Back to Journals » Breast Cancer: Targets and Therapy » Volume 16
A Prospective Tumour Marker for Breast Cancer: YWHAB and Its Role in Promoting Oncogenic Phenotypes
Authors Gopaul VL, Winstone L, Gatien BG, Nault BD, Maiti S, Opperman RM, Majumder M
Received 8 July 2024
Accepted for publication 5 December 2024
Published 14 December 2024 Volume 2024:16 Pages 935—956
DOI https://doi.org/10.2147/BCTT.S479384
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Robert Clarke
YWHAB Promotes Oncogenic Phenotypes – Video abstract [479384]
Views: 130
Vaishnavi L Gopaul,* Lacey Winstone,* Beatrice G Gatien,* Braydon D Nault, Sujit Maiti, Reid M Opperman, Mousumi Majumder
Department of Biology, Brandon University, Brandon, MB, Canada
*These authors contributed equally to this work
Correspondence: Mousumi Majumder, Email [email protected]
Background: YWHAB (14-3-3 Beta) was found in the secretome of miR-526b and miR-655 overexpressed breast cancer (BRCA) cell lines. The potential of YWHAB as a therapeutic target or biomarker for BRCA is investigated here.
Methods: After YWHAB was knocked down with siRNA, BRCA cell lines were used for in vitro assays (proliferation, migration, epithelial-to-mesenchymal transition). In silico analysis and in situ validation with BRCA plasma and biopsy tissues were used to test YWHAB’s biomarker potential.
Results: YWHAB RNA and protein expression are elevated in aggressive BRCA cell lines, and the knockdown of YWHAB inhibited cell migration, proliferation, and EMT in all subtypes of tumour cell lines. YWHAB expression is significantly higher in BRCA biopsy tissue and blood plasma compared to control tissues and benign plasmas. YWHAB is expressed in all hormonal subtypes of BRCA tumours and has shown increased expression in advanced tumour stages. Its high expression is linked to poor patient survival. YWHAB is a sensitivity tumour marker (AUC of 0.7340, p = 0.0012) but is not a promising blood biomarker. Nevertheless, combined with pri-miR-526b, YWHAB mRNA expression shows potential as a BRCA blood biomarker (AUC of 0.711, p = 0.032), which must be validated in a larger sample set.
Conclusion: We elucidate the novel role of YWHAB as a therapeutic target in BRCA, given that its inhibition mitigated aggressive phenotypes across all tumour subtypes, including triple-negative breast cancer. Furthermore, YWHAB emerges as a potential tumour marker, exhibiting high expression in metastatic BRCA and correlating with poor patient survival; however, it is not a sensitive blood biomarker.
Keywords: breast cancer, microRNA, miRNA, miR-526b, miR-655, YWHAB, 14-3-3 Beta, biomarker, migration, epithelial to mesenchymal transition, proliferation
Graphical Abstract:

Introduction
Globally, breast cancer is the most diagnosed and deadliest cancer in women.1 In Canada, an average of 78 women are diagnosed with breast cancer, and 15 deaths occur due to breast cancer every day.2 A mammogram is the standard diagnostic procedure. However, routine mammogram screening is only recommended for women aged 50.3 A more accessible screening test, such as a blood test, could significantly improve the chances of early breast cancer detection to ensure a good clinical outcome.4
MicroRNAs (miRNA) are small non-coding RNAs that regulate gene expression at the post-transcriptional level. Two miRNAs, miR-526b and miR-655, have been identified as oncogenic in human breast cancer and show biomarker potential. The overexpression of these miRNAs promotes aggressive breast cancer phenotypes, including migration, invasion, inducing EMT,5,6 oxidative stress, tumour-associated angiogenesis, and lymphangiogenesis.7,8 Cell-free miRNA in the secretome treatment altered phenotypes of normal epithelial and endothelial cells and altered tumour microenvironment (TME).7,8 To further investigate how these oncogenic miRNAs can alter the tumour microenvironment to promote metastasis, a secretome analysis was conducted by comparing miRNA-high and miRNA-low breast cancer cells. This identified several secretory proteins differentially regulated in the secretome that could drive these phenotypes.9 One of the identified proteins, tyrosine 3-monooxygenase/tryptophan 5-monooxygenase activation protein beta (YWHAB), was upregulated in the miRNA-high cell secretome.
YWHAB (also known as YWHAA or 14-3-3 Beta or alpha) is a member of the 14-3-3 protein family.10 The mammalian 14-3-3 protein family comprises seven paralogous, highly conserved proteins.11 These are phospho-serine/phospho-threonine binding proteins ubiquitously expressed in all human body tissues.12,13 Due to a wide range of binding partners, 14-3-3 proteins are crucial for many cellular functions,12 including cellular migration, apoptosis, proliferation, and cell cycle signalling.10,14 YWHAB has been identified as a driver of several types of cancer. The YWHAB protein has been linked to lymph node metastasis in gastric cancer and cervical cancer,15 and high YWHAB gene expression in blood serum has been related to tumour growth and poor patient survival.16,17 In a murine model, YWHAB expression was linked to cell proliferation and breast cancer in rats18 as well as in glioblastoma.19 Studies have also linked its expression with various miRNAs, such as a negative correlation between YWHAB and miR-129-5p in lung cancer.20 In another study investigating the effects of circ_0006282 and miR-144-5p in gastric cancer, a regulatory network with YWHAB was observed. Notably, YWHAB was positively modulated by miR-144-5p expression.21 miR-542-5p, a predictive breast cancer biomarker, is correlated with poor patient survival when overexpressed in tamoxifen-treated ER-positive breast cancer, and YWHAB is a downstream target of miR-542-5p.22 The roles of YWHAB in breast cancer cell migration require further investigation, and how miR-526b and miR-655 regulate YWHAB expression is currently unknown. Here, we aim to explore the roles of YWHAB in breast cancer and its potential as a biomarker for breast cancer.
Materials and Methods
Cell Culture
Cell lines MCF7, SKBR3 and Hs578T were purchased from the American Type Culture Collection (ATCC, Rockville, MD, USA). Stable miR-526b-, miR-655- and COX2-overexpressing cell lines (MCF7-miR-526b, MCF7-miR-655, MCF7-COX2, and SKBR3-miR-526b) and empty vector controls (MCF7-Mock and SKBR3-Mock) were established using transfection of the overexpression and empty vector plasmids respectively.5,6 These cells were cultured in RPMI media (Gibco, Mississauga, ON) supplemented with 10% fetal bovine serum (FBS) (Gibco, Mississauga, ON) and 1% penicillin-streptomycin (Gibco, Mississauga, ON). Additionally, transfected cells received Geneticin (Life Technologies ThermoFisher, Ottawa, ON, Canada) 200nM/mL. All cells were grown in an incubator at 37°C and 5% CO2.
RNA Extraction
From Cells and Cell-Free Secretion
Cells were grown until 90% confluent, and RNA was extracted from whole cells using miRNeasy Mini kit (Cat #217004, Qiagen, ON, Canada) following the manufacturer protocol. For RNA extraction from cell-free secretions (also known as conditioned media),7–9 cells were grown to 85% confluency in complete media, washed with PBS to remove the traces of complete media, and then further grown for 24 hours in the basal media. After 24 hours, the conditioned media (which contains cell secretion and metabolites) was collected and centrifuged to remove cell debris. The RNA was extracted from the clear supernatant using the miRNeasy Mini kit.7–9
From Human Specimens
Biopsy tissues and blood plasma RNA were also extracted using the miRNeasy Mini kit (Cat #217004, Qiagen, ON, Canada). We used 300–350 µL of plasma for miRNA and RNA extraction. 5mg of the flash-frozen biopsy tissues were used to extract RNA and miRNA, resulting in 500–600 ng of total RNA.23
cDNA Synthesis
Around 1–2 µg of RNA and 200 ng of miRNA were reverse transcribed into complementary DNA (cDNA) using the SuperScript cDNA reverse transcription kit (ThermoFisher Scientific, ON, Canada).
Quantitative Real-Time PCR (qRT-PCR)
Quantitative Real-Time polymerase chain reaction (qRT-PCR) uses cDNA, RNAse-free water, TaqMan Universal PCR Master Mix (ThermoFisher Scientific, ON, Canada), and gene-specific probes. To conduct qRT-PCR, an ubiquitous control gene, RPL5 (Hs303044958), the experimental YWHAB (Hs00793604) gene, pri-hsa-miR-526b (Hs03296227), and pri-hsa-miR-655 (Hs03304873) probes were used.
Mass-Spec Data
Using previously generated liquid chromatography-mass spectrometry (LC-MS) data,9 secretory protein expression of all isoforms within the 14-3-3 family of proteins was separated, enriched, and analyzed. Comparisons were made between the low miRNA MCF7-Parental and miRNA-overexpressed cell lines MCF7-miR526b and MCF7-miR655.
Western Immunoblotting
Total cellular protein was extracted by treating cells with 10X Cell Lysis Buffer (#9803, Cell Signaling Technology) and Protein Phosphatase Inhibitor (#58705, Cell Signaling Technology). Equal amounts of protein, ranging from 20µg to 40µg among replicates, were electrophoresed on a 10% polyacrylamide gel. After separation, protein samples were transferred onto a nitrocellulose membrane (Cytiva, Amersham, #10600006) and incubated in blocking solution (1% BSA in TBS), followed by overnight incubation in primary antibodies at 4°C (1:500 anti-14-3-3-beta, Santa Cruz Biotechnology, Cat#sc-25276; 1:1000 anti-alpha-tubulin, Applied Biological Materials, Cat#Y054861; 1:5000 anti-beta-actin, Santa Cruz Biotechnology, Cat#sc-47778; 1:2000 E-Cadherin, Cell Signalling Technology, Cat#3195S; 1:5000 Vimentin, Abcam, Cat#ab92547). After 12–20 hours of incubation, membranes were washed and then probed with secondary antibodies (1:10000 AzureSpectra 700 anti-mouse, 1:10000 AzureSpectra 800 anti-rabbit) for 1 hour. Membranes were imaged on the Sapphire Biomolecular Imager (Azure Biosystems, Dublin, CA, USA).
In-Cell Immunoblotting
Approximately 50,000 cells were seeded into a 96-well plate and grown to 80% confluency. Next, cells were fixed with 100% methanol for 15 minutes, then blocked with 1% BSA in PBS for 1 hour at room temperature. Following blocking, cells were incubated in primary antibodies (1:200 anti-YWHAB, 1:1000 anti-TUBA1, Santa Cruz Biotechnology, Dallas, TX, USA) overnight at 4°C, then incubated in secondary antibodies (1:5000 AzureSpectra 700 anti-mouse, 1:5000 AzureSpectra 800 anti-rabbit) for 1 hour at room temperature. The plate was imaged on the Biomolecular Imager and quantified with AzureSpotPro software.
Immunocytochemistry
Approximately 200,000 cells were seeded onto sterile coverslips in a 6-well plate and grown to 80% confluency. Fixation was done using 100% methanol in ice-cold for 10 minutes, and then the cells were blocked with 1% BSA in PBS for 1 hour at room temperature. The primary antibody (1:400 anti-14-3-3-beta, Santa Cruz Biotechnology) was incubated overnight at 4°C, followed by the secondary antibody (anti-m-IgGk BP-FITC, 1:1000, Cat# sc-516140, Santa Cruz Biotechnology) for 1 hour at room temperature followed by washing with PBS-T. Coverslips were mounted onto slides using Mounting Medium with DAPI (ab104139, Abcam, ON, Canada) and imaged on the Eclipse Ti2 microscope (Nikon, ON, Canada).
Knockdown (KD) of YWHAB
PolyPlus INTERFERin siRNA/miRNA transfections kit (VWR, ON, Canada) was used following the manufacturer’s protocol with a siRNA concentration of 1 nM. YWHAB siRNA (Ref# AM16708, Invitrogen, CA, USA) and scrambled siRNA (Ref# 9914G7, TX, USA) were used to knock down following manufacturer protocol. We observed an 80% reduction in YWHAB gene expression compared to scrambled after 24 hours of knockdown. All functional assays were conducted 24 hours post-knockdown.
Migration Assay
Cells were grown until 80–90% confluent, and then Mitomycin C (MMC) (Enzo Life Sciences, 10 ug/mL) was added for 2–3 hours. MMC is a cell proliferation inhibitor.24,25 After two hours, MMC was removed, and with a 0.1–200uL pipette tip, two vertical line scratches were made in each well. At this stage, media was removed, and PBS was used to wash the cells. Then, YWHAB siRNA and scrambled siRNA were used to knockdown the gene following manufacturer protocol. Images were taken at 2 hours intervals from 0–12 hours and at 24 hours.
Image Data Acquisition and Calculation
Images captured with a Nikon Eclipse Ti2 microscope. At 0 hours, picture locations were set using the NIS-Elements AR 5.42.01 for three different points along the scratch for each condition (CTRL, SCR, and KD). This program is saved, so next time, once the same plate or surface is added for image acquisition after the two hours, the program will automatically recognize all spots and capture pictures of the scratch wounds at 0, 2, 4, 6, 8, 10, 12, and 24 hours. Using NIS-Elements, the width of the wound was measured and analyzed. Three lines were drawn across the wound, and the mean of three measures was considered for analysis. The rate of wound healing was calculated using average distance (µm) for each time point. Subtracted the 0-hour distance by each interval distance, then divided by the 0-hour distance multiplied by 100%.
Proliferation Assay
Cells were grown in 96-well plates. Gene KD was conducted in the 96-well plate. After 24 hours post-KD, media with the siRNA cocktail was removed. Cell proliferation was measured using the CyQUANT NF Cell Proliferation Assay Kit (Ref#C35007, ThermoFisher Scientific, ON) following the manufacturer’s protocol. Cell proliferation rate was measured using a multi-mode TECAN Microplate Reader, using a DNA binding dye with 485 nm for excitation and 535 nm for emission. The data was taken four times from 30 minutes once the dye was added up to an hour.
Human Tissue
We followed Reporting Recommendations for Tumor Marker Prognostic Studies (REMARK) guidelines26 for tissue collection and reporting results.
Biopsy Tissue Samples
Frozen human breast tissue samples were collected from the Ontario Institute for Cancer Research (OICR) Tumour Bank, tumour (n=102) and adjacent non-cancerous tissues (n=19) (Supplementary Table 1). Most samples were recruited from females (n=99), and only a few were taken from males (n=3). Disease-free tissues are considered as control (n=19). We have n=76 ER-positive, n=65 PR-positive, n=22 HER2-positive samples, and only n=11 negative tumour samples. We have only a few n=7 stage I tumours, n=47 stage II, n=42 stage III and only a few n=6 stage IV tumours. As described above, sample processing, RNA extractions, experiments, and data analysis were conducted for plasma samples.5,6
Blood Plasma Samples
Frozen human plasma samples were retrieved from the London Tumour Biobank (LTB), managed by the London Regional Cancer Program (LRCP). The LRCP collects matched human breast biopsy tissues and plasma samples from participants with written consent.23 The non-cancerous patients were aged 52 to 87, and breast cancer patients aged 36 to 91. Within breast cancer patients, there is only one stage 0 (n=1), stage I (n=30), stage II (n=27), stage III (n=5), and no stage IV sample, unknown stage n=2. Samples were also stratified into hormone status: ER-positive (n=57), ER-negative (n=7), PR positive (n=54), PR negative (n=10), HER2 positive (n=14), HER2 negative (n=46), HER2 equivocal (n=4), and unknown status (n=1) (Supplementary Table 2).
Data Extracted from Databases: In silico Analysis
The Enrichr online database was used to identify transcription factors, resulting in a change in YWHAB expression.27 Predicted Targets of hsa-miR-526b and hsa-miR-655 were identified using TargetScanHuman V-8.0.28 YWHAB mRNA expression in breast cancer cell lines was obtained from the Gene Expression database of Normal and Tumor Tissues 2 (GENT2) database.29 Human breast cancer and healthy tissue data extracted from TCGA cBioPortal30 and Gene Expression Profiling Interactive Analysis 2 (GEPIA2).31 YWHAB immunohistochemistry and survival data for breast cancer patients and control tissue were accessed through the Human Protein Atlas (HPA).32 Liquid biopsy expression data for biomarker analysis was obtained from exoRBase.33
Receiver Operating Characteristic (ROC) Analysis
ROC analysis was used as the benchmark to evaluate YWHAB’s ability to differentiate two populations correctly: individuals with breast cancer and individuals in the control group. We used OICR and LTB samples for this analysis. We used benign blood plasma as a control for LTB samples and non-adjacent disease-free tissue as a control for OICR samples. For individual biomarker evaluation, RT-qPCR generated -∆Ct values for each sample representing the relative expression of the chosen marker. The data was analyzed using GraphPad Prism 10.4.1.627. When evaluating the combined effect of using two biomarkers (YWHAB along with pri-miR-526b or pri-miR-655), each sample was designated a predictive score through a binomial regression of the ∆Ct values for each of the two markers. The binomial regression was done using the IBM SPSS V.28.0 statistics package. Then, GraphPad Prism was used to generate ROC statistics using the predictive scores of each sample as described above.
Statistical Analysis
All statistical data were analysed using GraphPad Prism. T-tests were used to compare the mean of the two groups and the Pearson correlation coefficient for correlation analysis. Differences were calculated with the relevance of p<0.05 to determine statistical significance. Each data set was conducted with at least three biological replicates (N=3) and three experimental replicates.
Results
14-3-3 Protein Family Expression in MCF7-miR526b and MCF7-miR655 Secretomes
Here, we show all members of the 14-3-3 protein family are upregulated in the secretions of both MCF7-miR-526b and MCF7-miR-655 breast cancer cell secretome, in comparison to the secretome of parental MCF7 cells (Figure 1A). A data curation pipeline was applied, consisting of a ± 1.5 log2 threshold, exclusion of proteins not found in the breast proteome, and secretome prediction methods.9 We previously reported that two members of the 14-3-3 family, YWHAB (14-3-3 Beta) and SFN (14-3-3 Sigma), are high in miRNA-high cell secretions.9 However, we did not validate the function of either of these markers in breast cancer. Here, we investigate the roles of YWHAB in breast cancer and test its biomarker potential.
In silico Analysis
The Regulation of YWHAB by miR-526b and miR-655
YWHAB protein is upregulated in the secretome of miR-overexpressing cells. We conducted a combined analysis of predicted miRNA target genes, identified with the TargetScan database of predicted microRNA targets,28 and YWHAB transcription factors (TFs), identified via the interactive gene enrichment database Enrichr.27 This identified 74 TFs that regulate YWHAB expression, and several genes targeted by miR-526b and miR-655. By overlapping the lists, we identified eight TFs targeted by miR-526b and miR-655, of which the majority are negative regulators (three TFs, KLF10, ME1S2, and NANOG are negative regulators of YWHAB and two TFs, FOXP1 and MYC acts both as negative and positive regulators of YWHAB and three positive regulator TFs, MAF, ZNF148 and SP3, upregulates YWHAB). We predict that negative regulator TFs of YWHAB are targeted by miR-526b and miR-655, resulting in the upregulation of YWHAB (Figure 1B).
YWHAB Gene Expression in Breast Cancer Cell Lines
YWHAB gene expression in various breast cancer cell lines was analyzed using the Gene Expression database of Normal and Tumor Tissues 2 (GENT2) database29 (Figure 1C). The cell lines were categorized by breast cancer subtype: luminal A (MCF7 and T47D), human epidermal growth factor receptor 2 (HER2) enriched (SKBR3), and triple-negative (Hs578T and MDA-MB-231). We assessed variation in YWHAB expression among the breast cancer cell lines relative to the immortalized breast epithelial cell line, MCF10A. Each tumour cell line showed an upregulation of YWHAB, significantly high in T47D and MDA-MB-231 and low expression in MCF7.
YWHAB mRNA expression in Whole Cell and Cell-Free Extracted RNA
We reported for the first time the presence of YWHAB in the cell secretome.9 Here we validated the YWHAB expression in stable miR-526b and miR-655-transfected breast cancer cell lines: MCF7-miR526b, MCF7-miR655, and SKBR3-miR526b, as well as in naturally miRNA-overexpressing ER-positive MCF7-COX2 and triple-negative Hs578T cell lines using quantitative real-time polymerase chain reaction (qRT-PCR) (Figure 2A and B). We observed significantly high expression of YWHAB in all miRNA-high whole-cell lysates relative to MCF7-Mock and SKBR3-Mock cell lines (Figure 2A). In cell-free secretions, YWHAB mRNA expression was high in all cell line secretions, with significant upregulation in MCF7-miR526b, MCF7-miR655, and MCF7-COX2, compared to the respective MCF7-Mock cell line (Figure 2B).
Since we discovered YWHAB in the secretome of cells with high expression levels of miR-526b and miR-655, we wanted to investigate the correlation between miRNA and YWHAB. We measured the primary RNA of microRNA (pri-miRNAs) pri-miR-526b and pri-miR-655 expression in total cellular RNA and cell-free secretions via qRT-PCR. Both pri-miR-526b (Figure 2C and D) and pri-miR-655 (Figure 2E and F) were upregulated in the total RNA and cell-free media. These results indicate that YWHAB can be found in the cell-free RNA, increasing their potential to serve as a biomarker. YWHAB might play a role in miRNA-induced functions in TME regulation.
YWHAB Protein Expression
YWHAB gene expression demonstrated significant upregulation in all miRNA-high cell lines compared to miRNA low-expressing cells. Next, we measured the protein expression of YWHAB using a Western blot (full blot provided in Supplementary Figure 1). In ER-positive miRNA-high cell lines, MCF7-miR526b, MCF7-miR655, and MCF7-COX2 displayed higher expression of YWHAB protein compared to miRNA-low, COX2-low MCF7-Mock cells (Figure 3A and B). In the HER2-enriched cell line, SKBR3-miR526 showed higher expression than miRNA low-expressing SKBR-Mock (Figure 3A and B). The naturally miRNA-high triple-negative breast cancer cell line, Hs578T, also showed a significant increase in YWHAB protein compared to MCF7-Mock (Figure 3A and B). Further protein expression analyses were done using in-cell Western immunoblotting, which re-confirmed Western blot results, where miRNA-high cell lines, MCF7-miR526b, MCF7-miR655, and MCF7-COX2 cells showed upregulation of YWHAB protein expression compared to MCF7-Mock (Figure 3C). To visualize the localization of YWHAB within the cells, we conducted an immunocytochemistry assay. Predominantly, YWHAB protein seems to be expressed in the cytosol, and we observed a higher intensity of YWHAB in MCF7-COX2 cytosol compared to MCF7-Mock (Figure 3D and E). So, cells with high miR-526b, miR-655 and COX2 expression also show high expression of YWHAB protein.
Knockdown of YWHAB and Measure Changes in Cellular Phenotypes
Both miR-526b and miR-655 enhance breast cancer cell migration, invasion, and proliferation.5,6 Here, we observed that all miRNA overexpressing and triple-negative cell lines showed high expression of YWHAB. To test YWHAB’s contribution to aggressive breast cancer phenotypes, we knocked down (KD) YWHAB in all these cell lines using siRNA and a lipofectamine transfection method. The luminal A cell lines, including MCF7-Mock, MCF7-miR526b, MCF7-miR655, and MCF7-COX2, showed around 80%, 63%, 67%, and 55% knockdown, respectively, compared to the scramble (control) knockdown (Figure 4A) at the mRNA level. MCF7-Mock, which had comparatively low YWHAB expression, showed the highest knockdown of gene expression, reduced by almost 80%. The HER2-enriched cell lines, SKBR3-Mock and SKBR3-miR526b showed around 22% and 95% knockdown, respectively, compared to scramble KD (Figure 4B), and there was an average of 70% knockdown in the triple-negative cell line, Hs578T (Figure 4C).
To verify the knockdown efficiency of YWHAB at the protein level, Western blots of Luminal A breast cancer cells MCF7-miR526b, MCF7-miR655 and MCF7-Cox2 (Figure 4D), MCF7-Mock (Figure 4E); HER2-enriched cells SKBR3-Mock, SKBR3-miR526b and triple-negative breast cancer Hs578T (Figure 4E) were conducted, and relative protein expression was measured for YWHAB knockdown (KD) compared to Scrambled (SCR) KD (Figure 4F). Complete Western blots are provided in Supplementary Figures 2 and 3. At the protein level, YWHAB was significantly reduced (40–50%) in MCF7-miR526b, MCF7-miR655, MCF7-COX2, and Hs578T cells (Figure 4D–F). The HER2-enriched cell lines, SKBR3-Mock and SKBR3-miR526b demonstrated 10% and 15% knockdown, respectively, compared to SCR (Figure 4E and F). Further protein expression was validated with immunocytochemistry (ICC) of miRNA-high MCF7-cell lines (Figure 4G and H). ICC data also showed a significant reduction in YWHAB intensity after knockdown in all three cell lines; quantification was done compared to SCR KD for the respective cell lines (Figure 4H).
YWHAB Functional Assays
Cellular Migration
To investigate the role of YWHAB in cell migration, we conducted wound-healing cellular migration assays.7,8 To confirm the involvement of YWHAB in cell migration, we inhibited cell proliferation by pre-treating cells with MMC for two hours before we made the scratch. Changes in wound healing were recorded every 2 hours interval until 12 hours and at 24 hours in untreated control (CTRL) cells, scramble-KD cells and YWHAB-KD cells in MCF7-Mock (Figure 5A and B), MCF7-miR526b (Figure 5C and D), MCF7-miR655 (Figure 5E and F), MCF7-COX2 (Figure 5G and H), SKBR3-Mock (Figure 5I and J), SKBR-miR526b (Figure 5K and L), Hs578T (Figure 5M and N). The results showed inhibition of cell migration in all miRNA-overexpressed and Hs578T cells compared to scramble KD cells after YWHAB knockdown. This indicates the involvement of YWHAB in breast cancer cell migration. In untreated CTRL and scramble-KD cells, the wound was significantly healed by 24 hours in all cell lines, but after KD of YWHAB, this was significantly inhibited (Figure 5D, F, H, J, L and N). There was little change in migration in MCF7-Mock and SKBR3-Mock cells before and after YWHAB abrogation (Figure 5B–J). This further indicates that YWHAB might regulate miRNA function in aggressive breast cancer, such as migration.
Cell Proliferation
The 14-3-3 complex is a significant regulator of cell division. Cell proliferation was measured before and after YWHAB-KD in all miRNA-overexpressed cell lines. Each cell line showed significant downregulation of cellular proliferation in the case of YWHAB-KD compared to siRNA-scramble (SCR) (Figure 6A). This indicates that YWHAB is linked to cell cycle regulation.
EMT Marker Expression
Building on our observation that abrogation of YWHAB in breast cancer cells impedes cellular migration, indicating high YWHAB expression might promote mesenchymal phenotype, stimulating epithelial to mesenchymal (EMT) transition. Next, we compared the expression of EMT markers (E-Cadherin; CDH1, TWIST, Vimentin; VIM) in all miRNA-high cells (Figure 6B). In the YWHAB-KD cells, we observed an upregulation of epithelial marker CDH1 in all ER/PR positive cell lines, MCF7-Mock (Figure 6B), miRNA overexpressed cells MCF7-miR-526b and MCF7-miR-655 (Figures 6C and D) and MCF7-COX2 cells (Figure 6E), and triple-negative cells Hs578T (Figure 6H) compared to scramble-KD and a significant downregulation of all markers in HER2-enriched cells SKBR-Mock (Figure 6F), and SKBR3-miR-526b (Figure 6G). Another compelling finding is that all YWHAB-KD cell lines showed downregulation of mesenchymal markers Vimentin (Vim) and TWIST in all aggressive cell lines. We investigated the protein expression of EMT markers (E-cadherin and VIM) in all cell lines after YWHAB KD (Figure 6I and J). The full Western blot is provided in Supplementary Figures 2 and 3. In the YWHAB-KD cells, there was an upregulation of E-cadherin and downregulation of VIM in the ER/PR+ cell lines, MCF7-Mock (Figure 6K), MCF7-miR526b (Figure 6L), MCF7-miR655 (Figure 6M), and MCF7-COX2 cells (Figure 6N). In the HER2-enriched cell line, SKBR3-Mock, there was a marginal increase in E-cadherin post-YWHAB-KD and a significant decrease in VIM (Figure 6O). In SKBR3-miR526 (Figure 6P), the protein expression of E-cadherin and VIM remained the same. In the triple negative cell line, Hs578T, there was significantly lower E-cadherin expression as it is an aggressive breast cancer cell line (Figure 6J and Q) and a decrease in VIM protein expression in YHWAB-KD cells compared to scramble (SCR) KD. These findings imply that knocking down YWHAB reverts the cell to an epithelial phenotype. Hence, YWHAB plays a key role in cell migration and EMT.
Translational Validation
YWHAB Gene and Protein Expression in Human Tissue: In silico Analysis
We gathered immunohistochemistry data from breast tumours and control samples through the Human Protein Atlas (HPA).32 The cancerous samples were obtained from women ages 27 to 87 who were diagnosed with breast cancer comprising ductal and lobular carcinomas. Breast cancer and normal tissue samples were stained with three YWHAB antibodies (HPA007925, HPA11212, and CAB003759) (Figure 7A). Among the three non-cancerous control tissues, most showed low to medium YWHAB staining. In contrast, the majority of breast tumour tissue samples (72.22%, or 26 out of 36) exhibited medium YWHAB staining, while nine samples (25%) had high-intensity staining. This suggests that cancer tissues show increased YWHAB expression protein.
The expression of the YWHAB gene was examined using data from the TCGA PanCancer Atlas, which included breast cancer tissue samples (n=1085) as well as non-cancerous tissue samples (n=291). The mRNA expression level of YWHAB was notably higher in breast tumour samples compared to normal tissues (Figure 7B). Subsequently, the breast tumour samples were categorized by tumour stage. Each stage exhibited log2(TPM+1) median values of 7.51 or above, with stage IV reaching a higher value of 7.7 (Supplementary Figure 4). These findings were not statistically significant, suggesting that variations in YWHAB expression within our sample set were not influenced by the tumour stage (Figure 7B).
 |
Figure 7 Immunohistochemistry and mRNA expression of YWHAB in human tissues. (A) Immunocytochemistry data was extracted from the HPA database. Control tissues showed low expression of YWHAB. Breast cancer tissue showed mostly medium to high expression [light (n=1/36), medium (n=26/36), and high (n=9/36)]. Image credit: Human Protein Atlas, www.proteinatlas.org.32 Image available at the following URL; “Control”: v24.images.proteinatlas.org/11212/27931_B_1_4.jpg “Tumor Low”: v24.images.proteinatlas.org/11212/27928_A_5_5.jpg “Tumor Medium”: v24.images.proteinatlas.org/3759/10979_A_6_6.jpg “Tumor High”: v24.images.proteinatlas.org/3759/10979_A_6_7.jpg (B) YWHAB gene expression in breast cancer tissue extracted from GEPIA2 database. Breast cancer tumour samples are shown with a red box plot (n=1085), and paired non-cancerous samples are presented in a grey box plot (n=291). Each black dot represents one sample. The bold black line shows the median value. Quartile range lines are shown with coloured boxes. Quartile minimum and maximum without outliers are shown as the lines above and below the coloured box. P-value cut-off set at 0.01 (99% confidence level). * p-value < 0.05. (C) Data extracted from cBioPortal. YWHAB mRNA expression correlated with miR526b-cluster expression (left panel) and miR655-cluster expression (right panel) in various subtypes of tumours. A significant but moderate correlation (R2 values) was observed in luminal A tumours. Between YWHAB and miR526b-cluster (R2 0.0712, p = 0.001) and between YWHAB and miR655-cluster (R2 0.0283, p = 0.044). |
Correlation of YWHAB and miR-Clusters Expression in Breast Cancer Tissues
To assess the relationship between miRNA and YWHAB mRNA expression across various breast cancer subtypes, we extracted the expression levels of the miR-526b and miR-655 clusters, alongside YWHAB expression, from breast tissue samples obtained through cBioPortal.30 We analyzed data from 283 matched tumour tissue samples for these miRNA clusters and YWHAB (Figure 7C). The Pearson correlation coefficient was calculated to evaluate the relationship between miRNA cluster expression and YWHAB mRNA levels in non-stratified tumour samples, the luminal A subtype, and other subtypes combined due to their limited sample size. In luminal A subtype tumours, YWHAB expression exhibited a very weak correlation with the miR-526b and miR-655 clusters in luminal A subtype tumours. No correlation was observed between the miRNA clusters and YWHAB expression in other stratified groups.
Validation of YWHAB Expression in OICR Tumour Bank Tissues
To confirm YWHAB gene expression in breast cancer tissue, we evaluated YWHAB, miR-526b, and miR-655 expressions in both non-cancerous (control) tissues and breast tumour samples obtained from the Ontario Institute for Cancer Research (OICR), with sample demographics detailed in Supplementary Table 1. A flow diagram illustrating the samples included or excluded during the analysis is shown in Figure 8. We observed an upregulation of YWHAB in breast cancer samples compared to control tissues (Figure 9A). Among stratified tumour samples, significant upregulation was observed in all stages: stage I, n=7 (6.86%); stage II, n=47 (46.1%); stage III, n=42 (41.2%); and stage IV, n=6 (5.9%), compared to the control group (n=19) (Figure 9B). Nonetheless, ANOVA did not reveal significant changes in YWHAB expression. When breast tumour samples were categorized by hormonal subtype, a significant difference was observed for all subtypes, except luminal B, compared to control (Figure 9C). Thus, YWHAB expression is elevated in all cancer stages and hormonal subtypes, suggesting its role as an important cancer marker.
 |
Figure 8 The flow chart of the Ontario Institute for Cancer Research (OICR) and London Tumour Biobank (LTB) samples inclusion and exclusion criteria. |
Measure the Correlation Between YWHAB and miRNA Expression in OICR Samples
Since we found that miRNA clusters are positively correlated with YWHAB expression, we further validated this observation using OICR samples. We measured the Pearson correlation coefficient between YWHAB and miR-526b and miR-655 in breast tumour tissues, generating correlation coefficients using ΔCt values (Figure 9D–E). We did not find any significant correlation between YWHAB and miRNA expression. This could be due to the limited number of tissues showing expression of all three markers in OICR samples.
Validation of YWHAB Gene Expression in BRCA Blood Plasma
In silico Validation Using Exobase Samples
Through exoRBase,33 a repository of RNASeq data from different bodily fluids, we analyzed YWHAB mRNA expression in the blood plasma, as reported in exoRBase 2.0, we used healthy participants (n=118), benign samples (n=130), and breast cancer samples (n=140) data. We observed a significant difference in YWHAB expression in breast cancer blood samples compared to healthy and benign samples. The median expression of YWHAB in benign blood samples was marginally low compared to healthy samples; however, very significant upregulation was recorded in breast tumour blood samples compared to both healthy and benign samples (Figure 10A).
 |
Figure 10 YWHAB expression in human blood plasma Exobase and LTB. (A) Data was extracted from Exobase; RNA was extracted from extracellular vesicles in human blood samples. The horizontal bar represents the median value of each sample set. Dots represent samples that fall outside the standard error of mean bars but are still included in the sample set. (B-D) Validation in London Tumour Biobank plasma samples. YWHAB ΔCt expression normalized against RPL5 (control gene). (B) Non-cancerous control plasma (n=19) against breast cancer tumour plasma samples (n=65). (C) Non-cancerous control plasma (n=19) compared to breast stage I (n=27), stage II (n=22) and stage III.4 (D) Non-cancerous control plasma (n=19) compared to breast cancer subtypes: luminal A (n=38), luminal B (n=9), HER2-enriched (n=4), and triple-negative (n=3). YWHAB expression significantly differs in all datasets in various tumour stages and types. * p-value < 0.05. ** p-value < 0.005. *** p-value < 0.0001. |
In situ Validation Using London Tumour Biobank Blood Plasma Samples
YWHAB expression was validated in breast cancer patient blood plasma samples (n=65) and control plasma samples (n=19) collected from the London Tumour Biobank, ON, Canada (demographic data in Supplementary Table 2). A flow diagram of samples included or excluded during analysis is provided in Figure 8.
We observed an increase in YWHAB gene expression in malignant blood plasma samples compared to controls, as indicated by a lower ΔCt value for tumours (Figure 10B), although this finding did not reach statistical significance. Subsequently, we categorized samples according to tumour stages and hormonal subtypes: luminal A, luminal B, HER2-enriched, and triple-negative. When stratified the plasma samples by tumour stage, a trend of increased YWHAB expression was observed across all cancer stages compared to control samples; however, this was not statistically significant. We did observe a notable increase in YWHAB expression in stage I (Figure 10C), but this was not significant either. Similarly, there was no significant difference in YWHAB expression among molecular subtypes, including luminal A, luminal B, and HER2-positive samples compared to the control group (Figure 10D). Although the substantial TCGA dataset revealed significant YWHAB upregulation in blood plasma (Figure 10A), we found an upregulation trend in stage I and in luminal A, B, and HER2-positive tumors, though these findings are statistically inconclusive. This may be attributed to the small size of the LTB samples and variations within the PCR data, which necessitates further validation. Importantly, this observation requires confirmation in a larger sample size.
Testing Biomarker Potential of YWHAB
In situ Validation in OICR Biopsy Samples
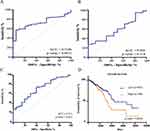
To test the effectiveness of YWHAB as a biomarker, we generated a receiver operating characteristic (ROC) curve using the OICR biopsy tissues (cancer samples n=102, normal tissue n=19) (Figure 11A). An AUC (area under the curve) of approximately 0.70 or higher indicates an effective marker for detecting breast cancer. YWHAB showed a statistically significant AUC of 0.734 in OICR tissues, suggesting it has potential as a breast cancer tumour marker.
In situ Validation in LTB Blood Plasma Samples
Next, we generated a ROC curve to evaluate the blood biomarker potential of YWHAB using patient blood plasma samples from the London Tumour Biobank (malignant plasma n=63, control plasma n=19) (Figure 11B). As a blood biomarker, YWHAB exhibited an AUC of 0.582, which was insignificant. Hence, YWHAB is not a sensitive blood biomarker for breast cancer. Previous studies have shown that pri-miR-526b is a sensitive blood biomarker for early breast cancer detection.23 We performed a combined biomarker analysis of YWHAB and pri-miR-526b, resulting in an AUC of 0.711, which is statistically significant (Figure 11C). This suggests that YWHAB might be considered as a blood biomarker in patients with elevated pri-miR-526b levels expression.
YWHAB Expression and BRCA Patient Survival: In silico Analysis
To test if high YWHAB expression correlates with breast cancer patient survival, 1052 breast tumour samples from The Cancer Genome Atlas (TCGA) were analyzed for mRNA expression. The 5-year survival rate was calculated using the Kaplan-Meier plot. With high YWHAB gene expression (n=384), we observed a significant decrease in patient overall survival compared to low YWHAB expression (n=691) (Figure 11D). Breast cancer patients with high YWHAB expression had a 5-year survival percent at 75%, whereas those with low expression showed a survival rate of 85%. Since high expression of YWHAB is linked with poor breast cancer patient survival, YWHAB can serve as a prognostic biomarker for breast cancer.
Discussion
In this study, we explored the roles of YWHAB in breast cancer. We discovered YWHAB in miR-526b and miR-655 overexpressed tumour cell secretome. YWHAB expression is high at total RNA, secretory RNA, and protein levels in miRNA-overexpressed cell lines, indicating a correlation between miR-526b and miR-655 with YWHAB in breast cancer. Two other studies found similar effects with YWHAB expression in other tumour models. For instance, overexpression of YWHAB was correlated with increasing grade and stage of tumour in hepatocellular carcinoma.34 In another study with lung cancer, YWHAB was shown as a downstream target of miR-129-5p, which was negatively correlated with the YWHAB expression in patient tissue and serum samples, leading to poor patient survival.20 We also found that YWHAB is overexpressed in triple-negative and HER2-positive breast cancer. However, the role of YWHAB in breast cancer progression and metastasis remained poorly explored.
YWHAB, a member of the 14-3-3 protein family, mediates signal transduction by binding to phosphoserine-containing proteins. It is ubiquitously expressed in cell cytosol and is involved in cell-cycle regulation. With immunocytochemistry, we also found that YWHAB is expressed in all tumour cells; however, the intensity of YWHAB was higher in miRNA-overexpressed cells. We showed the involvement of YWHAB in breast cancer cell proliferation and migration and that knocking down YWHAB in aggressive breast tumour cells abrogated these metastatic phenotypes. Previous reports indicated that overexpression of YWHAB in cervical cancer cells,15 gastric cancer cells,21 and breast cancer cells22 promotes cell migration. Also, the 14-3-3 family is known to be involved in EMT in cancer.35 In this current study, we investigated the direct roles of YWHAB in EMT alteration in breast cancer. YWHAB knockdown in luminal A, HER-2 positive and triple-negative breast cancer cell lines showed a downregulation of mesenchymal marker Vimentin and an upregulation of epithelial marker E-Cadherin both at RNA and protein levels and mesenchymal marker TWIST at the RNA level, strongly supporting the involvement of YWHAB in EMT regulation in breast cancer.
We observed the involvement of YWHAB in breast cancer cell proliferation. Here, we showed the novel roles of YWHAB in breast cancer and the knockdown of YWHAB-abrogated cell proliferation, especially in miRNA-overexpressing cell lines. The involvement of YWHAB in cell proliferation could be further regulated by miR-526b and miR-655. We previously showed that miRNA526b and miR-655 enhance cell proliferation, migration, and cancer stem cell population via PI3K/AKT signalling.5,6 So, YWHAB may enhance cell proliferation in collaboration with miR-526b and miR-655. Others support this observation. SMARCA5 is a helicase with intrinsic ATP-dependent nucleosome remodelling activity; the catalytic subunit of this protein directly participates in DNA replication. A cervical cancer study showed that knockdown of SMARCA5 caused inhibition of binding SND1 to YWHAB.15 In a rat liver cancer model, YWHAB was shown to be involved in cell proliferation.18 Similarly, in a glioma tumour model, YWHAB expression was linked to tumour cell proliferation.19 As observed by Hua et al, circulating miRNA and YWHAB collaborate to promote cell proliferation and metastasis.21 This was also reflected in our findings, as we observed an increase of miRNA and YWHAB transcripts in the secretions of aggressive breast cancer cells.
In addition, we discovered YWHAB in the cell secretion of miR-526b and miR-655 overexpressed breast tumour cells at both mRNA and protein levels. Here, we also observed that the knockdown of YWHAB in all miRNA-high expressing cell lines reverts miRNA-induced aggressive breast cancer phenotypes such as EMT. It is critical to note that YWHAB knockdown significantly reduced mesenchymal marker expression and upregulated the epithelial marker expression in the aggressive miRNA overexpressed and triple-negative cell lines. YWHAB might be a key player in oncogenic miR-526b and miR-655-induced functions. We identified transcription factors (TF) that are negative regulators of YWHAB, such as KLF10, MEIS2, NANOG, MYC, and FOXP1, which could be the target of miRNAs. MiRNA abrogates the expression of negative regulators; hence, YWHAB expression was high in miRNA-overexpressed cells. This is an in silico analysis of miRNA regulation, which needs further validation.
We further explored any correlation between miRNAs and YWHAB expression using breast cancer tissue. Expression of YWHAB is upregulated in breast cancer biopsy tumours and blood plasma compared to healthy or disease-free control tissues. A high expression of YWHAB is linked with poor survival of breast cancer patients. However, a pairwise comparison between tumour stages did not find a significant difference, indicating that YWHAB is the marker required for disease onset, and its expression remains high during disease progression. YWHAB is significantly upregulated in all hormone subtypes of the tumour biopsies, further supporting that high expression of YWHAB is essential for disease onset and progression. However, the prognostic biomarker roles of YWHAB need further investigation; we found high and significant expression in breast cancer patients’ blood plasma (Exobase data), but this was not significant in LTB samples.
We also showed that YWHAB is a highly sensitive tumour biomarker, and YWHAB expression is associated with poor breast cancer patient survival. In tumour tissues, we found a weak correlation between miR-526b and miR-655 clusters with YWHAB expression only in luminal A tumours in the multi-ethnic larger TCGA tissue dataset. Previously, we reported a significant positive correlation between miR-526b and miR-655 expression in OICR tumour bank samples.6 Although a weak positive correlation was observed between miRNA and YWHAB expression in the OICR tumour bank samples, this was insignificant. So, YWHAB expression is not directly correlated with miRNA expression in biopsy tissues.
A large number of single blood-based biomarkers are reported, including the most promising soluble proteins: Human Epidermal Growth Factor Receptor 2 (HER2), Cancer Antigen 15–3 (CA 15–3), Carcinoembryonic Antigen (CEA), and MUC1. In addition, circulating tumour cells (CTCs) and miRNAs are reported as blood biomarkers.36 Since YWHAB was detected in the miRNA high tumour secretome, we conducted a blood biomarker analysis. Next, we explored the blood biomarker potential of YWHAB using breast cancer patient blood plasma. Previously, we have shown that pri-miR-526 and pri-miR-655 were all upregulated in breast cancer plasma samples relative to control plasma samples, and pri-miR-526b is a sensitive blood biomarker for breast cancer early detection.23 The potential of YWHAB as a blood biomarker was confirmed using a larger dataset from exoRBase 2.0, which indicated a significant increase in YWHAB levels in the blood plasma of breast cancer patients from a diverse multiethnic population. While we validated this finding with plasma samples from the London Tumour Biobank, YWHAB alone showed limited sensitivity as a blood biomarker for breast cancer. Interestingly, we found that when combined with pri-miR-526b, which is already known to be a sensitive blood biomarker for early breast cancer detection.23 However, the sensitivity of the YWHAB and pri-miR-526b combination as a blood biomarker requires validation with a larger dataset. High YWHAB expression is associated with poorer survival rates in breast cancer patients, suggesting that YWHAB functions as an oncogenic tumor marker. Further research on YWHAB is essential to understand its regulation by miRNAs and to establish YWHAB as a potential therapeutic target for breast cancer.
Conclusion
We discovered a novel secretory protein, YWHAB, in miR-526b- and miR-655-overexpressed breast cancer cell secretions. YWHAB regulates cell migration and proliferation, and high YWHAB expression is associated with poor breast cancer patient survival; hence, it is an excellent therapeutic target to abrogate aggressive breast cancer phenotypes. YWHAB is a sensitive tumour marker that differentiates tumours from non-tumour samples. Combined with pri-miR-526b, YWHAB can serve as an RNA-based blood biomarker for breast cancer detection.
Clinical Significance
YWHAB can serve as a sensitive tumour biomarker that differentiates cancerous tissue from non-cancerous tissue. The combination of YWHAB mRNA and pri-miR-526b is a sensitive blood biomarker capable of detecting breast cancer within the bloodstream. This advancement may facilitate the development of RNA-based blood tests for breast cancer. Implementing a blood test to detect breast cancer or monitor disease progression holds significant clinical implications and will directly benefit patients suffering from the disease.
Data Sharing Statement
All data generated in this study are available within the article, its supplemental information and from the corresponding author MM upon reasonable request.
Ethics approval and consent of participants
This study is approved by the Brandon University Ethical Approval Committee (approval # 23056) and the Brandon University Biosafety Committee (approval # 2020-BIO-02). The Ontario Institute for Cancer Research and London Tumour Biobank obtained informed consent from each subject before collecting samples from participants. Our study complies with the Declaration of Helsinki.
Acknowledgments
We want to thank Riley Feser for helping us analyze cell secretome data and sincerely thank all participants in this study. The authors also thank Antoni Klonowski for assisting us with migration image capture. We appreciate the generosity of Prof. Peeyush K Lala and Prof. Muriel Brackstone for sharing RNA samples of breast tissue and blood plasma samples from the Ontario Institute for Cancer Research (OICR) in Ontario and the London Tumour Biobank (LTB) in London, Ontario, respectively.
Funding
This work is supported by Breast Cancer Canada, the Lotte and John Hecht Memorial Foundation, and the Natural Sciences and Engineering Research Council of Canada (NSERC) Discovery Grant to M.M. It is also supported by the Canada Research Chair Program (CRCP), Canada Foundation for Innovation (CFI), and Research Manitoba Matching fundings to M.M. L.W. received an NSERC-USRA award, and B.N. and R.M.O. both received Research Manitoba MSc scholarships and the CIHR MSc scholarships.
Disclosure
The authors declare no conflict of interest.
This paper has been uploaded to ResearchSquare as a preprint: https://doi.org/10.21203/rs.3.rs-4139025/v1
References
1. Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Canadian Cancer Society: breast cancer statistics. 2022. Available from: https://cancer.ca/en/cancer-information/cancer-types/breast/statistics.
3. Ebell MH, Thai TN, Royalty KJ. Cancer screening recommendations: an international comparison of high-income countries. Public Health Rev. 2018;39:7. doi:10.1186/s40985-018-0080-0
4. American Cancer Society: limitations of mammograms. 2022. Available from: https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/mammograms/limitations-of-mammograms.html#:~:text=False%2Dpositive%20results%20are%20more,positive%20finding%20at%20some%20point.
5. Majumder M, Landman E, Liu L, Hess D, Lala PK. COX-2 elevates oncogenic miR-526b in breast cancer by EP4 activation. Mol Cancer Res. 2015;13(6):1022–1033. doi:10.1158/1541-7786.MCR-14-0543
6. Majumder M, Dunn L, Liu L, et al. COX-2 induces oncogenic micro RNA miR-655 in human breast cancer. Sci Rep. 2018;8(1):327. doi:10.1038/s41598-017-18612-3
7. Hunter S, Nault B, Ugwuagbo KC, Maiti S, Majumder M. MiR-526b and MiR-655 promote tumour associated angiogenesis and lymphangiogenesis in breast cancer. Cancers. 2019;11(7):938. doi:10.3390/cancers11070938
8. Shin B, Feser R, Nault B, et al. miR-526b and miR-655 induce oxidative stress in breast cancer. Int J Mol Sci. 2019;20(16):4039. doi:10.3390/ijms20164039
9. Feser R, Opperman RM, Nault B, Maiti S, Chen VC, Majumder M. Breast cancer cell secretome analysis to decipher miRNA regulating the tumour microenvironment and discover potential biomarkers. Heliyon. 2023;9(4):e15421. doi:10.1016/j.heliyon.2023.e15421
10. van Hemert MJ, Steensma HY, van Heusden GP, van Hemert MJ. 14-3-3 proteins: key regulators of cell division, signalling and apoptosis. Bioessays. 2001;23(10):936–946. doi:10.1002/bies.1134
11. Foote M, Zhou Y. 14-3-3 proteins in neurological disorders. Int J Biochem Mol Biol. 2012;3(2):152–164.
12. Jang SW, Liu X, Fu H, et al. Interaction of Akt-phosphorylated SRPK2 with 14-3-3 mediates cell cycle and cell death in neurons. J Biol Chem. 2009;284(36):24512–24525. doi:10.1074/jbc.M109.026237
13. Aitken A. 14-3-3 proteins: a historic overview. Semin Cancer Biol. 2006;16(3):162–172. doi:10.1016/j.semcancer.2006.03.005
14. Wilker E, Yaffe MB. 14-3-3 Proteins—a focus on cancer and human disease. J Mol Cell Cardiol. 2004;37(3):633–642. doi:10.1016/j.yjmcc.2004.04.015
15. Zhang X, Zhang Q, Zhang K, Wang F, Qiao X, Cui J. Circ SMARCA5 inhibited tumor metastasis by interacting with SND1 and downregulating the YWHAB gene in cervical cancer. Cell Transplant. 2021;30:963689720983786. doi:10.1177/0963689720983786
16. Ma Y, Li YF, Wang T, Pang R, Xue YW, Zhao SP. Identification of proteins associated with lymph node metastasis of gastric cancer. J Cancer Res Clin Oncol. 2014;140(10):1739–1749. doi:10.1007/s00432-014-1679-2
17. Tseng CW, Yang JC, Chen CN, et al. Identification of 14-3-3beta in human gastric cancer cells and its potency as a diagnostic and prognostic biomarker. Proteomics. 2011;11(12):2423–2439. doi:10.1002/pmic.201000449
18. Zhang Y, Li M, Wei L, et al. Differential protein expression in perfusates from metastasized rat livers. Proteome Sci. 2013;11(1):37. doi:10.1186/1477-5956-11-37
19. Kang CM, Bai HL, Li XH, et al. The binding of lncRNA RP11-732M18.3 with 14-3-3 beta/alpha accelerates p21 degradation and promotes glioma growth. EBioMedicine. 2019;45:58–69. doi:10.1016/j.ebiom.2019.06.002
20. Xu C, Du Z, Ren S, Liang X, Li H. MiR-129-5p sensitization of lung cancer cells to etoposide-induced apoptosis by reducing YWHAB. J Cancer. 2020;11(4):858–866. doi:10.7150/jca.35410
21. Hua Y, Wang H, Wang H, et al. Circular RNA Circ_0006282 promotes cell proliferation and metastasis in gastric cancer by regulating MicroRNA-144-5p/Tyrosine 3-Monooxygenase/Tryptophan 5-monooxygenase activation protein beta axis. Cancer Manag Res. 2021;13:815–827. doi:10.2147/CMAR.S283952
22. Zhu QN, Renaud H, Guo Y. Bioinformatics-based identification of miR-542-5p as a predictive biomarker in breast cancer therapy. Hereditas. 2018;155:17. doi:10.1186/s41065-018-0055-7
23. Majumder M, Ugwuagbo KC, Maiti S, Lala PK, Brackstone M. Pri-miR526b and Pri-miR655 are potential blood biomarkers for breast cancer. Cancers. 2021;13(15). doi:10.3390/cancers13153838
24. Glenn HL, Messner J, Meldrum DR. A simple non-perturbing cell migration assay insensitive to proliferation effects. Sci Rep. 2016;6(1):31694. doi:10.1038/srep31694
25. Yang X, Jun W, Shui-Long G, et al. miR-21 promotes keratinocyte migration and re-epithelialization during wound healing. Int J Biol Sci. 2011;7(5):685. doi:10.7150/ijbs.7.685
26. Sauerbrei W, Taube SE, McShane LM, Cavenagh MM, Altman DG. Reporting recommendations for tumor marker prognostic studies (REMARK): an abridged explanation and elaboration. J Natl Cancer Inst. 2018;110(8):803–811. doi:10.1093/jnci/djy088
27. Chen EY, Tan CM, Kou Y, et al. Enrichr: interactive and collaborative HTML5 gene list enrichment analysis tool. BMC Bioinformatics. 2013;14:128. doi:10.1186/1471-2105-14-128
28. McGeary SE, Lin KS, Shi CY, et al. The biochemical basis of microRNA targeting efficacy. Science. 2019;366(6472). doi:10.1126/science.aav1741
29. Park SJ, Yoon BH, Kim SK, Kim SY. GENT2: an updated gene expression database for normal and tumor tissues. BMC Med Genomics. 2019;12(Suppl 5):101. doi:10.1186/s12920-019-0514-7
30. Cerami E, Gao J, Dogrusoz U, et al. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2(5):401–404. doi:10.1158/2159-8290.CD-12-0095
31. Tang Z, Kang B, Li C, Chen T, Zhang Z. GEPIA2: an enhanced web server for large-scale expression profiling and interactive analysis. Nucleic Acids Res. 2019;47(W1):W556–W60. doi:10.1093/nar/gkz430
32. Uhlen M, Fagerberg L, Hallstrom BM, et al. Proteomics. Tissue-based map of the human proteome. Science. 2015;347(6220):1260419. doi:10.1126/science.1260419
33. Lai H, Li Y, Zhang H, et al. exoRBase 2.0: an atlas of mRNA, lncRNA and circRNA in extracellular vesicles from human biofluids. Nucleic Acids Res. 2022;50(D1):D118–D28. doi:10.1093/nar/gkab1085
34. Hu X, Bao M, Huang J, Zhou L, Zheng S. Identification and validation of novel biomarkers for diagnosis and prognosis of hepatocellular carcinoma. Front Oncol. 2020;10:541479. doi:10.3389/fonc.2020.541479
35. Freeman AK, Morrison DK. 14-3-3 Proteins: diverse functions in cell proliferation and cancer progression. Semin Cell Dev Biol. 2011;22(7):681–687. doi:10.1016/j.semcdb.2011.08.009
36. Berghuis AMS, Koffijberg H, Prakash J, Terstappen LW, IJzerman MJ. Detecting blood-based biomarkers in metastatic breast cancer: a systematic review of their current status and clinical utility. Int J Mol Sci. 2017;18(2):363. doi:10.3390/ijms18020363
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
ITGA9 Inhibits Proliferation and Migration of Dermal Microvascular Endothelial Cells in Psoriasis
Hou H, Li J, Wang J, Zhou L, Li J, Liang J, Yin G, Li X, Cheng Y, Zhang K
Clinical, Cosmetic and Investigational Dermatology 2022, 15:2795-2806
Published Date: 20 December 2022
Serine/Threonine Protein Kinase-3 Promotes Oral Squamous Cell Carcinoma by Activating Ras-MAPK Mediated Cell Cycle Progression
Yue L, Xu Y, Lu P
International Journal of General Medicine 2023, 16:3115-3124
Published Date: 21 July 2023
Prognostic and Immune Infiltration Analysis of Transaldolase 1 (TALDO1) in Hepatocellular Carcinoma
Cen K, Lu C
International Journal of General Medicine 2023, 16:5779-5788
Published Date: 8 December 2023
circPVT1 Inhibits the Proliferation and Aids in Prediction of the Prognosis of Bladder Cancer
Zhou H, Cui X, Zhu L, Xu Z, Wang Z, Shao J
Pharmacogenomics and Personalized Medicine 2024, 17:1-11
Published Date: 5 January 2024
Cold Air Plasma Inhibiting Tumor-Like Biological Behavior of Rheumatoid Arthritis Fibroblast-Like Synovial Cells via G2/M Cell Cycle Arrest
Ni LY, Ding CB, Deng JM, Wu ZW, Zhou Y
Open Access Rheumatology: Research and Reviews 2024, 16:75-85
Published Date: 14 May 2024