Back to Journals » Drug Design, Development and Therapy » Volume 19
Alfentanil Enhanced the Sedation of Remimazolam During Anaesthesia Induction in Patients Undergoing Urological Day Surgery: A Randomised Controlled Trial
Authors Lin Y, Chen Q, Liao Y, Xu B, Zhang C, Luo J, Liu S, Wu X, Guan X
Received 27 November 2024
Accepted for publication 21 June 2025
Published 3 July 2025 Volume 2025:19 Pages 5653—5662
DOI https://doi.org/10.2147/DDDT.S508941
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Manfred Ogris
Yuliu Lin,1,* Qiuling Chen,1,* Yeqing Liao,1,* Bing Xu,2 Cuiwen Zhang,1 Jiaxin Luo,1 Susu Liu,1 Xiaoshan Wu,1 Xuehai Guan1
1Department of Anaesthesiology, the First Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, 530021, People’s Republic of China; 2Department of Rehabilitation, the People`s Hospital of Guangxi Zhuang Autonomous Region, Nanning, Guangxi, 530021, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xuehai Guan, Department of Anaesthesiology, the First Affiliated Hospital of Guangxi Medical University, 6 Shuangyong Road, Nanning, Guangxi, 530021, People’s Republic of China, Tel +86-771-5356250, Email [email protected]
Background: Remimazolam is a novel benzodiazepine sedative agent. Combining opioids with sedatives exerts a synergistic effect. The aim is to investigate whether alfentanil enhances sedative effects of remimazolam during anaesthesia induction in patients undergoing urological day surgery.
Methods: This was a single-centre, single-blinded, randomised clinical trial. The study was conducted between 1 September 2022 and 31 December 2023. We included 114 patients undergoing urological day surgery under general anaesthesia. Patients were randomly assigned to the RMZ-AF or AF-RMZ group (n=57). During induction, the RMZ-AF group received remimazolam then alfentanil, and the AF-RMZ group received alfentanil then remimazolam. Primary outcome was the time from remimazolam administration to loss of consciousness (LOC) during induction. Secondary outcomes included anaesthetic and surgical characteristics, vital signs, and adverse events.
Results: The time from remimazolam administration to LOC was shorter in the AF-RMZ group compared with the RMZ-AF group (87.3 [25.7] s vs 132.3 [32.3] s, P< 0.0001). Similarly, the time from remimazolam administration to a bispectral index (BIS) ≤ 60 was shorter in the AF-RMZ group compared with the RMZ-AF group (168.2 [58.1] s vs 207.8 [61.6] s, P=0.0006). Although no significant difference in the total amount of remimazolam administration between groups was observed, the RMZ-AF group required a higher dose of remimazolam to achieve LOC (P< 0.0001) and to reach a BIS of ≤ 60 (P=0.0058). No significant differences were observed between groups in the total administration of alfentanil, ephedrine, rocuronium, or crystalloid infusion volumes. The most common adverse events were hypotension, hypertension, and tachycardia, with no significant difference between groups.
Conclusion: Alfentanil enhanced remimazolam’s sedative effects during anaesthesia induction in patients undergoing urological day surgery. The combination of remimazolam and alfentanil for general anaesthesia would improve efficacy, reducing the adverse effects and dosage of drug. But the potential mechanisms need further study.
Clinical Trial Registration: The trial was registered before patient enrolment at http://www.chictr.org.cn (ChiCTR2200064130, principal investigator: Xuehai Guan; date of registration: 27 September 2022, https://www.chictr.org.cn/showproj.html?proj=179023).
Keywords: alfentanil, remimazolam, anaesthesia, sedation, day surgery
Introduction
The advancement of medical technology and evolving healthcare concepts has led to the widespread adoption of day surgery, a new medical service model.1 Anaesthetic techniques are the cornerstone of day surgery. Therefore, improving anaesthesia concepts and methods is essential to ensure safe and effective outcomes in this setting.
In clinical practice, drugs with complementary effects are often used together. The combination of sedatives and opioids is a standard practice for procedural sedation and general anaesthesia. For example, the combination of propofol with fentanyl, midazolam with fentanyl, and propofol with remifentanil improved efficacy, reducing the dosage of both drugs, and reducing adverse effects.2–5 However, drug interactions can alter pharmacological outcomes,6 making it essential to understand the characteristics of these interactions. Remimazolam, a novel, ultrafast, and short-acting benzodiazepine, gained approval for use in both procedural sedation and general anaesthesia.7–9 Alfentanil, a fentanyl derivative, is a short-acting μ-opioid analgesic widely used in various clinical settings, including endoscopy, abortion, and general anaesthesia.10–13
Given the rapid onset and offset of remimazolam and alfentanil, their combination could be an ideal anaesthetic regimen for day surgeries. Despite this potential, only a few studies have explored the remimazolam-alfentanil interaction. Our hypothesis is that alfentanil may enhance the sedative effects of remimazolam during anaesthesia induction in patients undergoing urological day surgery.
Methods
Study Design and Participants
This study was a single-centre, single-blinded, randomised clinical trial. Ethical approval was granted by the Medical Ethics Committee of the First Affiliated Hospital of Guangxi Medical University (identifier: 2022-KY-E-302; Chairperson: Prof. Songqing He) on 13 September 2022 and was registered with the Chinese Clinical Trial Registry (https://www.chictr.org.cn; registration number: ChiCTR2200064130, principal investigator: Xuehai Guan; date of registration: 27 September 2022). Written informed consent was obtained from all patients before enrolment. This trial was performed at the First Affiliated Hospital of Guangxi Medical University in accordance with the Declaration of Helsinki and CONSORT guidelines.
A total of 114 patients, aged 18–65 years, with an American Society of Anaesthesiologists (ASA)physical status I–III, undergoing elective urological day surgery under general anaesthesia, were enrolled. Patients with a history of difficult airway (modified Mallampati class 3–4), asthma, severe hypertension (systolic blood pressure ≥ 180 mmHg or diastolic blood pressure ≥ 110 mmHg), pulmonary heart disease, pulmonary arterial hypertension, cardiac insufficiency, hyperthyroidism, epilepsy, or psychosis were excluded. Further exclusion criteria included allergic reactions to drugs, obesity (body mass index, BMI ≥ 30 kg.m−2), pregnancy, and analgesic abuse.
Randomisation and Masking
Enrolled patients were randomly assigned to either the RMZ-AF or AF-RMZ group using a computer-generated randomisation code (EpiCalc 2000 software) in a 1:1 ratio. Randomisation was performed by an independent anaesthesiologist who was only involved in patient assignment and drug preparation. Group assignments were concealed in sealed envelopes. Patients, surgeons, and data collectors were blinded to the group allocation throughout the process, with the allocation only revealed after data collection and analysis were completed.
Anaesthesia Management and Intervention
All patients fasted for 8 h before surgery, with no premedication administered. Upon arrival in the operating room, standard monitoring was initiated, including non-invasive blood pressure measurement, electrocardiography, capnography, pulse oximetry (SpO2), and bispectral index (BIS). All patients inhaled 100% oxygen through a mask for 3 min before anaesthesia induction. In the RMZ-AF group, anaesthesia was induced using remimazolam tosilate (RMZ; Jiangsu Hengrui Medicine Co., Lianyungang, China; diluted with normal saline to 1 mg mL−1), starting at 6 mg kg−1 h−1 until the BIS reached 40–60 and was maintained between 0.2–2 mg kg−1 h−1. When BIS was within 40–60, alfentanil (AF; 30 µg kg−1 IV; Yichang Humanwell Pharmaceutical Co., Yichang, China) and rocuronium (0.6 mg kg−1 IV; Sinopharm Chemical Reagent Co., Shanghai, China) were administered. In the AF-RMZ group, anaesthesia was induced by using alfentanil (30µg kg−1 IV), followed by remimazolam tosilate, starting at 6 mg kg−1 h−1 until BIS reached 40–60 and was maintained between 0.2–2 mg kg−1 h−1. When BIS was within 40–60, rocuronium (0.6 mg kg−1 IV) was administered. In both groups, a laryngeal mask airway (LMA) was inserted 1 min after rocuronium administration. Anaesthesia was maintained using a combination of remimazolam (0.2–2 mg kg−1 h−1) and alfentanil (1–2 µg kg−1 min−1), adjusted based on the clinical signs and symptoms, BIS values (maintained at a range of 40–60), and the patient’s overall condition. Rocuronium was administered as a repeated bolus dose of 0.1–0.2 mg kg−1 when needed. All patients underwent mechanical ventilation (tidal volume, 8 mL kg−1; respiratory rate: 8–12 breaths min−1; oxygen concentration, 60%; and fresh gas flow, 2 L min−1). All patients with hypotension (a 30% decrease in mean arterial blood pressure (MBP) compared with baseline) were treated with ephedrine at the discretion of the attending anaesthesiologist.
If signs of intraoperative awakening (BIS > 60) were detected, the remimazolam infusion rate was adjusted to 10 mg kg−1 h −1 for up to 1 min. If awakening signs persisted, remimazolam was discontinued and replaced with propofol. All drugs were discontinued at the end of the surgery, and patients were transferred to the post-anaesthesia care unit (PACU) for recovery.
Outcomes
The primary outcome was the time from remimazolam administration to loss of consciousness (LOC) during anaesthesia induction. The consciousness was assessed by using Modified Observer`s Assessment Alertness/Sedation Scale (MOAA/S; 0, no response after painful trapezius squeeze, defined as LOC; 1, responds only after painful trapezius squeeze; 2, responds only after mild prodding or shaking; 3, response to name spoken loudly and/or repeatedly; 4, response to name spoken in normal tone; 5, response readily to name spoken in normal tone) with 10s interval during anaesthesia induction.
Secondary outcomes included anaesthetic and surgical characteristics, vital signs, and adverse events. The durations of surgery, anaesthesia, and PACU stay, as well as the time of eyes-opening and extubation, were recorded. We recorded the administration of remimazolam and alfentanil at the following time points: from administration to LOC, at BIS ≤ 60, and at the end of surgery. Total administration of rocuronium, ephedrine, and crystalloid infusion volumes were also recorded. Vital signs (mean arterial blood pressure [MBP], heart rate, SpO2, and BIS) were recorded at the following time points: 5 min before anaesthesia (baseline), at LOC, at BIS ≤ 60, at intubation, at 1 and 5 min after intubation, at the beginning of surgery, at 5 min after surgery, at time of eyes-opening, at time of extubation, and at discharge from the PACU. Adverse events such as hypertension (≥ 30% increase in MBP from baseline), hypotension (≥ 30% decrease in MBP from baseline), bradycardia (<50 beats min−1), tachycardia (>100 beats min−1), injection pain, dysphoria, nausea/vomiting, awareness, delirium, and hiccups were also recorded.
Statistical Analyses
Statistical analyses were performed using GraphPad Prism 9.0 (Dotmatics, Boston, MA, USA). The normality and equality of variances for continuous variables were tested using the Kolmogorov–Smirnov and sphericity tests, respectively. Continuous values with normal distribution and equal variance are presented as means (SD) and were analysed using an unpaired t-test or repeated-measures two-way analysis of variance (ANOVA), followed by Bonferroni's multiple comparison test. Continuous values with non-normal distribution and unequal variance are presented as medians (interquartile range [IQR]) and were analysed using the Mann–Whitney U-test. Categorical values are presented as numbers (%) and were analysed using Fisher’s exact test. A P-value of <0.05 was considered statistically significant.
This study was designed as a superiority trial. PASS software (version 11.0; NCCS, Utah, USA) was used to calculate the sample size. Preliminary tests showed that the time from remimazolam administration to LOC (mean [SD]) was 106.0 (30.0) s and 123.0 (32) s in the AF-RMZ and RMZ-AF groups, respectively. We calculated that 54 patients per group were required to achieve 80% power at a two-sided alpha of 0.05 to detect a significant difference in the primary outcome. To account for a potential 5% dropout rate, we enrolled 57 patients in each group.
Results
Between September 2022 and December 2023, 171 patients were screened for eligibility. Of these, 30 did not meet the inclusion criteria, 27 declined to participate, while 114 were successfully recruited and randomised into either the RMZ-AF or AF-RMZ group (n=57 per group). A total of 114 patients were included in the analysis (Figure 1). Table 1 presents the patient demographic data. No statistically significant differences were observed between the groups.
 |
Table 1 Baseline Characteristics of Patients |
 |
Figure 1 CONSORT diagram for the trial. CONSORT indicates Consolidated Standards for Reporting of Trials. |
The time from remimazolam administration to LOC during anaesthesia induction was significantly shorter in the AF-RMZ group than in the RMZ-AF group (87.3 [25.7] s vs 132.3 [32.3] s, P<0.0001, Table 2). Similarly, the time from remimazolam administration to BIS ≤ 60 was significantly shorter in the AF-RMZ group than in the RMZ-AF group (168.2 [58.1] s vs 207.8 [61.6] s, P=0.0006, Table 2).
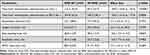 |
Table 2 Sedation Characteristics of Patients Receiving Remimazolam Combined with or Without Alfentanil for Anaesthesia Induction |
No significant differences were found between groups in terms of anaesthesia duration, surgery duration, eyes-opening time, extubation time, or PACU stay (Table 2). The total administration of remimazolam did not differ significantly between groups (Table 3). However, remimazolam doses were more in the RMZ-AF group than in the AF-RMZ group at LOC (14.7 [12.3, 16.4] mg vs 9.9 [8.5, 11.0] mg, P<0.0001) and at BIS ≤ 60 (21.3 [17.5, 25.1] mg vs 18.4 [13.1, 22.6] mg, P=0.0058). No differences were found between the groups in terms of the total administration of alfentanil, ephedrine, rocuronium, or crystalloid infusion volume.
 |
Table 3 Characteristics of Anaesthesia and Surgery in Patients Receiving Remimazolam Combined with or Without Alfentanil for Anaesthesia Induction |
Table 4 presents the incidence of adverse events. Hypotension was the most common adverse event, but no difference was found between the RMZ-AF and AF-RMZ groups (28 [49.1%] vs 22 [38.6%], 95% CI: 1.3 [0.84–2.0], P=0.3454). The incidence of hypertension was 10.5% (n=6) in the RMZ-AF group and 15.8% (n=9) in the AF-RMZ group (95% CI: 1.5 [0.59–3.8], P=0.5808). Tachycardia occurred in 12.3% of patients in both groups. No patients in either group experienced bradycardia, injection pain, dysphoria, nausea/vomiting, awareness, delirium, or hiccups.
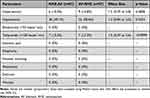 |
Table 4 Incidence of Adverse Event in Patients Receiving Remimazolam Combined with or Without Alfentanil for Anaesthesia Induction |
No significant differences were observed in MBP, heart rate, SpO2, or BIS values at any time point (Figure 2).
Discussion
This is the first reported randomised controlled trial investigating the interaction between remimazolam and alfentanil. The main finding of our results showed that the time to LOC and the doses of remimazolam required to reach LOC and BIS ≤ 60 during anaesthesia induction were shorter and lower, respectively, in the AF-RMZ group than in the RMZ-AF group. These results confirm our hypothesis that alfentanil enhances the sedative effects of remimazolam during anaesthesia induction in patients undergoing urological day surgery.
Drug interactions can be classified as synergism, additivity, or antagonism, regardless of whether one drug exerts an effect on its own.14–17 During anaesthesia induction and maintenance, it is a common practice to use two or more drugs either successively or simultaneously. Combining sedatives and opioids has a synergistic effect, enhancing anaesthesia, reducing the dosage of both drugs, and minimising adverse events.18 For instance, the combination of propofol and alfentanil changed alfentanil’s pharmacokinetics by decreasing elimination clearance by 15%, rapid distribution clearance by 68%, slow distribution clearance by 51%, and lag time by 62%.6 Although we did not conduct pharmacokinetic assessments in this study, we speculate that pretreatment with alfentanil can also affect the pharmacokinetics of remimazolam by decreasing elimination clearance and slowing distribution clearance, thereby enhancing the sedative effect of remimazolam.
Drug interactions may occur through the modulation of the action site.19 Therefore, understanding the mechanisms underlying these interactions is critical. The combination of propofol and alfentanil produced synergistic antinociceptive effects20 through the inhibition of phosphorylated extracellular signal-regulated kinase 1/2, c-Fos protein21 and the adenylyl cyclase pathway.22 Propofol exerts sedative effects by potentiating GABA responses and activating GABA type A receptors (GABAARs).23 Similarly, remimazolam exerts sedative effects by also acting on GABAARs.7 Alfentanil exerts its analgesic effect by acting on mu-opioid receptors (MOR). Since both GABAARs and MOR are co-expressed in some primary afferent neurons, it is plausible that propofol–alfentanil and remimazolam-alfentanil administration may activate the same neural pathways, thereby enhancing their sedative effects.
Alfentanil has been used as a sedative regimen in intensive care without causing prolonged respiratory depression.24 Given that the time to LOC or BIS ≤ 60 and the doses of remimazolam required were significantly shorter or lower, respectively, in the AF-RMZ group compared with the RMZ-AF group, we concluded that alfentanil enhances the sedative effect of remimazolam. The peak effect of a bolus injection of alfentanil occurs at approximately 3–4 min,25 while remimazolam reaches a peak effect at 2–3 min. By administering alfentanil immediately before remimazolam, the peak effect of both drugs overlaps, maximising remimazolam’s sedative efficacy. As the exact nature of their interaction – whether synergistic or additive – remains unclear, further investigation is required to elucidate the underlying mechanisms.
Combining alfentanil and midazolam is recommended in different clinical practices. The combination of remimazolam with alfentanil for anaesthesia during endoscopic retrograde cholangiopancreatography (ERCP), colonoscopy, and gastroscopy procedures showed fewer respiratory depression events and haemodynamic advantages than the propofol-alfentanil combination.26–28 Hypertension, hypotension, and tachycardia were the major adverse events among the two groups; however, no differences were found between the groups in our trial. The awakening time was slightly longer, and the incidence of adverse events (nausea, abdominal pain, fatigue, dizziness, and abdominal distension) were lower in remimazolam-alfentanil group than that in the propofol-alfentanil group during gastroscopy.27 The postoperative 15-item quality of recovery questionnaire score was higher, and the abdominal pain was lower in the remimazolam-alfentanil group than in the propofol-alfentanil group during ERCP procedure.26 Thus, combining remimazolam and alfentanil may be a safe option for anaesthesia.
Sedative-hypnotic drugs and opioids are risk factors for post-operative nausea and vomiting (PONV), which can prolong recovery. None of the patients developed PONV during our trial. Consistent with a previous report, alfentanil reduced the incidence of PONV than fentanyl.29 The use of rapidly metabolic sedative-hypnotic drugs and opioids for anaesthesia is effective in reducing the risk of PONV.30
None of the patients developed emergence delirium (ED) during our trial. Intranasal alfentanil, in addition to oral midazolam, did not decrease sevoflurane-induced ED.31 Intravenous alfentanil decreased the incidence of ED in the PACU.32 Compared with intravenous injection, the bioavailability of intranasal alfentanil was reduced to 64.7%.33 We infer that the different bio-availabilities of alfentanil result in this discrepancy in preventing ED.
Hiccups are a troublesome adverse event associated with remimazolam. Although remimazolam-induced hiccups are generally self-limiting, they are associated with the risk of regurgitation and aspiration, particularly in patients with a full stomach. No patients developed hiccups during this trial. The incidence of hiccups depends on the bolus rate of remimazolam administered during sedation induction.34 We believe that remimazolam administration at a rate of 6 mg kg−1 h−1 during anaesthesia induction would be appropriate. No patients in our trial experienced injection pain, dysphoria, or increased awareness.
Although there was no significant difference in the incidence of adverse events between the two groups in this study, which differed from those of other studies,26,27 the reasons may be differences in the study population, differences in drug dosage and administration methods, and the study sample size.
This study had several limitations. First, the trial focused exclusively on patients undergoing urological day surgery, limiting the generalisability of the findings to other populations. Further studies are needed to validate these conclusions in other contexts. Second, this was a single-blinded trial. Although the patients, surgeons, and data collectors were blinded to the group assignment throughout the process, the possibility of bias cannot be entirely excluded. Third, all patients were drawn from a single centre, and genetic and racial factors may limit the applicability of our findings to other populations. Further multi-centre clinical trials are required to confirm this conclusion.
Conclusion
In conclusion, alfentanil enhances the sedative effects of remimazolam during anaesthesia induction in patients undergoing urological day surgery. The combination of remimazolam and alfentanil for general anaesthesia would improve efficacy, reducing the adverse effects and dosage of drug. But the potential mechanisms need further study.
Abbreviations
MBP, mean arterial blood pressure; CI, confidence interval; GABAA, gamma-aminobutyric acid receptor subunit A; ASA, American Society of Anaesthesiologist; PACU, post-anaesthesia care unit; SpO2, pulse oximetry; BIS, bispectral index; LOC, loss of consciousness; IQR, interquartile range; ASD, absolute standardized difference; ANOVA, analysis of variance; RMZ, remimazolam; AF, alfentanil.
Data Sharing Statement
The data generated during the current study are available from the corresponding author on reasonable request.
Ethic Approval
This study was approved by the Medical Ethics Committee of the First Affiliated Hospital of Guangxi Medical University (identifier: 2022-KY-E-302; Chairperson: Prof. Songqing He) on 13 September 2022 and was registered with the Chinese Clinical Trial Registry (https://www.chictr.org.cn; registration number: ChiCTR2200064130, principal investigator: Xuehai Guan; date of registration: 27 September 2022). Written informed consent was obtained from all patients before enrolment. This trial was performed at the First Affiliated Hospital of Guangxi Medical University in accordance with the Declaration of Helsinki and CONSORT guidelines.
Acknowledgments
This study was supported by the Natural Science Foundation of Guangxi Zhuang Autonomous Region (2022GXNSFAA035628, 2024GXNSFAA010222), the Clinical Research “Climbing” Program of the First Affiliated Hospital of Guangxi Medical University (YYZS2022005), the Guangxi Zhuang Autonomous Region Health Commission’s Self-Fund Research Project on Western Medicine (Z-A20230492), and the Guangxi Zhuang Autonomous Region Traditional Chinese Medicine Appropriate Technology Development and Promotion Project (GZSY22-59). The funder had no role in the concept, patient recruitment, data collection, analysis, interpretation, trial design, or making the decision to submit for publication.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Palumbo P, Usai S, Amatucci C, et al. Inguinal hernia repair in day surgery: the role of MAC (Monitored Anesthesia Care) with remifentanil. G Chir. 2017;38(6):273–279. doi:10.11138/gchir/2017.38.6.273
2. Wiczling P, Bieda K, Przybylowski K, et al. Pharmacokinetics and pharmacodynamics of propofol and fentanyl in patients undergoing abdominal aortic surgery - a study of pharmacodynamic drug-drug interactions. Biopharm Drug Dispos. 2016;37(5):252–263. doi:10.1002/bdd.2009
3. Ben-Shlomo I, abd-el-Khalim H, Ezry J, Zohar S, Tverskoy M. Midazolam acts synergistically with fentanyl for induction of anaesthesia. Br J Anaesth. 1990;64(1):45–47. doi:10.1093/bja/64.1.45
4. Bouillon TW, Bruhn J, Radulescu L, et al. Pharmacodynamic interaction between propofol and remifentanil regarding hypnosis, tolerance of laryngoscopy, bispectral index, and electroencephalographic approximate entropy. Anesthesiology. 2004;100(6):1353–1372. doi:10.1097/00000542-200406000-00006
5. Zhang S, Wang J, Ran R, Peng Y, Xiao Y. Efficacy and safety of remimazolam tosylate in hysteroscopy: a randomized, single-blind, parallel controlled trial. J Clin Pharm Ther. 2022;47(1):55–60. doi:10.1111/jcpt.13525
6. Mertens MJ, Vuyk J, Olofsen E, Bovill JG, Burm AG. Propofol alters the pharmacokinetics of alfentanil in healthy male volunteers. Anesthesiology. 2001;94(6):949–957. doi:10.1097/00000542-200106000-00006
7. Lan H, Cao H, Liu S, et al. Efficacy of remimazolam tosilate versus propofol for total intravenous anaesthesia in urological surgery: a randomised clinical trial. Eur J Anaesthesiol. 2024;41(3):208–216. doi:10.1097/EJA.0000000000001938
8. Huang X, Cao H, Zhang C, et al. The difference in mean arterial pressure induced by remimazolam compared to etomidate in the presence of fentanyl at tracheal intubation: a randomized controlled trial. Front Pharmacol. 2023;14:1143784. doi:10.3389/fphar.2023.1143784
9. Yi F, Xiao H, Zhu T, Man Y, Ji F. Prevention of postoperative nausea and vomiting after gynaecological day surgery under remimazolam general anesthesia: a randomized double-blind controlled study. BMC Anesthesiol. 2022;22(1):292. doi:10.1186/s12871-022-01835-x
10. Zhang J, Liu R, Bi R, et al. Comparison of ciprofol-alfentanil and propofol-alfentanil sedation during bidirectional endoscopy: a prospective, double-blind, randomised, controlled trial. Dig Liver Dis. 2024;56(4):663–671. doi:10.1016/j.dld.2023.09.016
11. Jin LD, Xing L, Lin SF, et al. Comparison of different dosages of propofol combined with its equivalent alfentanil in outpatient abortion: a prospective, double-blinded, randomized trial. Eur Rev Med Pharmacol Sci. 2024;28(1):126–135. doi:10.26355/eurrev_202401_34898
12. Xu Q, Zou X, Wu J, Duan G, Lan H, Wang L. Low-Dose Alfentanil Inhibits Sufentanil-Induced Cough During Anesthesia Induction: a Prospective, Randomized, Double-Blind Study. Drug Des Devel Ther. 2024;18:1603–1612. doi:10.2147/DDDT.S464823
13. Zhu X, Chen X, Zheng X, et al. Effects of single-use alfentanil versus propofol on cognitive functions after colonoscopy: a randomized controlled trial. Heliyon. 2023;9(6):e17061. doi:10.1016/j.heliyon.2023.e17061
14. Gilron I, Orr E, Tu D, Jp O, Zamora JE, Bell AC. A placebo-controlled randomized clinical trial of perioperative administration of gabapentin, rofecoxib and their combination for spontaneous and movement-evoked pain after abdominal hysterectomy. Pain. 2005;113(1–2):191–200. doi:10.1016/j.pain.2004.10.008
15. Baillie JK, Power I. Morphine, gabapentin, or their combination for neuropathic pain. N Engl J Med. 2005;352(25):2650–2651. doi:10.1056/NEJM200506233522520
16. Freedman BM, O’Hara E. Pregabalin has opioid-sparing effects following augmentation mammaplasty. Aesthet Surg J. 2008;28(4):421–424. doi:10.1016/j.asj.2008.04.004
17. Jokinen V, Lilius TO, Laitila J, Niemi M, Rauhala PV, Kalso EA. Pregabalin enhances the antinociceptive effect of oxycodone and morphine in thermal models of nociception in the rat without any pharmacokinetic interactions. Eur J Pain. 2016;20(2):297–306. doi:10.1002/ejp.728
18. Yang H, Shi X, Li J, Yang L. Efficacy and safety of alfentanil plus propofol versus propofol only in painless gastrointestinal endoscopy: a meta-analysis. Medicine (Baltimore). 2023;102(32):e34745. doi:10.1097/MD.0000000000034745
19. Qiu Y, Qu J, Li X, Li H. Anesthesia with propofol-remifentanil combined with rocuronium for bronchial foreign body removal in children: experience of 2 886 cases. Pediatr Investig. 2018;2(1):25–29. doi:10.1002/ped4.12030
20. Deng S, Huang X, Lei X. Effects of different doses of alfentanil combined with target-controlled infusion (TCI) of propofol for daytime hysteroscopy. Heliyon. 2024;10(14):e34161. doi:10.1016/j.heliyon.2024.e34161
21. Jia N, Zuo X, Guo C, et al. Synergistic antinociceptive effects of alfentanil and propofol in the formalin test. Mol Med Rep. 2017;15(4):1893–1899. doi:10.3892/mmr.2017.6174
22. Cao S, Li Y, Wang L, et al. Synergistic analgesic effect of propofol–alfentanil combination through detecting the inhibition of cAMP signal pathway. J Pharm Pharmacol. 2016;68(9):1170–1176. doi:10.1111/jphp.12578
23. Sanna E, Garau F, Harris RA. Novel properties of homomeric beta 1 gamma-aminobutyric acid type A receptors: actions of the anesthetics propofol and pentobarbital. Mol Pharmacol. 1995;47(2):213–217. doi:10.1016/S0026-895X(25)08530-X
24. Cohen AT. Experience with alfentanil infusion as an intensive care sedative analgesic. Eur J Anaesthesiol Suppl. 1987;1:63–66.
25. Lichtenbelt BJ, Mertens M, Vuyk J. Strategies to optimise propofol-opioid anaesthesia. Clin Pharmacokinet. 2004;43(9):577–593. doi:10.2165/00003088-200443090-00002
26. Dong SA, Guo Y, Liu SS, et al. A randomized, controlled clinical trial comparing remimazolam to propofol when combined with alfentanil for sedation during ERCP procedures. J Clin Anesth. 2023;86:111077. doi:10.1016/j.jclinane.2023.111077
27. Xu C, He L, Ren J, et al. Efficacy and Safety of Remimazolam Besylate Combined with Alfentanil in Painless Gastroscopy: a Randomized, Single-Blind, Parallel Controlled Study. Contrast Media Mol Imaging. 2022;2022(1):7102293. doi:10.1155/2022/7102293
28. Xin Y, Chu T, Wang J, Xu A. Sedative effect of remimazolam combined with alfentanil in colonoscopic polypectomy: a prospective, randomized, controlled clinical trial. BMC Anesthesiol. 2022;22(1):262. doi:10.1186/s12871-022-01805-3
29. Langevin S, Lessard MR, Trepanier CA, Baribault JP. Alfentanil causes less postoperative nausea and vomiting than equipotent doses of fentanyl or sufentanil in outpatients. Anesthesiology. 1999;91(6):1666–1673. doi:10.1097/00000542-199912000-00019
30. Dershwitz M, Michalowski P, Chang Y, Rosow CE, Conlay LA. Postoperative nausea and vomiting after total intravenous anesthesia with propofol and remifentanil or alfentanil: how important is the opioid? J Clin Anesth. 2002;14(4):275–278. doi:10.1016/s0952-8180(02)00353-7
31. Bilgen S, Koner O, Karacay S, Sancar NK, Kaspar EC, Sozubir S. Effect of ketamine versus alfentanil following midazolam in preventing emergence agitation in children after sevoflurane anaesthesia: a prospective randomized clinical trial. J Int Med Res. 2014;42(6):1262–1271. doi:10.1177/0300060514543039
32. Zhao N, Zeng J, Fan L, et al. The Effect of Alfentanil on Emergence Delirium Following General Anesthesia in Children: a Randomized Clinical Trial. Paediatr Drugs. 2022;24(4):413–421. doi:10.1007/s40272-022-00510-5
33. Schwagmeier R, Boerger N, Meissner W, Striebel HW. Pharmacokinetics of intranasal alfentanil. J Clin Anesth. 1995;7(2):109–113. doi:10.1016/0952-8180(94)00023-w
34. Chen X, Sang N, Song K, et al. Psychomotor Recovery Following Remimazolam-induced Sedation and the Effectiveness of Flumazenil as an Antidote. Clin Ther. 2020;42(4):614–624. doi:10.1016/j.clinthera.2020.02.006
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Efficacy and Safety of Different Doses of Remimazolam Tosilate Applied in Upper Gastrointestinal Endoscopy: A Prospective Randomized Controlled Double-Blind Trial

Cui X, Cheng Z, Li H, Zhang X, Luan H, Zhao Z, Zhu P
Drug Design, Development and Therapy 2023, 17:2889-2896
Published Date: 20 September 2023
Comparing Remimazolam and Propofol for Postoperative Anesthesia Satisfaction in Outpatient Gynecological Surgery: A Randomized Clinical Trial
Wang XL, Dai LL, Li YN, Zhang JW, Qu MC, Zhou YY, Xing N
Drug Design, Development and Therapy 2024, 18:4615-4627
Published Date: 18 October 2024
Effect-Site Concentration of Remimazolam by Age Groups During Target-Controlled Infusion for Total Intravenous Anesthesia: A Retrospective Comparative Study
Park J, Seo KH, Kwak J, Baek H
Drug Design, Development and Therapy 2024, 18:5149-5159
Published Date: 12 November 2024
Effect of Remimazolam vs Midazolam on Early Postoperative Cognitive Recovery in Elderly Patients Undergoing Dental Extraction: A Prospective Randomized Controlled Study
Liu B, Wang P, Liang L, Zhu W, Zhang H
Drug Design, Development and Therapy 2024, 18:5895-5904
Published Date: 9 December 2024


