Back to Journals » Cancer Management and Research » Volume 17
A Nomogram Based on Fibrinogen-to-Neutrophil Ratio as a Novel Predictor of Lymph Node Metastasis in Patients with Cervical Cancer and Type 2 Diabetes Mellitus
Authors Kuang H, Yang D, Lin R , Tang Y, Luo Y , Wang S, Xia T, Lou G, Chen H
Received 24 December 2024
Accepted for publication 12 April 2025
Published 10 May 2025 Volume 2025:17 Pages 933—954
DOI https://doi.org/10.2147/CMAR.S510815
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Harikrishna Nakshatri
Hongying Kuang,1,* Dongxia Yang,2,* Ruoyao Lin,3 Yaling Tang,4 Yongli Luo,3 Shuwen Wang,5 Tingting Xia,5 Ge Lou,6 Hong Chen4
1Department of Gynecology, The First Affiliated Hospital of Heilongjiang University of Chinese Medicine, Harbin, Heilongjiang, 150040, People’s Republic of China; 2Department of Gynecology, The Second Affiliated Hospital of Heilongjiang University of Chinese Medicine, Harbin, Heilongjiang, 150001, People’s Republic of China; 3Department of Clinical Medicine, School of Medicine, Xiamen University, Xiamen, Fujian, 361005, People’s Republic of China; 4Department of Obstetrics and Gynecology, The First Affiliated Hospital of Xiamen University, Xiamen, Fujian, 361003, People’s Republic of China; 5Department of Obstetrics and Gynecology, The First Affiliated Hospital of Xiamen University, School of Medicine, Xiamen, Fujian, 361003, People’s Republic of China; 6Department of Gynecology, Harbin Medical University Cancer Hospital, Harbin, Heilongjiang, 150081, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hong Chen, Department of Obstetrics and Gynecology, The First Affiliated Hospital of Xiamen University, No. 150 Shanggu Street, Siming District, Xiamen, Fujian, 361003, People’s Republic of China, Tel +86 0592213 7307, Email [email protected]
Background: The rising incidence of cervical cancer among individuals with diabetes is a matter of significant concern, presenting profound implications for the health status and quality of life worldwide. In patients diagnosed with early-stage cervical cancer, the extent of lymph node involvement has emerged as a critical prognostic factor influencing recurrence risk and survival outcomes. Therefore, the precise prediction of pelvic lymph node metastasis is essential for an accurate assessment of prognosis. The preoperative identification of lymph node metastasis constitutes a pivotal element in the formulation of personalized treatment strategies. It has been demonstrated that inflammatory markers such as neutrophils, lymphocytes, and fibrinogen significantly contribute to cancer progression and prognostic evaluations. In this regard, we propose the fibrinogen-to-neutrophil ratio (FNR) as an innovative and promising biomarker for evaluating pelvic lymph node metastasis in cervical cancer patients with type 2 diabetes.
Methods: The study was conducted on 141 patients diagnosed with cervical cancer and concomitant type 2 diabetes, who were treated at the First Affiliated Hospital of Xiamen University. The patients were randomly divided into a training set (n=98) and a validation set (n=43), with a ratio of 7:3. Univariate and multivariate logistic regression analyses were performed to identify independent risk factors, and a prognostic model was established based on these findings. The model’s effectiveness was evaluated.
Results: A nomogram that integrates multiple factors, including FNR, triglycerides, maximum diameter, and total protein, demonstrates superior potential in predicting pelvic lymph node metastasis in patients with type 2 diabetes and cervical cancer, compared to the use of a single biomarker.
Conclusion: As a comprehensive biomarker, FNR shows significant potential in offering a more thorough and reliable approach for identifying cervical cancer patients with diabetes who are at an elevated risk of lymph node metastasis.
Keywords: cervical cancer, diabetes mellitus, pelvic lymph node metastasis, fibrinogen-to-neutrophil ratio, inflammatory biomarkers, preoperative prediction
Introduction
Cervical Cancer (CC) remains a formidable threat to women’s health, accounting for approximately 300,000 deaths each year.1 It is the third leading cause of cancer-related mortality globally, highlighting its substantial impact on women’s health worldwide.1,2 The global incidence and mortality rates of diabetes mellitus (DM) continue to rise, establishing it as a critical challenge to global health.3 According to projections from the World Health Organization (WHO), the number of individuals affected by diabetes is expected to reach 440 million by 2030.4 This escalating prevalence is driven by a combination of factors, including poor dietary habits, sedentary lifestyles, obesity, genetic predisposition, and an aging population. Diabetes presents a significant threat to individual health and is a major precursor to a range of severe complications, including cardiovascular diseases, stroke, vision impairment, renal failure, and neuropathy. Of particular concern is the impact of chronic hyperglycemia on immune function, which increases vulnerability to infections and exacerbates the risk of additional comorbidities.3–5 A systematic review encompassing 13 studies with a total of 11,091 participants revealed that cervical cancer patients with diabetes experience significantly poorer overall survival and disease-free survival rates in comparison to the non-diabetic counterparts.6 Subsequent research has found that the interplay between diabetes and human papillomavirus (HPV) may heighten the risk of persistent infection, potentially resulting in a cascade of complications. Elevated blood glucose levels, alongside the chronic inflammation linked to diabetes, foster an environment that is conducive to the replication and persistence of the virus.7 Consequently, this mechanism may facilitate the development of HPV-related lesions, which have the potential to advance to precancerous stages or even cancer. Furthermore, the proportion of individuals with diabetes among those diagnosed with cervical cancer has steadily risen, highlighting a growing challenge for patient care worldwide.8 Gaining a more profound understanding of this intricate relationship holds significant importance for the prevention and intervention of associated diseases. Therefore, it is crucial to focus on this vulnerable patient population. By optimizing the management of both diabetes and cervical cancer, patient outcomes can be significantly improved, disease burden alleviated, and the risk of further complications minimized.
Lymph nodes are a crucial and integral component of the immune system, serving as dynamic hubs for immune surveillance and response. They are densely populated with a variety of immune cells, including lymphocytes, macrophages, and dendritic cells, which collaborate seamlessly to mount effective defenses against infections and foreign antigens. In the process of antigen recognition and capture, lymph nodes proficiently present these antigens to immune cells, thereby triggering a cascade of finely tuned immune reactions. As a key node for immune surveillance, response, and regulation, lymph nodes play a pivotal role in the immune system, carrying out essential physiological functions.9 The involvement of lymph nodes plays a significant role in the recurrence and survival prognosis of patients with early-stage cervical cancer. Radical pelvic lymphadenectomy is the standard surgical approach for treating these patients and is considered the gold standard. By removing the lymph nodes, the spread of cancer cells through the lymphatic system can be effectively reduced, lowering the risk of recurrence and improving survival rates. The surgery also allows for accurate assessment of lymph node status, providing critical information for subsequent treatments, thereby optimizing the therapeutic outcome.10 Therefore, radical pelvic lymphadenectomy is one of the key treatment strategies for early-stage cervical cancer patients. Preoperative prediction of the likelihood of pelvic lymph node metastasis is crucial, as it helps in developing personalized treatment plans, further improving treatment efficacy and survival rates. By identifying patients at higher risk for metastasis to the para-aortic lymph nodes before surgery, unnecessary procedures can be avoided, and treatment plans can be specifically adjusted.
Researches have consistently demonstrated a significant interplay between lymph node metastasis and the inflammatory response in tumors.11,12 Inflammation triggers the release of inflammatory cytokines and various bioactive mediators, which not only stimulate tumor cell proliferation but also accelerate the onset and progression of lymph node metastasis.13 Chronic inflammation further impairs immune system function, leading to alterations in both the activity and quantity of immune cells.14 These changes reduce the immune system’s ability to effectively surveil and eliminate tumor cells. Numerous studies have established a close association between a range of inflammation-related biomarkers—such as neutrophils, lymphocytes, C-reactive protein, fibrinogen,15,16 and ratios like the neutrophil-to-lymphocyte ratio (NLR)17 and platelet-to-lymphocyte ratio (PLR)18—and the initiation, progression, and prognosis of cancer. Fibrinogen, a key glycoprotein involved in coagulation during inflammation, has garnered particular attention. Recent findings have underscored a strong correlation between elevated fibrinogen levels and the development, as well as the poor prognosis, of various malignancies.19,20 Based on this, our study proposes a novel predictive biomarker, the fibrinogen-to-neutrophil ratio (FNR), and evaluates its potential value in predicting pelvic lymph node metastasis in cervical cancer patients with concomitant type 2 diabetes. Currently, our study has not been indexed. Therefore, in clinical practice, monitoring and evaluating inflammatory markers is of crucial importance for the early prevention of cancer, the prediction of lymph node metastasis, the selection of treatment plans, and the assessment of patient prognosis. In the future, further exploration of the relationship between inflammation and cancer will not only help us gain a more comprehensive understanding of the mechanisms underlying cancer development, but also provide a solid theoretical foundation and practical guidelines for the formulation of personalized treatment plans and the implementation of early prevention strategies.
Methods
Patients
We included a cohort of 141 patients diagnosed with cervical cancer and concomitant type 2 diabetes, all of whom received treatment at the First Affiliated Hospital of Xiamen University between 2018 and 2022. Each patient underwent standard radical cervical cancer surgery, along with the corresponding lymphadenectomy. The following criteria were applied for exclusion from the study:
- Patients with incomplete or missing clinical data.
- Patients diagnosed with pathological types of cervical cancer other than the commonly occurring squamous cell carcinoma or adenocarcinoma, particularly those with rare histological variants.
- Patients with a history of other malignancies.
- Patients whose hemoglobin A1c levels exceeded 7%, or those with poorly controlled preoperative blood glucose levels that did not meet the surgical eligibility criteria.
- Patients who exhibited signs of pelvic or para-aortic lymph node enlargement, or had evidence of distant metastasis as determined by preoperative imaging.
Collection of Patients’ Information
The clinical dataset for all hospitalized patients encompassed a comprehensive and meticulously curated collection of critical data points. The foundational demographic section included essential details such as the patient’s name, age, and hospital admission number. A detailed medical history section systematically recorded pertinent past medical conditions, notably type 2 diabetes, cervical cancer, and other malignancies. The treatment history offered a thorough account of the therapeutic interventions and medications prescribed in the management of type 2 diabetes. With regard to clinical parameters, the dataset incorporated a wide range of essential diagnostic results, including imaging studies (such as MRI, CT, and PET-CT scans), blood tests (comprising complete blood count and comprehensive chemistry panel analyses), blood glucose monitoring, coagulation function evaluations, and tumor marker assessments. Additionally, histopathological findings from cervical cancer tissue specimens were provided, offering invaluable pathological evidence that supported and refined clinical decision-making.
All patients underwent a thorough preoperative evaluation, which included a comprehensive gynecological examination performed by two skilled gynecologic oncologists. Surgical records and postoperative pathological findings were meticulously documented and systematically organized. By carefully collecting and analyzing the comprehensive data from these patients, our goal is to provide valuable insights to further investigate the role of fibrinogen-to-neutrophil ratio in cervical cancer patients with type 2 diabetes, with a particular focus on the potential association with lymph node metastasis.
Data Analysis
Receiver Operating Characteristic (ROC) curve analysis was used to establish the optimal cutoff values for continuous clinical variables. This ensures that the identified thresholds for variables like FNR, neutrophil count, and others are statistically valid. The 141 patients were randomly divided into a training set (98 patients) and a validation set (43 patients) using a 7:3 ratio. This random allocation minimizes selection bias and ensures that both sets are representative of the overall cohort. Chi-square test was employed to compare baseline characteristics (eg, age, blood indices, pathology type) between the training and validation sets. This validation process helped to eliminate potential confounding factors, thereby reducing the risk of bias in subsequent analyses. Logistic regression analysis was employed to meticulously investigate the impact of various clinical and laboratory variables on the metastasis of lymph node metastasis in patients diagnosed with cervical cancer. To enhance the understanding of the independent risk factors linked to lymph node metastasis within the training set, we integrated variables with a P-value of less than 0.1 from the logistic regression analysis into a multivariate logistic regression model. This approach allows for a more nuanced and thorough evaluation of the associated factors. Through this multivariate analysis, we aim to identify the risk factors influencing lymph node metastasis in cervical cancer.
The nomogram was developed using independent predictors identified from the multivariate regression. This tool integrates multiple clinical factors into a single risk score, which helps in predicting pelvic lymph node metastasis. ROC curves assessed model performance by quantifying its discriminatory ability. Calibration curves confirmed the accuracy of the predicted probabilities compared to observed outcomes, ensuring that the model’s predictions align with actual clinical results. Decision Curve Analysis (DCA) was used to evaluate the clinical benefit of the nomogram across a range of decision thresholds. The newly developed model was evaluated against the original model through a statistical comparison of AUC values. This analysis underscores the improved predictive performance of the new model. Factors with P-value of less than 0.05 was considered statistically significant. Statistical analyses were performed by R 4.0.2.
Results
The Clinical Characteristics of Patients
Between 2018 and 2022, clinical data were collected from 141 patients diagnosed with both cervical squamous cell carcinoma (SCC) and type 2 diabetes mellitus (T2DM) who were admitted to the First Affiliated Hospital of Xiamen University. The data were systematically organized, and receiver operating characteristic (ROC) curve analysis was employed to determine the optimal cutoff values for various continuous variables. Table 1 summarizes the baseline characteristics of the 141 study participants, with data categorized and compared based on the presence or absence of pelvic lymph node metastasis (Metastasis - vs Metastasis +). The findings presented in Table 1 suggest that blood routine and biochemical indicators, along with other clinical parameters, may be significantly associated with the risk of pelvic lymph node metastasis.
 |
Table 1 The Baseline Characteristics of the Study Participants |
The Comparison of Baseline Characteristics Between the Training Set and Validation Set
Subsequently, we employed a random allocation method to divide the total of 141 patients into two groups: a training set consisting of 98 patients and a validation set comprising 43 patients, thus achieving a 7:3 ratio. To ensure the scientific integrity of the data processing, Table 2 presents a comprehensive baseline comparison of several clinical features between the training dataset (N=98) and the external validation dataset (N=43). The clinical variables include age, blood indices, pathological type, and others. Additionally, Table 2 displays the results of a Chi-square test conducted between these two datasets. The analysis reveals no statistically significant differences between the training and validation sets, suggesting a high degree of consistency between the two groups across multiple key indicators. This finding supports the conclusion that both datasets are comparable and can be effectively used for subsequent analyses.
 |
Table 2 The Baseline Characteristics of the Training and the External Validation Dataset |
The Association FNR and Clinicopathological Characteristics
Utilizing the optimal cutoff values for FNR, the subjects were stratified into two distinct groups: a high FNR group (N = 102) and a low FNR group (N = 39). Table 3 presents a detailed analysis of the correlations between various clinical characteristics and FNR, offering a comprehensive distribution of clinical features across the two FNR categories (≤0.659 and >0.659), along with the corresponding P-values to assess the significance of each feature’s association with FNR.
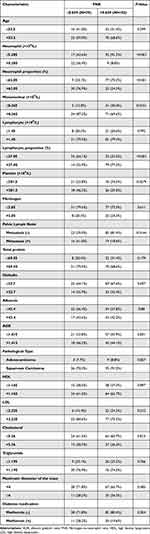 |
Table 3 The Correlations Between FNR and Clinical Characteristics |
The clinical characteristics found to exhibit a significant correlation with FNR included neutrophil count, neutrophil proportion, monocyte count, lymphocyte proportion, platelet count, and the presence of pelvic lymph node metastasis. These factors may play a pivotal role in predicting or influencing FNR outcomes. In contrast, other clinical attributes—such as age, pathology type, and total protein levels—did not demonstrate any significant association with FNR. Of particular note is the strong correlation between the presence of pelvic lymph node metastasis and FNR, suggesting that this factor may be of substantial importance in modulating FNR outcomes. For the remaining features, including age, pathology type, and total protein, no significant correlations were identified.
Univariate and Multivariate Analysis of Logistic Regression in the Training Data Set
Univariate and multivariate logistic regression analyses were performed to elucidate the associations between various characteristics within the training dataset and the risk of pelvic lymph node metastasis. The univariate regression analysis enabled us to assess the potential influence of multiple clinical and laboratory indicators on the risk of metastasis to the pelvic lymph nodes. As shown in Table 4, the findings from the analysis revealed that a number of clinical features and biochemical markers—such as neutrophil count, neutrophil percentage, monocyte count, lymphocyte count, lymphocyte percentage, fibrinogen levels, FNR, total protein levels, globulin levels, cholesterol, triglycerides, and maximum tumor diameter—exhibited significant correlations with the risk of pelvic lymph node metastasis. Subsequent multivariate regression analysis demonstrated that, after adjusting for numerous confounding variables, FNR, total protein, triglycerides, and maximum tumor diameter emerged as independently statistically significant predictors of pelvic lymph node metastasis.
 |
Table 4 Univariate and Multivariate Analysis of Logistic Regression in the Training Data Set |
The Construction of the Predictive Nomogram
A nomogram was developed based on independent predictive factors identified through multivariable analysis to assess the risk of pelvic lymph node metastasis. The Figure 1 illustrates the score assigned to each predictive factor, and by summing the individual scores, a total score is derived that serves to estimate the risk of pelvic lymph node metastasis prior to surgery. This nomogram offers clinicians a streamlined and efficient tool for calculating a patient’s total score based on specific clinical characteristics, thus enabling an accurate prediction of pelvic lymph node metastasis before surgical intervention.
 |
Figure 1 The nomogram for predicting pelvic lymph node metastasis in cervical cancer patients with type 2 diabetes mellitus. Abbreviation: FNR, fibrinogen-to-neutrophil ratio. |
The Evaluation of the Model’s Effectiveness
To thoroughly assess the accuracy and practical utility of the Nomogram model in predicting pelvic lymph node metastasis, we utilized the R package to generate the ROC curve, which served as a quantitative measure of model performance. Evaluation of both the training set (Figure 2A) and the validation set (Figure 2B) revealed area under the curve (AUC) values of 0.892 and 0.858, respectively. These results highlight the model’s robust predictive ability across both datasets, suggesting that the Nomogram provides a reliable forecast of pelvic lymph node metastasis and demonstrates strong discriminatory power. This indicates its potential to support clinicians in identifying high-risk patients.
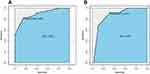 |
Figure 2 Receiver operating characteristic (ROC) curve analysis was utilized to evaluate the performance of the model. (A) The training dataset. (B) The external validation dataset. |
In addition to the AUC, we assessed the model’s goodness of fit through the Calibration curve. The results, presented in Figure 3A and B, show a high degree of concordance between the actual incidence of pelvic lymph node metastasis and the probabilities estimated by the model. To further evaluate the clinical relevance of this predictive tool, we performed a Decision Curve Analysis (DCA). As shown in Figure 4, the Nomogram model delivers a substantial net benefit across a wide range of risk thresholds, reinforcing its clinical applicability.
 |
Figure 3 The calibration curve of the nomogram was evaluated. (A) The training dataset. (B) The external validation dataset. |
 |
Figure 4 The validation of the decision curve analysis (DCA) for the nomogram. (A) The training dataset. (B) The external validation dataset. |
The Comparative Analysis With Preceding Models
In this study, we conducted a systematic comparative analysis between the newly developed model and the original model to assess the improvement in performance on the test dataset. The original model, proposed by Li-Xian Li et al, served as the benchmark for our comparison.21 This model, which takes into account factors such as stage, degree of differentiation, age, and pathology type, achieved AUC values of 0.835, 0.516, 0.511, and 0.479, respectively, on the test dataset. While demonstrating a reasonable level of accuracy, it revealed certain limitations in addressing specific factors. In contrast, the AUC value of our newly established model improved to 0.853 (Figure 5A and B), indicating a marked enhancement in performance, particularly in its predictive capabilities for stage, degree of differentiation, and pathology type, where it outperformed the original model.
 |
Figure 5 The comparative analysis with preceding models. (A) Receiver operating characteristic (ROC) curve analysis. (B) Comparative evaluation with the original model. |
Discussion
The findings of this study highlight the potential value of inflammatory biomarkers, particularly the fibrinogen-to-neutrophil ratio (FNR), in predicting pelvic lymph node metastasis in patients with type 2 diabetes and cervical cancer. To date, no similar research has been identified in the existing literature, positioning this study as a pioneering contribution to the field. Consequently, it addresses a critical gap in knowledge and introduces a novel, clinically relevant risk assessment tool, offering significant clinical contributions.
Pelvic lymphadenectomy has long been a standard procedure performed by gynecological oncologists in the management of cervical cancer. This surgical intervention has been widely regarded as the gold standard for evaluating lymph node involvement, offering critical insights into the extent of disease dissemination. The status of pelvic lymph nodes plays a pivotal role in shaping the treatment plan, including decisions regarding the potential need for adjuvant therapies such as radiation or chemotherapy. However, in recent years, there has been a growing debate within the clinical community regarding the therapeutic benefits and overall necessity of this procedure. Research has shown that lymph node dissection may not substantially improve overall survival rates, especially in patients with early-stage cervical cancer. A recent study has underscored the critical significance of lymph node assessment in patients with early-stage cervical cancer, particularly concerning fertility-sparing treatments. The status of lymph nodes serves as a pivotal prognostic factor within this patient population, exerting a direct influence on treatment decisions and subsequent outcomes. In a retrospective, multi-institutional study involving data from 123 patients diagnosed with early-stage cervical cancer, the research team observed results after a median follow-up period of 53.6 months. The findings revealed that disease-free survival and overall survival rates among the groups were comparable. The study notably demonstrated that, regardless of the method employed—whether sentinel node mapping or pelvic lymphadenectomy—no significant differences were observed in long-term oncological outcomes. Moreover, the pelvic lymphadenectomy approach was correlated with a decrease in several complications, including lymphocele, lymphedema, vascular injuries, nerve damage, and infections.22 Additionally, there is a lack of standardized clinical guidelines to determine the most appropriate types and extent of pelvic lymph node removal.23 There is ongoing professional debate regarding the necessity of pelvic lymphadenectomy, as well as the most effective method for determining the appropriate extent and depth of resection to be performed. Research has indicated that the incidence of lymph node metastasis in early-stage cervical cancer ranges from 15% to 25%, suggesting that approximately 75% to 85% of patients do not exhibit lymph node involvement.24 Consequently, the majority of patients undergoing lymph node dissection—approximately 80%—may derive little to no significant benefit from the procedure, unless metastasis is confirmed or the risk is deemed elevated. Nonetheless, lymph node dissection remains a pivotal component in the management of these patients, as it can play a crucial role in optimizing tumor control and improving overall survival outcomes.
Preoperative assessment of pelvic lymph node metastasis is critical for the development of tailored treatment strategies. While PET/CT and MRI are commonly employed to detect lymph node involvement, their sensitivity can be limited, particularly when assessing nodes smaller than 5 mm or in the presence of micro-metastases.25 Recently, the combined use of PET and MRI—especially with the incorporation of diffusion-weighted imaging (DWI)—has garnered increased attention due to its enhanced resolution and potential clinical relevance. Although initial studies have shown promising results, further validation is required to establish the clinical applicability of this approach.26 As a result, the accurate detection of pelvic lymph node metastasis remains a significant challenge in clinical practice, underscoring the need for more precise imaging modalities to guide clinical decision-making. To address this challenge, the current study proposes an innovative preoperative nomogram model, highlighting the potential role of inflammatory biomarkers, particularly the fibrinogen-to-neutrophil ratio, in predicting pelvic lymph node metastasis in patients with type 2 diabetes.
Based on our findings, the FNR serves as a composite biomarker that offers a robust and comprehensive approach to assessing alterations in fibrinogen and neutrophil levels. This dual evaluation significantly enhances its reliability as a tool for identifying high-risk patients. Its clinical relevance is particularly evident in predicting the likelihood of pelvic lymph node metastasis. However, the underlying mechanisms by which FNR reflects the tumor characteristics of cervical cancer remain not fully understood and warrant further investigation.
The following reasons and evidence provide important insights into our findings: An increasing number of studies have highlighted the crucial role of inflammation in the initiation, progression, and metastasis of cancer. Inflammation not only induces changes in the tumor microenvironment and modulates immune responses, but it also directly impacts fundamental processes such as tumor cell proliferation, survival, invasion, and metastatic potential. As a key biomarker in cancer, systemic inflammatory responses are increasingly recognized as critical factors in assessing cancer prognosis.27,28
The role of inflammation in the tumor microenvironment is multifaceted, influencing not only the remodeling of the tumor microenvironment and the regulation of immune responses but also, in certain instances, exerting direct effects on the proliferation, survival, invasion, and metastatic capabilities of tumor cells.28–30 Inflammatory cells serve a pivotal role as intermediaries between the neoplasm and the host’s inflammatory response. Within the tumor microenvironment, there is frequently a pronounced accumulation of these inflammatory cells in intimate proximity to the tumor cells.30 These cells engage in complex interactions with tumor cells and endothelial cells, collectively contributing to the dynamic and intricate nature of the tumor microenvironment. In recent years, neutrophils have emerged as a focal point of research due to their pivotal role in cancer progression. An elevated ratio of neutrophils is increasingly recognized as a significant prognostic indicator in cancer patients. The functions of neutrophils extend far beyond the traditional scope of innate immune cells; they exhibit remarkable diversity and high degrees of plasticity. This inherent plasticity enables neutrophils to adapt dynamically to various cancer microenvironments, thereby assuming multifaceted roles throughout the cancer process.31 Comprehensive pan-carcinoma screening has consistently identified the presence of CD66b+ tumor-associated neutrophils (TANs) within tumor-draining lymph nodes (TDLNs), with a notable prevalence of 59%. Microscopic examinations have further elucidated the formation of intra-lymphatic conjugates between TANs and cancer cells, highlighting a significant and active migration of these neutrophils through the lymphatic vessels.32 Extensive research has elucidated the complex interplay between chronic inflammatory states and the activation of various signaling pathways. These pathways are critical in regulating cytokine secretion patterns, which significantly enhance the ability of tumor cells to metastasize to distant organs via the bloodstream or lymphatic system, as illustrated in Figure 6.30,33 Another recent study has underscored the vital role of neutrophils in the lymph node metastasis of cervical cancer, particularly through the formation of neutrophil extracellular traps (NETs). The research revealed increased neutrophil infiltration and NETs formation in the lymph node metastases of cervical cancer patients. Further analysis showed a strong correlation between S100A7 expression and neutrophil infiltration, highlighting their notable interplay. Additionally, the study also demonstrated that NETs activate the TLR2 receptor, triggering the P38-MAPK/ERK/NFκB pathway and enhancing cervical cancer cell migration. Furthermore, NETs have been demonstrated to enhance lymphangiogenesis and vascular permeability, accelerating lymphatic metastasis in cervical cancer. This study investigated the critical function of neutrophils in the metastatic process, with a particular focus on the formation of NETs in the context of cervical cancer.34 Furthermore, in the inflammatory microenvironment, immune cells such as macrophages, T cells, dendritic cells, and other immune mediators play a pivotal role, acting as both key drivers of tumor initiation and progression, and contributing significantly to the modulation of the tumor microenvironment. These immune cells are capable of precisely regulating various tumor processes, including cell growth, survival, invasion, and metastasis, through the secretion of cytokines, chemokines, and other immune-active molecules.35 Biomarkers associated with systemic inflammatory responses serve as pivotal indicators of cancer prognosis, showcasing considerable promise as both predictive biomarkers and prospective therapeutic targets.
Fibrinogen plays a pivotal role in the complex process of blood coagulation and is intricately associated with a spectrum of diseases. Notably, elevated levels of fibrinogen have been correlated with adverse prognostic outcomes in various malignancies, including esophageal, lung, and kidney cancers.36,37 Recent research has underscored its significant involvement in tumor progression, highlighting its potential implications in the pathophysiology of these conditions.38 A comprehensive study investigated the prognostic significance of preoperative hyperfibrinogenemia (HF) in patients diagnosed with esophageal squamous cell carcinoma (ESCC). Among the 452 cases examined, a notable 24.8% exhibited elevated levels of HF, which was found to correlate significantly with tumor characteristics. Survival analysis revealed that patients presenting with high HF levels experienced markedly poorer disease-free survival and overall survival compared to the counterparts. Furthermore, multivariate Cox regression analysis affirmed HF as an independent negative prognostic factor. The investigation also uncovered that fibrin enhances the migration and invasion of ESCC cells through the induction of epithelial-mesenchymal transition (EMT) and by upregulating key signaling proteins within the p-AKT/p-mTOR pathway, thereby illustrating its detrimental effects. Consequently, preoperative fibrinogen levels may serve as a valuable independent predictive marker for adverse outcomes in ESCC.39 This correlation underscores its significant role in tumor progression and positions fibrinogen as a potential oncological biomarker of clinical relevance. Furthermore, fibrinogen is essential in promoting the interaction of thrombin within the complex mechanisms of tumor metastasis. Studies have highlighted that this interaction is particularly significant within the intricate network of relationships among thrombin, PAR-1, and fibrinogen. In genetically deficient mouse models lacking these pathways, a pronounced inhibition of colon adenocarcinoma growth was observed. This phenomenon was characterized by a significant reduction in cellular proliferation, an enhanced occurrence of tumor necrosis, and a marked decrease in vascular density.40 These findings provide significant evidence highlighting the essential role of fibrinogen in the growth and metastatic spread of malignant tumors.
Fibrinogen and albumin are pivotal biomarkers with extensive applications in evaluating the systemic inflammatory response (SIR) and nutritional status in a variety of cancers and other significant diseases. Fibrinogen, as a key acute-phase response protein, holds particular importance in clinical practice. It serves not only as an effective tool for monitoring disease activity but also as a prognostic indicator for patients, thereby offering critical insights to inform clinical decision-making.41,42 The fibrinogen-to-albumin ratio (FAR) has demonstrated significant correlations with various clinicopathological indicators of esophageal cancer, particularly with pN status. This suggests that elevated FAR may serve as a potential predictor of lymph node metastasis in esophageal cancer patients. These findings imply that FAR is closely associated with the metastatic potential of the tumor or alterations in the tumor microenvironment. Consequently, FAR could serve as a valuable biomarker in the early diagnosis, staging, and prognosis of esophageal cancer, and may offer new avenues for the development of personalized treatment strategies.43
The management of cervical cancer has witnessed considerable advancements over recent decades, chiefly attributable to improvements in early diagnosis, surgical techniques, and adjunctive therapies. As the landscape of cancer research has evolved, treatment guidelines for early-stage cervical cancer have been continually refined. The recently published findings from the SHAPE trial carry significant clinical implications, demonstrating that in low-risk cervical cancer patients—specifically those presenting with lesions measuring ≤2 cm and confined to stromal invasion—hysterectomy offers oncological outcomes comparable to those of radical surgery, while markedly reducing both short-term and long-term complications.44 This discovery underscores the pivotal role of lymph node metastasis as a prognostic factor in determining the necessity for adjuvant therapy, thereby highlighting the critical importance of lymph node assessment in treatment planning. Our research underscores the potential of inflammatory biomarkers, specifically FNR, in predicting pelvic lymph node metastasis in patients with type 2 diabetes and cervical cancer. Inflammation plays a pivotal role in cancer progression and metastasis, and our study suggests that FNR, as a multifaceted biomarker, holds promise for providing a more comprehensive and reliable method for identifying patients at elevated risk of lymph node metastasis. The distinctive advantage of FNR lies in its capacity to reflect systemic inflammation and immune response alterations, allowing for the assessment of a patient’s inflammatory status and metastasis risk through a non-invasive blood test. When compared to individual biomarkers, the nomogram that integrates FNR with triglycerides, maximum tumor diameter, and total protein offers clinicians a novel tool for personalized risk assessment and the optimization of treatment strategies. By accurately identifying patients at high risk for lymph node metastasis preoperatively, this approach helps to avoid unnecessary invasive procedures while ensuring more precise and individualized treatment plans.
In our research, the implementation of FNR as a solitary biomarker holds considerable significance; however, its use is accompanied by certain limitations. Primarily, the emphasis on FNR as an isolated indicator has culminated in a constrained understanding of its applicability across diverse populations. Consequently, future investigations should seek to explore the role of FNR in conjunction with other inflammatory biomarkers across various stages and types of cancer, marking a pivotal direction for research. Furthermore, the current lack of sample diversity may adversely affect the generalizability of the research findings, thereby restraining the broader applications. To address this concern, future studies should endeavor to expand the sample sources by incorporating populations from differing geographical regions and age cohorts, thereby enhancing the representativeness of the research. In addition, considering the heterogeneity of diseases and individual variations among patients, the adoption of a multi-center study design would significantly enrich the research sample and encompass a broader array of backgrounds. This approach would facilitate a more nuanced evaluation of the effectiveness of FNR as a biomarker. Lastly, clinical trials that integrate relevant treatment strategies will be essential for validating the efficacy and practical utility of these biomarkers in informed clinical decision-making.
Conclusion
In conclusion, the FNR is a promising predictive biomarker for pelvic lymph node metastasis in cervical cancer patients with type 2 diabetes. The nomogram developed in this study provides a reliable and clinically useful tool for predicting lymph node metastasis and guiding treatment decisions. Future studies with larger cohorts and long-term follow-up are needed to validate these findings and refine the nomogram for broader clinical use.
Through a comprehensive analysis, we have established that the FNR demonstrates both high sensitivity and specificity in reflecting the inflammatory response as well as the risk of tumor metastasis. Notably, in patients with diabetes, the inflammatory response may be further exacerbated, potentially enhancing the invasiveness of tumor cells and thereby accelerating the onset and progression of lymph node metastasis. As such, FNR not only serves as a valuable biomarker for inflammation but also holds promise as a crucial adjunct in predicting disease progression in cervical cancer patients.
Ethics Approval
The approval of the clinical ethics committee was obtained from the ethics committee of the First Affiliated Hospital of Xiamen University (No. SL-2024KY272-01). This study was conducted in accordance with the Declaration of Helsinki, and the use of data/material only for research purposes.
Ethical Approval and Informed Consent
Ethical approval for this study was obtained from the Ethics Committee of the First Affiliated Hospital of Xiamen University. The study was conducted in strict adherence to the principles set forth in the Declaration of Helsinki. All participants were thoroughly informed about the study’s objectives and procedures, and written informed consent was obtained from each participant prior to their involvement.
Consent for Publication
Written informed consent was obtained from the patient about publication.
Funding
This work supported by the Natural Science Foundation of Fujian Province, China. (Grant No. 2022J05310) and Natural Science Foundation of Xiamen, China (Grant No. 3502Z20227337).
Disclosure
All authors declare no potential conflicts of interest in this work.
References
1. Molina MA, Steenbergen RDM, Pumpe A, Kenyon AN, Melchers WJG. HPV integration and cervical cancer: a failed evolutionary viral trait. Trends Mol Med. 2024;30(9):890–902. doi:10.1016/j.molmed.2024.05.009
2. Arbyn M, Weiderpass E, Bruni L, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2020;8(2):e191–e203. doi:10.1016/S2214-109X(19)30482-6
3. Cloete L. Diabetes mellitus: an overview of the types, symptoms, complications and management. Nurs Stand. 2022;37(1):61–66. doi:10.7748/ns.2021.e11709
4. Nentwich MM, Ulbig MW. Diabetic retinopathy - ocular complications of diabetes mellitus. World J Diabetes. 2015;6(3):489–499. doi:10.4239/wjd.v6.i3.489
5. Lovic D, Piperidou A, Zografou I, Grassos H, Pittaras A, Manolis A. The Growing Epidemic of Diabetes Mellitus. Curr Vasc Pharmacol. 2020;18(2):104–109. doi:10.2174/1570161117666190405165911
6. Chen S, Tao M, Zhao L, Zhang X. The association between diabetes/hyperglycemia and the prognosis of cervical cancer patients: a systematic review and meta-analysis. Medicine. 2017;96(40):e7981. doi:10.1097/MD.0000000000007981
7. Yue C, Zhang C, Ying C, Jiang H. Diabetes associated with HPV infection in women aged over 50 years: a cross-sectional study from China’s largest academic woman’s hospital. Front Endocrinol. 2022;13:972963. doi:10.3389/fendo.2022.972963
8. Bhatia D, Lega IC, Wu W, Lipscombe LL. Breast, cervical and colorectal cancer screening in adults with diabetes: a systematic review and meta-analysis. Diabetologia. 2020;63(1):34–48. doi:10.1007/s00125-019-04995-7
9. du Bois H, Heim TA, Lund AW. Tumor-draining lymph nodes: at the crossroads of metastasis and immunity. Sci Immunol. 2021;6(63):eabg3551. doi:10.1126/sciimmunol.abg3551
10. Tohyama A, Murakami M, Yoshino K. Strategies for the Treatment of Cervical Cancer with Bulky Pelvic Lymph Nodes: an Overview of the Current Evidence. J UOEH. 2020;42(4):317–325. doi:10.7888/juoeh.42.317
11. Gu Y, Yu M, Deng J, Lai Y. The Association of Pretreatment Systemic Immune Inflammatory Response Index (SII) and Neutrophil-to-Lymphocyte Ratio (NLR) with Lymph Node Metastasis in Patients with Papillary Thyroid Carcinoma. Int J Gen Med. 2024;17:2887–2897. doi:10.2147/IJGM.S461708
12. Catal O, Ozer B, Sit M. Prediction of Lymph Node Metastasis in Colon Cancer via Platelet to Lymphocyte Ratio and Platelet Count. J Coll Physicians Surg Pak. 2020;30(3):250–253. doi:10.29271/jcpsp.2020.03.250
13. Ma Y, Ren Y, Dai ZJ, Wu CJ, Ji YH. IL-6 XJ, IL-8 and TNF-alpha levels correlate with disease stage in breast cancer patients. Adv Clin Exp Med. 2017;26(3):421–426. doi:10.17219/acem/62120
14. Lasser SA, Ozbay Kurt FG, Arkhypov I, Utikal J, Umansky V. Myeloid-derived suppressor cells in cancer and cancer therapy. Nat Rev Clin Oncol. 2024;21(2):147–164. doi:10.1038/s41571-023-00846-y
15. Ye L, Zhou G, Zhou L, et al. Diagnostic roles of neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio, platelet-to-lymphocyte ratio, C-reactive protein, and cancer antigen 125 for ovarian cancer. J Int Med Res. 2023;51(12):3000605231218557. doi:10.1177/03000605231218557
16. Acevedo-Leon D, Gomez-Abril SA, Sanz-Garcia P, Estan-Capell N, Banuls C, Saez G. The role of oxidative stress, tumor and inflammatory markers in colorectal cancer patients: a one-year follow-up study. Redox Biol. 2023;62:102662. doi:10.1016/j.redox.2023.102662
17. Cupp MA, Cariolou M, Tzoulaki I, Aune D, Evangelou E, Berlanga-Taylor AJ. Neutrophil to lymphocyte ratio and cancer prognosis: an umbrella review of systematic reviews and meta-analyses of observational studies. BMC Med. 2020;18(1):360. doi:10.1186/s12916-020-01817-1
18. Takada K, Kashiwagi S, Asano Y, et al. Prediction of Sentinel Lymph Node Metastasis Using the Platelet-to-lymphocyte Ratio in T1 Breast Cancer. Anticancer Res. 2020;40(4):2343–2349. doi:10.21873/anticanres.14202
19. Jiang C, Li Y, Li Y, et al. Fibrinogen promotes gallbladder cancer cell metastasis and extravasation by inducing ICAM1 expression. Med Oncol. 2022;40(1):10. doi:10.1007/s12032-022-01874-x
20. Li X, Shu K, Zhou J, et al. Preoperative Plasma Fibrinogen and D-dimer as Prognostic Biomarkers for Non-Muscle-Invasive Bladder Cancer. Clin Genitourin Cancer. 2020;18(1):11–9e1. doi:10.1016/j.clgc.2019.10.025
21. Deng YR, Chen XJ, Xu CQ, et al. A preoperative nomogram predicting risk of lymph node metastasis for early-stage cervical cancer. BMC Womens Health. 2023;23(1):568. doi:10.1186/s12905-023-02726-0
22. Bogani G, Scambia G, Fagotti A, et al. Sentinel node mapping, sentinel node mapping plus back-up lymphadenectomy, and lymphadenectomy in Early-sTage cERvical caNcer scheduled for fertilItY-sparing approach: the ETERNITY project. Eur J Surg Oncol. 2024;50(9):108467. doi:10.1016/j.ejso.2024.108467
23. Borcinova M, Ragosch V, Jarkovsky J, et al. Challenges in lower limb lymphoedema assessment based on limb volume change: lessons learnt from the SENTIX prospective multicentre study. Gynecol Oncol. 2022;164(1):76–84. doi:10.1016/j.ygyno.2021.10.089
24. Kuroda K, Yamamoto Y, Yanagisawa M, et al. Risk factors and a prediction model for lower limb lymphedema following lymphadenectomy in gynecologic cancer: a hospital-based retrospective cohort study. BMC Womens Health. 2017;17(1):50. doi:10.1186/s12905-017-0403-1
25. Mayoral M, Paredes P, Domenech B, et al. (18)F-FDG PET/CT and sentinel lymph node biopsy in the staging of patients with cervical and endometrial cancer. Role of dual-time-point imaging. Rev Esp Med Nucl Imagen Mol. 2017;36(1):20–26. doi:10.1016/j.remn.2016.07.003
26. Stecco A, Buemi F, Cassara A, et al. Comparison of retrospective PET and MRI-DWI (PET/MRI-DWI) image fusion with PET/CT and MRI-DWI in detection of cervical and endometrial cancer lymph node metastases. Radiol Med. 2016;121(7):537–545. doi:10.1007/s11547-016-0626-5
27. Singh N, Baby D, Rajguru JP, Patil PB, Thakkannavar SS, Pujari VB. Inflammation and cancer. Ann Afr Med. 2019;18(3):121–126. doi:10.4103/aam.aam_56_18
28. Khandia R, Munjal A. Interplay between inflammation and cancer. Adv Protein Chem Struct Biol. 2020;119:199–245. doi:10.1016/bs.apcsb.2019.09.004
29. Greten FR, Grivennikov SI. Inflammation and Cancer: triggers, Mechanisms, and Consequences. Immunity. 2019;51(1):27–41. doi:10.1016/j.immuni.2019.06.025
30. Wen Y, Zhu Y, Zhang C, et al. Chronic inflammation, cancer development and immunotherapy. Front Pharmacol. 2022;13:1040163. doi:10.3389/fphar.2022.1040163
31. Xiong S, Dong L, Cheng L. Neutrophils in cancer carcinogenesis and metastasis. J Hematol Oncol. 2021;14(1):173. doi:10.1186/s13045-021-01187-y
32. Lonardi S, Missale F, Calza S, et al. Tumor-associated neutrophils (TANs) in human carcinoma-draining lymph nodes: a novel TAN compartment. Clin Transl Immunology. 2021;10(2):e1252. doi:10.1002/cti2.1252
33. Hibino S, Kawazoe T, Kasahara H, et al. Inflammation-Induced Tumorigenesis and Metastasis. Int J mol Sci. 2021;22(11). doi:10.3390/ijms22115421
34. Ning Y, Chen Y, Tian T, et al. S100A7 orchestrates neutrophil chemotaxis and drives neutrophil extracellular traps (NETs) formation to facilitate lymph node metastasis in cervical cancer patients. Cancer Lett. 2024;605:217288. doi:10.1016/j.canlet.2024.217288
35. Liu Y, Li L, Li Y, Zhao X. Research Progress on Tumor-Associated Macrophages and Inflammation in Cervical Cancer. Biomed Res Int. 2020;2020:6842963. doi:10.1155/2020/6842963
36. Li W, Tang Y, Song Y, et al. Prognostic Role of Pretreatment Plasma D-Dimer in Patients with Solid Tumors: a Systematic Review and Meta-Analysis. Cell Physiol Biochem. 2018;45(4):1663–1676. doi:10.1159/000487734
37. Lin Y, Liu Z, Qiu Y, et al. Clinical significance of plasma D-dimer and fibrinogen in digestive cancer: a systematic review and meta-analysis. Eur J Surg Oncol. 2018;44(10):1494–1503. doi:10.1016/j.ejso.2018.07.052
38. Dzikowski L, Mirzaei R, Sarkar S, et al. Fibrinogen in the glioblastoma microenvironment contributes to the invasiveness of brain tumor-initiating cells. Brain Pathol. 2021;31(5):e12947. doi:10.1111/bpa.12947
39. Zhang F, Wang Y, Sun P, et al. Fibrinogen promotes malignant biological tumor behavior involving epithelial-mesenchymal transition via the p-AKT/p-mTOR pathway in esophageal squamous cell carcinoma. J Cancer Res Clin Oncol. 2017;143(12):2413–2424. doi:10.1007/s00432-017-2493-4
40. Adams GN, Rosenfeldt L, Frederick M, et al. Colon Cancer Growth and Dissemination Relies upon Thrombin, Stromal PAR-1, and Fibrinogen. Cancer Res. 2015;75(19):4235–4243. doi:10.1158/0008-5472.CAN-15-0964
41. You X, Zhou Q, Song J, Gan L, Chen J, Shen H. Preoperative albumin-to-fibrinogen ratio predicts severe postoperative complications in elderly gastric cancer subjects after radical laparoscopic gastrectomy. BMC Cancer. 2019;19(1):931. doi:10.1186/s12885-019-6143-x
42. Sun SY, Chen PP, Meng LX, et al. High preoperative plasma fibrinogen and serum albumin score is associated with poor survival in operable esophageal squamous cell carcinoma. Dis Esophagus. 2019;32(1). doi:10.1093/dote/doy057
43. Tan Z, Zhang M, Han Q, et al. A novel blood tool of cancer prognosis in esophageal squamous cell carcinoma: the Fibrinogen/Albumin Ratio. J Cancer. 2017;8(6):1025–1029. doi:10.7150/jca.16491
44. D’Augè TG, Donato VD, Giannini A. Strategic Approaches in Management of Early-Stage Cervical Cancer: a Comprehensive Editorial. CEOG. 2024;51(10). doi:10.31083/j.ceog5110235
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


