Back to Journals » Journal of Pain Research » Volume 18
An Evidence-Based Consensus for the Use of Neurostimulation for the Treatment of Non-Surgical Low Back Pain: The NEURON Group
Authors Deer TR , Pope JE, Petersen EA, Abdallah RT, Amirdelfan K, Azeem N , Bansal V, Barkoh K, Chapman KB , Denis DR, Dorsi MJ, Escobar A, Falowski SM , Garcia RA, Hagedorn JM , Heros RD , James WS, Kalia H , Lansford T, Malinowski MN , Manzi SM, Mehta P, Moghim RZ, Moore GA, Motivala SL, Navalgund YA, Patel RG , Pilitsis JG , Schatman ME , Shumsky PM, Strand NH , Tomycz ND, Yue JJ, Sayed D
Received 16 October 2024
Accepted for publication 23 February 2025
Published 14 March 2025 Volume 2025:18 Pages 1247—1274
DOI https://doi.org/10.2147/JPR.S500342
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Krishnan Chakravarthy
Timothy Ray Deer,1 Jason E Pope,2 Erika A Petersen,3 Rany T Abdallah,4 Kasra Amirdelfan,5 Nomen Azeem,6 Vishal Bansal,7 Kaku Barkoh,8 Kenneth B Chapman,9,10 Daniel R Denis,11 Michael J Dorsi,12 Alexander Escobar,13 Steven Michael Falowski,14 Rosa Amelia Garcia,15 Jonathan M Hagedorn,16 Robert D Heros,17 Whitney S James,18 Hemant Kalia,19 Todd Lansford,20 Mark N Malinowski,21 Suzanne Marie Manzi,22 Pankaj Mehta,23 Robert Z Moghim,24 Gregory Anthony Moore,25 Soriaya Lizette Motivala,26 Yeshvant A Navalgund,27 Raj G Patel,28 Julie G Pilitsis,29 Michael E Schatman,30,31 Philip Michael Shumsky,32 Natalie Holmes Strand,33 Nestor D Tomycz,34 James J Yue,35 Dawood Sayed36
1Pain Services, Spine and Nerve Center of the Virginias, Charleston, WV, USA; 2Evolve Restorative Center, Santa Rosa, CA, USA; 3Department of Neurosurgery, University of Arkansas for Medical Sciences, Little Rock, AR, USA; 4Pain Management, Apico Pain Management, Bear, DE, USA; 5Director of Clinical Research, Boomerang Healthcare, Walnut Creek, CA, USA; 6Pain Medicine, Florida Spine & Pain Specialists, Riverview, FL, USA; 7Department of Pain Medicine, the University of Texas MD Anderson Cancer Center, Houston, TX, USA; 8Orthopaedic Associates, Houston, TX, USA; 9Department of Anesthesiology, NYU Langone Medical Center, New York, NY, USA; 10Department of Anesthesiology, the Zucker School of Medicine at Northwell, New York, NY, USA; 11Neurosurgery, Ochsner Health, New Orleans, LA, USA; 12Neurosurgery, University of California Los Angeles, Los Angeles, CA, USA; 13Anesthesiology and Pain Medicine, University of Toledo, Toledo, OH, USA; 14Neurosurgery, Neurosurgical Associates of Lancaster, Lancaster, PA, USA; 15Department of Pain Medicine, University of Florida, Gainsville, FL, USA; 16Department of Anesthesiology and Perioperative Medicine, Mayo Clinic, Rochester, MN, USA; 17Spinal Diagnostics, Tualatin, OR, USA; 18Neurosurgery, James-Marco Health, Prescott, AZ, USA; 19Center for Research & Innovation in Spine & Pain (CRISP), Rochester, NY, USA; 20South Carolina Sports Medicine, Charleston, SC, USA; 21OhioHealth Neurological Physicians, OhioHealth, Columbus, OH, USA; 22Physician Co-Owner, Performance Pain and Sports Medicine, Houston, TX, USA; 23Division of Pain and Minimally Invasive Surgery, Pain Specialists of America, Austin, TX, USA; 24Interventional Spine and Pain, Colorado Pain Care, Denver, CO, USA; 25Pacific Sports and Spine, Eugene, OR, USA; 26Department of Neurosurgery, Northwell Health, New York, NY, USA; 27Office of the Chief Medical Officer, National Spine and Pain Centers, Frederick, MD, USA; 28Interventional Pain Management, Capitol Pain Institute, Austin, TX, USA; 29Department of Clinical Neurosciences, Florida Atlantic University, Boca Raton, FL, USA; 30Department of Anesthesiology, Perioperative Care & Pain Medicine, NYU Grossman School of Medicine, New York, NY, USA; 31Department of Population Health – Division of Medical Ethics, NYU Grossman School of Medicine, New York, NY, USA; 32Anesthesiology and Pain Medicine, Evolve Restorative Center, Santa Rosa, CA, USA; 33Anesthesiology and Pain Medicine, Mayo Clinic, Phoenix, AZ, USA; 34Neurological Surgery, Allegheny Health Network, Pittsburgh, PA, USA; 35Frank h Netter School of Medicine, Quinnipiac University; CT Orthopaedics, Hamden, CT, USA; 36Anesthesiology and Pain Medicine, the University of Kansas Medical Center, Kansas City, KS, USA
Correspondence: Timothy Ray Deer, Spine and Nerve Center of the Virginias, 400 Court Street, Suite 100, Charleston, West Virginia, 25304, USA, Tel +1 304 347-6141, Email [email protected]
Introduction: The use of electrical neuromodulation has often been limited to those with previous back surgery, peripheral neuropathy, and complex regional pain syndrome. Many patients with severe intractable low back pain were thought to be candidates for spinal cord stimulation (SCS), dorsal root ganglion stimulation, or peripheral nerve stimulation but did not meet the criteria. Recently, additional high-level data has supported the use of SCS in non-surgical low back pain (NSLBP), and United States Food and Drug Administration approval has been granted. The American Society of Pain and Neuroscience (ASPN) executive committee realized an unmet need to develop criteria for patient selection for this specific patient population. This is a NEURON project (neuroscience, education, utilization, risk mitigation, optimal outcomes, and neuromodulation), a living guideline for evolving therapies and indications, and is focused on the use of neuraxial stimulation for the treatment of refractory pain.
Methods: After board approval, the society accepted nominees for the project, with an emphasis on experience, publication, research, and diversity. The team created an outline for discussion, chose a grading system based on published guidelines, and created consensus points.
Results: The evidence led to several consensus points to best guide patient selection based on the level of evidence and expert opinion. The results will lead to improved safety and efficacy in implanted patients, and to a new standard for best practices.
Conclusion: The selection of patients for implantation in those who have NSLBP should be based on published literature, best practice, and expert opinion. This NEURON project will allow for regular updates to create a living guideline that will allow for better assimilation of information to improve safety and efficacy going forward.
Keywords: spinal cord stimulation, SCS, low back pain, lumbar degenerative disc disease, non-surgical back, non-surgical low back pain, NSLBP, failed back surgery syndrome, dorsal root ganglion stimulation, DRG, DRG-S, peripheral nerve stimulation, PNS
Introduction and Objectives
Non-Surgical Low Back Pain: Defining the Problem
Chronic low back pain (CLBP) affects approximately 13.1% of the US population and is linked with a higher level of medical comorbidities, health care costs and lost productivity.1,2 Although acute low back pain (LBP) typically resolves within 3 months, approximately 2% to 48% of patients progress to developing CLBP,3,4 with one-third of this population experiencing moderate-to-severe pain intensity.3 The management of CLBP can be multimodal and has a wide range of options. The important role of “collaboration in decision-making among different disciplines” is critical to determining when the patient with CLBP is accurately defined as a patient with also non-surgical low back pain (NSLBP). While the definition of NSLBP will undoubtedly evolve with the accessibility of innovative surgical approaches, it is important to define what NSLBP is today, currently with the writing of this guidance.
Despite considerable amounts of research completed on CLBP, there are inconsistent definitions and assessments. For this guideline, NSLBP refers to patients who have failed to respond to conventional medical management (CMM), have no history of spine surgery, and are not appropriate candidates for surgical intervention.1 CMM refers to physical or occupational therapy, analgesic medications, nerve blocks, steroid injections, radiofrequency ablation and other validated treatments for lumbar pain.1 The second qualifier, “not appropriate candidate for surgical intervention”, in this definition, means the absence of a symptomatic surgically correctable lesion or pathology. Patients with correctable surgical lesions who are not candidates due to comorbidities are not included in the study designs included in this guidance and will be considered in future guidance.
The etiology of NSLBP is multifaceted, often due to a combination of factors including but not limited to degenerative disc disease, facet joint disease, herniated discs, fractures, and spinal stenosis.5 Acute exacerbations can be triggered in these individuals from muscle and ligament strains, commonly precipitated by poor posture, lifting or abrupt movements. There is also an increased risk and severity of back pain in individuals with psychosocial factors such as anxiety and depression.3,5,6 Less advanced levels of education serve as strong predictors of prolonged episode duration and poorer outcomes.5
Taking this into consideration, NSLBP is a prevalent condition that is not limited to any specific demographic. It is associated with age, with the highest incidence in the third decade of life and increasing prevalence with age up to 60 to 85 years old.5,7 LBP is expected to rise in prevalence and incidence due to increasing sedentary behaviors and an aging population.7,8
Despite many therapeutic advances for this common and life altering condition, there are still controversies that exist, and many questions arise in the field that merit being addressed in guidelines.
- Is the use of neuromodulation an appropriate therapy for both mechanical/nociceptive and neuropathic pain, or is it more specific to pain of neuropathic origin?
- Is the degree of spinal stenosis well defined in NSLBP? Should we implant those with severe spinal stenosis that is not correctable?
- Do we need thoracic magnetic resonance imaging (MRI) as surgical staging in all patients or only those scheduled for paddles in pre-surgical work-up?
- What level of non-surgical scoliosis is appropriate for spinal cord stimulation (SCS) in NSLBP or is this a medical judgement decision?
The objective of the American Society of Pain and Neuroscience (ASPN) NEURON (neuroscience, education, utilization, risk mitigation, optimal outcomes, and neuromodulation) project for the treatment of NSLBP with neuromodulation is to provide evidence-based recommendations to address the appropriate utilization of this therapy in a group of patients who previously were treated on a case-by-case basis with no guidance. This guidance comes at a time of new peer-reviewed literature analyzed in this publication.
This guideline is intended to represent a comprehensive review of the neuromodulation options for those suffering from CLBP with NSLBP and offer recommendation based on the level of evidence and consensus. As this is a living document, this ASPN NEURON project is intended to be updated periodically to maintain relevance with the current treatment landscape and literature. The ASPN NEURON guidance does not necessarily represent a standard of care, but an expert driven assimilation of evidence to help develop patient centric treatment approaches and does not replace treatment based on an individual patient’s need and the physician’s professional judgement and experience. Further, this guideline is not intended to be used as the sole reason for denial or approval of treatment or services. See Table 1.
 |
Table 1 Consensus Statement on Candidacy for Surgery Vs Neuromodulation |
Methods for Literature Search, Evidence Ranking and Consensus Development
Working Group
The ASPN clinical guideline committee is comprised of a diverse group of physicians representing the specialties representative of the membership of ASPN and engaging in the care of patients suffering from NSLBP, including anesthesiology, neurosurgery, orthopedic surgery, physical medicine and rehabilitation, and radiology, as well as a pain psychologist/medical ethicist with many years of experience in consulting with implantable devices. Committee members were selected based on clinical experience, research, and previous publication history.
Disclosures of Potential Conflicts of Interests
All participants involved in the guideline development have been required to disclose all potential conflicts of interest, financial or otherwise. Although guidance exists regarding grading potential degree of conflict of interest and assessing the potential of bias, the organizing committee elected to have unbiased committee members finalize and approve consensus statements. All evidence grading was reviewed and validated by committee members with no perceived conflict of interest in any specific therapy. Authors with conflicts of interest on subjects with grading criteria were recused from those sections as appropriate.
Literature Review
The world literature in English from 2000 to May 2024 was searched using Medline, EMBASE, Cochrane CENTRAL, BioMed Central, Web of Science, Google Scholar, PubMed, Current Contents Connect, Meeting Abstracts, and Scopus to identify and compile the evidence for lower back interventional therapies for the treatment of pain. During the peer review process additional articles were identified, and the search was expanded to include articles through December 2024. Search words were created specific to the topics for each major section pertaining to SCS, dorsal root ganglion stimulation therapy, and peripheral nerve stimulation. The search terms included low back pain, neuromodulation, neurostimulation, non-surgically correctable back pain, spinal cord stimulation, dorsal root ganglion stimulation, and lumbar disc disease. Identified peer-reviewed literature was critiqued using the United States Preventive Services Task Force (USPSTF) criteria for quality of evidence,9 with modifications for neuromodulation therapies (Table 2). The hierarchy of evidence for the project considered randomized controlled trials (RCT) as the preeminent classification, followed by prospective observational studies, case series and finally expert opinion. Per the methodology, the process identified RCT and prospective observational studies of Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) criteria quality in the creation of guidelines. Interventions with more than one RCT were considered to have sufficient evidence to create conclusions, and observational studies were not considered. Interventions with no RCTs or only one RCT then also utilized prospective observational studies in the creation of guideline recommendations. Should an intervention be found to have no RCTs or observational studies, case series were used. These are clearly denoted by the taxonomy of the recommendation that the predominant quality of evidence is of a classification less than RCT. For interventions where RCT and prospective observational studies of requisite quality (STROBE) are not available, case series and/or expert opinion may be used in the creation of guidelines to fill in the current literature gap to assist the clinician in selecting care pathways. These designations follow a modified USPSTF process used previously by ASPN in the creation of guidelines. The details are listed in Table 2. After USPSTF letter grading was assigned, the working subgroup then assigned the “level of certainty regarding benefit” as described in Table 3. Definitions for the level of consensus are in Table 4.
 |
Table 2 Quality of Evidence Ranking Using United States Preventative Services Task Force Criteria Modified for Therapy |
 |
Table 3 Levels of Certainty Regarding Net Benefit |
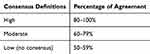 |
Table 4 Level of Consensus Definitions |
The ASPN neuromodulation group for NSLBP formulated consensus points based on graded evidence in the literature and the consensus of the authors.
Scope and Purpose: Why is Non-Surgical Low Back Pain Consensus Needed?
Previously, SCS has been proven to reduce costs and healthcare resource utilization vs CMM in conditions such as failed back surgery syndrome (FBSS), complex regional pain syndrome (CRPS), and painful diabetic neuropathy.11–13 The CMM for refractory NSLBP has historically consisted of medications, physical therapy, and interventional procedures (epidural steroid injections, nerve blocks, nerve ablations, etc.). There is a substantial economic burden associated with CMM for NSLBP, and opioids remain the most commonly prescribed medication.14 Surgery for chronic CLBP, such as spinal fusion, has not been shown to offer significant improvement in disability compared to CMM.15,16 Recent studies have demonstrated the superiority of SCS vs CMM in terms of pain scores, disability, pain catastrophizing, quality of life, and daily opioid use.1,17
Along with improvements in pain and patient-related outcomes, there is an economic benefit from the use of SCS for NSLBP. A 2023 prospective, randomized controlled trial comparing SCS to CMM for NSLBP over 12 months found a 33% average reduction in healthcare utilization cost in the SCS arm as compared to CMM.18 The cost-effectiveness of SCS was estimated to be achieved within 2.1 years. The study also reported a superior incremental cost-effectiveness ratio in the SCS arm, such that a significant quality of life improvement was achieved at a lower cost. A 2019 retrospective study evaluating cost before and after implantation of SCS for LBP found that the average total cost reduction at 6 months post-implantation was approximately $5840.19 The study estimated the time to offset total device costs to be approximately 2.3 years. Other studies evaluating SCS for this condition have found parallel reductions in opioid use, healthcare utilization, and pain-related procedures, suggesting similar economic benefits.20,21 Overall, there is increasing clarity and evidence for the favorable long-term economic impact of SCS in this population.
A myriad of studies also support the enhancement of quality of life (QOL) with SCS. This brief review summarizes the data from methodologically robust studies supporting SCS to improve QOL since the advent of new SCS waveforms more recently. Reviews, which tend to mix older and newer technologies, were excluded.
The 2017 study of 10kHz SCS (Nevro, Menlo Park, CA, USA)22 by Al-Kaisy and colleagues included QOL as a secondary outcome, determining a significant improvement at 1-year post-implant as measured by the EuroQOL 5-Dimensional Questionnaire (EQ-5D). In the 3-year follow-up study,20 significant improvement in QOL scores were once again identified, with even greater improvement than the 1-year data. Subsequent studies involving new waveform technologies1,18,23–29 have yielded similar results.
The results of a 2018 study by Amirdelfan et al in which QOL was a primary outcome measure, compared 10,000 Hz stimulation therapy to traditional low-frequency SCS. The authors determined that based on multiple measures (perceived disability, functionality, sleep, pain interference, and subject satisfaction), significantly greater gains occurred on all five measures in the 10,000 Hz stimulation therapy group as compared to the traditional SCS group.30
In all methodologically sound studies of novel waveform SCS strategies for LBP in which QOL was measured, significant improvements in life quality were identified. These findings were strongly supported in a recent systematic review/meta-analysis.31 However, a recent Cochrane Review32 did not support the use of SCS for the treatment of LBP, but this has been widely criticized by many because it excluded many level one studies approved and monitored by the United States (US) Food and Drug Administration (FDA). It has been stated that this Cochrane Review attempt to reduce bias led to an opposite effect of creating a negative bias against SCS.33,34
It is important to note that not all NSLBP patients are candidates for neuromodulation. For the purposes of this article, patients who have not responded to conservative strategies for treatment were not candidates. Of note, the efficacy of these interventional non-implantable approaches was more comprehensively described in the ASPN Back Guideline.9
Current Evidence for Neuromodulation with Spinal Cord Stimulation
Spinal Cord Stimulation Food and Drug Administration Labeling
FDA labeling for SCS therapy is manufacturer-specific and updated on a regular basis. The FDA approval process involves rigorous scientific and regulatory evaluation, aiming to ensure that the product’s benefits outweigh its potential risks, keenly evaluating safety and efficacy.35 Sponsors must submit comprehensive data from preclinical and clinical studies to demonstrate the product’s safety and efficacy. Once approved, the product can be legally marketed and distributed commercially in the United States, instilling confidence among healthcare providers, patients, and consumers in its safety and effectiveness. FDA approval serves as a critical milestone, opening doors to broader commercialization and accessibility of therapies for patients in need.
The FDA first approved SCS therapy for the treatment of chronic moderate or severe refractory pain in the trunk and limbs in 1989.36 Since then, in response to numerous clinical studies,1,17,37–47 the FDA has expanded indications for SCS therapies to specifically include treatment of failed back surgery syndrome, intractable LBP, intractable leg pain, diabetic peripheral neuropathy of the lower extremities, angina, and chronic limb ischemia.48–50 In February 2022, the FDA approved SCS therapy for the treatment of refractory NSLBP.49,50
Evidence of Efficacy for Spinal Cord Stimulation in the Treatment of Non-Surgical Low Back Pain
SCS is the most studied and established form of neuromodulation and its use for chronic pain related to FBSS, CRPS, and diabetic neuropathy has been supported via multiple RCTs.51 Despite a dearth of knowledge as to the therapeutic mechanisms behind not only conventional tonic SCS but also behind novel SCS waveforms, the clinical efficacy of SCS has been buttressed by more RCTs than any other form of neuromodulation, and some of these RCTs have met the criteria of high-quality.52 Moreover, the advent of paresthesia-free waveforms in SCS has heralded in a new era of SCS trials which involve a placebo or sham arm.53 Despite challenges in placebo/sham control and blinding in SCS trials, these studies have overall helped to improve the level of efficacy evidenced in SCS and have helped to strengthen the therapeutic benefit of SCS. There are numerous prospective studies of SCS that show it may reduce opioid consumption, improve quality of life, enhance return to work, and reduce the cost of health care.30,54,55
Historically, neurostimulation has been viewed as a therapy of last resort, when all other treatments – including surgery – have failed, and more so has been viewed as a treatment primarily for neuropathic lower extremity pain. For example, a 2014 review of SCS indications and patient selection highlighted sixteen indications; NSLBP was not one of them.56 To date, five (5) RCT studies have been conducted specifically investigating SCS for NSLBP.
Kapural et al 2022 randomized 159 patients with nonsurgical refractory back pain to either CMM or 10,000 Hz stimulation therapy, with an optional 6-month crossover for the CMM group.1 The primary endpoint was the percentage of patients with >50% reduction in numeric rating scale (NRS) at 3 months; 80.9% of the treatment group reached this endpoint as compared to only 1.3% of CMM patients. These numbers were stable at 6 months (80% vs 2.7%). Other 6-month secondary endpoints included ≥10-point reduction in Oswestry Disability Index (ODI) ratings (78.5% SCS vs 4% CMM), Patient Global Impression of Change (PGIC) (70.8% “Better” or “A great deal better” for SCS and 1.3% in CMM), and change in opioid use (−45.8% SCS and +12.1% CMM). Finally, when the CMM group was allowed to crossover to SCS treatment, their results were equivalent to that of the original SCS treatment group. More recently, 24-month results were published from the implanted cohort, in which 98 patients completed the 24-month follow-up. At 24 months after implantation, the mean back pain visual analog scale (VAS) score was reduced by 73%, and the responder rate was 82%. ODI and EQ-5D-5L both improved by twice the minimum clinically important difference (MCID) difference for each measure. The rates of serious adverse events (3.4%) and surgical device explants (4.8%) were low.57
Patel et al, 2024 conducted a multicenter RCT evaluating 10,000 Hz stimulation therapy plus CMM versus CMM alone for NSLBP.57 One hundred and fifty-nine patients were randomized, and a 6-month crossover option was provided for the CMM group. The primary endpoint, ≥50% pain relief on the VAS at 3 months, was achieved by 80.9% of SCS patients versus 1.3% of CMM patients, with stable results at 6 months (80% vs 2.7%). Secondary endpoints included ≥10-point ODI improvement (79% SCS vs 4% CMM), PGIC (71% “better” or “greatly better” for SCS vs 1.3% CMM) and reduced opioid use (−17.7 morphine milligram equivalents [MME] for SCS, unchanged in CMM). After crossover, SCS outcomes mirrored those of the original SCS group. At 24 months, in the implanted cohort (n=125), 98 patients completed follow-up. VAS back pain scores improved by 74%, with 82% achieving ≥50% pain relief and 58% achieving ≥80% relief. ODI and EQ-5D-5L scores improved by over twice the minimum clinically important difference. Serious adverse events (3.4%) and device explants (4.8%) were infrequent. Results confirm the long-term efficacy and safety of 10,000 Hz stimulation therapy for NSLBP.
Deer et al (2023) published the initial results from DISTINCT, an ongoing multicenter prospective randomized controlled trial comparing the use of passive recharge burst SCS (BurstDR, Abbott Neuromodulation, Austin, TX, USA) and conventional medical management in the treatment of refractory NSLBP.58 The primary endpoint was ≥50% reduction in NRS at 6 months for the first 200 patients enrolled. This was achieved by 72.6% of SCS patients vs 7.1% of CMM patients. An analysis of the overall cohort (N=269) revealed almost identical results. Secondary outcomes included a composite responder rate combining NRS and ODI outcomes (91% for SCS vs 16% for CMM), ODI improvement (30.6 points SCS, 0.7 points CMM) and meaningful change in the Pain Catastrophizing Scale (PCS) (88.2% SCS vs 23.5% CMM). DISTINCT will follow patients for 24 months and is a Level I Investigational Device Exemption study audited and monitored by the FDA.
In a study by Kallewaard et al (2024), differential targeted multiplexed (DTM) SCS (Medtronic Neurological, Minneapolis, MN, USA) was compared to conventional medical management in a group of 112 patients with persistent back pain who were ineligible for spine surgery. The primary endpoint of the study was the responder rate of patients achieving at least 50% benefit from the associated treatment as assessed using VAS scoring. These patients were followed to 24 months post implantation. The secondary endpoints included a comparison of changes in responder rates at 1, 3, 9, 12, 18, and 24 months, as well as changes in the ODI, EQ-5D-5L, PGIC, and opioid consumption. Patients in the DTM SCS group demonstrated a high responder rate exceeding 80%, with a mean reduction in symptoms of at least 70% reduction in symptoms, when compared to conventional medical management. Importantly, these results were sustained through the 24-month period.59
These studies show extremely promising results and demonstrate that SCS is superior to CMM for the NSLBP patient population. These results are early, however, and long-term outcomes are still needed before this patient population is more widely adopted as good SCS candidates. See Tables 5 and 6.
 |
Table 5 Literature Summary for Efficacy of SCS in NSLBP |
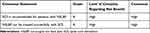 |
Table 6 Consensus Statement for SCS in NSLBP |
Diagnostic Testing for the Non-Surgical Low Back Pain Population
Patient selection is critical in the assignment of candidacy for NSLBP. The identification of a surgically correctable lesion precludes the diagnosis. Flexion and extension films to assess dynamic instability may be considered. Assessment of any sagittal and/or coronal deformity should be performed. Assessment of fractures (traumatic, osteoporotic and/or pathologic) and other imaging should be ascertained as needed. Plain x-ray analysis is followed by lumbar MRI evaluation. Patients with surgical pathology with concomitant complementary subjective and objective findings should undergo surgical evaluation. If there is no indication of surgery, the patient may undergo a thoracic MRI scan to assess spinal canal patency prior to undergoing SCS trialing. Thoracic preoperative MRI findings had an impact on surgical planning for 22% of patients, and in 3% of cases, additional surgical decompression was necessary to ensure safe paddle lead placement, according to one study.64
The presence of intrinsic spinal cord pathology may also be a relative contra-indication for SCS technology. Thoracic plain x-ray analysis can be obtained if there is concern for scoliosis. If there is a potential for the comorbidity of peripheral neuropathy, electromyography (EMG) can be performed. EMG assessment can be useful in planning trial electrode placement to optimize coverage of lower extremity symptomatology. This will not impact lead placement for NSLBP, however.
If MRI evaluation is contra-indicated, computed tomography (CT) imaging with the consideration of a myelogram of the thoracic and lumbar spine should be performed pre-operatively. The same assessment as above is then made following CT/myelogram testing.
It is essential to exercise prudence when interpreting imaging results and attributing causality of symptoms to any abnormal structural findings observed in the images. For example, emerging evidence indicates that traditional MRI evaluation may overestimate lateral recess dimensions in patients with lumbar spinal stenosis. A study demonstrated a reduction in foraminal area during upright and hyperlordotic positioning, which are positions associated with maximal symptoms.65 Additionally, the application of artificial intelligence (AI) and machine learning in imaging analysis shows promise in comprehensive evaluation, with a recent study showing comparable detection rates for central canal and lateral recess stenosis compared to sub-specialist radiology evaluation.66
Although not always applicable to NSLBP pain patients, in those with coexisting limb pain, electro-diagnostic testing may be helpful where radiculopathy and plexopathy may be indistinguishable, especially in ambiguous clinical presentations or those situations where diagnostic injections are unclear. In some cases, it may be used in conjunction with the patient’s clinical presentation to help determine the etiology of pain generation. For example, a study that enrolled 108 patients opined that certain electrophysiological parameters are helpful in diagnosing lumbosacral radiculopathy.67 In addition, EMG abnormalities were found in less than 50% of cases and could be predicted by specific clinical findings. This discrepancy between test results and symptoms is also observed in asymptomatic control subjects. While EMG and nerve conduction velocity (NCV) testing can be helpful additional diagnostic tools in differentiating peripheral neuropathy from lumbar spinal stenosis, they may lack the necessary specificity to provide definitive diagnostic aid.68–70
Therefore, a comprehensive diagnostic approach to identify and treat the root cause of pain can enhance the overall effectiveness of SCS therapy in such situations (see Table 7).
 |
Table 7 Consensus Statement on Diagnostic Testing in NSLBP |
Demographic Considerations for Spinal Cord Stimulation in the Non-Surgical Low Back Pain Population
Age/gender: Clinical studies on SCS implantation showed age-related differences in outcomes. In successful SCS cases (those with ≥ 50% pain relief), the median age was 54 years (interquartile range [IQR] 42–60 years) compared to 66 years (IQR 50–76 years) in unsuccessful cases. SCS effectively manages pain in patients both under 75 and over 75 years old, with similar complication rates, making it a suitable option for older adults.71–73 A survey study included patients of years 2000–2009 and significant variation in conversion rate by geographic area (patients in the North Central region vs Northeast region: odds ratio 1.48, 95% confidence interval (CI) [1.31, 1.66]; p < 0.0001).74 Younger patients had higher success rates with full implantation, while older patients faced a greater risk of explantation.74 However, a recently published study showed that from 2009 to 2018, SCS implantation rates in the Medicare group increased substantially, with notable rises in all age groups.75 Although women demonstrated more of a preponderance for device explant due to discomfort, SCS pain relief did not differ by sex,76 indicating that analgesic success is gender-neutral despite variances in device comfort.
Race/ethnicity: In the Medicare population, significant racial disparities were evident in the rates of SCS trials and placements. Caucasians led with the highest rates, with SCS trials increasing from 32 per 100,000 in 2009 to 72 in 2018, and placements from 19 per 100,000 to 47 in the same period. African Americans showed more moderate increases, with trials going from 21 to 35 per 100,000 and placements from 13 to 20 per 100,000. Other racial groups experienced the most substantial relative increase in placements, from 3 per 100,000 in 2009 to 10 in 2018, a 211% rise, compared to a 143% increase for Caucasians and 54% for African Americans.75,77
Body mass index (BMI): As obesity rates rise, more obese patients are receiving SCS implants without a corresponding increase in hospitalization costs compared to their non-obese counterparts. Obesity is associated with a higher risk of 30-day readmission and mechanical complications following SCS implantation.78 For each increment in BMI, SCS effectiveness decreases by 2% vs 20% for underweight and/or normal patients (≤24.9), though pain scores improved at 6–12 months in both groups, respectively.78 Individuals having a BMI ≥36.5 kg/m2 experienced less improvement at 6–12 months.79 Nevertheless, patients with a BMI of 40 or higher exhibit a mere 5.48% complication rate and a significant trial success rate of 93.3%, which is considerably higher than the 74.4% observed in those with a lower BMI.80
Pregnancy: The published literature surrounding spinal cord stimulation and pregnancy is primarily presented in case reports and small retrospective case series.81–90 The majority of the patients did not experience any complications, however complications of intrauterine growth retardation, hypertension, and abortion were reported in singular case reports.85,87,88 Causality is not noted and may be unrelated, but additional study is indicated.
History of chronic bleeding disorders: As spinal cord stimulation has expanded in use, the management of complex medical comorbidities has become more common as well. This includes chronic bleeding disorders. These disorders differ extensively from the management of anticoagulation medications, as the risk for these patients extends beyond the perioperative time frame when anticoagulation medications have specific discontinuation and restart time periods. In patients with chronic bleeding disorders, the risk of bleeding is ever-present, and given the permanent implantation of spinal cord stimulation hardware, the pain physician must be ready to identify and co-manage bleeding complications.
History of metallurgic allergy: Allergic contact dermatitis is a delayed-type hypersensitivity reaction caused by allergen-specific T-cells and subsequent T-cell-mediated response.91 Allergic contact dermatitis occurs in approximately one in five people, but the incidence in spinal cord stimulators is very low, estimated around 0.1%.92 These patients will present with chronic progressive cutaneous symptoms and discomfort without signs or symptoms of infection.
Increased risk of infection: Surgical site infection is one of the most serious complications of SCS trial and implantation. The overall incidence of surgical site infection following SCS implantation has been reported between 2.45% and 3.11%.93,94 Unfortunately, when this occurs treatment involves explantation of the implanted device, loss of therapy, and treatment with systemic antibiotics. Patient-related factors that increase the risk of post-operative surgical site infection include uncontrolled diabetes, advanced age, intravenous drug use, human immunodeficiency virus infection, immunosuppression, history of cancer, renal failure, infection at a distant source, liver cirrhosis, history of cigarette smoking, and history of prior surgical site infections.94
For the NSLBP patient population, there are no special techniques for SCS that need to be considered. In patients without existing disease states, the physician should follow standard of care when placing the trial leads and permanent leads and pulse generator. This should involve an awake, communicative patient. If general anesthesia is performed, the use of intraoperative neuromonitoring is recommended. For SCS devices utilizing a paresthesia-based programming, the leads should be placed in an area to allow paresthesia coverage over the painful areas. For SCS devices that are paresthesia-independent, the leads can be placed anatomically. In general, the SCS trial will last for approximately three to fourteen days depending on factors such as time off blood thinners, travel time and complexity. A successful trial involves pain relief and/or functional improvement of at least 50%. Currently, there are no measures that define success after implantation, but 50% improvement in pain is the most commonly reported metric. A summary of these findings is given in Table 8, and ASPN consensus statements are in Table 9.
 |
Table 8 Literature Summary of Demographic Considerations for SCS |
 |
Table 9 Consensus Statement on Patient Selection Criteria for SCS in NSLBP |
Lead Type, Waveform, and Frequency for Spinal Cord Stimulation in Non-Surgical Low Back Pain
There are several SCS paradigms that have demonstrated efficacy for NSLBP.1,17,47 The DISTINCT study compared SCS to CMM in patients with NSLBP. The study found a significant reduction in pain and pain-related disability with the use of passive recharge burst stimulation sustained at 12 months post-implant.17,47 The passive recharge burst stimulation paradigm consists of a five-pulse train stimulus at an internal frequency of 500 Hz delivered at 40 Hz intervals and was delivered via a paddle or percutaneous implanted electrodes.95,96 SCS implants in this study consisted of both percutaneous and paddle leads, primarily placed between T7 and T9.
The 2022 prospective RCT by Kapural et al examining 10,000 Hz stimulation therapy also demonstrated superiority versus CMM.1 The study reported significant improvement in pain, pain-related disability, quality of life, and daily opioid dose at 12 months post-implant in the SCS arm. This stimulation paradigm delivers electrical pulses at high frequency up to 10,000 Hz, with a 30 microsecond waveform.97,98 This combination allows paresthesia-free delivery of stimulation. SCS implants in this study consisted of percutaneous leads only, primarily placed between T8 and T11.
The EVOKE randomized controlled trial compared a novel, physiologic real-time closed-loop controlled evoked compound action potential (ECAP)-controlled, closed-loop SCS system (Evoke, Saluda Medical, Sydney, Australia) with a fixed output open-loop SCS system for back and leg pain of all types, finding significantly higher responder rates at 24 months within the closed-loop SCS arm.99,100 This stimulation paradigm measures ECAPs up to 4 million times per day to automatically adjust the strength of stimulation in order to deliver a maintain a consistent activation of the spinal cord. While the study only had a sub-population of a NSLBP population, the inclusion of this population in this RCT suggests that closed-loop stimulation paradigm may yield similar outcomes for the NSLBP population, although no conclusions can be made due to study design. Future studies will be needed to further establish its use for NSLBP. Fishman and colleagues performed a multicenter randomized controlled study to establish the impact of DTM SCS on low back pain, including a small population with non-surgical back pain. In this study, they compared the effectiveness of the novel therapy to traditional tonic SCS. This was done post-market and was not subject to FDA oversight since it was not an IDE. In addition, the endpoint was at 3 months. One hundred and twenty-eight subjects were treated in 12 centers, 67 multiplexed SCS and 61 traditional SCS. Only 46 patients reached the 3-month endpoint. In that implanted analysis, 80.1% of those treated with the novel waveform responded compared to 51.2% of conventional SCS (p = 0.0010). In that group, this response was maintained to 12 months. The small implant group and the post-market design make it difficult to make conclusions about the NSLBP group.101
White and colleagues demonstrated the efficacy of DTM when compared to conventional spinal cord stimulation in patients with chronic refractory axial low back pain who were not candidates for spine surgery.60 Study subjects totaled 121 patients randomized into two groups. The primary endpoint was the responder rate, defined as the proportion of patients achieving at least a 50% reduction in chronic low back pain at three months, assessed in a modified intention-to-treat population using both noninferiority and superiority hypotheses. Secondary endpoints included an analysis of mean changes from baseline VAS scores of chronic low back pain at 3, 6, 9 and 12 months, as well as the comparison of responder rates of the studied subjects at 6, 9 and 12 months. Additional outcome measures included analysis of leg pain VAS scores, Oswestry Disability Index changes, EQ5D-5L indices, as well as patient satisfaction and PGIC. At three months, the primary end point demonstrated statistical superiority of DTM spinal cord stimulation when compared to conventional spinal cord stimulation with a responder rate of 80.1% in the DTM SCS group compared to 51.2% in the conventional SCS group. These responder rates were maintained through 12 months with statistical superiority. Patients also demonstrated significantly better leg pain relief, less measured disability and perceived improvements in both satisfaction as well as quality of life. This study demonstrated that DTM spinal cord stimulation is clinically superior to traditional spinal cord stimulation in the treatment of chronic non-surgical low back pain up to 12 months.60
Ultimately, multiple SCS waveform, frequency, and lead types have demonstrated superior efficacy for NSLBP compared to CMM. Clinicians should ensure a thorough understanding of the differences in these stimulation paradigms and parameters and select the appropriate stimulation type based on patient criteria for each unique NSLBP patient, although no true guidance exists due to a paucity of data for a direct comparison. ASPN consensus statements are in Table 10.
 |
Table 10 Consensus Statement on Lead Type, Waveform, and Frequency for SCS in NSLBP |
Current Evidence for Neuromodulation with Dorsal Root Ganglion Stimulation for Non-Surgical Low Back Pain
Dorsal Root Ganglion Stimulation Food and Drug Administration Labeling
Dorsal root ganglion stimulation (DRG-S) received its FDA approval for the treatment of CRPS type I and type II and peripheral causalgia from the levels of T10 to S2 in February of 2016. This followed the CE Mark approval for use in the European Union in November 2011. Therefore, to note, the use of DRG-S for the treatment of NSLBP is off-label.
Dorsal Root Ganglion Stimulation for the Management of Non-Surgical Low Back Pain
In a 2020 study, seventeen consecutive patients suffering mainly from chronic axial LBP, with or without additional lower extremity pain, were examined.102 All participants underwent trials and subsequently received DRG-S implants with leads placed at T12 to target the low back. Notably, the stimulation levels were set at a very low intensity which was below the threshold for inducing paresthesias. The average follow-up period was 8.3 months. The results were encouraging, with over half of the patients experiencing significant pain relief of at least 80%, and an average relief of 78% for LBP at the last follow-up. Moreover, the study reported marked improvements in physical and mental functioning, reduced disability, and enhanced overall quality of life. In conclusion, T12 DRG-S proves to be an effective approach in treating chronic axial LBP. The stimulation leads to reduced pain and disability, leading to an improved quality of life for patients, all achieved without causing paresthesias.
Anatomically, the facet joints and posterior spinal structures are innervated by branches of individual spinal nerve roots, while the discs and anterior vertebrae receive innervation via L2. These nerve signals converge in the dorsal horn of the spinal cord around T8-T9. The T12 nerve root carries cutaneous afferents from the low back and reaches the dorsal horn of the spinal cord at T10.103 From there, Aδ and C-fibers from the low back ascend through Lissauer’s tract to T8-T9, where they join with other low back afferents. When DRG-S is applied at T12, it leads to the inhibition of the converged low back fibers through mechanisms involving endorphin and gamma-aminobutyric acid (GABA)ergic frequency-dependent processes. Consequently, T12 lead placement appears to be the most favorable location for DRG-S in treating LBP.104 In making this mechanistic revelation, clinical studies validate the theory. Chapman’s research showed significant pain reduction (76% VAS decrease), improved disability (78% ODI enhancement), better psychological well-being (93% improvement in mental functioning on the Short Form 36 health questionnaire [SF-36]), and enhanced physical health (108% boost in physical functioning on the SF-36). Notably, 70% of patients reduced opioid use, with two discontinuing entirely.104 In an additional study by Chapman and colleagues on 11 patients with FBSS and NSLBP showed positive outcomes: 77% VAS pain reduction, 62% ODI improvement, 80% EQ-5D enhancement, 24% improvement in mental functioning on the SF-36, and 104% improvement in physical functioning on the SF-36.105
Although not a specific study dedicated to NSLBP, a 2023 study conducted a retrospective analysis of patients with joint pain who underwent successful DRG-S trials and implants at the institute from September 2017 to September 2021.106 The case series included patients with intractable joint pain and without clear evidence of neuropathic pain. They used specific criteria and surveys to assess the presence of neuropathic pain. Baseline assessments for pain, function, quality of life, and joint surveys were taken before the trial and at follow-up appointments. The study identified five patients with refractory joint pain in the hip, knee, or ankle. The results showed a significant improvement in pain, function, and quality of life after DRG-S implantation. NRS pain scores improved by 74% from baseline to last follow-up, ODI scores improved by 65%, and EQ-5D scores more than doubled.
The findings suggest that DRG-S may be a valuable treatment option for predominantly refractory mechanical joint pain regardless of the location of the joint pain without a significant neuropathic component. The observed benefits could be due to DRG-S’s direct influence on nociceptive signaling at the DRG and within the spinal cord.104 This means it could be important in discogenic or facetogenic pain.
Lumbar intervertebral disc disruptions can result in severe discogenic LBP, negatively affecting both physical function and quality of life. A prospective study aimed to assess the impact of DRG-S in carefully selected patients with discogenic LBP who had no prior history of back surgeries was initiated. It was designed as a single-arm case series where DRG-S was studied as a treatment attributed to discogenic causes. The DRG-S was applied at the bilateral L2 level,107 with the rationale being the sympathetic convergence at this specific level, supported by the findings of Huygen et al.108 Twenty participants with confirmed discogenic LBP underwent DRG-S trials, and those with at least 50% pain reduction during the trial received permanent implants. Results showed a significant reduction in NRS scores (average 63.4% reduction at 6 months, 68.3% at 12 months), notable mood improvements (141% EQ-5D increase), enhanced functional status (58% ODI improvement), and remarkable mood state improvements (101% Profile of Mood States [POMS] improvement) over 12 months.107
In another study, the effects of frequency on outcomes were assessed in 20 patients who were titrated to 4 Hz.109 The patient cohort consisted of eight individuals with a history of prior lumbar fusion, two who underwent laminectomy/discectomy, and ten treated for NSLBP. All patients received bilateral T12 leads to address LBP, and a combination of unilateral or bilateral S1 or other lumbar leads was used to address lower extremity pain. The frequency was titrated from an average of 16 Hz to 4 Hz over an average period of 80 days, and outcomes were measured at pre-DRG-S, pre-titration, and post-titration stages. The efficacy of 4 Hz frequency was sustained, as indicated by the maintained improvements from baseline, which included a 77% reduction in VAS score (from 8.8 to 2.0), a 72% improvement in disability, and a remarkable 145% improvement in QOL (EQ-5D 0.33 to 0.81) at 366 days post-implant. Additionally, the cohort showed a continued reduction in opioid consumption from 87 to 43 MME, and a decrease in the number of interventional procedures performed from 0.5 to 0.04 per month during the equivalent pre-DRG-S period. The findings were published alongside a related review of literature article exploring the mechanisms underlying stimulation at 4 Hz.110
In another investigation focusing on the impact of frequency, 20 patients were systematically titrated to 4 Hz. The study found that the effectiveness of DRG-S was sustained at this frequency, with substantial improvements in pain (77% reduction in VAS), disability (72% improvement), mood (145% improvement in EQ-5D), and continued opioid reduction (from 87 to 43 MME) even after 366 days post-implant.109,110 A prospective, double-blinded trial included 20 DRG-S responders who were randomized to three consecutive two-week stimulation programs: continuous stimulation; 1 minute on: 1 minute off; or 1 minute on: 2 minutes off. Mean scores at the end of each program were similar for NRS pain (continuous = 2.9 ± 0.8, 1:1 on-off = 2.6 ± 0.7, and 1:2 on-off = 2.7 ± 0.7 cm, p = 0.39), disability (p = 0.72), and general health (p = 0.95). This suggests that intermittent cycled patterns can achieve comparable effects on pain relief, disability, and functional improvement as standard continuous stimulation.111
Ongoing research and technological advancements are anticipated to further refine this technique and broaden its application in addressing the burden of chronic back pain.1,22,38,40,112–115 Please refer to data in Table 11 and consensus statements in Table 12. Additional evidence is needed to define the role of DRG-S in treating NSLBP in wider clinical settings.
 |
Table 11 Literature Summary for the Efficacy of DRG-S for NSLBP |
 |
Table 12 Consensus Statements on DRG-S in the Treatment of NSLBP |
Diagnostic Work-up for the Implementation of Dorsal Root Ganglion Stimulation for the Treatment of Non-Surgical Low Back Pain
Imaging studies should be reviewed when considering treating a patient with NSLBP with DRG-S. Review spinal imaging such as x-rays, CT scans, and MRIs and treat or refer surgical indications appropriately and assure the absence of severe spinal stenosis.
Foraminal diameter is a concern given the 0.9-mm specifically designed DRG-S lead, although still significantly narrower than the typical 1.3-mm SCS lead,116 still poses the risk of mass effect and foraminal compromise. As such, avoid placing a DRG-S lead at a level with identified severe foraminal stenosis and consider placement at adjacent levels for potential ‘cross coverage’.
Current Evidence for Neuromodulation with Peripheral Nerve Stimulation in Non-Surgical Low Back Pain
Peripheral Nerve Stimulation for Low Back Pain Food and Drug Administration Labeling
There is currently no FDA labeling for peripheral nerve stimulation (PNS) specific to NSLBP. However, with recent advancements in technology and a proven safety profile, PNS is becoming a popular focal point for treatment advancements targeting painful neuralgias.117 For example, a recent systematic literature review by Deer et al on PNS for pain was conducted reviewing 14 RCTs studying PNS for various painful conditions such as headache, shoulder, pelvic, back, extremity, and trunk pain.118 The results demonstrated moderate to strong evidence supporting the use of PNS as an effective treatment for pain. The conclusion suggests that additional prospective trials could help further identify appropriate NSLBP populations and pain diagnoses for PNS treatment.
There are three focal areas specific to LBP which have garnered much attention based on recent evidence pertaining to the effectiveness and sustainability of PNS. These include the superior cluneal nerve,119 middle cluneal nerve,120 and medial branch stimulation for multifidus dysfunction.
For example, a 2023 article by Abd-Elsayed and Moghim reviewed 57 patients retrospectively with chronic pain who underwent PNS targeting various nerves.121 The mean baseline pain scores significantly reduced at different follow-up durations. In the one-month follow-up group, the mean pain score dropped from 7.44 ± 1.48 pre-procedure to 1.6 ± 1.49, and similar reductions were observed at 3, 6, 9, 12, 15, and 24 months (p ≤ 0.001). Additionally, patients reported a significant reduction in MME at 6, 12, and 24 months compared to pre-procedure levels (p ≤ 0.003). Complications occurred in a small number of cases, with 2 patients requiring explant and 1 patient with a lead migration.
Another study aimed to explore the use of percutaneous PNS as an alternative to repeat lumbar radiofrequency ablation and more invasive surgical procedures for chronic back pain.122 In a prospective, multicenter trial, patients who experienced a return of chronic axial pain after radiofrequency ablation received percutaneous PNS leads targeting the medial branch nerves. Stimulation was delivered for up to 60 days, and positive outcomes were observed. The results demonstrated that a majority of participants experienced highly clinically significant reductions in pain intensity (67%) and significant improvements in functional outcomes, such as disability (87%) and pain interference (80%), after two months with PNS. Five months after PNS, 93% of participants reported clinically meaningful improvements in one or more outcome measures, with many experiencing meaningful improvements in all three outcomes (pain intensity, disability, and pain interference). The findings suggest that percutaneous PNS could be an effective, nondestructive, and motor-sparing neuromodulation treatment option for chronic back pain, offering a promising shift in pain management approaches.122
CLBP has traditionally been treated with SCS when other treatments have been tried or when medical indications suggest neuromodulation is the next best approach in the patient treatment algorithm.123,124 However, more recently, there has been special attention to targeting the dorsal ramus at L2 bilaterally to treat CLBP. Both persistent and acute back pain have been evaluated using a 60-day implantation of percutaneous neuromodulation leads at L2.124 In addition, special attention has been paid to the possibility of the treatment, or reversal, of dynamic instability due to multifidus muscle deterioration. The restoration of dynamic stability of the lower back is efficacious by utilizing restorative neuromodulation.125–127
FDA approval has been gained for implantable and temporary PNS systems.128–130
Evidence of Efficacy in Peripheral Nerve Stimulation in Non-Surgical Low Back Pain
As chronic pain continues to increase in global prevalence, the need for evidence-based, efficacious solutions is critical. PNS, a pain treatment that dates back to the first century and the use of electrical discharges from torpedo fish,131,132 has in recent years become an increasingly utilized treatment option due to the minimally invasive nature and limited side effects and complications. The published literature regarding the overall efficacy of PNS depends on the indication for utilization.
In a study of NSLBP patients, Gilmore et al, in a prospective case series involving nine patients, showed a >50% reduction in pain intensity in 67% of patients which after 12 months was reported at a 63% reduction in pain intensity.133
Several studies have analyzed the efficacy and safety of PNS for LBP. D’Souza et al recently performed a systematic review that included twenty-nine articles (828 total participants) focusing on PNS as a primary therapy for LBP.134 All the included articles revealed improvement in LBP after PNS, which was rated between “modest to moderate” improvement as revealed by comparison of baseline pain scores to the individual follow-up periods. There is also emerging evidence of potential effectiveness of PNS in cancer-related pain etiologies presenting as NSLBP.135
Gilligan et al followed 204 patients in a randomized prospective controlled trial that utilized neuromuscular electrical stimulation of the L2 medial branch of spinal nerve dorsal rami and found an average VAS decrease of 3.3 points (7.3 to 4.0).136 In addition, the 3-year and 5-year data has been recently published showing persistent statistically significant making this therapy the most supported treatment for PNS therapy in the field. The 3-year data showed an 83% responder rate. The 5-year data showed 126 patients low back pain VAS had improved from 7.3 to 2.4 cm (−4.9; 95% CI, −5.3 to −4.5 cm; p < 0.0001), with a responder rate of 71.8% defined as a pain reduction greater than 50%. The ODI improved from 39.1 to 16.5 (−22.7; 95% CI, −25.4 to −20.8; p < 0.0001), with 61.1% being reduced ≥20 points. The EQ-5D-5L index significantly improved from 0.585 to 0.807 (0.231; 95% CI, 0.195–0.267; p < 0.0001).137,138
Eldabe et al looked at 116 patients in a separate study that showed peripheral nerve field stimulation (PNFS) in the area of back pain improved pain scores by an average of 47% after 9 months.139 Deer et al and Gilmore et al both lead prospective observational studies evaluating the use of 60-day PNS of the medial branch nerve and found 30% or greater pain relief in most subjects.122,140 Guentchev et al published a prospective observational study that showed average VAS scores improved from 8.8 to 1.6 in 16 patients with permanent PNS placement.141
Current Evidence for Neuromodulation with Peripheral Nerve Stimulation for Pain
Recent advancements in PNS have improved pain relief accessibility. Gilmore et al reported sustained ≥30% pain improvement in 72.97% (54/74) patients at 14 months.140 Deer et al showed ≥30% pain improvement in 86.66% (13/15) of patients at 2 months, with some reduction in efficacy at 5 months.122 Studies on 30-day PNS systems revealed significant pain reduction.124 In neuromuscular stimulation, Gilligan et al conducted an RCT comparing it to sham stimulation, showing no statistical significance in the primary outcome of ≥30% improvement in VAS scores at 120 days.136 However, the therapeutic stimulation group reported an average VAS reduction of 3.3 points, while the sham group also showed a significant average reduction of 2.4 points. For PNS as salvage or adjunctive therapy for LBP intensity, Rigoard et al conducted an RCT that demonstrated a 68.8% decrease in VAS scores at 3 months in the PNFS salvage cohort compared to a 4.0% increase in the SCS-only group.142 Van Gorp et al found a 30.7 point decrease in average VAS scores with PNFS plus SCS at the 3-month follow-up, compared to a 5.6 point average decrease in the SCS-only group.143 When the failed SCS group received PNFS after 3 months, the average VAS scores decreased by another 30.1 points at the 1-year follow-up.
A summary of these finding is presented in Table 13, and an ASPN consensus statement is in Table 14.
 |
Table 13 Literature Summary of Advanced Interventions: PNS |
 |
Table 14 Consensus Statement for PNS in NSLBP Treatment |
Diagnostic Work-up for the Implementation of Peripheral Nerve Stimulation for the Treatment of Non-Surgical Low Back Pain
Numerous PNS techniques have been described for the treatment of CLBP.134 At present, two emerging techniques are at the forefront of PNS for NSLBP.144,145 One is the permanent implantation of a neurostimulator device to target the multifidus muscles. This technique is considered restorative neurostimulation targeting the multifidus muscle by placement of leads at the lumbar medial branches of L2.136,145 The other is a 60-day temporary PNS system targeting the lumbar medial branch nerves. This technique is considered palliative neuromodulation targeting the medial branch nerves corresponding to primary area(s) of pain anywhere from L1-5.122,133 Physician knowledge of diagnostic criteria and use of appropriate imaging/diagnostic modalities is imperative for the use of PNS.
While CLBP is often nonspecific and multifactorial, multifidus muscle dysfunction and inhibition is believed to play a role in its development.136,144,146 Proper diagnosis of multifidus dysfunction prior to utilization of the restorative neurostimulation device is critical. The prone instability test (PIT) is considered the preferred test for evaluation of multifidus dysfunction as a source of CLBP.136,146 The multifidus lift test also serves to identify multifidus dysfunction as a source of CLBP, although it is considered less specific and to have less interrater reliability compared to the PIT.146 Lumbar MRI for the identification of multifidus atrophy and grading (grade 0–2) is also a useful adjunct; however, such findings must always be correlated to patient history and examination, including the aforementioned tests.146
The use of the 60-day temporary PNS system targeting the lumbar medial branch nerve has a broader diagnostic criterion for its use in NSLBP.122,133 In the prospective study by Deer et al, enrolled patients had MRI findings of facet arthrosis, degenerative disc disease, disc protrusion, and/or foraminal narrowing.122
Imaging and Scoliosis in NSLB Pain
For both techniques, lumbar imaging with MRI or CT scan is critical to ensure proper patient selection. Physicians must review this imaging to rule out pathology that may warrant surgical intervention. This imaging should also be utilized to identify any serious underlying cause of LBP (cancer, infection, metabolic bone disorder) or previous lumbar surgery.122,136,144 In cases of spondylolisthesis, lumbar flexion/extension x-rays should be utilized to assess for instability, in which case the patient may benefit from surgery.147 Lumbar x-rays or CT scans should also be utilized to identify conditions such as ankylosing spondylitis and spinal scoliosis. Patients with moderate-to-severe scoliosis (>25 degrees Cobb angle) warrant a surgical consultation.122,136 The use of EMG/NCV prior to PNS for NSLBP is limited, and not considered an integral component of patient selection of PNS.146 Lastly, physicians must always conduct a thorough patient history to rule out significant radicular complaints, as well as assess for timing of previous radiofrequency ablations and injections.122,133,136 Such information is a critical component of patient selection for PNS. Thus, as the role of PNS for NSLBP continues to grow, physician knowledge of device systems, their diagnostic criterion, and the use of appropriate imaging/diagnostic modalities is imperative.
Future Directions and Research
While current evidence has helped establish the use of neuromodulation for NSLBP pain, it is important that our field continues to grow this body of knowledge.1,17,47,99,100,102,107,137 Ongoing research efforts in a myriad of avenues will be critical to this.
First, as interdisciplinary collaboration becomes increasingly more important in our field, an ongoing collaborative effort to refine the definition of the NSLBP is important. As known, a myriad of pathologies can co-exist and culminate in CLBP.19,148–150 Being able to identify pain generators and which types of NSLBP respond to neuromodulation will help guide implementation of the optimal therapy for a given patient with NSLBP.
Level 1 studies are critical to further establish the use of these therapies versus conventional medical management or emerging minimally invasive procedures for NSLBP. This evidence will ultimately help guide clinician decision-making regarding the appropriate type of neuromodulation to utilize for their patients with NSLBP.
Finally, as technology advances, researchers must explore innovative directions to enhance the efficacy, personalization, and overall patient outcomes with neuromodulation. One such technological advancement to consider is the use of AI. AI presents several potential avenues to optimize neuromodulation. Some key applications would be using AI to aid in patient selection and to refine the targeting and programming of neuromodulation. While current systems generally require manual adjustments by clinicians and clinical specialists, AI-assisted algorithms that continuously adjust stimulation parameters based on real-time biofeedback, physiologic data, and patient feedback may help optimize therapy for each unique patient.
Another element to consider would be the use of AI to target neuromodulation based on neural data. While ECAP measurement for closed-loop stimulation is a step in this direction, further capture and utilization of the complex neural activity occurring in the spinal cord and DRG presents a potential leap forward. Future research to develop AI-assisted algorithms to adjust stimulation parameters based on this neural data presents potential means of increasing long-term patient outcomes and satisfaction as well as a reduction in loss of efficacy rates.
In conclusion, the treatment of NSLBP is poised to be transformed with the use of neuromodulation. Further research regarding current techniques will be critical to continue this transformation as will a concerted focus on the potential uses of emerging technology such as AI and closed-loop stimulation.
Psychological Considerations for Neuromodulation in Non-Surgical Low Back Pain
Despite being considered a “standard” aspect of presurgical evaluation prior to SCS and other forms of neuromodulation for back pain, a review of the literature on psychological evaluation yields a complete lack of consensus regarding what elements constitute a sound evaluation, by whom it should be provided, and even its efficacy for improving outcomes.
Results of a literature search published by Fama and colleagues151 demonstrate a complete lack of uniformity of the assessment tools utilized in published studies, with the authors concluding that, “no individual psychological factor in the literature has significantly correlated with outcomes” (p. 431). Although depression has been associated with diminished SCS efficacy in certain studies, these investigations were largely conducted prior to the advent of more sophisticated and effective waveforms,152–155 thus limiting their validity for outcome prediction at present.
A serious concern regarding psychological evaluations as prerequisites for neuromodulation trials and implantations relates to the severe shortage of trained pain psychologists in the US.156–158 Although there are no data on such, given the paucity of qualified pain psychologists in clinical practice, it is evident that only a small percentage of pre-trial or implantation psychological evaluations are being performed by pain psychologists. In an article written over two decades ago, the authors acknowledged that generalist psychologists do not understand the full scope of pain practice.159 There is no evidence that generalist psychologists currently have a better understanding of the scope and nuances of pain management than was the case two decades ago. As a result, we have witnessed these unqualified mental health care providers routinely “over-pathologize” reactively depressed chronic pain patients, thereby disqualifying them from neuromodulation treatments that have the potential to provide them not just with analgesia, but with emotional relief as well.
A review of the extant literature indicates that European studies and guidelines are more likely to identify and recommend psychosocial factors that should be considered relevant for SCS patient selection than is the case in the American literature. In a recent consensus guideline developed in Europe, these factors included lack of engagement, dysfunctional coping, unrealistic expectations, inadequate daily activity level, problematic social support, secondary gain, psychological distress and unwillingness to reduce high-dose opioids.160 Perhaps, the greater availability of pain psychologists to perform pre-trial evaluations in Europe as compared to the US represents a parsimonious explanation for this difference. Although there are no data on the availability of pain psychologists in European nations, a 2016 study by Darnall and colleagues156 indicated that only 11.5% of US psychologists and therapist considered themselves “very competent” in treating patients with chronic pain.
Finally, the possibility that insurance carriers consider delaying coverage for neuromodulation by requiring pre-trial psychological evaluations cannot be ruled out. Anecdotally, this is something of which pain physicians are aware. Given the literature identifying the strong inverse relationship between delayed neuromodulation and favorable long-term outcomes,161 the relationship between insurance insistence on still unproven psychological evaluations prior to neuromodulation trials, the delays in treatment that result from such, and the impact on outcomes certainly merits empirical investigation. ASPN consensus statements are in Table 15.
 |
Table 15 Consensus Statements for Psychological Screen for Neuromodulation in NSLBP Treatment |
Conclusions
The NEURON project is intended to be living guidance with regular updates on the evidence and best practices for topics in spine and nerve. As seen in this publication, the use of neuromodulation for NSLBP is building, and evidence has now led to FDA labeling for forms of SCS. The additional reproduction of these studies and real-world data will lead to more patient access, improved outcomes and safety. It appears that at this time the overall data is developing, and we will see additional modifications in recommended usage and patient selection over time.
Abbreviation
AI, Artificial intelligence; ASPN, American Society of Pain and Neuroscience; BMI, Body mass index; BPI, Brief Pain Inventory; CI, Confidence interval; CLBP, Chronic low back pain; CMM, Conventional medical management; CRPS, Complex regional pain syndrome; CT, Computed tomography; DRG, Dorsal root ganglion; DRG-S, Dorsal root ganglion stimulation; ECAP, Evoked compound action potential; EMG, Electromyography; EQ-5D, EuroQol 5-dimension questionnaire; FBSS, Failed back surgery syndrome; FDA, Food and Drug Administration; GABA, Gamma-aminobutyric acid; IQR, Interquartile range; LBP, Low back pain; MCID, Minimum clinically important difference; MME, Morphine milligram equivalents; MRI, Magnetic resonance imaging; NCV, Nerve conduction velocity; NEURON, Neuroscience, education, utilization, risk mitigation, optimal outcomes, and neuromodulation; NRS, Numeric rating scale; NSAID, Non-steroidal anti-inflammatory drug; NSLBP, Non-surgical low back pain; ODI, Oswestry Disability Index; PCS, Pain Catastrophizing Scale; PGIC, Patient Global Impression of Change; PIT, Prone instability test; PNFS, Peripheral nerve field stimulation; PNS, Peripheral nerve stimulation; POMS, Profile of Mood States; QOL, Quality of life; RCT, Randomized controlled trial; SCS, Spinal cord stimulation; SD, Standard deviation; SF-36, Short Form health questionnaire (36-item); STROBE, Strengthening the Reporting of Observational Studies in Epidemiology; US, United States; USPSTF, United States Preventative Services Task Force; VAS, Visual analog scale.
Acknowledgments
Editing was provided by Allison Foster, PhD, of Foster Medical Communications.
Funding
Development of this guideline was supported by an unrestricted educational grant from Abbott.
Disclosure
TRD is a consultant for Abbott, Vertos, SpineThera, Saluda Medical, Cornerloc, SPR Therapeutics, Boston Scientific, PainTEQ, Spinal Simplicity, and Biotronik; an advisory board member for Abbott, Vertos, SPR Therapeutics, and Biotronik; has a pending patent with Abbott; and has received research funding from Abbott, Vertos, Saluda, Mainstay, SPR Therapeutic, Boston Scientific, and PainTEQ. JEP is a consultant for Abbott, Medtronic, Saluda, Flowonix, SpineThera, PainTEQ, Vertos, Vertiflex, SPR Therapeutics, Tersera, Aurora, Spark, Ethos, Flowonix, Biotronik, Mainstay, WISE, Boston Scientific, Thermaquil, and SpineThera; has received grant/research support from Abbott, Flowonix, Saluda, Aurora, PainTEQ, Ethos, Muse, Boston Scientific, SPR Therapeutics, Mainstay, Vertos, AIS, and Thermaquil; and is a shareholder for Vertos, SPR Therapeutics, PainTEQ, Aurora, Spark, Celeri Health, Neural Integrative Solutions, Pacific Research Institute, Thermaquil, Saluda, Abbott, SpineThera, and Axonics. EAP has received research support from Mainstay, Medtronic, Nalu, Neuros Medical, Nevro Corp, ReNeuron, SPR, and Saluda, as well as personal fees from Abbott Neuromodulation, Biotronik, Medtronic Neuromodulation, Nalu, Neuros Medical, Nevro, Presidio Medical, Saluda, and Vertos; and holds stock options from SynerFuse and neuro42. KA is a consultant for Nevro, Saluda, Biotronik, Boston Scientific, and Presidio. NA is a speaker for PainTEQ, Vivex, Medtronic, Spinal Simplicity, and Vertos; serves on advisory boards for PainTEQ, Vivex, Medtronic, Spinal Simplicity, and Vertos; has received research funding from PainTEQ, Vivex, Medtronic, and Spinal Simplicity; has received grants from PainTEQ, Vivex, and Spinal Simplicity; and holds stock in Spinal Simplicity. KB is a consultant for Abbott and Degen Medical; and serves on advisory boards for XoBiologix and Spinal Simplicity. KBC receives research funding from Abbott. DRD is a consultant for Abbott, Johnson & Johnson, Globus Medical, SI-Bone, and receives royalties from Globus Medical. MJD is a consultant for Globus, Camber, LifeSpine, Vyrsa, PainTEQ, Nevro, Abbott, and Biotronik. AE is a consultant for Medtronic, Nevro, Stryker, and Vertos Medical. SMF is a consultant to Abbott, Medtronic, Saluda, Vertos, CornerLoc, and Mainstay; has equity in Backstop Neural, SurgenTec, SynerFuse, Aurora Spine, Thermaquil, SPR Therapeutics, Saluda, CornerLoc, PainTeq, SpineThera, and Celeri; and has research agreements with Aurora, Mainstay, Medtronic, Abbott, Vertiflex, Saluda, CornerLoc, and Biotronik. RDH is a consultant for Mainstay Medical, Abbott, Saluda, and Biotronik; a speaker for Mainstay Medical and Saluda; and has received research funding from Mainstay Medical, Abbott, Saluda, and Ethos Laboratories. HK is a consultant for Abbott and Nalu, and a speaker for Averitas Pharma. TL is a consultant for Abbott and Alpha Tec, and receives royalties from Alpha Tec. MNM has consulting agreements with Abbott, Nalu Medical, BiotronikNEURO, and SI Bone Inc.; and serves on the scientific advisory board of BiotronikNEURO. SMM is a consultant for Biotronik, Stratus Medical, Curonix, Medtronic, and Boston Scientific. RZM is a consultant for Saluda, Genesys Spine, Vertos, Curonix, Abbott, and PainTEQ. GAM receives research funding from Abbott, Boston Scientific, Nalu, and Mainstay Medical, and is a consultant for Abbott, Boston Scientific, Relievant, and Aurora. SM is a faculty/advisor for Medtronic, Boston Scientific, Nevro and Abbott. YAN is a consultant for Abbott Neuromodulation. RGP is a consultant for Abbott. JGP receives grant support from Medtronic, Boston Scientific, Abbott, Focused Ultrasound Foundation and the NIH (2R01CA166379, R01EB030324, R18EB036591, 5U54EB033650 and U44NS115111), is the medical advisor for Aim Medical Robotics and has stock equity. MES is a Senior Medical Advisor for Apurano Pharma (outside of the scope of this work) and is editor-in-chief of the Journal of Pain Research. PS is a consultant for Saluda. NDT is a consultant for Abbott Medical and SI Bone, and serves on an advisory board for Boston Scientific. JJY is a consultant for Abbott and Saluda. DS is a consultant to Abbott, PainTEQ, Saluda, Mainstay, Surgentec, and Nevro and holds stock options with PainTEQ, Neuralace, Mainstay, and Vertos. The authors report no other conflicts of interest in this work.
References
1. Kapural L, Jameson J, Johnson C. et al. Treatment of nonsurgical refractory back pain with high-frequency spinal cord stimulation at 10 kHz: 12-month results of a pragmatic, multicenter, randomized controlled trial. J Neurosurg Spine. 2022;37(2):188–199. doi:10.3171/2021.12.SPINE211301
2. Patel N, Calodney A, Kapural L, et al. High-Frequency Spinal Cord Stimulation at 10 kHz for the Treatment of Nonsurgical Refractory Back Pain: design of a Pragmatic, Multicenter, Randomized Controlled Trial. Pain Pract. 2021;21(2):171–183. doi:10.1111/papr.12945
3. Stevans JM, Delitto A, Khoja SS, et al. Risk Factors Associated With Transition From Acute to Chronic Low Back Pain in US Patients Seeking Primary Care. JAMA Network Open. 2021;4(2):e2037371. doi:10.1001/jamanetworkopen.2020.37371
4. Chou R, Shekelle P. Will this patient develop persistent disabling low back pain? JAMA. 2010;303(13):1295–1302. doi:10.1001/jama.2010.344
5. Patrick N, Emanski E, Knaub MA. Acute and chronic low back pain. Med Clin North Am. 2014;98(4):777–789. doi:10.1016/j.mcna.2014.03.005.
6. Ge L, Pereira MJ, Yap CW, Heng BH. Chronic low back pain and its impact on physical function, mental health, and health-related quality of life: a cross-sectional study in Singapore. Sci Rep. 2022;12(1):20040. doi:10.1038/s41598-022-24703-7
7. Wong AY, Karppinen J, Samartzis D. Low back pain in older adults: risk factors, management options and future directions. Scoliosis Spinal Disord. 2017;12:14. doi:10.1186/s13013-017-0121-3
8. Baradaran Mahdavi S, Riahi R, Vahdatpour B, Kelishadi R. Association between sedentary behavior and low back pain; A systematic review and meta-analysis. Health Promot Perspect. 2021;11(4):393–410. doi:10.34172/hpp.2021.50
9. Sayed D, Grider J, Strand N, et al. The American Society of Pain and Neuroscience (ASPN) Evidence-Based Clinical Guideline of Interventional Treatments for Low Back Pain. J Pain Res. 2022;15:3729–3832. doi:10.2147/JPR.S386879
10. Deer TR, Grider JS, Pope JE, et al. Best Practices for Minimally Invasive Lumbar Spinal Stenosis Treatment 2.0 (MIST): consensus Guidance from the American Society of Pain and Neuroscience (ASPN). J Pain Res. 2022;15:1325–1354. doi:10.2147/JPR.S355285
11. Farber SH, Han JL, Elsamadicy AA, et al. Long-term Cost Utility of Spinal Cord Stimulation in Patients with Failed Back Surgery Syndrome. Pain Physician. 2017;20(6):E797–E805.
12. McClure JJ, Desai BD, Ampie L, You W, Smith JS, Buchholz AL. A Systematic Review of the Cost-Utility of Spinal Cord Stimulation for Persistent Low Back Pain in Patients With Failed Back Surgery Syndrome. Global Spine J. 2021;11(1_suppl):66S–72S. doi:10.1177/2192568220970163
13. Niyomsri S, Duarte RV, Eldabe S, et al. A Systematic Review of Economic Evaluations Reporting the Cost-Effectiveness of Spinal Cord Stimulation. Value Health. 2020;23(5):656–665. doi:10.1016/j.jval.2020.02.005
14. Spears CA, Hodges SE, Kiyani M, et al. Health Care Resource Utilization and Management of Chronic, Refractory Low Back Pain in the United States. Spine. 2020;45(20):E1333–E1341. doi:10.1097/BRS.0000000000003572
15. Ibrahim T, Tleyjeh IM, Gabbar O. Surgical versus non-surgical treatment of chronic low back pain: a meta-analysis of randomised trials. Int Orthop. 2008;32(1):107–113. doi:10.1007/s00264-006-0269-6
16. Wang X, Wanyan P, Tian JH, Hu L. Meta-analysis of randomized trials comparing fusion surgery to non-surgical treatment for discogenic chronic low back pain. J Back Musculoskelet Rehabil. 2015;28(4):621–627. doi:10.3233/BMR-140571
17. Yue JJ, Gilligan CJ, Falowski S, et al. Surgical treatment of refractory low back pain using implanted BurstDR spinal cord stimulation (SCS) in a cohort of patients without options for corrective surgery: findings and results from the DISTINCT study, a prospective randomized multi-center controlled trial (226). Spine J. 2022;22(9):S120–S121. doi:10.1016/j.spinee.2022.06.246
18. Patel NP, Wu C, Lad SP, et al. Cost-effectiveness of 10-kHz spinal cord stimulation therapy compared with conventional medical management over the first 12 months of therapy for patients with nonsurgical back pain: randomized controlled trial. J Neurosurg Spine. 2023;38(2):249–257. doi:10.3171/2022.9.SPINE22416
19. Rajkumar S, Yang LZ, Venkatraman V, et al. Health Care Resource Utilization of High-Frequency Spinal Cord Stimulation for Treatment of Chronic Refractory Low Back Pain. Neuromodulation. 2023;26(1):115–123. doi:10.1016/j.neurom.2022.03.013
20. Kapural L, Calodney A. Retrospective Efficacy and Cost-Containment Assessment of 10 kHz Spinal Cord Stimulation (SCS) in Non-Surgical Refractory Back Pain Patients. J Pain Res. 2022;15:3589–3595. doi:10.2147/JPR.S373873
21. Goudman L, De Smedt A, Forget P, Eldabe S, Moens M. High-Dose Spinal Cord Stimulation Reduces Long-Term Pain Medication Use in Patients With Failed Back Surgery Syndrome Who Obtained at Least 50% Pain Intensity and Medication Reduction During a Trial Period: a Registry-Based Cohort Study. Neuromodulation. 2021;24(3):520–531. doi:10.1111/ner.13363
22. Al-Kaisy A, Palmisani S, Smith TE, et al. 10 kHz High-Frequency Spinal Cord Stimulation for Chronic Axial Low Back Pain in Patients With No History of Spinal Surgery: a Preliminary, Prospective, Open Label and Proof-of-Concept Study. Neuromodulation. 2017;20(1):63–70. doi:10.1111/ner.12563
23. Bolash R, Creamer M, Rauck R, et al. Wireless High-Frequency Spinal Cord Stimulation (10 kHz) Compared with Multiwaveform Low-Frequency Spinal Cord Stimulation in the Management of Chronic Pain in Failed Back Surgery Syndrome Subjects: preliminary Results of a Multicenter, Prospective Randomized Controlled Study. Pain Med. 2019;20(10):1971–1979. doi:10.1093/pm/pnz019
24. Goudman L, De Smedt A, Eldabe S, et al. High-dose spinal cord stimulation for patients with failed back surgery syndrome: a multicenter effectiveness and prediction study. PAIN. 2021;162(2):582–590. doi:10.1097/j.pain.0000000000002035
25. Hatheway JA, Mangal V, Fishman MA, et al. Long-Term Efficacy of a Novel Spinal Cord Stimulation Clinical Workflow Using Kilohertz Stimulation: twelve-Month Results From the Vectors Study. Neuromodulation. 2021;24(3):556–565. doi:10.1111/ner.13324
26. Baranidharan G, Feltbower R, Bretherton B, et al. One-Year Results of Prospective Research Study Using 10 kHz Spinal Cord Stimulation in Persistent Nonoperated Low Back Pain of Neuropathic Origin: maiden Back Study. Neuromodulation. 2021;24(3):479–487. doi:10.1111/ner.13345
27. Amirdelfan K, Hong M, Tay B, et al. High-Frequency Impulse Therapy for Treatment of Chronic Back Pain: a Multicenter Randomized Controlled Pilot Study. J Pain Res. 2021;14:2991–2999. doi:10.2147/JPR.S325230
28. Al-Kaisy A, Baranidharan G, Sharon H, et al. Comparison of Paresthesia Mapping With Anatomic Placement in Burst Spinal Cord Stimulation: long-Term Results of the Prospective, Multicenter, Randomized, Double-Blind, Crossover CRISP Study. Neuromodulation. 2022;25(1):85–93. doi:10.1111/ner.13467
29. Mons MR, Chapman KB, Terwiel C, Joosten EA, Kallewaard JW. A prospective study of BurstDRTM spinal cord stimulation for non-operated discogenic low back pain. Pain Pract. 2023;23(3):234–241. doi:10.1111/papr.13181
30. Amirdelfan K, Yu C, Doust MW, et al. Long-term quality of life improvement for chronic intractable back and leg pain patients using spinal cord stimulation: 12-month results from the SENZA-RCT. Qual Life Res. 2018;27(8):2035–2044. doi:10.1007/s11136-018-1890-8
31. Mong MSA, Lai MYC, Cheng LJ, Lau Y. Novel Spinal Cord Stimulation Waveforms for Treating Back and Leg Pain: a Systematic Review and Meta-Analysis of Randomized Controlled Trials. Neuromodulation. 2023;26(5):905–916. doi:10.1016/j.neurom.2022.11.003
32. Traeger AC, Gilbert SE, Harris IA, Maher CG. Spinal cord stimulation for low back pain. Cochrane Database Syst Rev. 2023;3(3):CD014789. doi:10.1002/14651858.CD014789.pub2
33. Durbhakula S, Broachwala MY, Schuster NM, McCormick ZL. Striking errors in the methodology, execution, and conclusions of the Cochrane Library review of spinal cord stimulation for low back pain by Traeger et al. Pain Med. 2023;24(8):923–925. doi:10.1093/pm/pnad047
34. NeuroNews International. Cochrane Library urged to retract and revise recent SCS review over “striking errors.” 2023. Available from: https://neuronewsinternational.com/cochrane-library-urged-to-retract-and-revise-recent-scs-review-over-striking-errors/.
35. Darrow JJ, Avorn J, Kesselheim AS. FDA Regulation and Approval of Medical Devices: 1976-2020. JAMA. 2021;326(5):420–432. doi:10.1001/jama.2021.11171
36. Thomson S. Spinal Cord Stimulation’s Role in Managing Chronic Disease Symptoms. International Neuromodulation Society. 2022.
37. North RB, Kidd DH, Farrokhi F, Piantadosi SA. Spinal cord stimulation versus repeated lumbosacral spine surgery for chronic pain: a randomized, controlled trial. Neurosurgery. 2005;56(1):98–106. (). doi:10.1227/01.NEU.0000144839.65524.E0
38. Kumar K, Taylor RS, Jacques L, et al. Spinal cord stimulation versus conventional medical management for neuropathic pain: a multicentre randomised controlled trial in patients with failed back surgery syndrome. Pain. 2007;132(1–2):179–188. doi:10.1016/j.pain.2007.07.028
39. Rigoard P, Desai MJ, North RB, et al. Spinal cord stimulation for predominant low back pain in failed back surgery syndrome: study protocol for an international multicenter randomized controlled trial (PROMISE study). Trials. 2013;14(1):376. doi:10.1186/1745-6215-14-376
40. Kapural L, Yu C, Doust MW, et al. Novel 10-khz high-frequency therapy (HF10 therapy) is superior to traditional low-frequency spinal cord stimulation for the treatment of chronic back and leg pain: the SENZA-RCT randomized controlled trial. Anesthesiology. 2015;123(4):851–860. doi:10.1097/ALN.0000000000000774
41. De Andres J, Monsalve-Dolz V, Fabregat-Cid G, et al. Prospective, Randomized Blind Effect-on-Outcome Study of Conventional vs High-Frequency Spinal Cord Stimulation in Patients with Pain and Disability Due to Failed Back Surgery Syndrome. Pain Med. 2017;18(12):2401–2421. doi:10.1093/pm/pnx241
42. Deer T, Slavin VK, Amirdelfan K, et al. Success Using Neuromodulation With BURST (SUNBURST) Study: results From a Prospective, Randomized Controlled Trial Using a Novel Burst Waveform. Neuromodulation: Technol Neural Interface. 2018;21(1):56–66. doi:10.1111/ner.12698
43. Schu S, Slotty PJ, Bara G, Knop M, Edgar D, Vesper J. A Prospective, Randomised, Double-blind, Placebo-controlled Study to Examine the Effectiveness of Burst Spinal Cord Stimulation Patterns for the Treatment of Failed Back Surgery Syndrome. Neuromodulation. 2014;17(5):443–450. doi:10.1111/ner.12197
44. Petersen EA, Stauss TG, Scowcroft JA, et al. Effect of High-frequency (10-kHz) Spinal Cord Stimulation in Patients With Painful Diabetic Neuropathy: a Randomized Clinical Trial. JAMA Neurol. 2021;78(6):687–698. doi:10.1001/jamaneurol.2021.0538
45. Slangen R, Schaper NC, Faber CG, et al. Spinal cord stimulation and pain relief in painful diabetic peripheral neuropathy: a prospective two-center randomized controlled trial. Dia Care. 2014;37(11):3016–3024. doi:10.2337/dc14-0684
46. de Vos CC, Meier K, Zaalberg PB, et al. Spinal cord stimulation in patients with painful diabetic neuropathy: a multicentre randomized clinical trial. Pain®. 2014;155(11):2426–2431. doi:10.1016/j.pain.2014.08.031
47. Fahey M, Deer T, Gilligan C, et al. ID: 220389 SCS in Patients Without Options for Corrective Surgery; Results From DISTINCT, a Prospective RCT Trial. Neuromodulation. 2023;26(4):S2–S3. doi:10.1016/j.neurom.2023.04.005
48. United States Food and Drug Administration (FDA). Evoke Spinal Cord Stimulation (SCS) System – P190002. 2022. Available from https://www.fda.gov/medical-devices/recently-approved-devices/evoke-spinal-cord-stimulation-scs-system-p190002.
49. United States Food and Drug Administration (FDA). Senza Spinal Cord Stimulation (SCS) System – P
50. United States Food and Drug Administration (FDA). Prodigy, Proclaim, and Proclaim XR Spinal Cord Stimulation (SCS) Systems – P010032/S189. 2022. Available from https://www.fda.gov/medical-devices/recently-approved-devices/prodigy-proclaim-and-proclaim-xr-spinal-cord-stimulation-scs-systems-p010032s189.
51. Sdrulla A, Guan Y, Raja S. Spinal Cord Stimulation: clinical Efficacy and Potential Mechanisms. Pain Pract. 2018;18(8):1048–1067. doi:10.1111/papr.12692
52. Grider JS, Manchikanti L, Carayannopoulos A, et al. Effectiveness of Spinal Cord Stimulation in Chronic Spinal Pain: a Systematic Review. Pain Physician. 2016;19(1):E33–54. doi:10.36076/ppj/2016.19.E33
53. Duarte RV, McNicol E, Colloca L, Taylor RS, North RB, Eldabe S. Randomized Placebo-/Sham-Controlled Trials of Spinal Cord Stimulation: a Systematic Review and Methodological Appraisal. Neuromodulation. 2020;23(1):10–18. doi:10.1111/ner.13018
54. Dauriac-Le Masson V, Gatt MT, Chekroun C, Turak B, Djian MC. Spinal cord stimulation and return to work of patients with failed back surgery syndrome. Pain Pract. 2023;23(5):493–500. doi:10.1111/papr.13205
55. Rojo E, Pérez Hernández C, Sánchez Martínez N, et al. Real-World Cost-Effectiveness Analysis of Spinal Cord Stimulation vs Conventional Therapy in the Management of Failed Back Surgery Syndrome. J Pain Res. 2021;14:3025–3032. doi:10.2147/JPR.S326092
56. Nagel SJ, Lempka SF, Machado AG. Percutaneous spinal cord stimulation for chronic pain: indications and patient selection. Neurosurg Clin N Am. 2014;25(4):723–733. doi:10.1016/j.nec.2014.06.005
57. Patel NP, Jameson J, Johnson C, et al. Durable responses at 24 months with high-frequency spinal cord stimulation for nonsurgical refractory back pain. J Neurosurg Spine. 2023;40(2):229–239. doi:10.3171/2023.9.SPINE23504
58. Deer T, Gilligan C, Falowski S, et al. Treatment of Refractory Low Back Pain Using Passive Recharge Burst in Patients Without Options for Corrective Surgery: findings and Results From the DISTINCT Study, a Prospective Randomized Multicenter Controlled Trial. Neuromodulation. 2023;26(7):1387–1399. doi:10.1016/j.neurom.2023.07.009
59. Kallewaard JW, Billet B, Van Paesschen R, et al. European randomized controlled trial evaluating differential target multiplexed spinal cord stimulation and conventional medical management in subjects with persistent back pain ineligible for spine surgery: 24-month results. Eur J Pain.;28(10):1745–1761. doi:10.1002/ejp.2306.
60. White T, Justiz R, Almonte W, et al. Twelve-month results from a randomized controlled trial comparing differential target multiplexed spinal cord stimulation and conventional spinal cord stimulation in subjects with chronic refractory axial low back pain not eligible for spine surgery. N Am Spine Soc J. 2024;19:100528. doi:10.1016/j.xnsj.2024.100528
61. Al-Kaisy A, Van Buyten JP, Kapural L, et al. 10 kHz spinal cord stimulation for the treatment of non-surgical refractory back pain: subanalysis of pooled data from two prospective studies. Anaesthesia. 2020;75(6):775–784. doi:10.1111/anae.15036
62. Mehta V, Poply K, Ahmad A, et al. Effectiveness of high dose spinal cord stimulation for non-surgical intractable lumbar radiculopathy - HIDENS Study. Pain Pract. 2022;22(2):233–247. doi:10.1111/papr.13087
63. Boston Scientific Corporation. SCS as an Option for Chronic Low Back and/or Leg Pain Instead of Surgery (SOLIS). clinicaltrials.gov; 2024. Available from: https://clinicaltrials.gov/study/NCT04676022.
64. Best BJ, Porwal MH, Pahapill PA. Preoperative Thoracic Spine Magnetic Resonance Imaging for Spinal Cord Stimulation: should Such a Recommendation Be an Absolute Requirement? Neuromodulation. 2022;25(5):758–762. doi:10.1111/ner.13518
65. Hallinan JTPD, Zhu L, Yang K, et al. Deep Learning Model for Automated Detection and Classification of Central Canal, Lateral Recess, and Neural Foraminal Stenosis at Lumbar Spine MRI. Radiology. 2021;300(1):130–138. doi:10.1148/radiol.2021204289
66. Lang G, Vicari M, Siller A, et al. Preoperative Assessment of Neural Elements in Lumbar Spinal Stenosis by Upright Magnetic Resonance Imaging: an Implication for Routine Practice? Cureus. 2018;10(4):e2440. doi:10.7759/cureus.2440
67. Mondelli M, Aretini A, Arrigucci U, Ginanneschi F, Greco G, Sicurelli F. Clinical findings and electrodiagnostic testing in 108 consecutive cases of lumbosacral radiculopathy due to herniated disc. Neurophysiol Clin. 2013;43(4):205–215. doi:10.1016/j.neucli.2013.05.004
68. Johnsson KE, Rosén I, Udén A. Neurophysiologic investigation of patients with spinal stenosis. Spine. 1987;12(5):483–487. doi:10.1097/00007632-198706000-00012
69. Jacobson RE. Lumbar stenosis. An electromyographic evaluation. Clin Orthop Relat Res. 1976;115:68–71.
70. Hirsh LF. Diabetic polyradiculopathy simulating lumbar disc disease. Report of four cases. J Neurosurg. 1984;60(1):183–186. doi:10.3171/jns.1984.60.1.0183
71. Odonkor C, Kwak R, Ting K, Hao D, Collins B, Ahmed S. Fantastic Four: age, Spinal Cord Stimulator Waveform, Pain Localization and History of Spine Surgery Influence the Odds of Successful Spinal Cord Stimulator Trial. Pain Physician. 2020;23(1):E19–E30. doi:10.36076/ppj.2020/23/E19
72. Higashiyama N, Tamura S, Sugawara T. Efficacy of Spinal Cord Stimulation for Failed Back Surgery Syndrome in Elderly Patients: a Retrospective Study. Pain Res Manag. 2023;2023:2136562. doi:10.1155/2023/2136562
73. Sheldon BL, Wilson BR, Miller MS, Zarrin DA, Teton Z, Dorsi MJ. Spinal cord stimulation for the octogenarian: a safe and effective modality for chronic low back and leg pain. Interdisciplinary Neurosurg. 2022;29:101530. doi:10.1016/j.inat.2022.101530
74. Huang KT, Martin J, Marky A, et al. A National Survey of Spinal Cord Stimulation Trial-to-Permanent Conversion Rates. Neuromodulation: Technol Neural Interface. 2015;18(2):133–140. doi:10.1111/ner.12199
75. Chow C, Rosenquist R. Trends in spinal cord stimulation utilization: change, growth and implications for the future. Reg Anesth Pain Med. 2023;48(6):296–301. doi:10.1136/rapm-2023-104346
76. Mekhail N, Costandi S, Saweris Y, Armanyous S, Chauhan G. Impact of biological sex on the outcomes of spinal cord stimulation in patients with chronic pain. Pain Pract. 2022;22(4):432–439. doi:10.1111/papr.13097
77. Manchikanti L, Pampati V, Vangala BP, et al. Spinal Cord Stimulation Trends of Utilization and Expenditures in Fee-For-Service (FFS) Medicare Population from 2009 to 2018. Pain Physician. 2021;24(5):293–308.
78. Elsamadicy AA, Sergesketter A, Ren X, et al. Drivers and Risk Factors of Unplanned 30-Day Readmission Following Spinal Cord Stimulator Implantation. Neuromodulation. 2018;21(1):87–92. doi:10.1111/ner.12689
79. Mekhail N, Mehanny D, Armanyous S, Saweris Y, Costandi S. The impact of obesity on the effectiveness of spinal cord stimulation in chronic spine-related pain patients. Spine J. 2019;19(3):476–486. doi:10.1016/j.spinee.2018.08.006
80. Sommer TW, Ivankovic S, McCall TD. Effect of Body Mass Index on Paddle Lead Spinal Cord Stimulator Safety Implantation for Chronic Pain Management. World Neurosurg. 2023;170:e712–e715. doi:10.1016/j.wneu.2022.11.101
81. Segal R. Spinal Cord Stimulation, Conception, Pregnancy, and Labor: case Study in a Complex Regional Pain Syndrome Patient. Neuromodulation. 1999;2(1):41–45. doi:10.1046/j.1525-1403.1999.00041.x
82. Hanson JL, Goodman EJ. Labor epidural placement in a woman with a cervical spinal cord stimulator. Int J Obstet Anesth. 2006;15(3):246–249. doi:10.1016/j.ijoa.2005.08.007
83. Saxena A, Eljamel MS. Spinal cord stimulation in the first two trimesters of pregnancy: case report and review of the literature. Neuromodulation. 2009;12(4):281–283. doi:10.1111/j.1525-1403.2009.00240.x
84. Bernardini DJ, Pratt SD, Takoudes TC, Simopoulos TT. Spinal cord stimulation and the pregnant patient-specific considerations for management: a case series and review of the literature. Neuromodulation. 2010;13(4):270–274. doi:10.1111/j.1525-1403.2010.00288.x
85. Sommerfield D, Hu P, O’Keeffe D, McKeating AK. Caesarean section in a parturient with a spinal cord stimulator. Int J Obstet Anesth. 2010;19(1):114–117. doi:10.1016/j.ijoa.2009.08.006
86. Gredilla E, Abejón D, Del Pozo C, Del Saz J, Gilsanz F. Failed back surgery, spinal cord stimulation and pregnancy: presentation of a case. Rev Esp Anestesiol Reanim. 2012;59(9):511–514. doi:10.1016/j.redar.2012.04.019
87. Das B, McCrory C. Spinal cord stimulation in pregnancy with failed back surgery syndrome. Ir Med J. 2014;107(4):117–118.
88. Edelbroek C, Terheggen M. High-Frequency Spinal Cord Stimulation and Pregnancy: a Case Report. Neuromodulation. 2015;18(8):757–758. doi:10.1111/ner.12314
89. Young AC, Lubenow TR, Buvanendran A. The parturient with implanted spinal cord stimulator: management and review of the literature. Reg Anesth Pain Med. 2015;40(3):276–283. doi:10.1097/AAP.0000000000000242
90. Ahmed S, Lindsay JM, Snyder DI. Spinal Cord Stimulation for Complex Regional Pain Syndrome: a Case Study of a Pregnant Female. Pain Physician. 2016;19(3):E487–493. doi:10.36076/ppj/2019.19.E487
91. Aquino M, Rosner G. Systemic Contact Dermatitis. Clin Rev Allergy Immunol. 2019;56(1):9–18. doi:10.1007/s12016-018-8686-z
92. Cameron T. Safety and efficacy of spinal cord stimulation for the treatment of chronic pain: a 20-year literature review. J Neurosurg. 2004;100(3 Suppl Spine):254–267. doi:10.3171/spi.2004.100.3.0254
93. Falowski SM, Provenzano DA, Xia Y, Doth AH. Spinal Cord Stimulation Infection Rate and Risk Factors: results From a United States Payer Database. Neuromodulation Technol Neural Interface. 2019;22(2):279–289. doi:10.1111/ner.12843
94. Duarte RM, Vaccaro AR. Spinal infection: state of the art and management algorithm. Eur Spine J. 2013;22(12):2787–2799. doi:10.1007/s00586-013-2850-1
95. De Ridder D, Plazier M, Kamerling N, Menovsky T, Vanneste S. Burst spinal cord stimulation for limb and back pain. World Neurosurg. 2013;80(5):642–649. doi:10.1016/j.wneu.2013.01.040
96. De Ridder D, Vanneste S, Plazier M, van der Loo E, Menovsky T. Burst Spinal Cord Stimulation. Neurosurgery. 2010;66(5):986–990. doi:10.1227/01.NEU.0000368153.44883.B3
97. Tiede J, Brown L, Gekht G, Vallejo R, Yearwood T, Morgan D. Novel spinal cord stimulation parameters in patients with predominant back pain. Neuromodulation. 2013;16(4):370–375. doi:10.1111/ner.12032
98. Russo M, Van Buyten J. 10-kHz High-Frequency SCS Therapy: a Clinical Summary. Pain Med. 2015;16(5):934–942. doi:10.1111/pme.12617
99. Mekhail N, Levy RM, Deer TR, et al. Long-term safety and efficacy of closed-loop spinal cord stimulation to treat chronic back and leg pain (Evoke): a double-blind, randomised, controlled trial. Lancet Neurol. 2020;19(2):123–134. doi:10.1016/S1474-4422(19)30414-4
100. Mekhail N, Levy RM, Deer TR, et al. Durability of Clinical and Quality-of-Life Outcomes of Closed-Loop Spinal Cord Stimulation for Chronic Back and Leg Pain: a Secondary Analysis of the Evoke Randomized Clinical Trial. JAMA Neurol. 2022;79(3):251–260. doi:10.1001/jamaneurol.2021.4998
101. Fishman M, Cordner H, Justiz R, et al. Twelve-Month results from multicenter, open-label, randomized controlled clinical trial comparing differential target multiplexed spinal cord stimulation and traditional spinal cord stimulation in subjects with chronic intractable back pain and leg pain. Pain Pract. 2021;21(8):912–923. doi:10.1111/papr.13066
102. Chapman KB, Groenen PS, Patel VK, Vissers KC, van Helmond N. T12 Dorsal Root Ganglion Stimulation to Treat Chronic Low Back Pain: a Case Series. Neuromodulation: Technol Neural Interface. 2020;23(2):203–212. doi:10.1111/ner.13047
103. Kaiser JT, Lugo-Pico JG. Neuroanatomy, Spinal Nerves. StatPearls. StatPearls Publishing; 2023. Available from. http://www.ncbi.nlm.nih.gov/books/NBK542218/.
104. Chapman KB, Groenen PS, Vissers KC, van Helmond N, Stanton‐Hicks MD. The Pathways and Processes Underlying Spinal Transmission of Low Back Pain: observations From Dorsal Root Ganglion Stimulation Treatment. Neuromodulation. 2021;24(4):610–621. doi:10.1111/ner.13150
105. Chapman KB, van Roosendaal BK, Yousef TA, Vissers KC, Hel V. Dorsal Root Ganglion Stimulation Normalizes Measures of Pain Processing in Patients with Chronic Low Back Pain: a Prospective Pilot Study using Quantitative Sensory Testing. Pain Pract. 2021;21(5):568–577. doi:10.1111/papr.12992
106. Chapman KB, Tupper C, Vissers KC, van Helmond N, Yousef T. Dorsal root ganglion stimulation for the treatment of joint pain with predominantly nociceptive characteristics: a case series. Pain Pract. 2023;23(3):317–324. doi:10.1111/papr.13180
107. Kallewaard JW, Edelbroek C, Terheggen M, Raza A, Geurts JW. A Prospective Study of Dorsal Root Ganglion Stimulation for Non-Operated Discogenic Low Back Pain. Neuromodulation. 2020;23(2):196–202. doi:10.1111/ner.12937
108. Huygen F, Liem L, Cusack W, Kramer J. Stimulation of the L2-L3 Dorsal Root Ganglia Induces Effective Pain Relief in the Low Back. Pain Pract. 2018;18(2):205–213. doi:10.1111/papr.12591
109. Chapman KB, Yousef TA, Vissers KC, van Helmond N, Stanton-Hicks DM. Very Low Frequencies Maintain Pain Relief From Dorsal Root Ganglion Stimulation: an Evaluation of Dorsal Root Ganglion Neurostimulation Frequency Tapering. Neuromodulation. 2021;24(4):746–752. doi:10.1111/ner.13322
110. Chapman KB, Yousef TA, Foster A, Stanton‐Hicks D, van Helmond MN. Mechanisms for the Clinical Utility of Low‐Frequency Stimulation in Neuromodulation of the Dorsal Root Ganglion. Neuromodulation. 2021;24(4):738–745. doi:10.1111/ner.13323
111. Chapman KB, Tupper C, Yang AH, van Helmond N, Yousef T. Intermittent Dorsal Root Ganglion Stimulation is as Efficacious as Standard Continuous Dosing in Treating Chronic Pain: results from a Randomized Controlled Feasibility Trial. Neuromodulation. 2022;25(7):989–997. doi:10.1016/j.neurom.2021.10.008
112. Al-Kaisy A, Palmisani S, Smith TE, et al. Long-Term Improvements in Chronic Axial Low Back Pain Patients Without Previous Spinal Surgery: a Cohort Analysis of 10-kHz High-Frequency Spinal Cord Stimulation over 36 Months. Pain Med. 2018;19(6):1219–1226. doi:10.1093/pm/pnx237
113. Van Buyten V, Al-Kaisy A, Smet I, Palmisani S, Smith T. High-frequency spinal cord stimulation for the treatment of chronic back pain patients: results of a prospective multicenter European clinical study. Neuromodulation. 2013;16(1):59–66. doi:10.1111/ner.12006
114. Van Buyten JP, Wille F, Smet I, et al. Therapy-Related Explants After Spinal Cord Stimulation: results of an International Retrospective Chart Review Study. Neuromodulation. 2017;20(7):642–649. doi:10.1111/ner.12642
115. Taylor RS, Desai MJ, Rigoard P, Taylor RJ. Predictors of pain relief following spinal cord stimulation in chronic back and leg pain and failed back surgery syndrome: a systematic review and meta-regression analysis. Pain Pract. 2014;14(6):489–505. doi:10.1111/papr.12095
116. Torun F, Dolgun H, Tuna H, Attar A, Uz A, Erdem A. Morphometric analysis of the roots and neural foramina of the lumbar vertebrae. Surg Neurol. 2006;66(2):148–151. doi:10.1016/j.surneu.2006.02.041
117. Stanton-Hicks M, Panourias IG, Sakas DE, Slavin KV. The future of peripheral nerve stimulation. Prog Neurol Surg. 2011;24:210–217. doi:10.1159/000324298
118. Chauhan G, Levy I, DeChellis D. Superior Cluneal Neuralgia Treated With Wireless Peripheral Nerve Stimulation. Cureus. 2022;14(3):e23711. doi:10.7759/cureus.23711
119. Deer TR, Esposito MF, McRoberts WP, et al. A Systematic Literature Review of Peripheral Nerve Stimulation Therapies for the Treatment of Pain. Pain Med. 2020;21(8):1590–1603. doi:10.1093/pm/pnaa030
120. Karl HW, Helm S, Trescot AM. Superior and Middle Cluneal Nerve Entrapment: a Cause of Low Back and Radicular Pain. Pain Physician. 2022;25(4):E503–E521.
121. Abd-Elsayed A, Moghim R. Efficacy of Peripheral Nerve Stimulation with a High Frequency Electromagnetic Coupled (HF-EMC) Powered Implanted Receiver in Treating Different Pain Targets/Neuralgias. J Pain Res. 2023;16:589–596. doi:10.2147/JPR.S399532
122. Deer TR, Gilmore CA, Desai MJ, et al. Percutaneous Peripheral Nerve Stimulation of the Medial Branch Nerves for the Treatment of Chronic Axial Back Pain in Patients After Radiofrequency Ablation. Pain Med. 2021;22(3):548–560. doi:10.1093/pm/pnaa432
123. Gilmore CA, Kapural L, McGee MJ, Boggs JW. Percutaneous Peripheral Nerve Stimulation (PNS) for the Treatment of Chronic Low Back Pain Provides Sustained Relief. Neuromodulation: Technol Neural Interface. 2019;22(5):615–620. doi:10.1111/ner.12854
124. Kapural L, Gilmore CA, Chae J, et al. Percutaneous Peripheral Nerve Stimulation for the Treatment of Chronic Low Back Pain: two Clinical Case Reports of Sustained Pain Relief. Pain Pract. 2018;18(1):94–103. doi:10.1111/papr.12571
125. Deckers K, De Smedt K, van Buyten JP, et al. Chronic Low Back Pain: restoration of Dynamic Stability. Neuromodulation. 2015;18(6):478–486. doi:10.1111/ner.12275
126. Mitchell B, Deckers K, DeSmedt K, et al. Targeting the cause, not just the symptoms: a new treatment for chronic low back pain – results of the ReActiv8-A trial. J Sci Med Sport. 2017:
127. Thomson S, Chawla R, Love-Jones S, et al. Restorative Neurostimulation for Chronic Mechanical Low Back Pain: results from a Prospective Multi-centre Longitudinal Cohort. Pain Ther. 2021;10(2):1451–1465. doi:10.1007/s40122-021-00307-3
128. US Food and Drug Administration (FDA). 510(k) Premarket Notification: SPRINT Peripheral Nerve Stimulation System. Available from: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm?ID=k181422.
129. US Food and Drug Administration (FDA). 510(k) Premarket Notification: nalu Neurostimulation Kit. Available from: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm?ID=K202274.
130. US Food and Drug Administration (FDA). 510(k) Premarket Notification. Freedom Peripheral Nerve Stimulator (PNS) System. Available from: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMN/pmn.cfm?ID=K233162.
131. Gildenberg PL. History of Electrical Neuromodulation for Chronic Pain. Pain Med. 2006;7(s1):S7–S13. doi:10.1111/j.1526-4637.2006.00118.x
132. Tsoucalas G, Karamanou M, Lymperi M, Gennimata V, Androutsos G. The “torpedo” effect in medicine. Int Marit Health. 2014;65(2):65–67. doi:10.5603/IMH.2014.0015
133. Gilmore CA, Kapural L, McGee MJ, Boggs JW. Percutaneous Peripheral Nerve Stimulation for Chronic Low Back Pain: prospective Case Series With 1 Year of Sustained Relief Following Short-Term Implant. Pain Pract. 2020;20(3):310–320. doi:10.1111/papr.12856
134. D’Souza RS, Jin MY, Abd-Elsayed A. Peripheral Nerve Stimulation for Low Back Pain: a Systematic Review. Curr Pain Headache Rep. 2023;27(5):117–128. doi:10.1007/s11916-023-01109-2
135. Mach S, Javed S, Chen GH, Huh BK. Peripheral Nerve Stimulation for Back Pain in Patients With Multiple Myeloma as Bridge Therapy to Radiation Treatment: a Case Series. Neuromodulation. 2023;26(3):694–699. doi:10.1016/j.neurom.2023.01.018
136. Gilligan C, Volschenk W, Russo M, et al. An implantable restorative-neurostimulator for refractory mechanical chronic low back pain: a randomized sham-controlled clinical trial. Pain. 2021;162(10):2486–2498. doi:10.1097/j.pain.0000000000002258
137. Gilligan C, Volschenk W, Russo M, et al. Three-Year Durability of Restorative Neurostimulation Effectiveness in Patients With Chronic Low Back Pain and Multifidus Muscle Dysfunction. Neuromodulation. 2023;26(1):98–108. doi:10.1016/j.neurom.2022.08.457
138. Gilligan C, Volschenk W, Russo M, et al. Five-Year Longitudinal Follow-up of Restorative Neurostimulation Shows Durability of Effectiveness in Patients With Refractory Chronic Low Back Pain Associated With Multifidus Muscle Dysfunction. Neuromodulation. 2024:S1094–7159(24)00055–2. doi:10.1016/j.neurom.2024.01.006
139. Eldabe SS, Taylor RS, Goossens S, et al. A Randomized Controlled Trial of Subcutaneous Nerve Stimulation for Back Pain Due to Failed Back Surgery Syndrome: the SubQStim Study. Neuromodulation. 2019;22(5):519–528. doi:10.1111/ner.12784
140. Gilmore CA, Desai MJ, Hopkins TJ, et al. Treatment of chronic axial back pain with 60‐day percutaneous medial branch PNS: primary end point results from a prospective, multicenter study. Pain Pract. 2021;21(8):877–889. doi:10.1111/papr.13055
141. Guentchev M, Preuss C, Rink R, Peter L, Sailer MHM, Tuettenberg J. Long-Term Reduction of Sacroiliac Joint Pain With Peripheral Nerve Stimulation. Oper Neurosurg (Hagerstown). 2017;13(5):634–639. doi:10.1093/ons/opx017
142. Rigoard P, Ounajim A, Goudman L, et al. The Added Value of Subcutaneous Peripheral Nerve Field Stimulation Combined with SCS, as Salvage Therapy, for Refractory Low Back Pain Component in Persistent Spinal Pain Syndrome Implanted Patients: a Randomized Controlled Study (CUMPNS Study) Based on 3D-Mapping Composite Pain Assessment. J Clin Med. 2021;10(21):5094. doi:10.3390/jcm10215094
143. van Gorp EJJAA, Teernstra O, Aukes HJ, et al. Long-Term Effect of Peripheral Nerve Field Stimulation as Add-On Therapy to Spinal Cord Stimulation to Treat Low Back Pain in Failed Back Surgery Syndrome Patients: a 12-Month Follow-Up of a Randomized Controlled Study. Neuromodulation. 2019;22(8):970–977. doi:10.1111/ner.12776
144. Gilmore CA, Patel J, Esebua LG, Burchell M. A Review of Peripheral Nerve Stimulation Techniques Targeting the Medial Branches of the Lumbar Dorsal Rami in the Treatment of Chronic Low Back Pain. Pain Med. 2020;21(Suppl 1):S41–S46. doi:10.1093/pm/pnaa084
145. Tieppo Francio V, Westerhaus BD, Rupp A, Sayed D. Non-Spinal Neuromodulation of the Lumbar Medial Branch Nerve for Chronic Axial Low Back Pain: a Narrative Review. Front Pain Res. 2022;3:835519. doi:10.3389/fpain.2022.835519
146. Chakravarthy K, Lee D, Tram J, et al. Restorative Neurostimulation: a Clinical Guide for Therapy Adoption. J Pain Res. 2022;15:1759–1774. doi:10.2147/JPR.S364081
147. Abdu WA, Sacks OA, Tosteson ANA, et al. Long-Term Results of Surgery Compared With Nonoperative Treatment for Lumbar Degenerative Spondylolisthesis in the Spine Patient Outcomes Research Trial (SPORT). Spine. 2018;43(23):1619–1630. doi:10.1097/BRS.0000000000002682
148. Freburger JK, Holmes GM, Agans RP, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169(3):251–258. doi:10.1001/archinternmed.2008.543
149. Shmagel A, Foley R, Ibrahim H. Epidemiology of Chronic Low Back Pain in US Adults: data From the 2009-2010 National Health and Nutrition Examination Survey. Arthritis Care Res (Hoboken). 2016;68(11):1688–1694. doi:10.1002/acr.22890
150. Fatoye F, Gebrye T, Ryan CG, Useh U, Mbada C. Global and regional estimates of clinical and economic burden of low back pain in high-income countries: a systematic review and meta-analysis. Front Public Health. 2023;11:1098100. doi:10.3389/fpubh.2023.1098100
151. Fama CA, Chen N, Prusik J, et al. The Use of Preoperative Psychological Evaluations to Predict Spinal Cord Stimulation Success: our Experience and a Review of the Literature. Neuromodulation. 2016;19(4):429–436. doi:10.1111/ner.12434
152. Burchiel KJ, Anderson VC, Wilson BJ, Denison DB, Olson KA, Shatin D. Prognostic factors of spinal cord stimulation for chronic back and leg pain. Neurosurgery. 1995;36(6):1101–1110. (). doi:10.1227/00006123-199506000-00006
153. North RB, Kidd DH, Wimberly RL, Edwin D. Prognostic value of psychological testing in patients undergoing spinal cord stimulation: a prospective study. Neurosurgery. 1996;39(2):301–310. doi:10.1097/00006123-199608000-00013.
154. Olson KA, Bedder MD, Anderson VC, Burchiel KJ, Villanueva MR. Psychological variables associated with outcome of spinal cord stimulation trials. Neuromodulation. 1998;1(1):6–13. doi:10.1111/j.1525-1403.1998.tb00025.x
155. Ruchinskas R, O’Grady T. Psychological variables predict decisions regarding implantation of a spinal cord stimulator. Neuromodulation. 2000;3(4):183–189. doi:10.1046/j.1525-1403.2000.00183.x
156. Darnall BD, Scheman J, Davin S, et al. Pain Psychology: a Global Needs Assessment and National Call to Action. Pain Med. 2016;17(2):250–263. doi:10.1093/pm/pnv095
157. Darnall BD, Carr DB, Schatman ME. Pain Psychology and the Biopsychosocial Model of Pain Treatment: ethical Imperatives and Social Responsibility. Pain Med. 2017;18(8):1413–1415. doi:10.1093/pm/pnw166
158. Schatman M, Fortino M. The Problem (and the Answer?) to the Limited Availability of Pain Psychologists: can Clinical Social Workers Help? J Pain Res. 2020;Volume 13:3525–3529. doi:10.2147/JPR.S297312
159. Simon EP, Folen RA. The role of the psychologist on the multidisciplinary pain management team. Prof Psychol. 2001;32(2):125–134. doi:10.1037/0735-7028.32.2.125
160. Thomson S, Huygen F, Prangnell S, et al. Appropriate referral and selection of patients with chronic pain for spinal cord stimulation: European consensus recommendations and e-health tool. Eur J Pain. 2020;24(6):1169–1181. doi:10.1002/ejp.1562
161. Kumar K, Hunter G, Demeria D. Spinal cord stimulation in treatment of chronic benign pain: challenges in treatment planning and present status, a 22-year experience. Neurosurgery. 2006;58(3):481–496. doi:10.1227/01.NEU.0000192162.99567.96.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

