Back to Journals » Journal of Inflammation Research » Volume 18
Abnormal CSF-Specific OCBs in Neuronal Surface Antibody-Associated Autoimmune Encephalitis Differentiating from Viral Encephalitis
Authors Qiao S, Zhang C , Li H, Zhou T, Wang A, Zhang S
Received 18 November 2024
Accepted for publication 30 January 2025
Published 17 February 2025 Volume 2025:18 Pages 2307—2316
DOI https://doi.org/10.2147/JIR.S504003
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Tara Strutt
Shan Qiao,1,2,* Chong Zhang,1,3,* Haiyun Li,4,* Tianyu Zhou,1,3 Aihua Wang,1 Shanchao Zhang1,5,6
1Department of Neurology, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Shandong Institute of Neuroimmunology, Jinan, People`s Republic of China; 2Department of Medical Genetics, School of Basic Medical Sciences, Cheeloo College of, Medicine, Shandong University, Jinan, People’s Republic of China; 3Shandong First Medical University & Shandong Academy of Medical Sciences, Jinan, People`s Republic of China; 4Department of Geriatric Medicine, Qilu Hospital, Cheeloo College of Medicine, Shandong University, Jinan, People’s Republic of China; 5School of Medicine, Cheeloo College of Medicine, Shandong University, Jinan, People’s Republic of China; 6Department of Neurology, Beijing Friendship Hospital, Capital Medical University, Beijing, People`s Republic of China
*These authors contributed equally to this work
Correspondence: Shanchao Zhang, Department of Neurology, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Shandong Institute of Neuroimmunology, Jinan, People`s Republic of China, Email [email protected]
Purpose: The present study aimed to examine the clinical distinctions among patients with neuronal surface antibody-associated autoimmune encephalitis (NSAE) diagnosed with anti-N-methyl-D-aspartate receptor encephalitis (NMDAR-E), anti-leucine-rich glioma-inactivated 1 encephalitis (LGI1-E), and anti-gamma aminobutyric acid-B receptor encephalitis (GABABR-E), compared with those with viral encephalitis (VE). Additionally, the study aimed to assess the impact of cerebrospinal fluid (CSF) oligoclonal bands (OCBs) on the severity and prognosis of NSAE.
Patients and Methods: This retrospective analysis included patients with NSAE, encompassing NMDAR-E, LGI1-E, and GABABR-E, alongside individuals with VE. Participants with NSAE were categorized into two groups based on the presence or absence of CSF-specific OCBs. Data regarding demographics, clinical manifestations, magnetic resonance imaging (MRI) findings, CSF analyses and prognosis were collected and analyzed.
Results: The findings indicated that younger female with NSAE exhibited a higher incidence of seizure onset, disruption of the blood-CSF barrier (BCSFB), and elevated QAlb/QLim ratios compared to VE patients, with NSAE patients demonstrating more severe clinical outcomes at discharge. Among the 185 NSAE patients, 43 (23.24%) were positive for OCBs, while 142 (76.76%) negative. The OCB-positive cohort displayed a greater prevalence of younger females and NMDAR-E (both P< 0.05). No significant differences were observed in CSF white blood cell counts, protein concentrations, or immunoglobulin G levels between the two groups (all P> 0.05). The modified Rankin Scale (mRS) scores at discharge and the final follow-up were higher in the OCB-positive group than the OCB-negative group (both P< 0.05). Both univariate and multivariate analyses identified OCBs and NSAE subtypes as independent risk factors influencing the clinical prognosis of NSAE.
Conclusion: In comparison to VE patients, NSAE patients with positive OCBs were more frequently female and exhibited CSF pleocytosis, particularly among those with NMDAR-E. Importantly, the presence of positive OCBs emerged as an independent predictor of unfavorable outcomes in patients with NMDAR-E, LGI1-E, and GABABR-E.
Keywords: autoimmune encephalitis, oligoclonal bands, prognosis, cerebrospinal fluid, viral encephalitis
Introduction
In China, three prevalent types of neuronal surface antibody-associated autoimmune encephalitis (NSAE) include NMDA receptor encephalitis (NMDAR-E), leucine-rich glioma inactivated protein-1 encephalitis (LGI1-E), and gamma-aminobutyric acid-B receptor encephalitis (GABABR-E). Patients suffering from these NSAE subtypes display various clinical symptoms, such as seizures, psychiatric and behavioral issues, speech difficulties, autonomic nervous system dysfunction, cognitive impairments and involuntary movements.1,2 However, the precise mechanisms behind these NSAE subtypes are not fully understood. Research indicates that immune responses involving B cells may significantly contribute to the pathogenesis of these conditions.3,4 The detection of immunoglobulin G (IgG) oligoclonal bands (OCBs) is an immune marker indicating the intrathecal production of immunoglobulins by activated B-cell clones mainly within the central nervous system (CNS).5 OCBs have been found in various immune-mediated and infectious neurological disorders, including multiple sclerosis (MS), neurosyphilis, Behçet’s disease, and neurosarcoidosis.6–8 In MS, OCBs are regarded as important biological marker.9 Previous studies have shown that CSF OCBs can be present in AE, with AE patients who have positive OCBs showing significantly higher median CASE and mRS scores before receiving immunotherapy compared to those with negative OCBs.10–12 However, there is limited researches on the relationship between OCBs and disease characteristics or clinical outcomes in a larger group of patients with NMDAR-E, LGI1-E, and GABABR-E. Consequently, we performed a retrospective analysis of the clinical and paraclinical characteristics of patients with NMDAR-E, LGI1-E, or GABABR-E based on their CSF OCBs status, as well as the association between OCBs and the severity and prognosis of NSAE.
Materials and Methods
Patients and Data Collection
Patients were retrospectively recruited from February 2016 to March 2023, with 185 NSAE subjects diagnosed with AE meeting specific inclusion criteria, as outlined in our previous study,11 and 38 subjects with viral encephalitis (VE). For NSAE patients, the criteria included a confirmed diagnosis of AE with positive CSF and/or serum anti-NMDAR, anti-LGI1, or anti-GABABR antibody, as defined using a fixed cell-based assay (Euroimmun, Germany).13 Data for NSAE patients were excluded for the following reasons: (1) laboratory evidence of infectious encephalitis (eg, viral, bacterial, mycobacterial tuberculosis); (2) incomplete data or a history of other central nervous system diseases (eg, multiple sclerosis, epilepsy, stroke, intracranial tumors, toxic-metabolic encephalopathy, schizophrenia or related conditions prior to the onset of encephalitis); and (3) presence of coexisting antibodies, such as myelin oligodendrocyte glycoprotein (MOG) antibody, aquaporin 4 (AQP4) antibody, and other AE neuronal antibody.
All VE patients met the clinical diagnostic criteria according to the Chinese Society of Neurology guidelines and had compatible laboratory and imaging results,14,15 including (1) altered mental status lasting > 24h; (2) at least 2 of the following: (a) fever ≥ 38° C within the 72 h before or after presentation, (b) generalized or partial seizures, (c) new onset of focal neurological findings, (d) CSF WBC counts ≥ 5/mm3, (e) abnormal imaging findings consistent with encephalitis, (f) abnormal EEG finding consistent with encephalitis; (3) Patient CSF samples tested positive for viruses, including HSV-1 and −2, varicella zoster virus (VZV), Epstein-Barr virus (EBV), pseudorabies virus (PRV) and parvovirus B19, through real-time PCR or metagenomic next-generation sequencing (mNGS) and were negative for antibodies against neuronal autoantigens. Patients with infections such as mycobacterium tuberculosis, parasites and fungi and other pathogens were excluded from this study.
The 185 NSAE patients were recruited from The First Affiliated Hospital of Shandong First Medical University and Qilu Hospital, Shandong University, comprising 102 with NMDAR-E, 68 with LGI1-E and 15 with GABABR-E. The 38 VE patients, including 13 with HSV encephalitis, 14 with VZV encephalitis, 7 with EBV encephalitis, 2 with PRV encephalitis and 2 with parvovirus B19 encephalitis, were also sourced from The First Affiliated Hospital of Shandong First Medical University. Clinical data, including demographic details, age at onset, prodromal symptoms, clinical manifestations, CSF findings, CSF-specific OCBs, presence of coexisting tumors, MRI results, ICU requirements and treatment regimens, were gathered through a retrospective review of medical records. Paired serum and CSF samples were tested for CSF-specific OCBs during the initial lumbar puncture (LP) of the recruited patients. Follow-up data were collected through clinical examinations during return visits and telephone interviews. The modified Rankin scale (mRS) was utilized to assess each patient’s neurological status, and the Clinical Assessment Scale in Autoimmune Encephalitis (CASE) score was calculated for each patient with NMDAR-E.16
Definitions
Pleocytosis was defined as having more than 5 leukocytes per microliter. The parameter of QAlb was used to estimate the permeability of brain barriers.17 As QAlb is age dependent, the age-normalized QAlb (QAlb/Qlim) was determined by dividing QAlb by the age-specific upper limit (Qlim; 4+age/15×10−3).18 A break in the blood-CSF barrier (BCSFB) was indicated by a QAlb/Qlim ratio greater than 1. mRS score ≤2 was indicative of good functional status, while a score >2 indicated poor functional status.
Blood and CSF Analysis
The samples of serum and CSF were acquired simultaneously at acute stage of NSAE and VE. The CSF samples were tested for white blood cells, total protein, albumin, and IgG et al. Paired serum and CSF were tested for OCBs using isoelectric focusing followed by IgG immunofixation during the recruited patients` initial LP.
Acquirement and Interpretation of Neuroimaging
Brain magnetic resonance imaging (MRI) examinations were performed during the acute stage of NSAE and VE using 1.5 T or 3.0 T scanner. Images were independently evaluated by two neurologists (SQ and AHW). Brain MRI abnormalities were defined as new-onset brain lesions with abnormal signals on T1-weighted, T2-weighted, fluid attenuated inversion recovery (FLAIR), diffusion weighted or contrast enhanced T1-weighted images.
Statistical Analysis
The findings were presented as percentages, medians and interquartile ranges (IQR). The Kolmogorov–Smirnov test was utilized to assess the distribution of the variables. Univariate analyses were conducted using the Chi-square test or Fisher’s exact test for categorical data, and the Mann–Whitney U-test for continuous data when the distribution was non-normal. The Student’s t-test or Mann–Whitney U-test was employed for two groups, while the Kruskal–Wallis test followed by the Dunn multiple comparisons test was used for more than two groups. Multivariate logistic regression analyses were carried out after adjusting for various potential confounding factors to identify the risk factors associated with long-term prognosis. Odds ratios (OR) and 95% confidence intervals (CI) were provided for the risk estimates. A p-value < 0.05 was deemed statistically significant. The statistical analyses were conducted using SPSS (version 25.0) and R software (version 4.0.2).
Results
Demographic and Clinical Characteristics of the Participants
In our study, we consecutively recruited 185 patients with NSAE and 38 patients with VE. Table S1 presented the demographic and clinical characteristics of these two groups. A greater percentage of female patients was observed in the NSAE group compared to the VE group (48.1% vs 28.9%, P=0.031). The median age of onset for NSAE was 38.0 years (IQR: 16.0, 62.0), which was lower than the median age for VE at 53.0 years (IQR: 27.0, 63.5). Seizures were more frequently the initial symptom in NSAE patients than in VE patients (81.08% vs 44.7%, P<0.001). In terms of CSF tests, NSAE patients had significantly higher levels of CSF protein compared to VE patients (P=0.001). The QAlb/QLim ratio was also notably higher in NSAE patients (1.56 [IQR: 0.86, 2.79] vs 0.70 [IQR: 0.48, 1.01], P<0.001), as was the rate of BCSFB disruption (70.8% vs 26.3%, P<0.001). However, there were no significant differences in CSF white blood cell (WBC) counts or CSF IgG levels between the two groups (all P>0.05). Regarding MRI findings, the incidence of lesions in the frontal lobe, parietal lobe, basal ganglia and white matter were significantly higher in VE patients than that in NSAE patients (all P<0.05). Additionally, the mRS scores at discharge were significantly higher for NSAE patients compared to VE patients (P<0.001).
OCBs and Clinical Manifestations
As indicated in Table 1, the OCB positive group had a higher percentage of females compared to the OCB negative group (67.40% vs 42.30%, P=0.040). Additionally, the patients in the OCB positive group were significantly younger than those in the OCB negative group (P=0.018). There were notable differences in NSAE subtypes between the two groups (P<0.001), with a higher percentage of positive OCB in NMDAR-E patients (79.07% vs 47.90%) and a lower percentage in LGI1-E patients (11.63% vs 44.40%). Regarding disease severity, the mRS scores at admission were higher in the OCB positive group compared to the OCB negative group (P=0.003). However, there were no significant differences in prodromal symptoms, disease duration at admission, presence of concomitant tumors, or ICU requirements during hospitalization between the two groups (all P>0.05). The initial symptoms, such as seizures, psychiatric issues, memory problems and others, were similar across both subgroups (P>0.05) as shown in Table 1. Among NMDAR-E patients, concomitant tumors were more frequently found in the OCB negative group compared to the OCB positive group (11.8% vs 0.0%, P=0.037), with no significant differences in other characteristics, as presented in Table S2.
 |
Table 1 Comparison of Demographic and Clinical Characteristics Between OCB(+) and OCB(-) Groups of NSAE |
OCBs and Serum/CSF Profiles, Brain Lesions on MRI
According to Table 2, there were no significant differences in CSF WBC, CSF protein levels, CSF IgG and QAlb/QLim between the two groups (all P>0.05). However, a higher percentage of NSAE patients with pleocytosis was found in the OCB positive group compared to the OCB negative group (P=0.025). NSAE patients in the OCB positive group showed no significant differences in brain lesions on MRI compared with those in the OCB negative group (P>0.05). Regarding lesion distribution, the occurrence rates of lesions in the frontal lobe, parietal lobe, temporal lobe, occipital lobe, basal ganglia, brainstem, cerebellum, and white matter were comparable between the OCB positive and OCB negative groups (all P>0.05) (Table 2). For patients with NMDAR-E, the CSF parameters were also similar between the OCB positive and OCB negative groups, as were the brain MRI regions (all P>0.05) (Table S3).
 |
Table 2 Comparison of Paraclinical Profiles Between OCB(+) and OCB(-) Groups of NSAE |
OCBs and Clinical Outcomes
As indicated in Table 3, the majority of patients received first-line immunotherapies, such as steroids and intravenous immunoglobulin, during their hospital stay, with similar treatment rates in both OCB positive and OCB negative groups (both P>0.05). The median years of follow-up time did not differ between OCB positive and OCB negative groups (1.50 [IQR: 0.83, 2.42] vs 1.33 [IQR: 0.75, 2.08], P=0.124) (P>0.05). The mRS scores at discharge were significantly higher in the OCB positive group compared to the OCB negative group (2.0 [IQR: 2.0, 3.0] vs 2.0 [IQR: 1.0, 2.0], P=0.019). At the last follow-up, the median mRS scores remained higher in the OCB positive group than in the OCB negative group (1.0 [IQR: 0.0, 2.0] vs 1.0 [IQR: 0.0, 1.0], P=0.014) (Table 3, Figure 1A and B). However, among the patients with NMDAR-E, the mRS scores at the last follow-up were significantly higher in the OCB positive group compared to the OCB negative group (1.0 [IQR: 0.0, 2.0] vs 1.0 [IQR: 0.0, 1.0], P=0.037) despite no difference in the median follow-up time (1.50 [IQR: 0.69, 2.25] vs 1.17 [IQR: 0.75, 1.98], P>0.05) (Table S4). To further investigate the relationship between OCBs and long-term outcomes, the patients were categorized into a good prognosis group (mRS ≤2, n=149) and a poor prognosis group (mRS >2, n=36). In the univariate analysis, as shown in Table S5, all factors, not including gender, NSAE subtype, concomitant tumor, BCSFB disruption and OCBs, were not statistically different between the good and poor prognosis groups (all P>0.05).
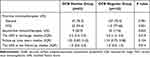 |
Table 3 Comparison of Clinical Outcome Between OCB(+) and OCB(-) Groups of NSAE |
To evaluate the significance of OCB as an independent risk factor, we conducted multivariate analyses considering various confounding factors in NMDAR-E, LGI1-E, and GABABR-E. As presented in Table S6, multivariate logistic regression models indicated that, unlike NMDAR-E and LGI1-E which predicted favorable outcomes compared to GABABR-E (OR=0.037, 95% CI=0.09–0.163, P<0.001; OR=0.024, 95% CI=0.05–0.117, P<0.001), Positive OCB was identified as an independent risk factor for poor prognosis (OR=3.185, 95% CI=1.254–8.095, P=0.015).
Discussion
NSAE vs VE
VE and NSAE exhibit similarities in clinical manifestations. However, they differ significantly in their underlying pathogenesis and treatment protocols. Consequently, prompt and accurate identification, along with timely intervention, is essential. Diagnostic methods such as polymerase chain reaction (PCR) and next-generation sequencing (NGS) have been extensively employed for the identification of VE.19 Various techniques, including immunoblotting, cell-based assays (CBA), immunohistochemistry, and indirect immunofluorescence (IIF) assays, are utilized to detect highly specific autoantibodies associated with AE.20 It is important to note that negative results for pathogens or specific autoantibodies do not rule out the possibility of VE or AE.19 Clinically, there are notable differences in specific features and lesions observed in brain imaging, electroencephalograms (EEG), and laboratory findings between VE and NSAE. Our recent retrospective study analyzed the clinical characteristics, CSF auxiliary examinations, and imaging findings that differentiate VE from NSAE within our patient cohort. Additionally, we explored the relationship between CSF-specific OCBs and the distinct features and prognosis of NSAE.
OCB+ vs OCB- Patients with NSAE
OCBs serve as an important clinical marker for multiple sclerosis (MS), being present in up to 95% of MS cases, and their diagnostic and prognostic roles in CSF analysis are well recognized.21–23 OCB is included in the diagnostic criteria for NMDAR-E, which aids in identifying potential cases of this condition.13 Furthermore, specific OCB in CSF is part of the criteria for diagnosing probable AE in patients who test negative for autoantibodies.24 Therefore, OCBs testing is crucial for accurate diagnosis and treatment planning, especially when antibodies are absent. A previous study analyzed the inflammatory CSF parameters in three AE subgroups respectively, including NMDAR, LGI1 and GABABR encephalitis, but not in the whole patient cohort, and then acquired potential predictors for the occurrence of NMDAR or LGI1 encephalitis.11 Our current study reanalyze the clinical data in our previous study,11 and indicated that OCBs positivity is an independent prognostic factor for poor outcomes in NSAE cases involving NMDAR-E, LGI1-E, and GABABR-E. Although these three conditions are distinct, OCBs may play a significant role in their pathogenesis and progression.
Our investigation initially identified a higher prevalence of younger female patients and an increased incidence of seizure onset in individuals with NSAE compared to those with VE, corroborating findings from prior research.10 Given that brain MRI results are typically normal during the acute phases of autoimmune encephalitis onset,25 abnormal MRI findings were more frequently observed in the VE cohort in our study. Although neuroimaging may not consistently assist in identifying a specific etiology in cases of VE, certain distinctive neuroimaging patterns have been associated with particular viral pathogens.26 For example, lesions in the brainstem, cerebellum, or temporal lobes, with or without ischemic or hemorrhagic changes, are characteristic of VZV encephalitis.27 Similarly, findings related to HSV encephalitis are often noted in the medial temporal lobe, cingulate gyrus, and the orbital surface of the frontal lobes.28 In contrast to previous studies,29 our VE cohort did not exhibit elevated CSF leukocyte counts or significant BCSFB disruption when compared to the NSAE cohort. This discrepancy may be explained by the predominance of patients with NMDAR encephalitis within the overall NSAE population, which has been documented to present with a pronounced and severe inflammatory response in the CSF.11
Next, we analyzed the discrepant clinic features in the presence or absence of CSF-specific OCBs in NSAE. In our study, the overall OCBs positivity rate among NSAE patients was 23.24%, with the highest rate in NMDAR-E at 33.33% and the lowest in the LGI1-E group at 7.35%. These findings are consistent with previous reports of OCBs positivity in NMDAR-E, while the occurrence of OCBs in LGI1-E remains notably low at just 5%.10,30 There were no significant differences in major clinical symptoms between the OCBs positive and negative groups. We observed that females, particularly younger ones, were more prevalent among NSAE patients with positive OCBs, suggesting that female may be a risk factor for abnormal immune globulin synthesis. In studies of anti-MOG-IgG associated disorders (MOGAD),31 a higher proportion of female patients tested positive for OCBs compared to males. Additionally, in a cohort study of MS, female patients with OCBs showed a higher annual relapse rate.32 Key diagnostic parameters for AE include CSF pleocytosis, specific OCBs in CSF, and elevated CSF IgG levels, with CSF pleocytosis being particularly important for confirming AE diagnosis.11,30 Previous research has shown that AE subtypes with frequent CSF pleocytosis often also have high OCBs positivity.30,33 However, our data indicated no significant differences in CSF cell count, CSF IgG levels, or QAlb elevation between OCB positive and negative groups in NMDAR-E, LGI1-E, and GABABR-E. To account for the influence of different NSAE subtypes on these CSF parameters, we further analyzed NMDAR-E patients and found no significant differences in CSF WBC count, pleocytosis, IgG levels, or QAlb elevation between OCBs positive and negative cases.
In our study, a significant proportion of patients demonstrated favorable long-term functional outcomes, aligning with the results reported in previous studies.34–36 The mRS scores at both discharge and the final follow-up were markedly higher in the group with positive OCBs compared to those with negative OCBs. However, the frequency of first-line and second-line immunotherapies administered did not differ between the two groups in our study. It is widely acknowledged that patients with AE derive substantial benefits from the early initiation of immunotherapy following disease onset.37,38 The timing of first-line and second-line immunotherapy is influenced by factors such as the duration of hospitalization, disease severity, progression, and therapeutic responses, rather than the status of CSF-specific OCBs. Furthermore, multivariate logistic regression analysis indicated that positive OCBs serve as an independent risk factor for poor prognosis in cases of NMDAR-E, LGI1-E, and GABABR-E. These results suggest that patients exhibiting severe intrathecal immune responses may demonstrate reduced responsiveness to first-line immunotherapies and experience poorer short- and long-term outcomes. The NMDAR-E cohort exhibited similar trends. An increased presence of immune cells and autoantibodies within CNS may elicit a heightened immune response in the brain, resulting in unfavorable prognoses. Consequently, the status of OCBs may serve as a potential prognostic indicator for patients with NMDAR-E, LGI1-E, or GABABR-E.
Our findings further indicated that neurological dysfunction at discharge, as assessed by the mRS, was more pronounced in the OCBs positive group compared to the OCBs negative group. For NMDAR-E, the majority of clinical and paraclinical characteristics were consistent with the overall profile of AE. Notably, the incidence of concurrent tumors was lower in the OCBs positive group within our study. The severity of the disease at admission did not significantly differ between the OCBs positive and negative groups in our cohort of NMDAR-E, LGI1-E, and GABABR-E. Correspondingly, our results indicated that the severity of the disease at admission, as measured by mRS, was not significantly different between the OCBs positive and negative groups. However, another study reported that AE patients with positive CSF-specific OCBs were more likely to exhibit greater disease severity than those with negative OCBs.12 NMDAR-E patients with compromised blood-brain barriers tended to present with increased disease severity prior to the initiation of immunotherapy.39 In the context of other inflammatory CNS disorders, OCB positivity was found to be unrelated to disease severity in MS patients.22 Therefore, the relationship between initial disease severity and OCB status warrants further exploration.
Our study is subject to several limitations. First, the retrospective nature of the cohort study may have introduced information bias. Second, the exclusion of patients who did not undergo OCB testing could lead to selection bias. The timing of immunotherapy initiation varied among AE patients due to the interval between disease onset and hospital treatment, which may have influenced clinical outcomes during follow-up. Third, the limited number of cases for NMDAR-E, LGI1-E, and GABABR-E restricted our ability to conduct subgroup analyses beyond NMDAR-E, however, the findings in the primary cohort were not validated in the external patient cohort. Consequently, further research involving prospective multicenter studies with larger patient populations and extended follow-up periods is necessary to validate our findings.
Conclusion
In conclusion, our study primarily examined the clinical manifestations, CSF auxiliary tests, and outcomes of patients diagnosed with NSAE in comparison to those with VE. The results indicated that certain clinical features, such as younger age, female sex, predisposition to seizures, significant disruption of the BCSFB, and normal neuroimaging findings, were more prevalent in patients diagnosed with AE. Following this, the NSAE cohort was further analyzed to investigate the relationship between OCBs in CSF and various clinical characteristics, CSF findings, neuroimaging results, and, importantly, long-term clinical outcomes. This analysis demonstrated that the NSAE group, which included cases of NMDAR, LGI1, and GABABR encephalitis, exhibited these associations collectively rather than within specific encephalitis subtypes. Additionally, the presence of CSF-specific OCBs in NSAE was found to correlate with disease severity and poor prognosis, indicating their potential as biomarkers. We recommend the initial assessment of CSF-specific OCBs as a strategy to monitor disease progression and predict clinical outcomes, as well as to identify patients at risk of severe illness early in the treatment process, which may facilitate the initiation and enhancement of clinical management strategies during the acute phase of the disease.
Abbreviations
NSAE, neuronal surface antibody-associated autoimmune encephalitis; NMDAR-E, anti-N-methyl-D-aspartate receptor encephalitis; LGI1-E, anti-leucine-rich glioma-inactivated 1 encephalitis; GABABR-E, anti-gamma aminobutyric acid-B receptor encephalitis; VE, viral encephalitis; VZV, varicella zoster virus; EBV, Epstein-Barr virus; PRV, pseudorabies virus; mNGS, metagenomic next-generation sequencing; CSF, cerebrospinal fluid; LP, lumbar puncture; OCBs, oligoclonal bands; AE, autoimmune encephalitis; MRI, magnetic resonance imaging; mRS, modified Rankin Scale; MS, multiple sclerosis; ICU, intensive care unit; CASE, Clinical Assessment Scale in Autoimmune Encephalitis; MOG, myelin oligodendrocyte glycoprotein; AQP4, aquaporin 4; FLAIR, fluid attenuated inversion recovery; IQR, interquartile range; OR, odds ratio; CI, confidence interval; MOGAD, anti-MOG-IgG associated-disorders; BCSFB, blood-CSF barrier.
Data Sharing Statement
Anonymized data not published within this article will be made available upon reasonable request from any qualified investigator.
Ethics Approval and Consent to Participate
Our study complied with the Declaration of Helsinki and Basel Declaration, and was approved by Institutional Review Board of The First Affiliated Hospital of Shandong First Medical University and Qilu Hospital, Shandong University, and the participants were fully informed about the purpose of the study and patient consent was acquired prior to the initiation of the experiment.
Acknowledgments
We thank the patients for participating in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by grants from the Natural Science Foundation of Shandong Province, China (No. ZR2016HP04, No.ZR2024MH269), and China Postdoctoral Science Foundation (2021M691227).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Masciocchi S, Businaro P, Scaranzin S, Morandi C, Franciotta D, Gastaldi M. General features, pathogenesis, and laboratory diagnostics of autoimmune encephalitis. Crit Rev Cl Lab Sci. 2024;61(1):45–69. doi:10.1080/10408363.2023.2247482
2. Shan W, Yang H, Wang Q. Neuronal surface antibody-medicated autoimmune encephalitis (limbic encephalitis) in China: a multiple-center, retrospective study. Front Immunol. 2021;12:621599. doi:10.3389/fimmu.2021.621599
3. Shang H, Shen X, Yu X, Zhang J, Jia Y, Gao F. B-cell targeted therapies in autoimmune encephalitis: mechanisms, clinical applications, and therapeutic potential. Front Immunol. 2024;15:1368275. doi:10.3389/fimmu.2024.1368275
4. Wagnon I, Helie P, Bardou I, et al. Autoimmune encephalitis mediated by b-cell response against n-methyl-d-aspartate receptor. Brain. 2020;143(10):2957–2972. doi:10.1093/brain/awaa250
5. Carta S, Ferraro D, Ferrari S, Briani C, Mariotto S. Oligoclonal bands: clinical utility and interpretation cues. Crit Rev Cl Lab Sci. 2022;59(6):391–404. doi:10.1080/10408363.2022.2039591
6. Taskiran E, Terzi M, Helvaci EM, et al. The role of oligoclonal band count and igg index in treatment response and disease activity in multiple sclerosis. Mult Scler Relat Dis. 2024;83:105391. doi:10.1016/j.msard.2023.105391
7. Mizoguchi T, Hara M, Nakajima H. Neurosyphilis presenting as autoimmune limbic encephalitis: a case report and literature review. Medicine. 2022;101(33):e30062. doi:10.1097/MD.0000000000030062
8. Arun T, Pattison L, Palace J. Distinguishing neurosarcoidosis from multiple sclerosis based on csf analysis: a retrospective study. Neurology. 2020;94(24):e2545–e2554. doi:10.1212/WNL.0000000000009491
9. Maglio G, D’Agostino M, Caronte FP, et al. Multiple sclerosis: from the application of oligoclonal bands to novel potential biomarkers. Int J Mol Sci. 2024;25(10):5412. doi:10.3390/ijms25105412
10. Durr M, Nissen G, Suhs KW, et al. Csf findings in acute nmdar and lgi1 antibody-associated autoimmune encephalitis. Neurol-Neuroimmunol. 2021;8(6). doi:10.1212/NXI.0000000000001086
11. Qiao S, Li H, Cui C, et al. Csf findings in Chinese patients with nmdar, lgi1 and gababr antibody-associated encephalitis. J Inflamm Res. 2024;17:1765–1776. doi:10.2147/JIR.S383161
12. Xue H, Guo X, Jiang Y, et al. Comparing clinical features, severity and prognosis of autoimmune encephalitis and with and without oligoclonal bands. Front Neurol. 2023;14:1281276. doi:10.3389/fneur.2023.1281276
13. Graus F, Titulaer MJ, Balu R, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016;15(4):391–404. doi:10.1016/S1474-4422(15)00401-9
14. Chinese Society of Infectious Diseases and Cerebrospinal Fluid Cytology. Expert consensus on clinical application of metagenomic next-generation sequencing of cerebrospinal fluid in the diagnosis of infectious diseases of the central nervous system. Chin J Neurol. 2021;54(12):1234–1240. doi:10.3760/cma.j.cn113694-20210730-00532
15. Zhao WL, Wu YH, Li HF, et al. Clinical experience and next-generation sequencing analysis of encephalitis caused by pseudorabies virus. Zhonghua Yi Xue Za Zhi. 2018;98(15):1152–1157. doi:10.3760/cma.j.issn.0376-2491.2018.15.006
16. Lim JA, Lee ST, Moon J, et al. Development of the clinical assessment scale in autoimmune encephalitis. Ann Neurol. 2019;85(3):352–358. doi:10.1002/ana.25421
17. Deisenhammer F, Bartos A, Egg R, et al. Guidelines on routine cerebrospinal fluid analysis. Report from an efns task force. Eur J Neurol. 2006;13(9):913–922. doi:10.1111/j.1468-1331.2006.01493.x
18. Reiber H. Flow rate of cerebrospinal fluid (csf)--a concept common to normal blood-csf barrier function and to dysfunction in neurological diseases. J Neurol Sci. 1994;122(2):189–203. doi:10.1016/0022-510x(94)90298-4
19. Tunkel AR, Glaser CA, Bloch KC, et al. The management of encephalitis: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2008;47(3):303–327. doi:10.1086/589747
20. Ricken G, Schwaiger C, De Simoni D, et al. Detection methods for autoantibodies in suspected autoimmune encephalitis. Front Neurol. 2018;9:841. doi:10.3389/fneur.2018.00841
21. Kennedy P, George W, Yu X. The elusive nature of the oligoclonal bands in multiple sclerosis. J Neurol. 2024;271(1):116–124. doi:10.1007/s00415-023-12081-7
22. Zhang X, Hao H, Jin T, et al. Cerebrospinal fluid oligoclonal bands in Chinese patients with multiple sclerosis: the prevalence and its association with clinical features. Front Immunol. 2023;14:1280020. doi:10.3389/fimmu.2023.1280020
23. Fonderico M, Portaccio E, Razzolini L, et al. Cerebrospinal fluid igm and oligoclonal igg bands in multiple sclerosis: a meta-analysis of prevalence and prognosis. Brain Sci. 2021;11(11):1444. doi:10.3390/brainsci11111444
24. Hebert J, Gros P, Lapointe S, et al. Searching for autoimmune encephalitis: beware of normal csf. J Neuroimmunol. 2020;345:577285. doi:10.1016/j.jneuroim.2020.577285
25. Sanvito F, Pichiecchio A, Paoletti M, et al. Autoimmune encephalitis: what the radiologist needs to know. Neuroradiology. 2024;66(5):653–675. doi:10.1007/s00234-024-03318-x
26. Vova JA, Howarth RA. Evaluation, treatment, and outcomes of viral and autoimmune encephalitis in children. Pediatr Clin North Am. 2023;70(3):429–444. doi:10.1016/j.pcl.2023.01.007
27. Venkatesan A, Tunkel AR, Bloch KC, et al. Case definitions, diagnostic algorithms, and priorities in encephalitis: consensus statement of the international encephalitis consortium. Clin Infect Dis. 2013;57(8):1114–1128. doi:10.1093/cid/cit458
28. Venkatesan A, Murphy OC. Viral encephalitis. Neurol Clin. 2018;36(4):705–724. doi:10.1016/j.ncl.2018.07.001
29. Granillo A, Le Marechal M, Diaz-Arias L, Probasco J, Venkatesan A, Hasbun R. Development and validation of a risk score to differentiate viral and autoimmune encephalitis in adults. Clin Infect Dis. 2023;76(3):e1294–e1301. doi:10.1093/cid/ciac711
30. Zrzavy T, Hoftberger R, Wimmer I, Berger T, Rommer P, Macher S. Longitudinal csf findings in autoimmune encephalitis-a monocentric cohort study. Front Immunol. 2021;12:646940. doi:10.3389/fimmu.2021.646940
31. Tomizawa Y, Hoshino Y, Kamo R, Cossu D, Yokoyama K, Hattori N. Comparing clinical and imaging features of patients with mog antibody-positivity and with and without oligoclonal bands. Front Immunol. 2023;14:1211776. doi:10.3389/fimmu.2023.1211776
32. Capuano R, Zubizarreta I, Alba-Arbalat S, et al. Oligoclonal igm bands in the cerebrospinal fluid of patients with relapsing ms to inform long-term ms disability. Mult Scler J. 2021;27(11):1706–1716. doi:10.1177/1352458520981910
33. Blinder T, Lewerenz J. Cerebrospinal fluid findings in patients with autoimmune encephalitis-a systematic analysis. Front Neurol. 2019;10:804. doi:10.3389/fneur.2019.00804
34. Huang T, Liu F, Wang B, Wang C, Hao M, Guo S. Clinical characteristics and prognosis in patients with neuronal surface antibody-mediated autoimmune encephalitis: a single-center cohort study in China. Front Immunol. 2023;14:1213532. doi:10.3389/fimmu.2023.1213532
35. Qiao S, Wu HK, Liu LL, et al. Characteristics and prognosis of autoimmune encephalitis in the east of China: a multi-center study. Front Neurol. 2021;12:642078. doi:10.3389/fneur.2021.642078
36. Wang B, Wang C, Feng J, Hao M, Guo S. Clinical features, treatment, and prognostic factors in neuronal surface antibody-mediated severe autoimmune encephalitis. Front Immunol. 2022;13:890656. doi:10.3389/fimmu.2022.890656
37. Abboud H, Probasco JC, Irani S, et al. Autoimmune encephalitis: proposed best practice recommendations for diagnosis and acute management. J Neurol Neurosurg Psychiatry. 2021;92(7):757–768. doi:10.1136/jnnp-2020-325300
38. Thaler FS, Zimmermann L, Kammermeier S, et al. Rituximab treatment and long-term outcome of patients with autoimmune encephalitis: real-world evidence from the generate registry. Neurol Neuroimmunol Neuroinflamm. 2021;8(6). doi:10.1212/NXI.0000000000001088
39. Yu Y, Wu Y, Cao X, et al. The clinical features and prognosis of anti-nmdar encephalitis depends on blood brain barrier integrity. Mult Scler Relat Dis. 2021;47:102604. doi:10.1016/j.msard.2020.102604
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
CSF Findings in Chinese Patients with NMDAR, LGI1 and GABABR Antibody-Associated Encephalitis
Qiao S, Li H, Cui C, Zhang C, Wang A, Jiang W, Zhang S
Journal of Inflammation Research 2024, 17:1765-1776
Published Date: 18 March 2024
Identifying Key Prognostic Indicators for Relapse and Chronic Epilepsy in Autoimmune Encephalitis: Insights from a Multicenter Retrospective Study
Lai Q, Chen Y, Wang W, Lian Z, Liu T, Wen C
Journal of Inflammation Research 2024, 17:11529-11543
Published Date: 24 December 2024


