Back to Journals » Vascular Health and Risk Management » Volume 21
Age and Sex Differences in the Risk of Sudden Cardiac Death in Patients with Hypertrophic Cardiomyopathy: A Multi-Centre Cohort Study
Authors Ma H, Xu F, Liu L, Pan C, Luo R, Liu M, Liu T, Shu Y, Li X
Received 21 December 2024
Accepted for publication 25 March 2025
Published 21 April 2025 Volume 2025:21 Pages 251—267
DOI https://doi.org/10.2147/VHRM.S511689
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Harry Struijker-Boudier
Huihui Ma,1,2 Fengcheng Xu,3,4 Lei Liu,5 Caixia Pan,1,2 Rong Luo,6 Mingjiang Liu,1,2 Tianhu Liu,3 Yan Shu,1,2 Xiaoping Li1,2
1School of Medicine, University of Electronic Science and Technology of China, Institute of Cardiovascular Diseases & Department of Cardiology, Sichuan Provincial People’s Hospital, Chengdu, 610072, People’s Republic of China; 2Chinese Academy of Sciences Sichuan Translational Medicine Research Hospital, Chengdu, 610072, People’s Republic of China; 3Department of Cardiology, Pidu District People’s Hospital, Chengdu, Sichuan, 611730, People’s Republic of China; 4Cardiology and Vascular Health Research Center, Chengdu Medical College, Chengdu, Sichuan, 610500, People’s Republic of China; 5Department of cardiology, Suining Central Hospital, Suning, Sichuan, 629000, People’s Republic of China; 6Institute of Geriatric Cardiovascular Disease, Chengdu Medical College, Chengdu, Sichuan, 610500, People’s Republic of China
Correspondence: Xiaoping Li, Institute of Cardiovascular Diseases & Department of Cardiology, Sichuan Provincial People’s Hospital, School of Medicine, University of Electronic Science and Technology of China, Chengdu, 610072, People’s Republic of China, Email [email protected] Yan Shu, Institute of Cardiovascular Diseases & Department of Cardiology, Sichuan Provincial People’s Hospital, School of Medicine, University of Electronic Science and Technology of China, Chengdu, 610072, People’s Republic of China, Email [email protected]
Objective: There is a significant difference in prognosis among patients with hypertrophic cardiomyopathy (HCM) across different age groups and gender groups. This study aims to explore the risk of sudden cardiac death (SCD) in various age groups and genders.
Methods: A cohort of 2781 patients with HCM, initially evaluated between 1996 and 2023, were followed for a median of 4.54 years. The patients were divided into three age groups: youth group (aged ≤ 40 years), middle-aged group (aged between 40 and 60 years), and elderly group (aged ≥ 60 years). The outcome event was (SCD). Kaplan-Meier survival curves and Cox regression analysis were employed to compare outcomes across different age groups for both genders. Additionally, restricted cubic splines (RCS) were utilized to evaluate the potential relationship between age and prognosis within different gender categories.
Results: A total of 128 patients (4.6%) experienced SCD. In the whole population, significant age differences were observed in the Kaplan-Meier survival curves for SCD (log-rank P< 0.0001). Significant age differences in SCD were also noted in both genders (log-rank P< 0.0001). In multivariate Cox regression analysis, age was an independent predictor of SCD in the whole population [HR: 0.983; 95% CI: 0.972– 0.994; P=0.003] and female patients [HR: 0.963; 95% CI: 0.947– 0.98; P< 0.001]. However, it was not significant in male patients [HR: 0.995; 95% CI: 0.98– 1.01; P=0.538].
Conclusion: In patients with HCM, age was an independent predictor of SCD both the whole population and female patients. Compared to young patients, the risk of SCD is reduced by 71.4% in middle-aged patients and by 43.5% in elderly patients across the whole population. Among male patients, the risk of SCD decreases by 68.5% in middle-aged patients and by 10.7% in elderly patients. In female patients, the risk of SCD is reduced by 77.8% in middle-aged patients and by 75.3% in elderly patients.
Keywords: hypertrophic cardiomyopathy, sudden cardiac death, restricted cubic splines
Introduction
Hypertrophic cardiomyopathy (HCM) is a genetic heart disease known for its unpredictable nature and recognised risk for sudden cardiac death (SCD).1 It is the leading cause of SCD among adolescents and young athletes.2–4 However, as the disease progresses and cardiac remodelling worsens, adult HCM patients also have an increased risk of SCD.4 Moreover, the incidence of HCM in elderly patients is increasing, which is attributed to increased awareness among physicians and advancements in imaging techniques.1 Recent evidence suggests that implantable cardioverter-defibrillators (ICDs) are effective in preventing SCD in high-risk HCM patients.5,6 Nonetheless, the natural history of HCM and the risk of adverse events in elderly patients have not been fully resolved.
Sex differences in the clinical presentation of HCM have received increasing attention.7 A series of studies have indicated that female HCM patients have a greater risk of cardiovascular mortality and all-cause mortality, yet no significant association has been found between female sex and the risk of SCD.7–12 Notably, current HCM management guidelines have yet to provide specific commentary on sex differences in prognosis.3,13 Additionally, SCD has always been a topic of great concern for HCM patients. Therefore, this study aims to investigate the differences in SCD among HCM patients of various ages and sexes.
Methods
Study Population
This observational cohort study included 2781 patients diagnosed with HCM, all of whom were hospitalised across 13 tertiary hospitals from 1996 to 2023. Patients with cardiac or systemic conditions that could result in comparable degrees of hypertrophy, such as Fabry disease, Noonan syndrome, cardiac amyloidosis, and amyloid cardiomyopathy, were excluded from the study (Figure 1). Given the large time span of data collection, we have segmented the patient data by year and conducted baseline comparison analysis according to the different stages of the release of relevant guidelines. The results show that there are indeed significant differences among the data of different time periods (Supplement Table 1). But among the three groups of patients, there was no significant difference in the KM survival curves between males and females (Supplement Figure 1). However, there were significant differences in SCD across different age groups from 1996 to 2014 (Supplement Figure 2a), while no significant differences were observed between the age groups from 2015- 2019 and from 2020- 2023 (Supplement Figure 2 b-c). This may also reflect from a certain perspective that with the continuous progress in the management of HCM and the improvement of medical standards, the SCD rate of patients with HCM has indeed been significantly reduced.
 |
Figure 1 Patient flow diagram. |
Diagnostic Criteria and Definitions
The diagnosis of HCM is based on a maximal end-diastolic wall thickness of ≥15 mm anywhere in the left ventricle, in the absence of another cause of hypertrophy in adults. This measurement can be obtained via various imaging techniques, including echocardiography and cardiac magnetic resonance imaging (CMR).3 More limited hypertrophy (13–14 mm) can also be diagnostic when present in family members of a patient with HCM or in conjunction with a positive genetic test that identifies a pathogenic or likely pathogenic variant, typically found in a sarcomere gene.3
The patients were categorised into three age groups: the youth group (aged ≤ 40 years), the middle-aged group (aged between 40 and 60 years), and the elderly group (aged ≥60 years).
Follow-up and Endpoints
The follow-up period of this study began in October 2011 and ended in April 2024. The primary endpoint of the study was SCD, defined as an unexpected death occurring either in the absence of symptoms or within one hour of symptom onset in patients who had previously exhibited a relatively stable or uneventful clinical course.14 Data regarding the occurrence of SCD were meticulously collected through a combination of methods, which included reviewing medical records from outpatient clinic visits and hospitalisations, conducting telephone interviews with patients or their families, and verifying survival status through national police records. Patients who could not be contacted within six months following discharge were classified as lost to follow-up.
Statistical Analysis
In this study, continuous variables are presented as the means ± standard deviations (SDs) for normally distributed data or as the medians with interquartile ranges (IQRs) for nonnormally distributed data. The differences between groups for continuous variables were assessed via the unpaired Student’s t test for normally distributed data and the Wilcoxon rank test for nonnormally distributed data. Categorical variables are expressed as proportions, with group differences evaluated via the Pearson chi-square test.
To identify factors independently associated with mortality, Cox proportional hazards modelling was employed. Hazard ratios (HRs), along with 95% confidence intervals (CIs) and P values, were reported to support the analysis. In the multivariate Cox regression analysis, factors were adjusted on the basis of a significance level of P ≤ 0.05, as determined by univariate analysis.
In the multivariate model adjustment, the variables adjusted for the whole population are age, hyperlipemia, atrial fibrillation (AF), atrioventricular block (AVB), intraventricular conduction block (IVCD), pulmonary hypertension (PH), apical HCM (AHCM), hypertrophic obstructive cardiomyopathy (HOCM), modified shock index (MSI), left ventricular diameter (LVD), left atrial diameter (LAD), left ventricular ejection fraction (LVEF), left ventricular posterior wall thickness (LVPW), left ventricular outflow tract gradient (LVOTG), N - terminal pro - B - type natriuretic peptide Log (NT-pro-BNP), uric acid (UA), alkaline phosphatase (ALP), creatinine, triglyceride - glucose index (TyG), creatinine kinase-myocardial band (CK-MB) etc, while for the male cohort, they are age, ventricular tachycardia (VT), AF, IVCD, familial HCM (FHCM), alcohol septal ablation (ASA) or septal myectomy (SM), AHCM, QRS, LVD, LAD, LVEF, LVPW, Log (NT-pro-BNP), albumin, TSH, ALP, random blood glucose, TyG, CK-MB etc, and for the female cohort, they are age, PH, LVD, LVEF, LVPW, LVOTG, Log (NT-pro-BNP), UA, ALP, creatinine, LDL-C, lactic dehydrogenase (LDH) etc.
All the statistical analyses were conducted via R version 4.2.3 (R Foundation for Statistical Computing, Vienna, Austria), with a significance threshold set at P values ≤ 0.05 considered statistically significant.
Results
Baseline Clinical Characteristics
The study included a total of 2781 patients with HCM, with a median follow-up period of 4.54 years (IQR: 2.13–7.99 years). The study population consisted of 375 patients in the youth group (13.5%), 1131 patients in the middle-aged group (40.7%), and 1275 patients in the elderly group (45.8%), of whom 1717 were men (61.7%) and 1064 were women (38.3%). A total of 128 patients (4.6%) experienced SCD, with 41 patients (10.9%) in the youth group, 34 patients (3%) in the middle-aged group, and 53 patients (4.2%) in the elderly group.
The baseline demographic, clinical, and biochemical characteristics across different age groups and sexes are detailed in Table 1. Compared with younger patients, there is a gradual decline in the proportion of individuals with a history of syncope, as well as a decrease in the incidence of a family history of SCD. As age progresses, the prevalence of stroke, coronary artery disease (CAD), and AF steadily increases, whereas the proportion of patients classified as intermediate risk or high risk for 5-year SCD decreases. Additionally, the maximal thickness of the left ventricular wall gradually decreases. The proportion of patients with ICD implantation is relatively low, with only 58 patients (2.1%) undergoing ICD implantation. It is notable that the proportion of ICD implantation is relatively higher in the young (2.4%) and middle-aged groups (2.7%) than in the elderly group (1.5%). However, there is no significant difference in gender distribution between men (2.1%) and women (2.1%). In CMR, there were a total of 451 patients showing late gadolinium enhancement (LGE). It is notable that the proportion of LGE was significantly higher in the young (69.7%) and middle-aged groups (61.5%) than in the elderly group (28.8%), and the proportion of male patients (18.2%) was also higher than that of female patients (13.1%).
 |
Table 1 Baseline Demographic and Clinical Characteristics of the Whole Population in Different Age Groups and Gender Groups |
Table 2 outlines the baseline demographic, clinical, and biochemical characteristics of the males and females among the different age groups. In the youth group, a greater proportion of women exhibited concomitant PH, and their levels of Log (NT-proBNP) were elevated. Conversely, men had a higher TyG index. In the middle-aged group, men had a greater incidence of CAD and a relatively greater incidence of AHCM, along with elevated TyG index and creatinine levels. Additionally, more women presented with left bundle branch block (LBBB). In the elderly group, women were older on average (71.13 years vs 69.27 years), and a greater proportion of them were classified as New York Heart Association (NYHA) class 3–4, with elevated log (NT-proBNP) levels. In terms of ICD implantation and LGE, no significant differences were observed between men and women of different age groups.
 |
Table 2 Baseline Demographic and Clinical Characteristics of Different Genders in Different Age Groups |
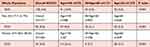 |
Table 3 Proportion of SCD in Patients According to Age and Gender Groups |
Outcomes of SCD Across Different Age Groups and Sexes
Table 3 presents the incidence of SCD across different age groups. The data revealed that the incidence of SCD was highest in the young group at 10.9%, whereas the middle-aged group presented the lowest incidence at 3%. The elderly group fell in between these two groups, with an incidence of 4.2%. Furthermore, the incidence of SCD among elderly male patients was greater than that among their female counterparts (5.3% vs 3.1%). The Kaplan‒Meier survival curve indicated a significant difference in SCD between men and women in the youth group (log-rank P = 0.036); however, no significant difference was observed between sexes in either the middle-aged group or the elderly group (log-rank P = 0.92; log-rank P = 0.054) (Figure 2).
Role of Age in the Prediction of SCD Across the Whole Population and in Both Sexes
The Kaplan‒Meier analysis revealed significant differences in SCD across the age groups within the whole population and among both sexes (log-rank P < 0.0001, Figure 3A–C). Furthermore, the multivariable Cox regression analysis indicated that age was an independent predictor for SCD in the whole population [HR: 0.983; 95% CI: 0.972–0.994; P = 0.003] and in females [HR: 0.963; 95% CI: 0.947–0.98; P < 0.001]. However, in male patients, age was not significantly associated with SCD [HR: 0.995; 95% CI: 0.98–1.01; P = 0.538] (Table 4).
 |
Table 4 Association of Age and SCD via Cox Regression Analysis |
Role of Different Age Groups in Predicting SCD Across the Whole Population and in Both Sexes
In the whole population, the risk of SCD in the middle-aged group was significantly lower (71.4%) than that in the young group [HR: 0.286; 95% CI: 0.18–0.455; P < 0.001], whereas the risk in the elderly group was 43.5% lower [HR: 0.565; 95% CI: 0.368–0.867; P = 0.009]. For male patients, the risk of SCD in the middle-aged group decreased by 68.5% [HR: 0.315; 95% CI: 0.176–0.563; P < 0.001], whereas the risk in the elderly group was reduced by only 10.7% [HR: 0.893; 95% CI: 0.495–1.614; P = 0.709], although this reduction was not statistically significant. In contrast, among female patients, the risk of SCD in the middle-aged group was reduced by 77.8% [HR: 0.222; 95% CI: 0.093–0.526; P = 0.001], and the risk in the elderly group decreased by 75.3% [HR: 0.247; 95% CI: 0.122–0.5; P < 0.001] (Table 4).
RCS Analysis and Threshold Analysis in Predicting SCD
As illustrated in Figure 4a–c, the fully adjusted RCS analysis revealed that age was significantly associated with SCD in the whole population, with all demonstrating a nonlinear relationship (P-overall<0.001, P for nonlinearity<0.001). When stratified by sex, the results indicated that age remained significantly associated with SCD among male (P<0.001, P for nonlinearity <0.001) and female patients (P<0.001, P for nonlinearity= 0.008), indicating that a nonlinear relationship was maintained.
Discussion
The study indicated that age was an independent predictor of SCD in both the whole population and among female patients. Compared with that of younger patients, the risk of SCD was reduced by 71.4% in middle-aged patients and by 43.5% in elderly patients across the entire population. In male patients, the risk of SCD decreased by 68.5% in middle-aged individuals and by 10.7% in elderly individuals. In contrast, female patients experienced a more significant reduction in risk, with a 77.8% decrease in middle-aged patients and a 75.3% decrease in elderly patients.
SCD is one of the most serious and devastating outcomes that patients with HCM may experience.15 Research has indicated that the risk of SCD is generally highest during adolescence and young adulthood rather than in later adulthood.16,17 The incidence of adverse events in young HCM patients (7–29 years old) was ≈2-fold greater than that in middle-aged patients (30–59 years old). However, following major treatment interventions, the annual mortality rate for HCM remains nearly the same in both groups (0.5%).18,19 This elevated risk in younger populations is partly due to the active and dynamic physiological changes occurring during growth, as well as the potentially more aggressive disease phenotypes that may manifest during these years.17,20,21 During childhood and adolescence, certain risk factors for SCD, such as severe left ventricular hypertrophy, left ventricular outflow tract obstruction (LVOTO), and arrhythmias, can be more pronounced.22–25 Additionally, young individuals may be more likely to engage in physical activities that could trigger arrhythmic events in.26
In the present study, 375 young patients (12.8%) were included in the whole population. The prevalence of SCD was 3.6 times greater in the middle-aged group (10.9% vs 3%) and 2.6 times greater in the elderly group (10.9% vs 4.2%). Notably, the youth group represented the highest proportion of individuals at high risk of 5-year SCD. Additionally, the incidence of SCD among young female patients was greater than that among their male counterparts (16.1% vs 9.4%). Research has indicated that the incidence of unexplained SCD in female patients under the age of 40 years is greater than that in males, particularly within the 35 to 44 years age range.27 In the present study, the proportion of female patients who experienced SCD was significantly greater than that of male patients, suggesting that younger female patients may be more susceptible to SCD. This observation may be related to the fact that the female patients in this study tended to be younger than their male counterparts (28 vs 30 years).
Furthermore, the number of young female patients was considerably lower than that of young male patients, which highlights the issue of insufficient early diagnosis among females. This finding is consistent with prior conclusions that female patients are generally diagnosed at an older age.7,8,28,29 However, it is important to note that the data are not entirely consistent with the previous research, in which young female patients had a greater risk of SCD than young male patients did. Therefore, further research is needed to validate these findings. Although the risk of SCD among young female patients is significantly greater than that among young male patients, female sex is not an independent risk factor for SCD.
In adult cardiovascular practice, the subgroup of HCM patients aged 30 to 59 years (middle-aged) is the most frequently assessed group and is associated with a higher incidence of adverse complications.19 For middle-aged HCM patients, prognosis is influenced by a variety of factors, including the age at diagnosis, genetic mutations, and sex.10,30,31 Notably, those diagnosed at a younger age (under 40 years) tend to experience poorer outcomes than their counterparts diagnosed at an older age (over 60 years).30 Research indicates that the cumulative incidence of overall composite outcomes by age 60 years for patients diagnosed before age 40 years is 77%, whereas for patients diagnosed at age 60 years or older, it is 32% by age 70 years.30 Additionally, mortality rates for young HCM patients (aged 20 to 29) are four times higher than those of the general US population.30
In this study, middle-aged patients constituted 40.7% of the overall population, with a notable predominance of males in this age group. While ventricular arrhythmia was more prevalent among these patients, the incidence of SCD was the lowest, at just 3%. In the present study, it is important to highlight that this demographic group represents the primary group receiving ICD treatment, accounting for 2.7% of the population. When the middle-aged group was compared with the youth group, the risk of SCD in the middle-aged group was reduced by 71.4%. Further analysis by sex revealed that the risk of SCD was decreased by 68.5% in males and 77.8% in females in the middle-aged group. Consequently, middle-aged patients had a lower risk of SCD than their younger counterparts did. Previous research supports these findings, demonstrating that the 5-year and 10-year survival rates for patients aged 30 to 59 years under contemporary treatment strategies are 98% and 94%, respectively, which are not significantly different from the all-cause mortality rates of the general population.19
In elderly HCM patients, the overall prognosis is relatively favourable, with a low risk of HCM-related mortality.1,32 Most deaths in this population are attributed to causes unrelated to HCM.32 Heart failure and AF are the most common adverse events among HCM patients; however, these conditions typically emerge several years after the initial diagnosis.10,30 While HF is more prevalent among elderly HCM patients, their prognosis is comparable to that of younger individuals.33 Notably, female patients with HCM generally experience poorer cardiovascular outcomes than their male counterparts do, with elderly women being particularly susceptible to HF and cardiovascular mortality.31 Even in the presence of conventional risk factors, the risk of SCD remains low in elderly HCM patients.1 As a result, proactive implantation of an ICD for preventive measures is generally not recommended.1,34
In this study, the incidence of SCD among elderly patients was found to be 4.2%, with men exhibiting a greater likelihood of experiencing SCD than women (5.3% vs 3.1%). Across each category of 5-year SCD risk, men consistently demonstrated a greater risk than women; however, the differences between the sexes were not statistically significant. Overall, the risk of SCD among elderly patients was reduced by 43.5%, with a decrease of 10.7% observed in males and a notable 75.3% in females. This finding indicates that elderly patients, compared with their younger counterparts, have a lower risk of SCD and that this difference is even more noticeable in women. Additionally, elderly HCM patients often present with a greater burden of cardiovascular comorbidities, which are closely associated with a poorer prognosis for HCM patients. These comorbidities included AF,35 CAD,36 and PH,37 all of which were more common in this age group in the present study.
Furthermore, quantitative CMR-LGE can provide important prognostic information for SCD in patients with HCM.38 The larger the LGE range, the higher the risk of patients developing ventricular arrhythmias and SCD,39 for every 10% increase in LGE, the risk of SCD increases by approximately 1.56 times (HR: 1.56 per 10% LGE).40 For HCM patients over 60 years old, the association between the range of LGE and the risk of SCD is not significant.41 This indicates that in elderly patients, LGE may play a limited role in the risk stratification of SCD. In the present study, the detection rate of LGE was higher in the young and middle-aged groups than in the elderly group, which might partly explain the higher rate of SCD in the young group. However, this study failed to achieve quantitative analysis of LGE.
According to the current guidelines, ICD is one of the effective strategies for preventing SCD.42 The implantation of ICD has changed the natural course of HCM, enabling many patients to achieve normal or near-normal lifespan.43,44 In young patients, ICD is equally effective and can prevent potentially fatal arrhythmias.45 Through risk stratification, the decision-making for ICD implantation has become more precise. In the present study, a total of 58 patients received ICD implantation. Among them, the proportion of patients in the young group and the middle-aged group was relatively high, which might be related to the higher proportion of high-risk patients in these two age groups. Among all age groups, the gender differences are not significant.
The prognosis of young HCM patients is influenced by several factors, including age, genetic mutations, family history, and sex.3,30 Young individuals have a greater risk of SCD, and female patients have a worse prognosis.7,10 Therefore, individualised risk assessment and long-term monitoring are crucial for improving the prognosis of these patients. In contrast, middle-aged patients generally have a better overall prognosis, with lower mortality rates related to HCM. For this group, the primary causes of death were often non-HCM-related diseases.1,30 HF and AF are the main adverse events, and female patients have poorer cardiovascular outcomes.30 The prognosis of asymptomatic patients is significantly better than that of symptomatic patients.46 For patients over the age of 60, HCM-related mortality is low, with an annual mortality rate of approximately 0.64%.1 The leading causes of death in this age group include embolic stroke, HF, postoperative complications, and SCD due to arrhythmias.
Based on the present research findings, young patients have a higher risk of experiencing SCD, and a larger proportion of them show LGE. Therefore, early clinical management of young patients is of crucial importance. Moreover, further research is still needed to clarify the gender differences between male and female patients with HCM in order to formulate evidence-based guidelines for gender-specific management of HCM. However, this study acknowledges the potential confounding factors, as the time span of the cohort is long and the proportion of patients undergoing CMR examination is relatively low. Future research should include larger and more comprehensive cohorts to better assess the risk of SCD in HCM patients.
Study Limitations
There are several limitations to this study. First, given that the study’s results are derived from a Chinese cohort, it is important to conduct further research to evaluate the applicability of these findings to other populations. Second, the fact that the patients in the study were drawn from different hospitals over a substantial time span introduces data heterogeneity. This variability can affect the consistency and reliability of the findings, as differences in medical practices, patient demographics, and temporal healthcare advancements can lead to variations in outcomes. Understanding and accounting for these factors is crucial for accurately interpreting the study’s conclusions and assessing their broader relevance. Third, LGE is indeed recognised as an important prognostic marker for HCM, as it can indicate myocardial fibrosis and is associated with adverse cardiac events. However, the small sample size of patients who underwent CMRI imaging limits the statistical power and the ability to draw strong conclusions about the relationship between LGE and clinical outcomes within our cohort. Finally, the absence of genetic testing in our cohort limits the ability to explore the role of genetic factors in the prognosis of patients with HCM and different sexes.
Conclusion
In patients with HCM, age was an independent predictor of SCD across the entire population. Compared with that of young patients, the risk of SCD was reduced by 71.4% in middle-aged patients and by 43.5% in elderly patients. Specifically, among male patients, the risk of SCD decreased by 68.5% in middle-aged individuals and by 10.7% in elderly individuals. In contrast, female patients experienced a more significant reduction, with the risk of SCD declining by 77.8% in middle-aged patients and by 75.3% in elderly patients.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding author upon request.
Ethics Statement
Ethical approval was obtained from the Research Ethics Committees of Sichuan Provincial People’s Hospital (No. 2022424), and the study protocol was approved by the Institutional Review Board. Given the nature of the anonymized data and the low-risk profile of the research, ethical guidelines do not require informed consent. This study was conducted in accordance with the principles of the Declaration of Helsinki.
Acknowledgment
The authors would like to thank the following hospitals for the multicenter data:
Fuwai Hospital; The First Affiliated Hospital of Chengdu Medical; The Second Affiliated Hospital of Chengdu Medical College & Nuclear Industry 416 hospital; The Third Affiliated Hospital of Chengdu Medical & Pidu District People’s Hospital; Mianyang Central Hospital; Sichuan Mianyang 404 hospital; The Third People’s Hospital of Chengdu; Hospital of Chengdu University of TCM & TCM Hospital of Sichuan Province; Suining People’s Hospital; The First Affiliated Hospital of Chongqing Medical University; The Second Affiliated Hospital of Chongqing Medical University; The Affiliated Hospital of Southwest Medical University and so on.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Supported by Sichuan Science and Technology Program (No. 2022NSFSC0538); National Natural Science Foundation of China (No. 32171182); Chengdu Medical College - Pidu District People’s Hospital Joint Science Foundation (No. 2021LHZD-03).
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Maron BJ, Rowin EJ, Casey SA, et al. Risk stratification and outcome of patients with hypertrophic cardiomyopathy ≥60 years of age. Circulation. 2013;127:585–593. doi:10.1161/CIRCULATIONAHA.112.136085
2. Spirito P, Autore C, Formisano F, et al. Risk of sudden death and outcome in patients with hypertrophic cardiomyopathy with benign presentation and without risk factors. Ame J Cardiol. 2014;113:1550–1555. doi:10.1016/j.amjcard.2014.01.435
3. Ommen SR, Ho CY, Asif IM, et al. AHA/ACC/AMSSM/HRS/PACES/SCMR guideline for the management of hypertrophic cardiomyopathy: a report of the American heart association/American college of cardiology joint committee on clinical practice guidelines. Circulation. 2024;151:149. doi:10.1161/CIRCULATIONAHA.124.072055
4. Jacobs C. Hypertrophic cardiomyopathy in adults: an overview. J Ame Assoc Nurse Pract. 2014;26:465–470. doi:10.1002/2327-6924.12156
5. Maron BJ, Shen WK, Link MS, et al. Efficacy of implantable cardioverter-defibrillators for the prevention of sudden death in patients with hypertrophic cardiomyopathy. N Engl J Med. 2000;342(6):365–373. doi:10.1056/NEJM200002103420601
6. Maron BJ, Spirito P, Shen WK, et al. Implantable cardioverter-defibrillators and prevention of sudden cardiac death in hypertrophic cardiomyopathy. JAMA. 2007;298(4):405–412. doi:10.1001/jama.298.4.405
7. Zhao H, Tan Z, Liu M, et al. Is there a sex difference in the prognosis of hypertrophic cardiomyopathy? A systematic review and meta‐analysis. J Ame Heart Association. 2023;12:e026270.
8. Geske JB, Ong KC, Siontis KC, et al. Women with hypertrophic cardiomyopathy have worse survival. Eur Heart J. 2017;38:3434–3440. doi:10.1093/eurheartj/ehx527
9. Rowin EJ, Maron MS, Wells S, et al. Impact of sex on clinical course and survival in the contemporary treatment era for hypertrophic cardiomyopathy. J Ame Heart Association. 2019;8:e012041.
10. Kim M, Kim B, Choi Y-J, et al. Sex differences in the prognosis of patients with hypertrophic cardiomyopathy. Scient Rep;2021. 11. doi:10.1038/s41598-020-79680-6
11. Tyw L, Yeo S, Ngiam NJH, et al. Effects of sex on clinical outcomes of hypertrophic cardiomyopathy in Singapore. Annals Acad Med Singapore. 2023;52:348–355. doi:10.47102/annals-acadmedsg.2022344
12. Montenegro Sá F, Oliveira M, Belo A, et al. The sex gap in hypertrophic cardiomyopathy. Revista Española de Cardiología. 2020;73:1018–1025. doi:10.1016/j.rec.2020.01.007
13. Ommen SR, Mital S, Burke MA, et al. AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: executive summary. Circulation. 2020;142:3022–3055.
14. Minami Y, Kajimoto K, Terajima Y, et al. Clinical implications of midventricular obstruction in patients with hypertrophic cardiomyopathy. J Ame College Cardiol. 2011;57:2346–2355. doi:10.1016/j.jacc.2011.02.033
15. Bianco F, Bucciarelli V. Hypertrophic cardiomyopathy risk scoring for sudden cardiac death in paediatrics, adolescents, and adults: stuck on the puzzle of clinical, imaging, and genetic features. Eur J Preventive Cardiol. 2022;29:675–677. doi:10.1093/eurjpc/zwab199
16. Pay L, Çetin T, Dereli Ş, et al. Validation of the HCM Risk‐SCD model in patients with hypertrophic cardiomyopathy and future perspectives. Pacing Clin Electrophysiol. 2023;46:1519–1525. doi:10.1111/pace.14876
17. Wang S, Zhu C. Hypertrophic cardiomyopathy in children. Asian Cardiovasc Thoracic Annals. 2021;30:92–97. doi:10.1177/02184923211041285
18. Maron BJ, Rowin EJ, Casey SA, et al. Hypertrophic cardiomyopathy in children, adolescents, and young adults associated with low cardiovascular mortality with contemporary management strategies. Circulation. 2016;133:62–73. doi:10.1161/CIRCULATIONAHA.115.017633
19. Maron BJ, Rowin EJ, Casey SA, et al. Hypertrophic cardiomyopathy in adulthood associated with low cardiovascular mortality with contemporary management strategies. J Ame College Cardiol. 2015;65:1915–1928. doi:10.1016/j.jacc.2015.02.061
20. Elliott P, McKenna WJ. Hypertrophic cardiomyopathy. Lancet. 2004;363:1881–1891. doi:10.1016/S0140-6736(04)16358-7
21. Rossano JW, Lin KY. Hypertrophic Cardiomyopathy. J Ame College Cardiol. 2022;79:1998–2000. doi:10.1016/j.jacc.2022.03.356
22. Norrish G, Cantarutti N, Pissaridou E, et al. Risk factors for sudden cardiac death in childhood hypertrophic cardiomyopathy: a systematic review and meta-analysis. Eur J Preventive Cardiol. 2017;24:1220–1230. doi:10.1177/2047487317702519
23. Giamouzis G, Dimos A, Xanthopoulos A, et al. Left ventricular hypertrophy and sudden cardiac death. Heart Failure Rev. 2021;27:711–724. doi:10.1007/s10741-021-10134-5
24. Norrish G, Ding T, Field E, et al. Relationship between maximal left ventricular wall thickness and sudden cardiac death in childhood onset hypertrophic cardiomyopathy. Circulation. 2022;15:e010075.
25. Christiaans I, van Engelen K, Van langen IM, et al. Risk stratification for sudden cardiac death in hypertrophic cardiomyopathy: systematic review of clinical risk markers. EP Europace. 2010;12:313–321. doi:10.1093/europace/eup431
26. Forså MI, Smedsrud MK, Haugaa KH, et al. Distinguishing left ventricular hypertrophy from hypertrophic cardiomyopathy in adolescents: a longitudinal observation study. Eur J Preventive Cardiol. 2024;31:591–598. doi:10.1093/eurjpc/zwad361
27. Chugh SS, Chung K, Zheng Z-J, et al. Cardiac pathologic findings reveal a high rate of sudden cardiac death of undetermined etiology in younger women. Ame Heart J. 2003;146:635–639. doi:10.1016/S0002-8703(03)00323-5
28. Olivotto I, Maron MS, Adabag AS, et al. Gender-related differences in the clinical presentation and outcome of hypertrophic cardiomyopathy. J Ame College Cardiol. 2005;46:480–487. doi:10.1016/j.jacc.2005.04.043
29. Liu G, Su L, Lang M. A systematic review and meta-analysis of sex differences in clinical outcomes of hypertrophic cardiomyopathy. Front Cardiovas Med. 2023;10:1252266.
30. Ho CY, Day SM, Ashley EA, et al. Genotype and lifetime burden of disease in hypertrophic cardiomyopathy. Circulation. 2018;138:1387–1398. doi:10.1161/CIRCULATIONAHA.117.033200
31. Savarese G, Lee H-J, Kim H-K, et al. Age-related sex differences in the outcomes of patients with hypertrophic cardiomyopathy. PLoS One. 2022;17:e0264580.
32. Alashi A, Smedira NG, Popovic ZB, et al. Characteristics and outcomes of elderly patients with hypertrophic cardiomyopathy. J Ame Heart Association. 2021;10:e018527.
33. Ghersin I, Bahouth F, Farah J, et al. P5550 The prognostic and therapeutic characteristics of heart failure among elderly patients with hypertrophic cardiomyopathy. Eur Heart J. 2019;40(Supplement_1):ehz746–0494
34. Fumagalli C, De Filippo V, Zocchi C, et al. Strength of clinical indication and therapeutic impact of the implantable cardioverter defibrillator in patients with hypertrophic cardiomyopathy. Int J Cardiol. 2022;353:62–67. doi:10.1016/j.ijcard.2022.01.022
35. Rattanawong P, Upala S, Riangwiwat T, et al. Atrial fibrillation is associated with sudden cardiac death: a systematic review and meta-analysis. J Interventional Cardiac Electrophysiol. 2018;51:91–104. doi:10.1007/s10840-017-0308-9
36. Wu S, Yang L, Sun N, et al. Impact of coronary artery disease in patients with hypertrophic cardiomyopathy. Hellenic Journal of Cardiology. 2024;77:27–35. doi:10.1016/j.hjc.2023.08.002
37. Ong KC, Geske JB, Hebl VB, et al. Pulmonary hypertension is associated with worse survival in hypertrophic cardiomyopathy. Eur Heart J Cardiovasc Imaging. 2016;17:604–610. doi:10.1093/ehjci/jew024
38. Kiaos A, Daskalopoulos GN, Kamperidis V, et al. Quantitative late gadolinium enhancement cardiac magnetic resonance and sudden death in hypertrophic cardiomyopathy. JACC. 2024;17:489–497. doi:10.1016/j.jcmg.2023.07.005
39. Todiere G, Nugara C, Gentile G, et al. Prognostic role of late gadolinium enhancement in patients with hypertrophic cardiomyopathy and low-to-intermediate sudden cardiac death risk score. Ame J Cardiol. 2019;124:1286–1292. doi:10.1016/j.amjcard.2019.07.023
40. Weng Z, Yao J, Chan RH, et al. Prognostic value of LGE-CMR in HCM. JACC: Cardiovascular Imaging. 2016;9:1392–1402. doi:10.1016/j.jcmg.2016.02.031
41. Nakamori S, Maron M, Rowin EJ, et al. Abstract 16793: the impact of late gadolinium enhancement on sudden death risk stratification in older patients with hypertrophic cardiomyopathy. Circulation. 2023;148:A16793–A16793.
42. Santos-Veloso MAO, Chaves ÂVF, Calado EB, et al. ICD indication in hypertrophic cardiomyopathy: which algorithm to use? Revista da Associação Médica Brasileira. 2022;68:1059–1063. doi:10.1590/1806-9282.20220199
43. Maron BJ, Rowin EJ, Maron MS. Evolution of risk stratification and sudden death prevention in hypertrophic cardiomyopathy: twenty years with the implantable cardioverter-defibrillator. Heart Rhythm. 2021;18:1012–1023. doi:10.1016/j.hrthm.2021.01.019
44. Maron BJ, Maron MS. Contemporary strategies for risk stratification and prevention of sudden death with the implantable defibrillator in hypertrophic cardiomyopathy. Heart Rhythm. 2016;13:1155–1165. doi:10.1016/j.hrthm.2015.12.048
45. Rowin EJ, Sridharan A, Madias C, et al. Prediction and prevention of sudden death in young patients (<20 years) with hypertrophic cardiomyopathy. Ame J Cardiol. 2020;128:75–83. doi:10.1016/j.amjcard.2020.04.042
46. Takagi E, Yamakado T, Nakano T. Prognosis of completely asymptomatic adult patients with hypertrophic cardiomyopathy. J Am Coll Cardiol. 1999;33(1):206–211. doi:10.1016/S0735-1097(98)00555-5
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




