Back to Journals » Neuropsychiatric Disease and Treatment » Volume 21
An Evaluation a PrEP-Focused HIV Prevention Intervention Tailored for Individuals with Opioid Use Disorder and Cognitive Dysfunction
Authors Mistler CB , Huedo-Medina TB, Shrestha R, Gunstad J, Zelenev A, Copenhaver MM
Received 19 September 2024
Accepted for publication 6 June 2025
Published 24 June 2025 Volume 2025:21 Pages 1235—1248
DOI https://doi.org/10.2147/NDT.S490266
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Roger Pinder
Colleen B Mistler,1,2,* Tania B Huedo-Medina,2– 5,* Roman Shrestha,2,3 John Gunstad,6 Alexei Zelenev,7 Michael M Copenhaver2,3
1Department of Psychiatry, Yale School of Medicine, New Haven, CT, USA; 2Institute for Collaboration on Health, Intervention, and Policy (Inchip), University of Connecticut, Storrs, CT, USA; 3Department of Allied Health Sciences, University of Connecticut, Storrs, CT, USA; 4Department of Clinical and Health Psychology and Research Methods, Faculty of Psychology, University of the Basque Country UPV/EHU, Donostia-San Sebastián, Spain; 5Basque Foundation for Science, IKERBasque, Bilbao, 48011, Spain; 6Department of Psychological Sciences, Kent State University, Kent, OH, USA; 7Department of Internal Medicine, AIDS Program, Yale School of Medicine, New Haven, CT, USA
*These authors contributed equally to this work
Correspondence: Colleen B Mistler, Yale University, The Consultation Center, 389 Whitney Ave, New Haven, CT, 06511, USA, Email [email protected]
Purpose: This study aimed to test the efficacy of the 4-week Bio-behavioral Community-Friendly Health Recovery Program (CHRP-BB) at improving HIV prevention outcomes among individuals receiving medication for opioid use disorder (MOUD) and to examine the extent to which cognitive dysfunction impacts outcomes.
Patients and Methods: This randomized controlled trial included 237 individuals receiving MOUD and Pre-Exposure Prophylaxis (PrEP) in New Haven, CT. We conducted a longitudinal regression analysis to evaluate the impact of the intervention on HIV risk behaviors and PrEP-related outcomes over time. We estimated the effect of treatment on the outcome variables that include PrEP knowledge and adherence skills, HIV risk behavior, Syringe cleaning skills, and Condom skills using a difference-in-differences framework across four time periods (Post-intervention, and 3-, 6-, and 9-month follow-ups).
Results: The CHRP-BB intervention exerted a positive effect on experimental group participants across a range of key outcomes, particularly among shorter term IDUs. Improvements that were the most pronounced included PrEP outcomes (knowledge and adherence skills) and syringe cleaning skills. Most outcomes were not significantly disrupted by cognitive dysfunction.
Conclusion: Outcomes from this trial highlight the efficacy of the CHRP-BB intervention, including the use of cognitive dysfunction compensatory strategies, to significantly improve HIV prevention efforts among individuals on MOUD. We suggest that future efforts focus on refining and testing additional strategies that can further optimize intervention effects across a broader range of outcomes and MOUD patients.
Keywords: cognitive dysfunction, people who inject drugs, pre-exposure prophylaxis, HIV prevention, opioid use disorder, medication for opioid use disorder
Introduction
The opioid epidemic in the US has halted HIV prevention progress, as one in ten new HIV infections are attributed to people who inject drugs (PWID).1 Evidence-based HIV prevention interventions for people with opioid use disorder (OUD) typically consist of individual or group behavioral counseling sessions to improve HIV risk perception, HIV prevention knowledge, and HIV risk reduction behaviors.2 These sessions, by nature, require participants to have intact cognitive functioning in order to fully participate and maximize efficacy. People with OUD often demonstrate cognitive dysfunction, with the pattern and severity of deficits similar to those found in persons with attention deficit hyperactivity disorder (ADHD) and traumatic brain injury (TBI). Deficits often include dysfunction in executive functioning, attention, memory, and information processing.3–5 This specific cognitive profile can disrupt treatment engagement and retention,5 lead to increased HIV risk behaviors, increased risk of HIV transmission, and decreased adherence to medications.6,7 While the prevalence of cognitive dysfunction among people with OUD is disproportionately higher than in the general population, it is often overlooked in HIV prevention and addiction treatment efforts.8,9
In a 2013 study, a new HIV prevention medication strategy, Pre-exposure prophylaxis (PrEP), demonstrated efficacy in reducing HIV transmission by almost 50% among very high-risk HIV-negative people who inject drugs (PWID).10 This HIV prevention medication strategy was supported by the use of behavioral counseling and medication for opioid use disorder (MOUD).10 Despite the efficacy of PrEP at preventing HIV transmission, PrEP uptake and adherence has been disturbingly low among PWID in the US (0–3%).11 PrEP is most effective at preventing HIV transmission when taken precisely as prescribed; the pill requires daily adherence, and the long-acting injectable (LAI) requires bi-monthly injections.12 The cognitive challenges of many high-risk individuals receiving MOUD, however, contribute to the low uptake and adherence to PrEP among this risk group. There is also evidence that other patient attributes, such as the extent of injection drug use history, influences how patients respond to harm reduction strategies.13 Thus, PrEP-focused evidence-based behavioral interventions must be tailored to accommodate a range of patient attributes that are common among individuals on MOUD.
Integrating PrEP services into existing substance use treatment settings and syringe service programs has shown feasibility, acceptability, and preliminary efficacy in improving PrEP interest and uptake among individuals with OUD.14–19 One such integrated intervention approach is the Bio-behavioral Community-Friendly Health Recovery Program (CHRP-BB),20,21 designed for implementation in real-world substance use treatment settings. Although preliminary research on the Bio-Behavioral Community-friendly Health Recovery Program (CHRP-BB) demonstrated acceptability and feasibility of improving adherence to PrEP and reducing HIV risk in PWID, its efficacy has not been evaluated across a diverse sample of patients on MOUD. Therefore, this study seeks to evaluate the efficacy of CHRP-BB at improving HIV prevention outcomes among individuals receiving MOUD, and to examine the extent to which patient attributes (eg, cognitive dysfunction, IDU history), influence HIV prevention outcomes.
Based on the information, motivation, and behavioral skills (IMB) model,22 this intervention was adapted and tailored to accommodate the cognitive profiles of individuals receiving MOUD with the aim of optimizing PrEP interest, uptake, adherence, and HIV risk reduction among people receiving MOUD. The CHRP-BB approach addresses cognitive dysfunction through a variety of compensatory strategies that are incorporated into the brief HIV prevention group sessions.5 A number of evidence-based strategies are implemented, including the use of structured sessions with a written agenda, a multi-modal presentation of information, hands-on activities, immediate feedback, and memory aids (eg, daily text message reminders).
In the present study, a fully powered randomized controlled clinical trial of the CHRP-BB intervention was conducted to test its efficacy at improving PrEP- and HIV risk reduction-related outcomes among individuals receiving MOUD. Differences were also assessed between participants with intact vs impaired cognitive functioning. We hypothesized that participants who received the 4-week bio-behavioral intervention would demonstrate significantly greater improvements in PrEP and HIV risk reduction outcomes compared to participants who received treatment as usual (TAU) care in a substance use treatment program.
Material and Methods
Recruitment and Sample
A purposive sample was recruited through an opioid replacement substance use treatment program in New Haven, CT, via clinic-based advertisements and flyers, word-of-mouth, and direct referrals from their counselors. Participants were included in the study if they met the following criteria: a) DSM-V criteria for opioid use disorder (OUD); b) enrolled in opioid substitution therapy for OUD; c) self-reported being HIV negative; d) at least 18 years or older; e) reported unsafe injection drug use practices or unprotected sex within (past 3 months); f) have a cell phone; g) able to understand, speak, and read English; and h) willing to initiate PrEP use; and i) able to communicate (read, write and speak) in English. Participants were excluded if they were a) unable to attend all intervention and follow-up assessment sessions; and/or b) actively suicidal, psychotic, and/or homicidal.
Procedures
Study Design
Participants were randomized into one of the two conditions: CHRP-BB intervention (experimental condition) vs a time- and attention-matched control condition. The power analysis was computed for an effect size (d) of 0.37, a small-medium effect size to be conservative, based on similar intervention studies in similar facilities comparing groups in terms of high levels of medication adherence and changes in HIV risk behavior. The computations assumed an intra-class correlation (ICC) of 0.500. All participants were linked to PrEP services, and after confirmation of PrEP prescription, they completed baseline assessments. Participants in the experimental condition attended 4-weekly 50-minute group sessions and one 8-week booster session, in which two trained facilitators provided HIV prevention sessions using a multimodal presentation style. Intervention fidelity was measured by an independent reviewer’s checklist to ensure that each session was delivered in a standardized manner. Any discrepancies were discussed weekly by the facilitators and the reviewer. The 4 weekly sessions topics included: ‘Making the Most of PrEP as an Active Health Manager’, ‘Reducing Drug Risk and Taking PrEP’, ‘PrEP Adherence and Sex Risk Reduction Strategies’, and Negotiating Partner Support for HIV Prevention. A detailed overview of this intervention and associated protocols has been reported eleswhere.21 Participants in the control condition received TAU, consisting of ongoing MOUD and a matching amount of group counseling time and attention routinely offered by the substance use treatment program. After 8-weeks, all participants completed a post-assessment and then 3-, 6-, and 9-month follow-up assessments.
During the initial intake session, participants completed self-report surveys to collect data on their demographics, as well as PrEP and HIV risk reduction constructs22 using Qualtrics survey software.23 Participants also completed a risk reduction skills assessment at the intake session.24–26 The surveys and skills assessments were also completed at the 8-week post and at 3-, 6-, and 9-month follow-ups. Cognitive status was assessed retrospectively using a combination of electronic medical records review and self-reported cognitive functioning items.27 The study was approved by the University of Connecticut Institutional Review Board (IRB; H17-200) and the APT foundation, Inc., a substance use treatment program. This study complies with the Declaration of Helsinki principles; all participants provided fully informed consent prior to their enrollment in the study. This study was registered at ClinicalTrials.gov (# NCT03282890).
Material and Methods
Demographics
Participants were asked to report their age, gender, racial-ethnic identity, sexual identity, marital status, education level, primary language, employment status, yearly income, and health insurance status.
Cognitive Dysfunction Risk Score (CDRS)
The CDRS consists of a total score of 11-items designed to assess cognitive functioning among individuals with opioid use disorder (OUD) who are enrolled in opioid replacement therapy (ORT).27 Each of the following demographic/medical variables were converted to binary indicators, which are equal to “1” if a condition is met, and “0” otherwise: ≥50 years of age, education less than high school graduate, non-white, history of head injury, any other psychological diagnosis (ie, in addition to OUD), history of overdose, history of polysubstance use in past two years. Self-reported questions required participants to respond to the following questions on a four-point Likert Scale ranging from not at all, slightly, somewhat, moderately, and extremely: If they count with their fingers, forget the names of common things, drop things frequently, and if part of their body feels numb. These items were recoded for “not at all” and “slightly” to equal 0, and for “somewhat”, “moderately”, and “extremely” to equal 1. A total score was calculated using these 11 items, ranging from 0–11. Scores of 0–4 were categorized as “Intact cognitive functioning”, and 5–11 as “Impaired cognitive functioning.”
PrEP-Related Measures
PrEP-related measures included 12 items focused on each participant’s PrEP Knowledge as well as 11 items designed to assess their PrEP Adherence Skills.22,28 The 12 PrEP Knowledge items (eg, “PrEP provides protection against other sexually transmitted infections”) required participants to indicate whether the items were true, false, or if they were unsure. The 11 PrEP Adherence Skills items (eg, “How confident are you that you could make PrEP part of your daily routine?”) required participants to indicate either: not at all, somewhat confident, moderately confident, very confident, or completely confident.
HIV Risk Reduction Measures
Categorical HIV risk reduction measures22,28 consisted of Information, Motivation, and Behavioral skills questions based on the IMB model of health behavior change. Four information (knowledge) variables included questions such as “If an HIV+ person only has sex with another HIV+ person, they don’t need to use a condom”. Participants were asked to indicate if the four questions were true, false, or if they were unsure. Eight motivation items included questions on readiness to change and intentions to change HIV risk behavior, such as “I plan not to have sex during the next 3 months”. Participants were asked to indicate whether the eight statements were very true, somewhat true, neither true nor untrue, somewhat untrue, or very untrue. Four behavioral skills items related to self-efficacy about risk reduction skills, such as “How hard would it be for you to always use condoms or latex protection if you have oral, vaginal, or anal sex?” Participants were asked to indicate whether these behaviors would be very hard to do, fairly, hard to do, neither hard nor easy to do, somewhat easy to do, or very easy to do.
Behavioral Skills
Participants’ HIV risk reduction behavioral skills were systematically assessed as in prior randomized controlled trials24–26 by having participants demonstrate the 16 steps necessary to properly clean a syringe, 17 steps necessary to properly use a male condom, and 15 steps necessary to properly use a female condom. Ratings of audio-taped demonstrations of these standardized procedures have shown high inter-rater reliability in similar prior trials (inter-rater reliability = 0.98).25 A total score was calculated for each of the three HIV risk reduction skills assessments; a higher total score indicated a greater HIV risk reduction skill level.
Data Analysis
First, t-tests and Chi-squared tests were conducted to determine if there were any significant differences between conditions for all demographic variables at baseline. Second, to assess the impact of the intervention on HIV risk behaviors and PrEP-related outcomes, we conducted a longitudinal regression analysis. More specifically, we estimated the effect of treatment on the outcome variables across four time periods (Post-intervention, and 3-, 6-, and 9-month follow-ups) using a difference-in-differences framework.29 The model includes a Time indicator, equal to unity for each post-intervention period and “0” otherwise, a Group indicator identifying intervention group, and interaction terms between Group and Time. Based on prior research,13 we also included injection drug use (IDU) history as a moderator variable, categorized as longer term IDU (above the median in years) and shorter term IDU (below the median in years). Two-way interaction terms between IDU history and Time and three-way interactions between IDU history, Group, and Time were also included to assess differential treatment effects by IDU history. The statistical significance was evaluated using t-tests, with inference drawn from robust clustered standard errors to adjust for the correlated structure resulting from repeated longitudinal measures. CDRS, and IDU history by Group, and Time interactions were also used to test the possible moderation effect of the intervention due to the intact or impaired cognitive functioning of participants, and IDU history. PrEP- and HIV risk-related variables were recoded to standardize the scales using reverse coding as applicable to make the results more intuitive, as higher scores indicate better HIV risk reduction information, motivation, and behavioral skills. Missing data were assumed to be missing at random and multiple imputations with chained equations, using the Markov chain Monte Carlo (MCMC) method to impute the missing data.30 Data analyses were conducted using SPSS v. 2831 and Stata.32
Results
Demographics
The average age of the 237 participants was 43 years old (S.D. = 10.06), and 51% of the sample identified as male. Those identifying as White made up 61% of the sample population; participants identifying as African American or Black made up 21%, 15% identified as Hispanic/Latinx, and 3% identified as Others. Most participants identified as heterosexual (79%) and having health insurance (99%). More than half of the participants had at least a high school diploma / GED (74%), and more than half reported having less than $10,000 annual income (79%). Participants with intact cognitive functioning comprised 58% of the sample, while 42% had impaired cognitive functioning. Approximately half of the sample reported an injection drug use (IDU) history of greater than 20 years. There was a statistically significant difference between conditions in terms of Ethnicity (Table 1), so that variable was controlled in all analyses.
 |
Table 1 Baseline Characteristics and Demographic Variables |
Intervention Outcomes
PrEP Outcomes (Knowledge and Adherence Skills)
Participants in the intervention group with a shorter IDU history showed statistically significant improvements in PrEP Knowledge scores at the Post (β =1.15, p < 0.01), 6-month (β = 0.84, p = 0.06) and 9-month points following the intervention (β = 1.09, p < 0.01). By contrast, individuals with a longer IDU history had lower PrEP Knowledge scores in both the control and intervention group (β = −0.368, p = 0.07). At 9-months, shorter IDU history was associated with higher PrEP Knowledge scores in the intervention group, as evidenced by the 3-way interaction term (β = −1.00, p = 0.02).
As evidenced by the two way and three way interactions, cognitive dysfunction did tend to disrupt the treatment effect on PrEP Knowledge, but only at the Post and 3-month follow-up points (β =−1.17, p < 0.01 and β = −0.92, p = 0.034). At the 6- and 9-month points, the intervention effect was not significantly impacted by cognitive dysfunction relative to baseline (β = −0.44, p = 0.34 and β =−0.30, p = 0.50).
For the PrEP Adherence Skills outcome, we tested the presence of a moderator effect of IDU history and found no evidence that the intervention had a differential impact on PrEP adherence skills based on the length of participants’ IDU history. Thus, we excluded the IDU history moderator from the model based on the relative goodness of fit metric, adjusted R2. Participants in the intervention group showed statistically significant improvements in PrEP adherence skills at 6-months (β = 5.15, p = 0.04) and 9-months following the intervention (β = 5.16, p = 0.08). We found evidence that this effect was moderated by cognitive dysfunction at 6 months and 9 months, such that the impact of the intervention was reduced by the presence of cognitive dysfunction, as evidence by the interaction between cognitive dysfunction, intervention and the 6 and 9-month time indicators (β = −6.42, p = 0.06) and (β = −6.65, p = 0.06), respectively (Table 2).
 |
Table 2 Intervention Effects for PrEP Knowledge and PrEP Adherence Behavior Outcomes (n = 237) |
HIV Risk Reduction Outcomes
The intervention group showed a significant improvement in HIV Risk reduction behavior scores at the 9-month follow-up point (β = 2.39, p = 0.012), while scores at the other time points showed positive but non-significant intervention effects in the predicted direction (Table 3). The coefficients for the Time variables were positive and significant, indicating that the HIV risk behavior scores increased over time in both the control and intervention groups relative to baseline. In addition, cognitive dysfunction did not have a statistically significant association with HIV risk behavior scores. Participants with a shorter IDU history had lower HIV risk behavior scores at baseline (β = −0.96, p = 0.041), but the interactions between IDU history and time indicators were not statistically significant. We found no statistical difference over time between groups in terms of changes in HIV risk reduction knowledge (Table S1).
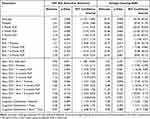 |
Table 3 Intervention Effects for HIV Risk Reduction Behaviors and Syringe Cleaning Skills Outcomes (n = 237) |
Behavioral Skills
Syringe Cleaning Skills
The intervention effect on syringe cleaning skills showed that participants in the intervention group demonstrated statistically significantly improvements in syringe cleaning skills over time relative to the control group at Post (β = 16.77, p = 0.014), 6-months (β = 15.59, p = 0.015), and 9-months (β = 22.47, p = 0.001). A significant three-way interaction between Group, IDU history, and 9-month period (β = −14.59, p = 0.047) showed that longer-term IDUs had significantly smaller improvements stemming from the intervention effect relative to those with shorter-term IDUs.
In addition, White participants (β = −2.70, p = 0.001) and those with cognitive dysfunction (β = −7.56, p = 0.015) showed lower syringe cleaning skill scores at baseline in both control and intervention groups. We did not find any significant evidence that cognitive dysfunction disrupted syringe cleaning skills in the intervention group over time.
Male Condom Application Skills
The intervention effect on male condom application skills was statistically significant at the 9-month point (β = 6.92, p = 0.031), indicating that shorter term IDUs in the intervention group demonstrated greater improvements in male condom application skills at 9 months compared to those in the control group. Individuals with a longer IDU history showed less improvements in male condom skills compared to shorter term IDUs in the treatment group at 9-months (β = −6.58, p = 0.032). At the other time points, the difference between control and intervention groups was not statistically significant. Both the control and intervention groups, however, exhibited positive effects at all time points (p < 0.01) indicating that male condom application skills improved over time relative to baseline. In addition, White participants (β = −1.35, p = 0.009) and those with cognitive dysfunction (β = −5.55, p = 0.009) demonstrated significantly lower male condom application skill scores across time. There was also a statistically significant Cognitive Dysfunction × Time interaction (β = 5.19, p = 0.042), suggesting that cognitively impaired participants in both conditions made some improvements at posttest (Table 4).
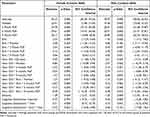 |
Table 4 Intervention Effects for Female Condom Skills and Male Condom Skills Outcomes (n =237) |
Female Condom Application Skills
The intervention effect on female condom application skills was statistically significant at the 9-month point (β = 9.6, p = 0.03), indicating that shorter-term IDUs in the intervention group demonstrated greater improvements in female condom application skills at 9 months compared to those in control group. At other time points, the difference between groups was not statistically significant. Both control and intervention groups exhibited positive effects at all time points (p < 0.01), indicating that female condom skills improved over time relative to the baseline. The 3-way interaction between IDU history, intervention group, and 9-month time period was statistically significant, such that individuals with a longer IDU history demonstrated less improvement in female condom skills compared to shorter term IDUs at 9-months (β = −8.4, p = 0.03). In addition, White participants (β = −1.2, p = 0.03) demonstrated significantly lower female condom skill scores across time. There was no statistically significant association between cognitive dysfunction and intervention; thus, there was no significant difference in female condom application skill changes due to cognitive dysfunction.
Discussion
The design and focus of this study was guided by recommendations from the Substance Abuse and Mental Health Services Administration (SAMHSA), which promotes the need to review patients’ psychosocial history and cognitive functioning in order to properly design behavioral interventions.33 Our preliminary work3–5 also provided the rationale for adapting an existing evidence-based intervention to better accommodate the cognitive profiles of individuals with OUD receiving MOUD. Following adaptation and feasibility testing,34,35 the present study tested the impact of the experimental CHRP-BB intervention, a PrEP-focused HIV risk reduction approach specifically tailored for individuals on MOUD, many of whom demonstrate mild to moderate cognitive dysfunction. The CHRP-BB approach includes compensatory strategies specifically designed to enhance participants’ ability to process and utilize intervention content.
Encouraging outcomes were found in terms of improvements in PrEP-related knowledge, PrEP adherence skills, HIV risk reduction, and various HIV prevention skills stemming from the CHRP-BB intervention approach relative to the time-and-attention-matched control condition. Interestingly, certain outcomes were most pronounced among a subgroup of patients with a shorter history of injection drug use, including significantly greater improvements in PrEP Knowledge, male condom application skills, and female condom application skills. This is consistent with prior work showing that diverse samples of IDUs tend to exhibit differential responses to harm reduction strategies based on their injection history, which may be a proxy for a host of other unmeasured attributes.13 Although there was no evidence that cognitive dysfunction impeded improvements in male and female condom application skills, it did attenuate the intervention effect on PrEP Knowledge at the Post and 3-month period, and PrEP adherence skills at the 6 and 9-month periods. This points toward the potential benefit of incorporating more potent compensatory intervention strategies to enhance PrEP-focused outcomes.
In contrast, the intervention effects on syringe cleaning skills and HIV risk reduction outcomes did not diverge based on cognitive dysfunction or IDU history. Thus, the CHRP-BB approach tended to exert positive outcomes on intervention group participants regardless of cognitive dysfunction. It is particularly encouraging that the experimental intervention strategies that were designed to compensate for (ie, work around) cognitive dysfunction may have enhanced many participants’ ability to accrue the expected intervention effects in this case, as intended.36 Interestingly, although the pattern of syringe cleaning skills and HIV risk reduction outcomes were in the predicted direction earlier, they reached significance only at the latter time point. We note, however, that delayed emergence of treatment effects is not unusual in response to behavioral interventions, and is arguably even more important than early treatment success that often decays rapidly.37
Overall, the pattern of findings suggests that the CHRP-BB intervention may benefit from further refinement in order to optimize a broader range of PrEP-focused outcomes and a more diverse range of patients on MOUD, including those with a more extensive history of IDU. Relatedly, continuing along this line of research, it would be helpful to determine which specific compensatory strategies – alone or in varied combinations – are the most potent in terms of boosting HIV prevention outcomes in this priority population.
Limitations
While this study examines an innovative approach, as the first PrEP-focused intervention tailored to the cognitive profiles of individuals receiving MOUD, there are some limitations worth mentioning. This study only recruited participants who could understand, speak, and read the English language, and participants who had a phone for communicating daily text messages in English. Therefore, we may have missed the opportunity to test the impacts of this intervention on non-English speakers, which presents a sample-selection bias. Cognitive functioning was measured via a validated item;27 however, this cognitive dysfunction risk score provides a score based on a one-time measurement that does not account for fluctuations in daily cognitive function or extraneous variables that may influence cognitive functioning. Future studies should measure cognitive functioning more frequently in order to improve the precision of this measurement. While this intervention was designed for implementation within a common type of opioid replacement drug treatment setting, the generalizability to other clinical settings may be reduced. Despite a time- and attention-match control condition, the benefits of this particular intervention should be further researched using an active control condition. In addition, despite efforts for equal distribution of demographic variables between conditions there were significant differences between the two intervention conditions regarding ethnicity. Thus, findings should be interpreted in the context of these limitations.
Conclusion
This study used a randomized controlled trial designed to test a novel experimental intervention approach – CHRP-BB,20,21 a PrEP-focused adapted evidence-based HIV prevention intervention, vs a time- and attention-matched control condition. The CHRP-BB intervention was specifically tailored to accommodate the mild to moderate cognitive dysfunction found in many patients enrolled in MOUD treatment. In terms of treatment outcomes, a key reason that cognitive dysfunction is relevant to this patient population is that it can disrupt patients’ ability to fully process and utilize intervention content. Not surprisingly, prior studies have shown differential outcomes when comparing those classified as having cognitive dysfunction relative to their counterparts classified with intact cognitive functioning.38 Thus, our aim in developing CHRP-BB was to enhance HIV prevention outcomes by integrating proven compensatory strategies to work around their common cognitive challenges, which would allow them to accrue the expected intervention benefits.
Overall, our outcomes suggest that the CHRP-BB intervention exerted an important positive effect on experimental group participants across a range of key outcomes, and the level of improvement went well beyond what was evidenced among participants in the active control condition, particularly among shorter term IDUs. Improvements that were the most pronounced included PrEP behavior (adherence skills) and syringe cleaning skills. Of significant interest, the intervention effect on some PrEP-related outcomes was disrupted to a degree, suggesting the need to continue refining more potent compensatory strategies in this case. It is encouraging, however, that the majority of improvements were not hampered by cognitive dysfunction, as that was our objective in designing the CHRP-BB intervention approach.
We suggest that future efforts focus on refining and testing intervention strategies that can further optimize intervention effects across a broader range of outcomes and MOUD patients, including those characterized by a longer history of IDU. It is plausible that additional compensatory strategies that have been successful in other patient populations5 may also be successfully applied to a wider range of patients on MOUD and cognitive dysfunction. Furthermore, it may be useful to apply other research designs, such as a Multiphase Optimization Strategy (MOST),39,40 to more precisely investigate how to maximize the potency of various combinations of evidence-based intervention strategies targeting patients on MOUD who are impeded by cognitive dysfunction.
Data Sharing Statement
The authors intend to share individual de-identified participant data, upon request to the first author’s contact information. The authors are also willing to share intervention manuals, recruitment flyers, and data collection measurement tools upon request.
Acknowledgments
The authors would like to thank Brian Sibilio and Tanya Adler for their assistance with data collection and study coordination.
Funding
This work was funded by the National Institute of Drug Abuse (NIDA); R01DA044867 (Copenhaver, PI); NIDA K24DA051344 (Copenhaver, PI). CM was supported by T32-DA019426.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Centers for Disease Control and Prevention. HIV and People Who Inject Drugs. https://www.cdc.gov/hiv/risk/drugs/index.html.
2. Mathers BM, Degenhardt L, Ali H, et al. HIV prevention, treatment, and care services for people who inject drugs: a systematic review of global, regional, and national coverage. Lancet. 2010;375(9719):1014–1028. doi:10.1016/S0140-6736(10)60232-2
3. Gunstad J, Disabato D, Shrestha R, Sanborn V, Mistler CB, Copenhaver MM. Latent profile analysis of data from the brief inventory of neurocognitive impairment (BINI) to develop neuro-cognitive profiles among opioid-dependent patients in drug treatment. J Addict Dis. 2022;1–8. doi:10.1080/10550887.2022.2080626
4. Sanborn V, Gunstad J, Shrestha R, Mistler CB, Copenhaver MM. Cognitive profiles in persons with opioid use disorder enrolled in methadone treatment. Applied Neuropsychology: Adult. 2020;1–7. doi:10.1080/23279095.2020.1769099
5. Mistler CB, Shrestha R, Gunstad J, Sanborn V, Copenhaver MM. Adapting behavioural interventions to compensate for cognitive dysfunction in persons with opioid use disorder. General Psychiatry. 2021;34(4):e100412. doi:10.1136/gpsych-2020-100412
6. Buckingham E, Schrage E, Cournos F. Why the Treatment of Mental Disorders Is an Important Component of HIV Prevention among People Who Inject Drugs. Adv Prevent Med. 2013;2013:690386. doi:10.1155/2013/690386
7. Huedo-Medina TB, Shrestha R, Copenhaver M. Modeling a Theory-Based Approach to Examine the Influence of Neurocognitive Impairment on HIV Risk Reduction Behaviors Among Drug Users in Treatment. AIDS Behavior. 2016;20(8):1646–1657. doi:10.1007/s10461-016-1394-x
8. Bruijnen C, Dijkstra BAG, Walvoort SJW, et al. Prevalence of cognitive impairment in patients with substance use disorder. Drug Alcohol Rev. 2019;38(4):435–442. doi:10.1111/dar.12922
9. Shrestha R, Copenhaver M. The Influence of Neurocognitive Impairment on HIV Risk Behaviors and Intervention Outcomes among High-Risk Substance Users: a Systematic Review. Rev Front Public Health. 2016;4:16. doi:10.3389/fpubh.2016.00016
10. Choopanya K, Martin M, Suntharasamai P, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled Phase 3 trial. Lancet. 2013;381(9883):2083–2090. doi:10.1016/s0140-6736(13)61127-7
11. Mistler CB, Copenhaver MM, Shrestha R. The Pre-exposure Prophylaxis (PrEP) Care Cascade in People Who Inject Drugs: a Systematic Review. AIDS Behav. 2021;25(5):1490–1506. doi:10.1007/s10461-020-02988-x
12. Centers for Disease Control and Prevention. PreExposure Prophylaxis for the Prevention of HIV Infection in the United States. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf.
13. Montain J, Ti L, Hayashi K, Nguyen P, Wood E, Kerr T. Impact of length of injecting career on HIV incidence among people who inject drugs. Addict Behav. 2016;58:90–94. doi:10.1016/j.addbeh.2016.02.020
14. Meyer JP, Price CR, Ye Y, et al. A PrEP Demonstration Project Using eHealth and Community Outreach to Justice-Involved Cisgender Women and Their Risk Networks. AIDS Behav. 2022;26(12):3807–3817. doi:10.1007/s10461-022-03709-2
15. Meyer J, Price C, Tracey D, et al. Preference for and Efficacy of a PrEP Decision Aid for Women with Substance Use Disorders. Patient Preference Adherence. 2021;15:1913–1927. doi:10.2147/PPA.S315543
16. Ni Z, Altice FL, Wickersham JA, et al. Willingness to initiate pre-exposure prophylaxis (PrEP) and its use among opioid-dependent individuals in drug treatment. Drug Alcohol Depend. 2021;219:108477. doi:10.1016/j.drugalcdep.2020.108477
17. Shrestha R, Karki P, Altice FL, et al. Measuring Acceptability and Preferences for Implementation of Pre-Exposure Prophylaxis (PrEP) Using Conjoint Analysis: an Application to Primary HIV Prevention Among High Risk Drug Users. AIDS Behav. 2018;22(4):1228–1238. doi:10.1007/s10461-017-1851-1
18. Shrestha R, Altice FL, Karki P, Copenhaver MM. Integrated Bio-behavioral Approach to Improve Adherence to Pre-exposure Prophylaxis and Reduce HIV Risk in People Who Use Drugs: a Pilot Feasibility Study. AIDS Behav. 2018;22(8):2640–2649. doi:10.1007/s10461-018-2099-0
19. Bazzi AR, Bordeu M, Baumgartner K, et al. Study protocol for an efficacy trial of the “PrEP for Health” intervention to increase HIV PrEP use among people who inject drugs. BMC Public Health. 2023;23(1):513. doi:10.1186/s12889-023-15429-w
20. Shrestha R, Altice F, Karki P, Copenhaver R. Developing an Integrated, Brief Bio-Behavioral HIV Prevention Intervention for High Risk Drug Users in Treatment: the Process and Outcome of Formative Research. Front Immunol. 2017;8. In press. doi:10.3389/fimmu.2017.00561
21. Shrestha R, Altice FL, Sibilio B, Ssenyonjo J, Copenhaver MM. Rationale and design of an integrated bio-behavioral approach to improve adherence to pre-exposure prophylaxis and HIV risk reduction among opioid-dependent people who use drugs: the CHRP-BB study. Contemp Clin Trials. 2019;82:77–84. doi:10.1016/j.cct.2019.06.012
22. Wa F, Jd F, Harman J. The information-motivation-behavioraI skills model: a general social psychological approach to understanding and promoting health behavior. In: Social Psychological Foundations of Health and Illness. Blackwell Publishing; 2003:82–106.
23. 2021. Available from: https://www.qualtrics.com.
24. Avants SK, Margolin A, Usubiaga MH, Doebrick C. Targeting HIV-related outcomes with intravenous drug users maintained on methadone: a randomized clinical trial of a harm reduction group therapy. J Substance Abuse Treatment. 2004;26(2):67–78. doi:10.1016/S0740-5472(03)00159-4
25. Margolin A, Avants SK, Warburton LA, Hawkins KA, Shi J. A randomized clinical trial of a manual-guided risk reduction intervention for HIV-positive injection drug users. Health Psychol. 2003;22(2):223–228. doi:10.1037/0278-6133.22.2.223
26. Copenhaver MM, Lee IC, Baldwin P. A randomized controlled trial of the community-friendly health recovery program (CHRP) among high-risk drug users in treatment. AIDS Behav. 2013;17(9):2902–2913. doi:10.1007/s10461-013-0539-4
27. Copenhaver MM, Sanborn V, Shrestha R, Mistler CB, Sullivan MC, Gunstad J. Developing a cognitive dysfunction risk score for use with opioid-dependent persons in drug treatment. Drug Alcohol Depend. 2021;224:108726. doi:10.1016/j.drugalcdep.2021.108726
28. Shrestha R, Altice FL, Huedo-Medina TB, Karki P, Copenhaver M. Willingness to Use Pre-Exposure Prophylaxis (PrEP): an Empirical Test of the Information-Motivation-Behavioral Skills (IMB) Model among High-Risk Drug Users in Treatment. AIDS Behav. 2017;21(5):1299–1308. doi:10.1007/s10461-016-1650-0
29. Wooldridge J. Econometric Analysis of Cross Section and Panel Data.
30. White I, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30(4):377–399. doi:10.1002/sim.4067
31. IBM. SPSS Statistics for Windows. Version 25. IBM Corp. 2017.
32. StataCorp. Stata: Release 14. Statistical Software. College Station, TX: StataCorp LP.; 2015.
33. Substance Abuse and Mental Health Services Administration. TIP 29: substance Use Disorder Treatment for People With Physical and Cognitive Disabilities. https://store.samhsa.gov/product/TIP-29-Substance-Use-Disorder-Treatment-for-People-With-Physical-and-Cognitive-Disabilities/SMA12-4078.
34. Mistler CB, Idiong CI, Copenhaver MM. Integrating Cognitive Dysfunction Accommodation Strategies Into Behavioral Interventions for Persons on Medication for Opioid Use Disorder. Original Research. Front Public Health. 2022;10:825988.
35. Mistler C, Copenhaver M. Integrating Cognitive Dysfunction Accommodation Strategies into an HIV Prevention Session: a 2-Arm Pilot Feasibility Study. Int J Environ Res Public Health. 2022;19(15):9430. doi:10.3390/ijerph19159430
36. Wang Y, Wouldes T, Russell B. Methadone Maintenance Treatment and Cognitive Function: a Systematic Review. Curr Drug Abuse Rev. 2013;6(3):220–230. doi:10.2174/18744737112059990020
37. Carroll KM, Rounsaville BJ, Nich C, Gordon LT, Wirtz PW, Gawin F. One-year follow-up of psychotherapy and pharmacotherapy for cocaine dependence. Delayed emergence of psychotherapy effects. Arch Gen Psychiatry. 1994;51(12):989–997. doi:10.1001/archpsyc.1994.03950120061010
38. Baldacchino A, Armanyous M, Balfour DJK, Humphris G, Matthews K. Neuropsychological functioning and chronic methadone use: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2017;73:23–38. doi:10.1016/j.neubiorev.2016.11.008
39. Gwadz MV, Collins LM, Cleland CM, et al. Using the multiphase optimization strategy (MOST) to optimize an HIV care continuum intervention for vulnerable populations: a study protocol. BMC Public Health. 2017;17(1):383. doi:10.1186/s12889-017-4279-7
40. Collins L. Optimization of Behavioral, Biobehavioral, and Biomedical Interventions: The Multiphase Optimization Strategy (MOST). Cham: Springer International Publishing. 2018;10:978.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

