Back to Journals » Therapeutics and Clinical Risk Management » Volume 21
AI-Assisted 3D Planning of CT Parameters for Personalized Femoral Prosthesis Selection in Total Hip Arthroplasty
Received 19 February 2025
Accepted for publication 25 May 2025
Published 18 June 2025 Volume 2025:21 Pages 905—916
DOI https://doi.org/10.2147/TCRM.S521755
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Tian-Jiao Yang, Wei Qian
Department of Orthopedics, Renmin Hospital of Hubei University of Medicine, Shiyan, Hubei, 442000, People’s Republic of China
Correspondence: Wei Qian, Email [email protected]
Objective: To investigate the efficacy of CT measurement parameters combined with AI-assisted 3D planning for personalized femoral prosthesis selection in total hip arthroplasty (THA).
Methods: A retrospective analysis was conducted on clinical data from 247 patients with unilateral hip or knee joint disorders treated at Renmin Hospital of Hubei University of Medicine between April 2021 and February 2024. All patients underwent preoperative full-pelvis and bilateral full-length femoral CT scans. The raw CT data were imported into Mimics 19.0 software to reconstruct a three-dimensional (3D) model of the healthy femur. Using 3-matic Research 11.0 software, the femoral head rotation center was located, and parameters including femoral head diameter (FHD), femoral neck length (FNL), femoral neck-shaft angle (FNSA), femoral offset (FO), femoral neck anteversion angle (FNAA), tip-apex distance (TAD), and tip-apex angle (TAA) were measured. AI-assisted THA 3D planning system AIJOINT V1.0.0.0 software was used for preoperative planning and design, enabling personalized selection of femoral prostheses with varying neck-shaft angles and surgical simulation. Groups were compared by gender, age, and parameters. ROC curves evaluated prediction efficacy.
Results: Females exhibited smaller FHD, FNL, FO, TAD, TAA but larger FNSA/FNAA vs males (P< 0.05). Patients > 65 years had higher FO, TAD, TAA (P< 0.05). TAD-TAA correlation was strong (r=0.954), while FNSA negatively correlated with TAD/TAA (r=− 0.773/-0.701). ROC analysis demonstrated high predictive accuracy: TAD (AUC=0.891, sensitivity=91.7%, specificity=87.6%) and TAA (AUC=0.882, sensitivity=100%, specificity=88.8%).
Conclusion: CT parameters (TAA, TAD, FNSA, FO) are interrelated and effective predictors for femoral prosthesis selection. Integration with AI-assisted planning optimizes personalized THA, reducing biomechanical mismatch risks.
Keywords: CT measurement parameters, total Hip arthroplasty, femoral prosthesis, personalized selection, impact study
Introduction
Total hip arthroplasty (THA) is a well-established orthopedic surgical technique widely employed to treat various hip joint disorders, including degenerative arthritis, femoral head necrosis, and traumatic arthritis.1,2 THA not only significantly alleviates pain but also restores hip joint function, thereby improving patients’ quality of life.3 However, despite its widespread application worldwide, achieving precise matching between the prosthesis and the patient’s anatomical structure remains a major clinical challenge. The degree of prosthesis-bone compatibility directly influences postoperative functional recovery and the long-term stability of the prosthesis.4 Poor prosthesis matching may result in issues such as prosthesis loosening, stress shielding, and bone loss, increasing the risk of revision surgeries.5 Particularly, the complexity of the hip joint anatomy poses higher demands on prosthesis design and selection, given the variability in femoral anatomical features.6 Conducting studies on personalized prosthesis selection based on individual anatomical characteristics is therefore essential, not only to enhance surgical success rates but also to reduce postoperative complications.
Traditional preoperative prosthesis selection typically relies on two-dimensional (2D) X-ray imaging combined with the surgeon’s experience. While this approach is operationally feasible, the limited information provided by 2D imaging makes it challenging to accurately reflect the 3D anatomical features of the femur.7 This limitation can result in suboptimal prosthesis design and compatibility, hindering load transfer and joint function recovery. In recent years, with the rapid advancement of computer-assisted and medical imaging technologies, high-resolution CT scanning and 3D reconstruction techniques have enabled more precise measurements of key femoral anatomical parameters. These technologies comprehensively capture individual anatomical characteristics, providing more scientific data to support preoperative planning.8 Recent studies have further validated the efficacy of 3D CT-based planning in improving implant size prediction accuracy. For instance, Huo et al demonstrated that artificial intelligence (AI)-driven 3D preoperative planning significantly enhanced the precision of femoral stem sizing in THA, reducing intraoperative adjustments and improving biomechanical compatibility.9 Similarly, 3D CT templating has proven effective in robot-assisted total knee arthroplasty, achieving superior alignment and implant sizing outcomes.10
Studies11 have demonstrated significant individual variability in femoral anatomical parameters, influenced by factors such as gender and age. Furthermore, complex interrelationships exist among multiple anatomical parameters, but their specific implications for prosthesis design and personalized selection require further investigation. Against this backdrop, this study retrospectively analyzed the clinical data of 247 patients with unilateral hip or knee joint disorders treated at Renmin Hospital of Hubei University of Medicine. It explored the variations in CT-measured anatomical parameters across genders and age groups and analyzed their correlations with prosthesis selection. In addition, ROC curves were employed to quantify the predictive efficacy of CT parameters for prosthesis type selection. By improving preoperative accuracy, this approach may mitigate complications such as aseptic loosening and stress shielding, thereby reducing revision rates—a critical consideration given the impact of prosthesis mismatch on surgical outcomes.12
While 3D CT and AI-assisted planning show promise, their translation into diverse clinical settings requires addressing challenges such as variations in imaging protocols and integration with hospital workflows. These considerations further underscore the need for standardized guidelines and robust preoperative parameters, as explored in this study. The aim of this study was to provide more precise guidance for preoperative planning and personalized femoral prosthesis selection in THA, thereby optimizing postoperative outcomes.
Materials and Methods
Basic Information
This study retrospectively analyzed the clinical data of 247 consecutively enrolled patients with unilateral hip or knee joint lesions treated in Renmin Hospital of Hubei University of Medicine from April 2021 to February 2024. To minimize selection bias, all eligible patients meeting inclusion criteria within the study period were included, and exclusion criteria were strictly applied by two independent investigators. Among the enrolled patients, there were 82 males and 165 females, with ages ranging from 21 to 85 years and an average age of (65.07 ± 8.94) years. The body mass index (BMI) ranged from 21.29 to 41.87 kg/m², with an average of (27.59 ± 4.16) kg/m². The specific case distribution was as follows: 152 cases of knee joint disease, including 83 in the left knee and 69 in the right knee, all diagnosed as knee osteoarthritis; 95 cases of hip joint disease, including 44 in the left hip and 51 in the right hip, comprising 12 cases of hip osteoarthritis, 36 cases of femoral head necrosis, and 47 cases of femoral neck fractures. Among the study population, 61 patients had hypertension, 30 had diabetes, and 18 had a history of cerebral ischemia or previous cerebral infarction. The patients were divided into groups based on sex and age: sex-based groups included the male group and female group, and age-based groups included the ≤65 years group (n=111) and the >65 years group (n=136). This study was approved by the Medical Ethics Committee of Renmin Hospital of Hubei University of Medicine (Ethics Approval Number: Lunzhun 2024031), and was conducted in strict accordance with the Declaration of Helsinki and relevant medical ethical guidelines. Informed consent was obtained from all study participants.
Inclusion and Exclusion Criteria
Inclusion Criteria
① Lesions confined to a unilateral hip or knee joint, with intact and normal anatomical structure of the contralateral hip and knee joints; ② Patients aged ≥18 years, regardless of gender; ③ All participants completed preoperative CT scans of the entire pelvis and full-length femurs of both legs.
Exclusion Criteria
① A clear history of trauma, surgery, or anatomical abnormalities (eg, deformity or dysplasia) in the contralateral hip joint, including the acetabulum or proximal femur; ② Significant bone hyperplasia, wear, or defects in the medial, lateral, or posterior condyles of the contralateral knee joint, or developmental abnormalities; ③ CT image quality not meeting study requirements, such as artifacts causing measurement errors or unclear imaging.
CT Scanning and Reconstruction of the Three-Dimensional Model of the Healthy Femur
A 128-slice spiral CT scanner from Philips, Netherlands, was used to scan and reconstruct three-dimensional models of the healthy femur. During scanning, patients were placed in a supine position with both legs fully extended and knees in a naturally straightened state. The scanning range covered the full length from the superior edge of the pelvis to the femoral condyles on both sides, including the entire anatomical structure of the hip joint and femur. The scanning parameters were set as follows: tube voltage 120 kV, tube current in a 3D auto-adjustment mode with an average of 250 mAs, pitch 1.20 mm, single rotation time 0.5 seconds, collimation 64×0.625, slice thickness 2.0 mm, and slice spacing 1.0 mm. After scanning, all original CT data were stored in DICOM format for subsequent processing and model construction.
The collected CT raw data were imported into Mimics 19.0 software (Materialise, Belgium; version 19.0.0.406). Using the threshold segmentation function (Hounsfield Unit range: 150–3000), the healthy femur and its medullary cavity were segmented for each patient. To ensure reproducibility across software platforms, segmentation thresholds and geometric fitting algorithms followed manufacturer-recommended protocols for bone tissue analysis. In cases where incomplete imaging regions were found during segmentation, the software’s completion function was employed to ensure the integrity of the femoral and medullary cavity anatomy. The medullary cavity region was filled with solid material to restore its normal anatomical structure. The three-dimensional models of the femur and medullary cavity were then optimized for surface smoothing to remove artifacts or spurs, improving surface flatness and accuracy to ensure model applicability for subsequent analysis.
Upon completing the model processing, the femur and medullary cavity models were exported in STL format and further adjusted using 3-matic Research 11.0 software (Materialise, Belgium; version 11.0.0.2). The models were aligned in three-dimensional space such that the line connecting the lowest points of the medial and lateral posterior condyles was parallel to the coronal plane. Additionally, the posterior condyles and the lowest point of the lesser trochanter were positioned on the same plane, while the femoral anatomical axis was adjusted to be perpendicular to the horizontal plane, ensuring standardized spatial positioning of the 3D models.
Anatomical Measurement Parameters and Methods of the Healthy Femur
Using 3-matic Research 11.0 software, a series of precise anatomical parameters of the reconstructed 3D femoral models were measured. The specific methods and parameter definitions were as follows: ① FHC and FHD: The “Best-Fit Sphere” function of the software was used to perform 3D fitting on the femoral head surface, generating a sphere that best matched the femoral head. The sphere’s center was defined as the FHC, and its diameter as the FHD. ② FNL: Two uniform cross-sections with a diameter of 5 mm were selected in the femoral neck region. The geometric centers of these cross-sections were calculated and connected by a line to form the femoral neck axis. In the proximal femur, within 20 cm below the apex of the greater trochanter, the medullary cavity segment was identified, and the center axis of this segment was determined using the “Create Line” function with the “Fit Ruled Surface Direction” algorithm. The distance from FHC to the intersection of the femoral neck axis and the medullary cavity center axis was defined as the FNL. ③ FNSA: The angle between the femoral neck axis and the center axis of the proximal third of the femoral medullary cavity was measured to determine the FNSA. ④ FO: The vertical distance from FHC to the center axis of the proximal third of the femoral medullary cavity was defined as FO, reflecting the spatial relationship between the femoral head and the femoral axis. ⑤ FNAA: Defined as the angle between the femoral neck axis and the line connecting the lowest points of the medial and lateral posterior condyles. This parameter was measured in combination with the anatomical axis and joint plane of the femur to ensure accuracy. ⑥ TAD: A perpendicular line was drawn from the apex of the greater trochanter to the center axis of the proximal femoral medullary cavity. The vertical distance from FHC to this line was defined as the TAD. TAD was recorded as positive if the femoral head center was below the apex of the greater trochanter and negative if above. ⑦ TAA: The angle between the line connecting the apex of the greater trochanter and FHC and a line perpendicular to the center axis of the proximal femoral medullary cavity was defined as the TAA, describing the spatial relationship between the greater trochanter and femoral head.
Measurement Procedure and Data Processing: All parameters were independently measured twice by two experienced orthopedic attending physicians, with a one-month interval between the two measurements to reduce subjective errors. The average value of each physician’s measurements was taken, and the final measurement data were calculated as the combined average of both physicians’ results. Inter-rater reliability was assessed using intraclass correlation coefficients (ICC), with all parameters achieving ICC > 0.85, indicating excellent agreement.
Preoperative Planning and Surgical Simulation
This study utilized the AI-assisted THA 3D planning system (AIJOINT V 1.0.0.0, Beijing Changmugu Medical Technology Co., Ltd). to conduct preoperative planning and surgical simulation for the pelvis and bilateral femurs of 247 patients. To address potential software dependency limitations, all AI algorithms (eg, G-NET convolutional neural network) were validated against manual measurements in a pilot cohort of 30 patients, achieving >90% concordance in landmark identification. Firstly, the original CT scan data of the pelvis and full-length femur were imported into the system. Using the convolutional neural network (G-NET) based on deep learning, the system automatically identified and segmented the skeletal regions in the CT images, rapidly capturing and marking anatomical landmarks such as the iliac crest, anterior superior iliac spine, pubic symphysis, greater trochanter, lesser trochanter, and ischial tuberosity. Subsequently, the system corrected the pelvis to a neutral position based on the spatial positions of these anatomical landmarks relative to the horizontal plane and the body’s central axis. Lateral tilt correction was achieved by aligning the line connecting the bilateral anterior superior iliac spines with the horizontal plane. Rotational correction relied on ensuring parallelism of the inferior edges of the bilateral teardrop shapes and symmetry of obturator foramen morphology. Anterior-posterior tilt correction was performed by aligning the pelvic anterior plane, determined by the bilateral anterior superior iliac spines and the pubic symphysis, with the coronal plane. After the pelvis was corrected to a neutral position, the system intelligently calculated the eccentricity difference (FO difference) between the bilateral acetabula and the limb length discrepancy. It also generated a standardized corrected pelvic and bilateral hip joint anteroposterior X-ray image to provide precise preoperative prosthesis matching references.
For the 3D model of the affected limb, the system selected the Pinnacle acetabular cup and Corail femoral stem (including two neck-shaft angles: 125° and 135°) produced by DePuy, USA, as prosthetic templates. Using the pelvis-corrected coordinate system, the software simulated the placement of the acetabular cup prosthesis at a 40° abduction and 25° anteversion. By applying computer graphics algorithms, the software fitted the acetabular morphology, calculated its rotational center and radius, and positioned the acetabular cup to the preset angle and depth. For the femoral stem, the system matched an appropriate size based on the diameter of the femoral medullary cavity and precisely determined the prosthesis insertion depth. It also simulated the osteotomy process of the femoral neck. Using intelligent segmentation algorithms, the system removed data from the femoral head and neck after osteotomy and measured the distance from the osteotomy line to the upper edge of the lesser trochanter to provide intraoperative guidance. To further optimize postoperative limb length discrepancy and FO difference, the AIJOINT software combined templates of femoral head prostheses of different lengths to calculate and adjust, in real time, the bilateral hip joint eccentricity and limb length discrepancy under various schemes. Through iterative adjustments, the final goal was achieved, ensuring both the limb length discrepancy and FO difference were ≤5 mm, thereby meeting the standard for optimal postoperative balance.
Observation Indicators
① Differences in CT-measured parameters: Observed in the three-dimensional model of the healthy femur across different genders and age groups, along with their correlations. ② Grouping by femoral stem type: Patients were divided into Group A (135° Corail) and Group B (125° Corail) based on the femoral stem type selected in preoperative planning and simulated surgery. Differences in baseline characteristics such as gender, age, height, weight, and body mass index (BMI), as well as CT-measured parameters, were compared between the two groups. ③ Selection efficacy analysis: Receiver operating characteristic (ROC) curve analysis was used to evaluate the effectiveness of rotational CT-measured parameters in selecting THA femoral prosthesis types.
Statistical Methods
Statistical analyses were performed using SPSS 23.0 (IBM Corp., Armonk, NY) and R 4.3.1.0 (R Foundation for Statistical Computing, Vienna, Austria). Continuous variables with normal distribution were expressed as ( ), and intergroup comparisons were conducted using the independent sample t-test or one-way ANOVA. Categorical variables were expressed as n (%), and intergroup comparisons were performed using the chi-square test. To address potential confounding factors in the retrospective design, multivariable logistic regression adjusting for age, sex, and BMI was performed. Correlations between variables were assessed using Pearson analysis, where r > 0 indicates positive correlation, r < 0 indicates negative correlation, |r| < 0.20 is very low, 0.20 ≤ |r| < 0.40 is weak, 0.40 ≤ |r| < 0.60 is moderate, 0.60 ≤ |r| < 0.80 is strong, and |r| ≥ 0.80 is very strong. ROC curves were used to evaluate the diagnostic efficacy of CT parameters in femoral prosthesis selection. Measurement consistency was assessed using ICC (two-way random effects model for absolute agreement), with ICC < 0.40 indicating poor, 0.40–0.75 indicating moderate, and ICC > 0.75 indicating good. A P-value < 0.05 was considered statistically significant.
), and intergroup comparisons were conducted using the independent sample t-test or one-way ANOVA. Categorical variables were expressed as n (%), and intergroup comparisons were performed using the chi-square test. To address potential confounding factors in the retrospective design, multivariable logistic regression adjusting for age, sex, and BMI was performed. Correlations between variables were assessed using Pearson analysis, where r > 0 indicates positive correlation, r < 0 indicates negative correlation, |r| < 0.20 is very low, 0.20 ≤ |r| < 0.40 is weak, 0.40 ≤ |r| < 0.60 is moderate, 0.60 ≤ |r| < 0.80 is strong, and |r| ≥ 0.80 is very strong. ROC curves were used to evaluate the diagnostic efficacy of CT parameters in femoral prosthesis selection. Measurement consistency was assessed using ICC (two-way random effects model for absolute agreement), with ICC < 0.40 indicating poor, 0.40–0.75 indicating moderate, and ICC > 0.75 indicating good. A P-value < 0.05 was considered statistically significant.
Results
Consistency Analysis
The consistency of measurements obtained by two physicians showed ICC values > 0.75, indicating good consistency.
Measurements of the Contralateral Femur in 3D Models and Their Comparisons Across Genders and Age Groups
Gender Differences: Female patients showed significantly smaller FHD, FNL, FO, TAD, and TAA compared to male patients, while FNSA and FNAA were significantly larger in females (P < 0.05). Age Differences: Patients aged > 65 years exhibited significantly larger FO, TAD, and TAA compared to those aged ≤ 65 years (P < 0.05). However, there were no significant differences in FHD, FNL, FNSA, or FNAA between the two age groups (P > 0.05). Details are shown in Tables 1 and 2.
 |
Table 1 Comparison of Measurements of Contralateral Femoral 3D Models by Gender ( |
 |
Table 2 Comparison of Measurements of Contralateral Femoral 3D Models by Age ( |
Correlation Analysis of Anatomical Measurements of Contralateral Femur
Pearson correlation analysis revealed the following relationships: TAD was strongly positively correlated with TAA (r = 0.954, P < 0.001) and moderately positively correlated with FO (r = 0.527, P < 0.01). TAA was weakly positively correlated with FO (r = 0.393, P < 0.001). FNSA showed strong negative correlations with FO, TAA, and TAD (r = −0.669, −0.701, −0.773, respectively; P < 0.001). Details are shown in Table 3 and Figures 1–3.
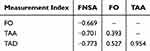 |
Table 3 Correlation Analysis Among Anatomical Measurements of Contralateral Femur |
 |
Figure 1 Correlation Analysis Between FO, TAA, TAD, and FNSA. |
 |
Figure 2 Correlation Analysis Between TAA, TAD, and FO. |
 |
Figure 3 Correlation Analysis Between TAD and TAA. |
Comparison of Observational Indicators Among Different Femoral Stem Types
Based on preoperative planning and simulated surgery for femoral stem type matching, Group A (135° Corail) included 111 cases, and Group B (125° Corail) included 136 cases. Significant differences were observed in age, FNSA, FO, TAD, and TAA between the two groups (P < 0.05), as shown in Table 4.
 |
Table 4 Comparison of Observational Indicators Among Different Femoral Stem Types ( |
Efficiency of CT Parameters in Selecting THA Femoral Prosthesis Types
The ROC curves for CT parameters in selecting femoral prosthesis types in THA showed that the AUC values of FNSA, FO, TAD, and TAA were 0.794, 0.825, 0.891, and 0.882, respectively. The optimal cutoff values, sensitivity, and specificity are presented in Table 5 and Figure 4.
 |
Table 5 Efficiency of CT Parameters in Selecting THA Femoral Prosthesis Types |
 |
Figure 4 ROC Curve for Efficiency of CT Parameters in Selecting THA Femoral Prosthesis Types. |
Discussion
Advantages of Using 3D Reconstructed Femoral Models for Measuring Anatomical Parameters
In THA, accurately restoring the proximal femoral anatomy is crucial for reconstructing postoperative hip joint function and maintaining soft tissue tension balance.13 Among these parameters, the FNSA and FO serve as key anatomical indicators, playing a central role in hip prosthesis design and implantation.14,15 However, traditional two-dimensional (2D) imaging methods, such as X-rays, are prone to being influenced by patient positioning and projection angles.16 As early as 2000, Kay et al17 reported that a mere 7° external rotation of the femur could lead to an FNSA measurement deviation exceeding 10°, highlighting the limitations of 2D imaging in terms of accuracy. To address this issue, this study employed CT scans combined with three-dimensional (3D) reconstruction technology to establish 3D models of the contralateral femur, enabling precise measurement of parameters such as FNSA, FO, FHD, and FNL. This approach effectively eliminates data deviation caused by projection angle errors, thereby improving measurement objectivity and reliability.
Current Research Status of Imaging Measurements for Femoral Anatomical Parameters
In recent years, imaging measurements of femoral anatomical parameters have played an important role in preoperative evaluations and postoperative outcome optimization in THA. Studies18–20 have indicated that differences in countries, regions, and measurement techniques (eg, X-ray versus CT) result in significant variations in FNSA and FO measurements. The range of FNSA measurements is approximately 123.1°–129.5°, while FO generally falls between 33.6 mm and 43.0 mm. In this study, the measured values of FNSA and FO align well with previously reported data, demonstrating high consistency with earlier research. Studies based on CT reconstruction technology are gradually becoming mainstream. For example, Carmona et al21 analyzed the proximal femora of 628 healthy French adults through 3D modeling and investigated the effects of gender, age, and ethnicity on anatomical parameters. The results indicated that males had lower FNSA and FNAA than females, while FO was significantly higher in males (P < 0.001). Moreover, the study revealed dynamic changes in anatomical parameters with age: FNSA increased gradually, while FO decreased with age, possibly due to age-related declines in bone density causing continuous morphological changes. Other studies have further explored the impact of age stratification on anatomical parameters. For instance, Jiawei et al22 measured parameters such as FHD, FNSA, and FO based on full-length femoral CT images of 236 healthy individuals, grouped by age (<60 years, 60–69 years, 70–79 years, and >80 years). The results showed that FNSA decreased with age, while FO differences between age groups were not statistically significant (P > 0.05). Additionally, the study noted that, regardless of age group, males had significantly higher FHD and FO than females (P < 0.05). These findings further underscore the anatomical challenges that elderly males may face during THA. Specifically, smaller FNSA and larger FO may necessitate femoral prostheses designed to better align with individual anatomical characteristics. In this study, FHD, FNSA, FNAA, and FO were all found to exhibit gender differences, consistent with previous literature. However, when subjects were divided into two groups based on age (≤65 years and >65 years), only FO was significantly higher in the older group (P < 0.05), while differences in FNSA and FNAA between age groups were not statistically significant (P > 0.05). These results differ from some prior research, potentially due to a relatively small sample size and coarse age stratification.
TAD is another hip reconstruction parameter of considerable interest, used to evaluate the alignment between the greater trochanter apex and the femoral head center.23 Kumar et al24 conducted 2D measurements of TAD in standard bilateral hip anteroposterior X-rays of 175 Indian patients, reporting a range of −2.6 mm to 38 mm. The authors emphasized referencing the contralateral hip’s TAD during surgery to avoid postoperative discrepancies in limb length. In this study, the TAD of 247 patients ranged from −6.84 mm to 27.75 mm, consistent with the aforementioned research, further underscoring the critical importance of accurate preoperative TAD measurements for surgical planning. In summary, key anatomical parameters such as FNSA, FO, and TAD exhibit significant individual variability among patients. This variability suggests that a single FNSA-designed femoral prosthesis may not fully meet surgical demands. Therefore, how to integrate imaging measurement results to precisely match individual anatomical characteristics remains an urgent area for future exploration in prosthesis design and clinical applications.
Feasibility of Using TAA and TAD for Preoperative Selection of Femoral Prostheses in THA
As traditional anatomical parameters, FNSA and FO have long occupied an important position in femoral prosthesis design. Previous studies25,26 have confirmed the significant correlation between FNSA and FO and their profound impact on postoperative functional recovery and mechanical stability. Boese et al27 conducted 3D reconstructions of proximal femurs in 400 patients using CT imaging, identifying a sine function relationship between FO, FNL, and FNSA (sin FNSA = FO/FNL), thereby elucidating the geometric association between FNSA and FO from a mathematical perspective. Another study by Yi et al,28 based on 3D CT reconstruction of the Chinese population, identified a negative correlation between FNSA and FO, with correlation coefficients of −0.262 for males and −0.350 for females. These findings provide theoretical support for individualized prosthesis selection. However, traditional imaging evaluation methods still have limitations in clinical practice. X-rays are the most commonly used tool for preoperative evaluation, but due to improper patient positioning or variations in imaging projection angles, FNSA and FO measurements are often constrained. Additionally, changes in X-ray magnification may affect the accuracy of TAD measurements, further limiting the application value of traditional parameters in precise preoperative evaluations. To address these issues, this study introduces the TAA and explores its feasibility and potential application in femoral prosthesis selection. TAA, as a geometric angle parameter, is simple to measure without requiring corrections for imaging magnification. It is easy to measure both in 2D X-ray planes and 3D CT spaces and exhibits higher measurement stability and operational convenience compared to FNSA and FO. This study systematically analyzed the correlations among TAA, TAD, FO, and FNSA, revealing significant negative correlations between TAA and FNSA, significant positive correlations between TAA and FO, and strong positive correlations between TAA and TAD. These findings validate TAA as a reliable evaluation parameter. Furthermore, TAD was positively correlated with FO and negatively correlated with FNSA, providing data support for TAD’s clinical application. These results suggest that TAA and TAD have high applicability in the geometric relationships of anatomical parameters and can serve as important preoperative evaluation tools to replace FNSA and FO. By accurately assessing preoperative femoral anatomy, TAA and TAD can not only enhance the matching of prosthesis design to individual anatomical characteristics but also significantly reduce the risk of postoperative complications arising from measurement errors in traditional methods.
CT Measurement Parameters and Their Efficacy in the Selection of Femoral Prostheses with Different FNSA Designs
In recent years, artificial intelligence-assisted preoperative planning software has demonstrated significant advantages in prosthesis selection, positioning accuracy, and optimization of intraoperative decision-making.9 Preoperative planning using AIJOINT software not only enables efficient selection of appropriate prosthesis types and sizes but also achieves ideal results in reconstructing limb length equality and optimizing FO.29 In this study, preoperative planning guided by AIJOINT software was performed, utilizing the Corail femoral stem prosthesis. Results showed that the differences in bilateral limb lengths and FO were controlled within 5 mm, consistent with previous research findings.30 This validates the software’s outstanding performance in surgical simulation accuracy and efficiency, laying the foundation for evaluating the efficacy of CT measurement parameters in prosthesis selection. The study results indicate that when using femoral stem prostheses with different FNSA designs (135° and 125° Corail), there were significant differences in patients’ FNSA, FO, TAD, and TAA parameters (P < 0.05). Analysis using ROC curves showed that FNSA, FO, TAD, and TAA demonstrated high sensitivity, specificity, and AUC in prosthesis type selection, further highlighting the critical value of these CT measurement parameters in preoperative imaging evaluation and prosthesis design selection. Notably, by establishing optimal critical values, these parameters can provide reliable references for precise femoral prosthesis selection in THA. However, this study’s significant premise assumes that the acetabular prosthesis position has achieved an optimal reconstruction of the rotational center during planning. In cases where intraoperative abnormalities such as superior, lateral, or inferior displacement of the acetabular rotational center occur, inconsistencies in the rotational center heights of both hip joints may arise.31 This could render the CT measurement parameters of the unaffected femur non-referential. Under such circumstances, relying solely on unaffected side parameters for prosthesis selection may be unsuitable.
This study also has certain limitations: ① As a retrospective study with cases derived from a single center and a limited sample size, the generalizability of the findings may be restricted. ② The study only included patients with at least one anatomically normal hip joint. For cases with femoral developmental abnormalities or significant anatomical alterations, difficulty in identifying anatomical landmarks could result in measurement bias. ③ This study only evaluated femoral stem prostheses with 125° and 135° FNSA designs. Further research is required for prostheses with other angular designs. ④ The data were based solely on preoperative CT 3D reconstruction images of the entire unaffected femur. ⑤ While our focus was on femoral parameters (TAA, TAD, FNSA, FO), the study did not evaluate the accuracy of 3D CT in predicting acetabular component sizing. Future research should integrate acetabular morphology analysis to provide a comprehensive preoperative planning framework. For patients with normal bilateral hip joints but knee joint pathologies, the study methodology remains a surgical simulation, and its clinical accuracy and applicability require further validation. Future research should expand the sample size, collect more cases through multi-center studies, and conduct comprehensive validations of the reliability and practicality of CT measurement parameters by comparing preoperative simulations with postoperative actual CT measurements. Additionally, exploring the applicability of these parameters across different races, genders, and anatomical variations is essential. Combining these findings with further optimization of artificial intelligence-assisted planning systems will provide more comprehensive support for personalized prosthesis selection and postoperative functional recovery. Prospective studies are particularly needed to eliminate retrospective design biases and validate the generalizability of TAA/TAD-based planning.
Conclusion
In conclusion, constructing 3D femoral models based on CT data enables more accurate measurement of multiple anatomical parameters (TAA, TAD, FNSA, FO), providing scientific evidence for selecting prostheses with different FNSA designs. The quantitative thresholds derived from ROC analysis (eg, TAA cutoff of 12.57°, TAD of 10.51 mm) offer actionable clinical benchmarks. Surgeons can directly apply these values during preoperative planning to objectively categorize patients into 125° or 135° femoral stem groups, reducing reliance on subjective experience. By integrating intelligent planning software such as AIJOINT, these parameters serve as critical reference indicators, supporting personalized THA design and precise treatment. The enhanced preoperative accuracy may significantly reduce postoperative complications such as aseptic loosening (attributable to biomechanical mismatch) and leg length discrepancy. Improved prosthesis-bone compatibility could mitigate stress shielding risks, potentially lowering revision rates—a key consideration given that up to 30% of early revisions are linked to implant malposition.12 These findings align with the paradigm shift toward personalized medicine in orthopedics, where AI-driven 3D planning bridges anatomical variability with standardized implant solutions. As next-generation surgical technologies evolve, integrating CT-based geometric parameters into automated planning systems will further optimize individualized care, setting a foundation for predictive analytics in joint arthroplasty.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Scott CEH, Clement ND, Davis ET, et al. Modern total hip arthroplasty: peak of perfection or room for improvement? Bone Joint J. 2022;104-b(2):189–192. doi:10.1302/0301-620X.104B2.BJJ-2022-0007
2. Solasz S, Ganta A, Egol KA, et al. Acute total hip replacement for geriatric acetabular fracture: anterior intrapelvic approach + posterolateral approach. J Orthop Trauma. 2023;37(8s):S5–s6. doi:10.1097/BOT.0000000000002633
3. Courtine M, Bourredjem A, Gouteron A, et al. Functional recovery after total hip/knee replacement in obese people: a systematic review. Ann Phys Rehabil Med. 2023;66(1):101710. doi:10.1016/j.rehab.2022.101710
4. Roe SC, Marcellin-Little D. Stem selection for total Hip replacement. Vet Surg. 2022;51(3):383. doi:10.1111/vsu.13792
5. Perticarini L, Rossi SMP, Benazzo F. Unstable total hip replacement: why? Clinical and radiological aspects. Hip Int. 2020;30(2_suppl):37–41. doi:10.1177/1120700020971725
6. Soliman MM, Islam MT, Chowdhury MEH, et al. Advancement in total hip implant: a comprehensive review of mechanics and performance parameters across diverse novelties. J Mater Chem B. 2023;11(44):10507–10537. doi:10.1039/D3TB01469J
7. Ampadi Ramachandran R, Lee C, Zhang L, et al. Total hip replacement monitoring: numerical models for the acoustic emission technique. Med Biol Eng Comput. 2022;60(5):1497–1510. doi:10.1007/s11517-022-02548-6
8. Ramesh A, Di Laura A, Henckel J, et al. The variability of CT scan protocols for total hip arthroplasty: a call for harmonisation. EFORT Open Rev. 2023;8(11):809–817. doi:10.1530/EOR-22-0141
9. Huo J, Huang G, Han D, et al. Value of 3D preoperative planning for primary total hip arthroplasty based on artificial intelligence technology. J Orthop Surg Res. 2021;16(1):156. doi:10.1186/s13018-021-02294-9
10. Londhe SB, Shetty S, Vora NL, et al. Efficacy of the pre-operative three-dimensional (3D) CT scan templating in predicting accurate implant size and alignment in robot assisted total knee arthroplasty. Indian J Orthop. 2022;56(12):2093–2100. doi:10.1007/s43465-022-00742-0
11. Migliorini F, Cuozzo F, Oliva F, et al. CT-based navigation for total hip arthroplasty: a meta-analysis. Eur J Med Res. 2023;28(1):443. doi:10.1186/s40001-023-01437-4
12. Bozic KJ, Lau E, Ong K, et al. Risk factors for early revision after primary total hip arthroplasty in medicare patients. Clin Orthop Relat Res. 2014;472(2):449–454. doi:10.1007/s11999-013-3081-9
13. Gaujac N, Sariali E, Grimal Q. Does the bone mineral density measured on a preoperative CT scan before total Hip arthroplasty reflect the bone’s mechanical properties? Orthop Traumatol Surg Res. 2023;109(1):103348. doi:10.1016/j.otsr.2022.103348
14. Pornrattanamaneewong C, Ruangsomboon P, Wingprawat K, et al. Accuracy of empirical distal femoral valgus cut angle of 4° to 6° in total knee arthroplasty: a randomized controlled trial. Eur J Orthop Surg Traumatol. 2022;32(1):175–181. doi:10.1007/s00590-021-02890-9
15. Fujita M, Hayashi S, Kamenaga T, et al. Ligament preserving total hip arthroplasty prevents different leg length and femoral offset. Acta Ortop Bras. 2022;30(spe1):e242758. doi:10.1590/1413-785220223001e242758
16. Palit A, King R, Pierrepont J, et al. Development of bony range of motion (B-ROM) boundary for total Hip replacement planning. Comput Methods Programs Biomed. 2022;222:106937. doi:10.1016/j.cmpb.2022.106937
17. Kay RM, Jaki KA, Skaggs DL. The effect of femoral rotation on the projected femoral neck-shaft angle. J Pediatr Orthop. 2000;20(6):736–739. doi:10.1097/01241398-200011000-00007
18. Liu Z, Song K, Jiang Q, et al. [Analysis of factors associated with the influence of femoral stem anteversion after total Hip arthroplasty]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2023;37(9):1075–1080. Danish. doi:10.7507/1002-1892.202304063
19. Wells J, Nepple JJ, Crook K, et al. Femoral morphology in the dysplastic hip: three-dimensional characterizations with CT. Clin Orthop Relat Res. 2017;475(4):1045–1054. doi:10.1007/s11999-016-5119-2
20. Darwich A, Geiselhardt C, Bdeir M, et al. Anthropometry of the proximal femur and femoral head in children/adolescents using three-dimensional computed tomography-based measurements. Surg Radiol Anat. 2021;43(12):2009–2023. doi:10.1007/s00276-021-02841-3
21. Carmona M, Tzioupis C, LiArno S, et al. Upper femur anatomy depends on age and gender: a three-dimensional computed tomography comparative bone morphometric analysis of 628 healthy patients’ hips. J Arthroplasty. 2019;34(10):2487–2493. doi:10.1016/j.arth.2019.05.036
22. Jiawei L, Kai Z, Haiyan W, et al. Digital measurement and clinical significance of proximal femur in the older people of Inner Mongolia population, China. BMC Geriatr. 2023;23(1):632. doi:10.1186/s12877-023-04254-w
23. Kumar AJ, Parmar VN, Kolpattil S, et al. Significance of hip rotation on measurement of ‘tip apex distance’ during fixation of extracapsular proximal femoral fractures. Injury. 2007;38(7):792–796. doi:10.1016/j.injury.2006.12.002
24. Kumar A, Passey J, Kumar M, et al. Reliability of relation between greater trochanter and center of rotation of femoral head in Indian population. J Clin Orthop Trauma. 2020;11(Suppl 4):S522–s525. doi:10.1016/j.jcot.2020.04.017
25. Qin S, Li M, Jia Y, et al. How do the morphological abnormalities of femoral head and neck, femoral shaft and femoral condyle affect the occurrence and development of medial knee osteoarthritis. Orthop Surg. 2023;15(12):3174–3181. doi:10.1111/os.13910
26. Çukurlu M, Karagoz B, Keceli O. The effect of pre-fracture proximal femur geometry on hip fracture type in elderly patients. Medicine. 2023;102(19):e33622. doi:10.1097/MD.0000000000033622
27. Boese CK, Dargel J, Jostmeier J, et al. Agreement between proximal femoral geometry and component design in total hip arthroplasty: implications for implant choice. J Arthroplasty. 2016;31(8):1842–1848. doi:10.1016/j.arth.2016.02.015
28. Yi LH, Li R, Zhu Z-Y, et al. Anatomical study based on 3D-CT image reconstruction of the hip rotation center and femoral offset in a Chinese population: preoperative implications in total hip arthroplasty. Surg Radiol Anat. 2019;41(1):117–124. doi:10.1007/s00276-018-2143-9
29. Chen X, Liu X, Wang Y, et al. Development and validation of an artificial intelligence preoperative planning system for total hip arthroplasty. Front Med. 2022;9:841202. doi:10.3389/fmed.2022.841202
30. Li S, Liu X, Chen X, et al. Development and validation of an artificial intelligence preoperative planning and patient-specific instrumentation system for total knee arthroplasty. Bioengineering. 2023;10(12):1417. doi:10.3390/bioengineering10121417
31. Prabowo Y, Alhuraiby SS, Putera GU, et al. Acetabular reconstruction with total hip replacement and femoral head autograft following pelvic resection of malignant bone tumour: a case report. Int J Surg Case Rep. 2022;96:107267. doi:10.1016/j.ijscr.2022.107267
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




