause a deletion of phenylalanine (Phe) at position 409 in the amino acid sequence of the INSR (β subunit) and probably induce insulin signaling impairment, severe insulin resistance and hyperandrogenemia in this girl. Thus, further confirmative research is necessary in the future.
Conclusions
Notwithstanding these limitations, we tentatively diagnosed this girl as type A insulin resistance syndrome and postulate that the heterozygous variant of c.1225_1227delTTC (p.Phe409del) in exon 19 of the INSR gene might play a causative role in severe insulin resistance and hyperandrogenemia in female.
Institutional Review Board Statement
The study complies with the Declaration of Helsinki and was approved by the ethics committee of Huazhong University of Science and Technology in Wuhan, China. The institution has granted approval for the public publication of the article, and the ethical committee approval number is UHCT-IEC-SOP-016-03-01.
Informed Consent Statement
Informed consent was obtained from the patient’s guardian involved in the study, and the informed consent form was signed by the guardian. The patient’s guardian had given permission for the publication of case details and information about the accompanying images.
Acknowledgments
We are extremely grateful to the patient and their families who have been involved in this study.
Author Contributions
Yuqing Song and Wenjie Lei contributed equally to this work and share first authorship. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by grants from the National Natural Science Foundation of China (82173517, 81800762, 82170822, 82000366 and 81974111). We would like to include a funding statement in the manuscript.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Kahn SE. The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of type 2 diabetes. Diabetologia. 2003;46(1):3–19. doi:10.1007/s00125-002-1009-0
2. Semple RK, Savage DB, Cochran EK, Gorden P, O’Rahilly S. Genetic syndromes of severe insulin resistance. Endocr Rev. 2011;32(4):498–514. doi:10.1210/er.2010-0020
3. Lee SH, Park SY, Choi CS. Insulin resistance: from mechanisms to therapeutic strategies. Diabetes Metab J. 2022;46(1):15–37. doi:10.4093/dmj.2021.0280
4. He FF, Li YM. Role of gut microbiota in the development of insulin resistance and the mechanism underlying polycystic ovary syndrome: a review. J Ovarian Res. 2020;13(1):73. doi:10.1186/s13048-020-00670-3
5. Esquivel-Zuniga MR, Kirschner CK, McCartney CR, et al. Non-PCOS hyperandrogenic disorders in adolescents. Semin Reprod Med. 2022;40(1–2):42–52. doi:10.1055/s-0041-1742259
6. Wang J, Wu D, Guo H, et al. Hyperandrogenemia and insulin resistance: the chief culprit of polycystic ovary syndrome. Life Sci. 2019;236:116940. doi:10.1016/j.lfs.2019.116940
7. Wan Y, Hong Z, Ma B, He X, Ma L, Wang M, Zhang Y. Identification of compound heterozygous variants in MSH4 as a novel genetic cause of diminished ovarian reserve. Reprod Biol Endocrinol. 2023;21(1):76. doi:10.1186/s12958-023-01127-0
8. Ebina Y, Ellis L, Jarnagin K, et al. The human insulin receptor cDNA: the structural basis for hormone-activated transmembrane signalling. Cell. 1985;40(4):747–758. doi:10.1016/0092-8674(85)90334-4
9. Ullrich A, Bell JR, Chen EY, et al. Human insulin receptor and its relationship to the tyrosine kinase family of oncogenes. Nature. 1985;313(6005):756–761. doi:10.1038/313756a0
10. Choura M, Rebaï A. Receptor tyrosine kinases: from biology to pathology. J Recept Signal Transduct Res. 2011;31(6):387–394. doi:10.3109/10799893.2011.625425
11. Musso C, Cochran E, Moran SA, et al. Clinical course of genetic diseases of the insulin receptor (type A and Rabson-Mendenhall syndromes): a 30-year prospective. Medicine. 2004;83(4):209–222. doi:10.1097/01.md.0000133625.73570.54
12. Arioglu E, Andewelt A, Diabo C, et al. Clinical course of the syndrome of autoantibodies to the insulin receptor (type B insulin resistance): a 28-year perspective. Medicine. 2002;81(2):87–100. doi:10.1097/00005792-200203000-00001
13. Koca SB, Kulali MA, Güğüş B, et al. Type A insulin resistance syndrome due to a novel heterozygous c.3486_3503del (p.Arg1163_Ala1168del) INSR gene mutation in an adolescent girl and her mother. Arch Endocrinol Metab. 2024;68:e210305. doi:10.20945/2359-4292-2021-0305
14. Takasawa K, Tsuji‐Hosokawa A, Takishima S, et al. Clinical characteristics of adolescent cases with type A insulin resistance syndrome caused by heterozygous mutations in the β-subunit of the insulin receptor (INSR) gene. J Diabetes. 2019;11(1):46–54. doi:10.1111/1753-0407.12797
15. Sanderson EE, Shah M, Hooper AJ, Bell DA, Choong CS. Monogenic diabetes due to an INSR mutation in a child with severe insulin resistance. Endocrinol Diabetes Metab Case Rep. 2022;2022.
16. Ben Abdelaziz R, Ben Chehida A, Azzouz H, et al. A novel homozygous missense mutation in the insulin receptor gene results in an atypical presentation of Rabson-Mendenhall syndrome. Eur J Med Genet. 2016;59(1):16–19. doi:10.1016/j.ejmg.2015.11.015
17. Angelidi AM, Filippaios A, Mantzoros CS. Severe insulin resistance syndromes. J Clin Invest. 2021;131(4). doi:10.1172/JCI142245
18. Longo N, Wang Y, Smith SA, Langley SD, DiMeglio LA, Giannella-Neto D. Genotype-phenotype correlation in inherited severe insulin resistance. Hum Mol Genet. 2002;11(12):1465–1475. doi:10.1093/hmg/11.12.1465
19. Ogawa W, Araki E, Ishigaki Y, et al. New classification and diagnostic criteria for insulin resistance syndrome. Endocr J. 2022;69(2):107–113. doi:10.1507/endocrj.EJ21-0725
20. Maassen JA, Tobias ES, Kayserilli H, et al. Identification and functional assessment of novel and known insulin receptor mutations in five patients with syndromes of severe insulin resistance. J Clin Endocrinol Metab. 2003;88(9):4251–4257. doi:10.1210/jc.2003-030034
21. Mukherjee S, Maitra A. Molecular & genetic factors contributing to insulin resistance in polycystic ovary syndrome. Indian J Med Res. 2010;131:743–760.
22. Vuguin PM. Interventional studies for polycystic ovarian syndrome in children and adolescents. Ped Health. 2010;4(1):59–73. doi:10.2217/phe.09.69
23. McDonald A, Williams RM, Regan FM, Semple RK, Dunger DB. IGF-I treatment of insulin resistance. Eur J Endocrinol. 2007;157(Suppl 1):S51–6. doi:10.1530/EJE-07-0271
24. Taylor SI, Arioglu E. Syndromes associated with insulin resistance and acanthosis nigricans. J Basic Clin Physiol Pharmacol. 1998;9(2–4):419–439. doi:10.1515/JBCPP.1998.9.2-4.419
25. Zhu AN, Yang XX, Sun MY, et al. Associations between INSR and MTOR polymorphisms in type 2 diabetes mellitus and diabetic nephropathy in a Northeast Chinese Han population. Genet Mol Res. 2015;14(1):1808–1818. doi:10.4238/2015.March.13.9
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


