Back to Journals » Drug Design, Development and Therapy » Volume 19
An Open-Label, Single and Multiple Dose Study to Evaluate the Pharmacokinetics and Safety of Fezolinetant in Healthy Chinese Female Subjects
Authors Li Y, Liu Y, Iwai M, Takeuchi M, Song N, Li Y, Shi A
Received 23 September 2024
Accepted for publication 28 February 2025
Published 26 March 2025 Volume 2025:19 Pages 2243—2252
DOI https://doi.org/10.2147/DDDT.S486562
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Manfred Ogris
Yang Li,1 Yue Liu,1 Megumi Iwai,2,3 Masato Takeuchi,3 Nan Song,4 Yuan Li,4 Aixin Shi1
1Clinical Trial Center, Beijing Hospital, National Center of Gerontology; Institute of Geriatric Medicine, Chinese Academy of Medical Sciences, Beijing, People’s Republic of China; 2Astellas Pharma Global Development, Inc, Northbrook, IL, USA; 3Astellas Pharma Inc, Tokyo, Japan; 4Astellas (China) Investment Co, Ltd, Beijing, People’s Republic of China
Correspondence: Aixin Shi, Clinical Trial Center, Beijing Hospital, National Center of Gerontology; Institute of Geriatric Medicine, Chinese Academy of Medical Sciences, Beijing, 100730, People’s Republic of China, Email [email protected]
Purpose: To evaluate pharmacokinetics (PK) and safety of fezolinetant after single-dose and multiple-dose administration of 15, 30, and 60 mg in healthy Chinese women.
Patients and Methods: This was a fixed-sequence crossover study in 16 healthy Chinese female subjects, 18– 45 years old. All received single doses of fezolinetant 15 mg, 30 mg or 60 mg with a 3-day washout. From Day 10, subjects received multiple doses of 30 mg fezolinetant once-daily for 7 days. PK parameters were obtained during the single- and multiple-dose periods. Safety assessments were based on adverse events, vital signs, and laboratory tests.
Results: Fezolinetant exhibited rapid absorption, with median time of the maximum concentration (tmax) 1.50 to 1.75 hours after single-dose administration of fezolinetant tablets in the fasted state, followed by a decline in plasma levels, with a mean t1/2 of 6.12– 7.69 hours at dose levels of 15, 30 and 60 mg. There was a dose-proportional increase in maximum concentration and total exposure for fezolinetant across the doses studied. Mean peak concentration (Cmax) values were 221, 439 and 834 ng/mL, for the 15, 30, and 60 mg doses, respectively. The drug exposure parameters had a low-to-moderate variability (21.1– 39.7%). Minimum accumulation was observed after multiple doses. Metabolite ES259564 showed rapid formation following a single dose of fezolinetant, with a median tmax of 1.50– 2.00 hours. Plasma levels then declined, with mean t1/2 ranging from 5.72– 6.31 hours. Dose-proportional increases in Cmax and AUCinf were observed following single-doses of fezolinetant. Steady state was achieved on the second day after starting multiple-dose administration. In total, 3 (18.8%) subjects experienced 4 drug-related treatment-emergent adverse events; all mild in severity.
Conclusion: Linear PK was confirmed within the dose range of 15 to 60 mg in healthy Chinese women.
Keywords: vasomotor symptoms, menopause, nonhormonal, neurokinin receptor
Introduction
Vasomotor symptoms (VMS), also known as hot flashes and night sweats, are a major reason for menopausal women to seek medical attention and have been associated with reduced quality of life via affects on mood, sleep, and cognitive functioning and by contributing to anxiety, fatigue, and work-related difficulties.1–6 VMS are caused by disproportionate activity of neurons in the hypothalamic thermoregulatory center.7 The median duration of VMS is 7.4 years,8 however, moderate-to-severe symptoms may continue for more than 10 years in one-third of women.9 In the Study of Women’s Health Across the Nation (SWAN), up to 80% of Chinese women experienced VMS.10
The commonly used effective treatment for VMS is hormone therapy (HT),11–13 but this may not be appropriate for everyone, depending on risk factors, concomitant medical conditions, time since menopause, and age.11 Further, some women make a conscious choice not to take HT. Nonhormonal treatments available to manage menopause-associated symptoms include selective serotonin reuptake inhibitors, serotonin noradrenaline reuptake inhibitors, gabapentin, herbal remedies, and cognitive behavioral therapy. However, they may be associated with adverse effects such as sedation and nausea, and their clinical effectiveness is limited.14 Perceived HT limitations, together with the adverse effects and limited efficacy seen with nonhormonal therapies, have prompted the search for other treatment options. A growing body of evidence has implicated neurokinin B (NKB)/neurokinin 3 receptor (NK3R) signaling in menopausal VMS etiology.15
Fezolinetant is an oral, nonhormonal, NK3R antagonist treatment option for moderate-to-severe VMS, and is approved in many countries, including the US, in Europe and in Asia at a dose of 45 mg once daily.16–21
It moderates neuronal activity in the thermoregulatory center by blocking NKB binding on the kisspeptin/neurokinin B/dynorphin neurons in the hypothalamus.15,22–24
Fezolinetant is well absorbed and extensively metabolized, primarily to the oxidated metabolite ES259564. In clinical studies conducted in the USA and Europe, the observed overall exposure (AUC) and maximum concentration (Cmax) increased dose proportionally when once-daily doses ranging from 20 to 60 mg were administered, which covered the recommended therapeutic dose.18 While mean Cmax was lower and median tmax was delayed about 30 min compared with under fasted conditions, food does not affect fezolinetant AUC, and it can therefore be taken without regard to meals.18
As part of the fezolinetant clinical development program in Asia, the MOONLIGHT 1 pivotal Phase 3, double-blind study compared fezolinetant 30 mg once-daily dose over 12 weeks versus placebo, followed by an open-label extension phase with fezolinetant 30 mg/day for 12 weeks in an East Asian population.25 MOONLIGHT 3 was a phase 3, open-label, long-term safety study investigating 52 weeks of treatment with once-daily fezolinetant 30 mg in women in mainland China, and found that fezolinetant at a dose of 30 mg was generally safe and well tolerated in this population.26 To support the development of fezolinetant in China, an open-label study was conducted to evaluate the pharmacokinetics (PK) and safety of fezolinetant after single-dose and multiple-dose administration of 15, 30, and 60 mg, in healthy Chinese women. The study was designed to cover the expected therapeutic dose.
Materials and Methods
The study was conducted in compliance with ethical principles originating from the Declaration of Helsinki, Good Clinical Practice (GCP), International Council for Harmonization (ICH) guidelines, Council for Organizations of Medical Sciences (CIOMS) International Ethical Guidelines and applicable laws and regulations. An independent ethics committee approved the study (the Institutional Review Board of Beijing Hospital), and prior to initiation of any study-related procedures, all subjects provided written informed consent.
Study Design
The study was conducted from March to May 2021 in China and registered at ClinicalTrials.gov (NCT04793204). Subjects enrolled in the study were healthy Chinese women with BMI (range, >19 kg/m2 to ≤24.9 kg/m2) and weight (≥45.0 kg), aged between 18 and 45 years. Women who had been pregnant in the past 6 months or breastfed in the past 3 months were excluded from participation. Figure 1 shows the study design. The number of subjects was based on the National Medical Products Administration (NMPA)’s guideline for Pharmacokinetic Study, which recommends 8 to 12 subjects per dose group.
Subjects were screened for eligibility during the 21-day period prior to study enrollment, and subsequently admitted to the clinical unit the day prior to administration (Day −1). Study participants then stayed in the clinical unit up until 48 hours after last dose administration (Day 18). The single-dose period constituted Days 1 to 7. At the start of the investigational period (Day 1), subjects were given a single dose of 15 mg fezolinetant. After a 3-day washout period, subjects were given a single dose of 30 mg fezolinetant (Day 4) followed by another 3-day washout period. On Day 7, subjects were given a single dose of 60 mg fezolinetant. Blood sampling for PK analyses for fezolinetant and its major metabolite, ES259564, was performed pre-dose, and at 0.5, 1, 1.5, 2, 3, 4, 6, 8, 12, 24 and 48 hours after administration of each dose during this single-dose period (Days 1, 4 and 7). Starting on Day 10, subjects received multiple doses of 30 mg fezolinetant once-daily for 7 consecutive days. Blood samples were collected pre-dose on Days 10, 11, 12, 13, 14 and 15. On Day 16, subjects received the final dose of fezolinetant while fasting and blood samples were collected pre-dose, and at 0.5, 1, 1.5, 2, 3, 4, 6, 8.12, 24 and 48 hours post-dose. Fezolinetant administration on Days 1, 4, 7 and 16 took place in the morning after an approximate 10-hour fast and approximately 4 hours before the following meal. Dose administration on Days 10 through 15 took place after breakfast. Each dose administration was given with 150 mL of water. The end-of-study visit was 19 to 23 days after the last PK sample was collected or at the time the subject withdrew (ie, early discontinuation from the clinical study).
Bioanalytical Analysis
Blood samples for analysis were collected in tubes containing lithium heparin. Plasma was separated and shipped to Wuxi AppTec Co., Ltd. (Shanghai, China), where concentrations of fezolinetant and ES259564, the major metabolite of fezolinetant, were measured using liquid chromatography-tandem mass spectrometry (LC-MS/MS); a method that was validated. In brief, solid-phase extraction was used to extract fezolinetant, ES259564 and the internal standard from 50 µL of plasma, and separation was by reversed-phase liquid chromatography on a Phenomenex Kinetex C18 column. This used a gradient mobile phase consisting of methanol/acetonitrile/water/formic acid. Detection was via an API 6500 (AB/MDS Sciex, Nieuwerkerk a/d Ijssel, The Netherlands) using positive atmospheric pressure chemical ionization. Validation of the method for both fezolinetant and ES259564 was over a range of 1 to 1000 ng/mL, and inter-run accuracy and precision were within acceptance criteria.
Study Endpoints
PK Assessments
Phoenix WinNonlin software (version 8.0, Certara L.P., Princeton, NJ, USA) was used to calculate descriptive pharmacokinetic parameters from noncompartmental analysis. Following single-dose administration, the following PK parameters were obtained for fezolinetant and the metabolite ES259564: maximum concentration (Cmax), time of the maximum concentration (tmax), AUC from the time of dosing to time 24 hours (AUC24), AUC from the time of dosing to the last measurable concentration (AUClast), AUC from the time of dosing extrapolated to time infinity (AUCinf), apparent total clearance after extra-vascular dosing (CL/F), apparent volume of distribution during the terminal elimination phase after extra-vascular dosing (Vz/F), terminal elimination half-life (t1/2). During the multiple-dose period, concentration immediately before dosing at multiple dosing (trough concentration) (Ctrough) was assessed on Days 11 to Day 16. Day 16 PK parameters assessed were Cmax, tmax, AUC from the time of dosing to the start of the next dosing interval (AUCtau), CL/F, Vz/F, t1/2, accumulation ratio calculated using AUC (Rac[AUC]), and metabolite-to-parent ratio (MPR). Temporal change of Ctrough was plotted and a visual evaluation of steady state was conducted.
Safety
Safety was assessed based on the nature, frequency, and severity of adverse events (AEs), vital signs (blood pressure, pulse and ear temperature), routine 12-lead ECGs, and clinical laboratory tests (hematology, biochemistry, and urinalysis).
Results
Demographic Characteristics
In total,16 women were enrolled and received fezolinetant at dosage of 15 mg, 30 mg (single and multiple doses), and 60 mg. All subjects were female and of Asian race (Chinese), with a mean (SD) age of 33.1 (5.8) years.
PK Characteristics
Figure 2 shows concentration–time profiles of fezolinetant following single-dose administration of 15 mg, 30 mg, and 60 mg. Plasma PK parameters of fezolinetant at 15 mg, 30 mg and 50 mg on Days 1, 4 and 7 following single-dose administration are summarized by dose in Table 1. Fezolinetant exhibited rapid absorption, with median tmax 1.50 hours after single-dose administration of fezolinetant tablets in the fasted state, followed by a decline in plasma levels, with mean t1/2 of 6.12 to 7.69 hours at 15, 30 and 60 mg doses levels (Table 1). Cmax and AUCinf showed a dose-proportional increase for fezolinetant across the 15, 30 and 60 mg doses studied. Mean Cmax values were 221, 439 and 834 ng/mL, respectively, for the 15, 30 and 60 mg single doses. The drug exposure parameters had a low to moderate variability (21.1% to 39.7%) at the dose levels tested. Mean AUCinf values were 1330, 2530 and 4930, respectively. Mean AUC24 values were 1240 h*ng/mL for 15 mg, 2330 h*ng/mL for 30 mg and 4520 for 60 mg, with a CV% ranging from 27.4% to 29.3% across the doses tested (Table 1). The mean Vz/F values for single dose were 104, 142 and 139 L in the 15, 30 and 60 mg dose groups, respectively.
 |
Table 1 Plasma PK Parameters of Fezolinetant After Single- and Multiple-Dose Administration of Fezolinetant (Pharmacokinetic Analysis Set) |
 |
Figure 2 Mean plasma concentration–time profiles of fezolinetant following single-dose administration of 15 mg, 30 mg and 60 mg; linear scale. |
Concentration–time profiles after 7 days administration are shown in Figure 3, and mean Ctrough of fezolinetant on the first day of multiple dosing through 7 days multiple administrations is shown in Figure 4. Steady state was achieved after first dose with once daily dosing (Figure 4). At steady-state, on Day 7, median tmax was 1.25 hours (Table 1). Mean Cmax was 481 ng/mL and the mean AUC24 value was 2690 h*ng/mL Mean t1/2 was 9.74 hours, which was slightly longer than observed for single-dose administration of 15 to 60 mg (6.12 to 7.69 hours) (Table 1). The mean CL/F was comparable across single and multiple-dose administration. Fezolinetant had minimal accumulation after 7 days of once daily dosing of 30 mg with accumulation ratios (Rac[AUC] of 1.15, respectively.
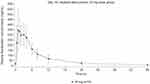 |
Figure 3 Mean plasma concentration–time profiles of fezolinetant following multiple-dose administration of 30 mg (Day 16); linear scale. |
 |
Figure 4 Individual and mean trough concentration–time profiles of fezolinetant following multiple-dose oral administration of 30 mg on Day 10 through Day 16. |
Figure 5 shows concentration–time profiles of ES259564 following single- and multiple-dose administration. Metabolite ES259564 showed rapid formation following a single-dose of fezolinetant, with a median tmax of 1.50 to 2.00 hours (Table 2). Plasma levels then declined, with mean t1/2 ranging from 5.72 to 6.31 hours across the doses tested (this parameter showed moderate variability; CV% ranged from 23.5% to 30.5%). Only minor metabolite levels were detected beyond 24 hours post-dose. A dose-proportional increase in Cmax and AUCinf were observed for ES259564 following single-dose administration of 15, 30 and 60 mg fezolinetant (Table 2). Mean ES259564 Cmax values were 88.2, 190 and 389 ng/mL, following 15, 30 and 60 mg doses of fezolinetant, respectively, with a moderate variability (CV% range: 26.3% to 29.4%) (Table 2). After multiple administration of 30 mg fezolinetant once daily for 7 days (from Day 10 to Day 16), there was a marginal accumulation of ES259564 (Rac[AUC] was 1.17). ES259564 systemic exposure was less than 70% of the parent AUC. The MPR ranged from 0.652 to 0.696 following single and multiple-dose administration of fezolinetant.
 |
Table 2 Plasma PK Parameters of Fezolinetant Metabolite ES259564 After Single- and Multiple-Dose Administration of Fezolinetant (Pharmacokinetic Analysis Set) |
Safety
In total, 6 (37.5%) subjects experienced 12 treatment-emergent adverse events (TEAEs) (Table 3). TEAEs by preferred term were diarrhea, increased blood cholesterol and decreased hemoglobin (each event was reported by 2 [12.5%] subjects). Of the TEAEs, 3 (18.8%) subjects experienced 4 drug-related TEAE. All TEAEs were of mild severity; over the entire study period, there were no deaths, SAEs, TEAEs leading to discontinuation of study drug, or AEs of special interest. Overall, there were no clinically meaningful findings related to fezolinetant in vital signs and 12-lead ECG.
 |
Table 3 Summary of Treatment-Emergent Adverse Events (Safety Analysis Set) |
Discussion
This clinical study was the first study to assess the PK and safety profile of fezolinetant in a Chinese population. Fezolinetant’s PK profile has been previously evaluated in White and Japanese individuals. The PK profile and safety and tolerability data for fezolinetant for doses up to 180 mg from the Japanese study were used to support initiation of the Eastern Asian Phase 3 study (MOONLIGHT studies). Based on Phase 2 studies, the therapeutic dose of fezolinetant was expected to be between 30 and 45 mg. As a result, we investigated the PK profile of fezolinetant in the expected therapeutic range (15 to 60 mg). Given that the target population of fezolinetant is limited to women, the study was conducted in Chinese female subjects to support the development further directly in China.
In this study, rapid absorption of fezolinetant with a short half-life (6 to 8 h) and linear PK exposure was observed relative to dose following oral administration to healthy Chinese women. A similar PK profile was also observed for its metabolite ES259564. These findings are similar to results from other Phase 1 studies of fezolinetant in healthy women. While comparison between these studies is limited by the different dose ranges, the observed fezolinetant exposure (AUC and Cmax) normalized by dose level is generally comparable to that in Japanese women. Further investigation requires a more integrated evaluation.
Over the course of this study, oral administration of fezolinetant was safe and well tolerated after administration of single-doses (15 to 60 mg) and 7-day multiple-doses (30 mg once daily) in healthy Chinese female subjects. No new safety findings were identified during the study, and although fezolinetant’s safety profile was favorable, few conclusions can be drawn from these short-term safety data. However, these results mirror those of studies conducted in other countries in healthy white women, which showed that fezolinetant was well tolerated during single- and multiple-dose escalation. Furthermore, the longer-term safety for fezolinetant in Chinese women has also been demonstrated in the MOONLIGHT study, at a dose of 30 mg.26 There were no clinically significant changes over the dose groups in any laboratory parameters, vital signs, or electrocardiographic measurements.24
Conclusion
In summary, this was the first study to assess PK in a Chinese population. Oral administration of fezolinetant was safe and well tolerated after administration of single-doses (15 to 60 mg) and 7-day multiple-doses (30 mg once daily) in healthy Chinese female subjects. A linear PK was confirmed within the tested dose range of 15 to 60 mg, and the reported PK was similar to those reported for White and Japanese women. These findings support fezolinetant’s continued development as a novel nonhormonal treatment option for VMS associated with menopause.
Abbreviations
AEs, Adverse Events; AUC, Area Under the Concentration–Time Curve; AUC24, Area Under the Concentration–Time Curve from the time of dosing to 24 hours; AUCinf, Area Under the Concentration–Time Curve extrapolated to infinity; AUClast, Area Under the Concentration–Time Curve from the time of dosing to the last measurable concentration; AUCtau, Area Under the Concentration–Time Curve over the dosing interval (time between doses); BMI, Body Mass Index; CIOMS, Council for International Organizations of Medical Sciences; CL/F, Apparent Total Clearance after extravascular dosing; Cmax, Maximum Concentration; Ctrough, Trough Concentration (concentration immediately prior to the next dose); CV%, Coefficient of Variation Percentage; ECG, Electrocardiogram; ES259564, Metabolite of fezolinetant; GCP, Good Clinical Practice; HT, Hormone Therapy; ICH, International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use; LC-MS/MS, Liquid Chromatography-Tandem Mass Spectrometry; MOONLIGHT, Name of the clinical studies mentioned; MPR, Metabolite-to-Parent Ratio; NCT, National Clinical Trial number (identifier for clinical trial registration); NKB, Neurokinin B; NK3R, Neurokinin 3 Receptor; NMPA, National Medical Products Administration; PK, Pharmacokinetics; Rac[AUC], Accumulation Ratio calculated using Area Under the Curve; SAEs, Serious Adverse Events; SWAN, Study of Women’s Health Across the Nation; t1/2, Terminal Elimination Half-Life; TEAE, Treatment emergent adverse event; tmax, Time of Maximum Concentration; VMS, Vasomotor Symptoms; Vz/F, Apparent Volume of Distribution during the terminal elimination phase after extravascular dosing.
Data Sharing Statement
Details for how researchers may request access to anonymized participant level data, trial level data and protocols from Astellas sponsored clinical trials can be found at https://www.clinicaltrials.astellas.com/transparency/
Ethical Approval and Informed Consent
The study was conducted in compliance with ethical principles originating from the Declaration of Helsinki, Good Clinical Practice (GCP), International Council for Harmonization (ICH) guidelines, Council for Organizations of Medical Sciences (CIOMS) International Ethical Guidelines and applicable laws and regulations. An independent ethics committee approved the study, and prior to initiation of any study-related procedures, all subjects provided written informed consent.
Acknowledgments
The authors would like to thank the study investigators, and all individuals who took part in the study. Medical writing support was provided by Sue Cooper of Envision Scientific Solutions and funded by Astellas Pharma Global Development.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by Astellas Pharma China, Inc.
Disclosure
Yang Li reports study funding from Astellas, Aixin Shi and Yue Liu report no competing interests, Megumi Iwai, Masato Takeuchi, Nan Song, and Yuan Li are employees of Astellas.
Ms Megumi Iwai reports personal fees for Medical Writing from Envision Pharma Group, during the conduct of the study.
The authors report no other conflicts of interest in this work.
References
1. Whiteley J, Wagner JS, Bushmakin A, Kopenhafer L, Dibonaventura M, Racketa J. Impact of the severity of vasomotor symptoms on health status, resource use, and productivity. Menopause. 2013;20(5):518–524. doi:10.1097/GME.0b013e31827d38a5
2. Whiteley J, DiBonaventura M, Wagner JS, Alvir J, Shah S. The impact of menopausal symptoms on quality of life, productivity, and economic outcomes. J Womens Health. 2013;22(11):983–990. doi:10.1089/jwh.2012.3719
3. Ayers B, Hunter MS. Health-related quality of life of women with menopausal hot flushes and night sweats. Climacteric. 2013;16(2):235–239. doi:10.3109/13697137.2012.688078
4. Yu Q, Chae HD, Hsiao SM, et al. Prevalence, severity, and associated factors in women in East Asia with moderate-to-severe vasomotor symptoms associated with menopause. Menopause. 2022;29(5):553–563. doi:10.1097/GME.0000000000001949
5. English M, Stoykova B, Slota C, et al. Qualitative study: burden of menopause-associated vasomotor symptoms (VMS) and validation of PROMIS sleep disturbance and sleep-related impairment measures for assessment of VMS impact on sleep. J Patient Rep Outcomes. 2021;5(1):37. doi:10.1186/s41687-021-00289-y
6. Utian WH. Psychosocial and socioeconomic burden of vasomotor symptoms in menopause: a comprehensive review. Health Qual Life Outcomes. 2005;3:47. doi:10.1186/1477-7525-3-47
7. Deecher DC, Dorries K. Understanding the pathophysiology of vasomotor symptoms (hot flushes and night sweats) that occur in perimenopause, menopause, and postmenopause life stages. Arch Womens Ment Health. 2007;10(6):247–257. doi:10.1007/s00737-007-0209-5
8. Avis NE, Crawford SL, Greendale G, et al. Duration of menopausal vasomotor symptoms over the menopause transition. JAMA Intern Med. 2015;175(4):531–539. doi:10.1001/jamainternmed.2014.8063
9. Freeman EW, Sammel MD, Sanders RJ. Risk of long-term hot flashes after natural menopause: evidence from the Penn Ovarian Aging Study cohort. Menopause. 2014;21(9):924–932. doi:10.1097/GME.0000000000000196
10. Gold EB, Colvin A, Avis N, et al. Longitudinal analysis of the association between vasomotor symptoms and race/ethnicity across the menopausal transition: study of women’s health across the nation. Am J Public Health. 2006;96(7):1226–1235. doi:10.2105/AJPH.2005.066936
11. The Hormone Therapy Position Statement of The North American Menopause Society” Advisory Panel. The 2022 hormone therapy position statement of The North American Menopause Society. Menopause. 2022;29(7):767–794. doi:10.1097/GME.0000000000002028
12. National Institute for Health and Care Excellence. Menopause: diagnosis and management. Available from:https://www.nice.org.uk/guidance/ng23/resources/menopause-diagnosis-and-management-pdf-1837330217413.
13. Baber RJ, Panay N, Fenton A, IMSW Writing Group. 2016 IMS Recommendations on women’s midlife health and menopause hormone therapy. Climacteric. 2016;19(2):109–150. doi:10.3109/13697137.2015.1129166
14. British Menopause Society BMS Consensus Statement. Non-hormonal-based treatments for menopausal symptoms. https://thebms.org.uk/publications/consensus-statements/non-hormonal-based-treatments-menopausal-symptoms/.
15. Depypere H, Lademacher C, Siddiqui E, Fraser GL. Fezolinetant in the treatment of vasomotor symptoms associated with menopause. Expert Opin Investig Drugs. 2021;30(7):681–694. doi:10.1080/13543784.2021.1893305
16. Astellas Pharma AG. VEOZATM (Fezolinetant): public risk management plan (RMP) summary. Available from:. https://www.swissmedic.ch/dam/swissmedic/en/dokumente/marktueberwachung/rmp/fezolinetant_veoza_rmp-summary.pdf.download.pdf/Fezolinetant_Veoza_Public_Risk_Management_Plan_Summary.pdf.
17. Astellas Pharma Australia Pty Ltd. Australian product information - VEOZA™ (Fezolinetant). Available from https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent=&id=CP-2024-PI-01388-1&d=20240314172310101.
18. Astellas Pharma US Inc. VEOZAHTM Highlights of prescribing information. Available from https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/216578s000lbl.pdf.
19. European Medicines Agency. Veoza. Annex I. Summary of Product Characteristics. Available from: https://www.ema.europa.eu/en/documents/product-information/veoza-epar-product-information_en.pdf.
20. Medicines & Healthcare Products Regulatory Agency. Public Assessment Report. National procedure. Veoza 45 mg film-coated tablets fezolinetant. PLGB00166/0437. Available from https://mhraproducts4853.blob.core.windows.net/docs/452eebb63cf697a3a4bea8b85ed6effbfa0f7332.
21. Astellas Pharma (Thailand) Co., Veoza. National Drug Information. 2024. Available from: https://ndi.fda.moph.go.th/uploads/drug_detail_corporation/doc/word/1263/7da2f987ac81862a9307dca4e641557d-a1.pdf.
22. Depypere H, Timmerman D, Donders G, et al. Treatment of menopausal vasomotor symptoms with fezolinetant, a neurokinin 3 receptor antagonist: a phase 2a trial. J Clin Endocrinol Metab. 2019;104(12):5893–5905. doi:10.1210/jc.2019-00677
23. Fraser GL, Hoveyda HR, Clarke IJ, et al. The NK3 receptor antagonist ESN364 interrupts pulsatile LH secretion and moderates levels of ovarian hormones throughout the menstrual cycle. Endocrinology. 2015;156(11):4214–4225. doi:10.1210/en.2015-1409
24. Fraser GL, Ramael S, Hoveyda HR, Gheyle L, Combalbert J. The NK3 receptor antagonist ESN364 suppresses sex hormones in men and women. J Clin Endocrinol Metab. 2016;101(2):417–426. doi:10.1210/jc.2015-3621
25. Ruan X, Bai W, Ren M, et al. Efficacy and safety of fezolinetant for moderate to severe vasomotor symptoms associated with menopause among women in East Asia: a phase 3 randomized study (MOONLIGHT I). J Int Med Res. 2024;52(5):3000605241247684. doi:10.1177/03000605241247684
26. Yu Q, Ming F, Ma J, et al. Long-term safety of fezolinetant in Chinese women with vasomotor symptoms associated with menopause: the phase 3 open-label MOONLIGHT 3 clinical trial. J Int Med Res. 2024;52(5):3000605241246624. doi:10.1177/03000605241246624
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



