Back to Journals » Drug Design, Development and Therapy » Volume 19
Analgesic Efficacy of Thoracoscopic Direct-View Versus Ultrasound-Guided Thoracic Paravertebral Block in Multi-Port Video-Assisted Thoracoscopic Lung Surgery: A Randomized Controlled Non-Inferiority Study
Authors Tong Y, Wu J, Wu X, Mo Y, Wang F
Received 19 August 2024
Accepted for publication 25 February 2025
Published 12 March 2025 Volume 2025:19 Pages 1825—1838
DOI https://doi.org/10.2147/DDDT.S492040
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Georgios Panos
Yao Tong,1,* Jimin Wu,2,* Xuhui Wu,3 Yunchang Mo,1 Faxing Wang2,4
1Department of Anesthesiology, the First Affiliated Hospital of Wenzhou Medical University, Wenzhou, People’s Republic of China; 2Department of Anesthesiology, Lishui People’s Hospital, Lishui Hospital of Wenzhou Medical University, Lishui, People’s Republic of China; 3Department of Thoracic Surgery, Lishui People’s Hospital, Lishui Hospital of Wenzhou Medical University, Lishui, People’s Republic of China; 4Oujiang Laboratory (Zhejiang Lab for Regenerative Medicine, Vision and Brain Health), Wenzhou Medical University, Wenzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Faxing Wang, Department of Anesthesiology, Lishui People’s Hospital, Lishui Hospital of Wenzhou Medical University, No. 15, Dazhong Street, Lishui, Zhejiang Province, 323000, People’s Republic of China, Email [email protected] Yunchang Mo, Department of Anesthesiology, the First Affiliated Hospital of Wenzhou Medical University, Shangcai Village, Nanbaixiang Street, Ouhai District, Wenzhou, Zhejiang, 325000, People’s Republic of China, Email [email protected]
Purpose: This study compares the analgesic effects of the Thoracoscopic Direct-view Thoracic Paravertebral Nerve Block (DTPVB) with those of the Ultrasound-guided Thoracic Paravertebral Nerve Block (UTPVB), providing a clinical reference.
Patients and Methods: Sixty-eight patients undergoing three-port video-assisted thoracic surgery (VATS) with general anesthesia were randomly assigned to either the DTPVB group (Group D, n = 34) or the UTPVB group (Group U, n = 34). Both groups received a 10 mL injection of 0.75% ropivacaine at the T4 and T7 interspaces. Primary outcomes were cumulative sufentanil equivalents from the start of lung manipulation to 24 hours postoperatively, with group differences assessed against a non-inferiority margin of 5 μg (Δ). Secondary outcomes include postoperative pain scores, analgesic consumption, patient satisfaction, adverse effects, and other related indicators.
Results: The cumulative use of sufentanil equivalents from the start of lung manipulation to 24 hours postoperatively was 35.0 ± 6.1 μg in Group D and 33.2 ± 5.6 μg in Group U, with no significant difference (P = 0.217). The difference in cumulative sufentanil equivalents (Group D minus Group U) was 1.8 (95% CI − 1.07, 4.65), within the non-inferiority margin of 5 (Δ). Postoperative pain scores, analgesic consumption, adverse effects, and complications were similar were similar between groups. However, DTPVB was associated with lower anxiety and higher satisfaction (P< 0.001). At 15 minutes post-block, ropivacaine plasma concentrations were higher in Group D (P=0.024).
Conclusion: DTPVB, via transmural pleural puncture, was non-inferior to UTPVB in analgesic efficacy from the beginning of the manipulation of the lungs in operation to 24h postoperatively. DTPVB provides a good alternative, especially for patients who are anxious before surgery, have difficulty cooperating with UTPVB, or in cases where UTPVB puncture fails. However, when using high concentrations of ropivacaine, greater vigilance for toxicity is required.
Keywords: thoracic paravertebral block, TPVB, video-assisted thoracoscopic surgery, VATS, pain management
Introduction
Video-assisted thoracoscopic surgery (VATS) has become the preferred approach for non-small cell lung tumor surgery.1,2 Compared to traditional open-chest surgery, VATS offers various advantages, including minimal surgical trauma, less pain, faster postoperative recovery, and a noticeably improved quality of life.3,4 Despite the relatively mild postoperative pain associated with VATS, some patients may still experience moderate to severe pain, necessitating the implementation of effective perioperative analgesic strategies.5 Additionally, the concept of enhanced recovery after surgery (ERAS) emphasizes early postoperative functional exercises and advocates minimizing opioid use during the perioperative period (both intraoperative and postoperative).6,7 ERAS suggests combining alternative analgesic methods and prioritizes ultrasound-guided regional nerve blocks.8,9
To address these problems, VATS commonly employs thoracic paravertebral nerve block (TPVB), a regional analgesic technique recommended for previous open-chest surgeries and shown to be comparable to Thoracic Epidural Analgesia (TEA).10,11 Studies suggest that a single TPVB effectively alleviates pain 12 to 24 hours postoperatively.12 It can also extend postoperative analgesia when used in conjunction with other medications.13,14 However, although ultrasound-guided Thoracic Paravertebral Nerve Block (UTPVB) is a reliable technique, the application of UTPVB in VATS lung surgery is limited by differences in anesthesiologist’s skill, the possibility of complications such as thoracic paravertebral hematoma and pneumothorax, and the need for patients to be awake and cooperative during TPVB in the upper thoracic scapular region.15–18
Recently, a new method called thoracoscopic Direct-view Thoracic Paravertebral Nerve Block (DTPVB), transmural pleura puncture, has been used for postoperative pain management in thoracoscopic surgery patients. Studies showed that combining DTPVB with Patient-Controlled Intravenous Analgesia (PCIA) was more effective in reducing postoperative pain and opioid use compared to PCIA with intravenous sufentanil alone.19,20 Therefore, DTPVB under VATS may be a good alternative with the advantage of visualizing the pleural cavity under direct thoracoscopic visualization, ensuring accurate rib clearance and depth, especially in patients with poor-quality ultrasound imaging. This technique may be better at reducing the number of punctures, minimizing postoperative complications, relieving patient perioperative tension as well as promoting faster recovery.
However, the effectiveness of DTPVB was mainly compared to a non-intervention group rather than a well-established UTPVB. Limited research exists on the clinical application and safety of DTPVB when performed through the mural pleura. Our randomized controlled study aims to demonstrate that DTPVB performed through the mural pleura by surgeons under direct thoracoscopic vision is not inferior to UTPVB performed by anesthesiologists through ultrasound-guided percutaneous puncture.
Materials and Methods
Ethics and Registration
This study, conducted at the People’s Hospital in Lishui, Zhejiang, China, adhered to CONSORT guidelines. The research protocol was approved by the Ethics Review Committee of the Lishui People’s Hospital (Approval No. 2022–096) and registered with the Chinese Clinical Trial Registry (ChiCTR2300071834, http://www.chictr.org.cn, May 26, 2023). Written informed consent was obtained from all participants. This study complies with the Declaration of Helsinki, and all procedures involving human participants were approved by the relevant ethics review board.
Patient Inclusion and Exclusion Criteria
Patients aged 18–80, classified as ASA I–III, scheduled for three-port VATS lung surgery under general anesthesia between June and December 2023, were included during the pre-anesthetic assessment. All participants provided written informed consent upon entry into the study. Exclusion criteria included bilateral surgery, previous same-side surgery, mental or neurological disorders, history of liver or kidney dysfunction, BMI >30 kg/m2 or <18 kg/m2, preoperative lung infection, severe obstructive lung disease, severe asthma or chronic pain history, coagulation disorders for any reason, and extensive pleural adhesions.
Randomization and Masking
Patients were randomly assigned to either the DTPVB group (Group D) or the UTPVB group (Group U) in a 1:1 ratio, with blocks of two patients, based on a computer-generated random number sequence. The sequence was generated by an anesthesiologist not involved in the study using IBM SPSS Statistics V22.0 software (SPSS, Chicago, IL, USA). The random numbers were sealed in opaque envelopes and opened by the attending anesthesiologist after the patient entered the operating room and completed electrocardiographic monitoring. As both nerve block techniques required the cooperation of the patient, anesthesiologist, and surgeon, this study was not blinded.
Methods of Anesthesia
All patients fasted for 6 hours and refrained from drinking water for 2 hours before surgery without the use of anxiolytic medications. Upon entering the operating room, patients received routine intravenous fluid infusion and oxygen via a mask at 6 L/min and had intravenous access established. Lactated Ringer’s solution was administered at a rate of 6–10 mL · kg−1· h−1. Monitoring included electrocardiography (ECG), heart rate (HR), non-invasive systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), pulse oxygen saturation (SpO2) and bispectral index (BIS) (ConView YY-106, Pearlcare, Zhejiang, China). In addition, the End-Tidal Carbon Dioxide (EtCO2) was measured using the Mindray iPM10 monitor (Mindray Medical International Limited, China).
Induction of general anesthesia was performed using midazolam (0.04 mg/kg), propofol (1.5 mg/kg), sufentanil (0.4 µg/kg), and cisatracurium besylate (0.3 mg/kg). After the disappearance of the eyelash reflex, mask ventilation was initiated, and a suitable double-lumen endotracheal tube was inserted under visual laryngoscopy after 5 minutes. Anesthesia was maintained with inhaled 1% sevoflurane and propofol. Cisatracurium bromide (0.1 mg/kg) was intravenously injected every 40 minutes. The depth of anesthesia was maintained with BIS between 40 and 60, and sufentanil (5–10 μg) was administered when the patient’s HR or blood pressure increased >20% from the baseline measurement. Flurbiprofen ester (50 mg) was given before chest closure. Intraoperative mechanical ventilation was maintained with a tidal volume of 6–8 mL/kg and an inspired oxygen concentration of 50–100%, with the respiratory rate adjusted to target an end-tidal carbon dioxide level of 35–45 mmHg.
All patients who underwent VATS had three trocars placed intraoperatively, and a single chest tube (Ch 28) was used postoperatively. Postoperative analgesia was administered through a patient-controlled intravenous sufentanil analgesia pump containing 100 µg of sufentanil and 10 mg of tropisetron, diluted to 100 mL with 0.9% saline. There was no background dose, and each dose administered was 4 mL per press, with a lock-out time of 15 minutes. Additional intravenous analgesics such as tramadol or non-steroidal anti-inflammatory drugs were given if pain NRS remained > 3 after two consecutive sufentanil 4 µg boluses. We recorded analgesic doses and converted the tramadol dose to an equivalent dose of intravenous sufentanil: Intravenous tramadol equivalent to 5 µg intravenous sufentanil.21 Postoperative pain intensity at rest and during coughing was evaluated using an 11-point NRS score (0 = no pain, 10 = worst imaginable pain) at 0.5, 2, 6, 12, 24, 36, and 48 h after surgery.
Thoracic Paravertebral Block
UTPVB Procedure
After sterile disinfection of the operating room, UTPVB was performed in the lateral position using a transverse, planar technique. The patient was positioned on the healthy side, with the surgical side facing upward. A 2–5 MHz low-frequency convex probe was used to identify the C7 spinous process and sequentially locate the T4 and T7 levels. The probe was then rotated 90° to align parallel with the ribs. Under ultrasound guidance, the ribs, inner edge of the rib, intercostal fascia, and pleura were visualized. Once the target area was identified, a puncture was made in-plane, and when the needle tip reached the deep surface of the intercostal fascia, an injection of local anesthetic was performed. Proper positioning was confirmed by observing pleural movement and pleura moving downward after injection.22,23
DTPVB Procedure
After entering the chest and before the beginning of the manipulation of the lungs in operation, a trained thoracic surgeon identified the T4 and T7 paravertebral spaces under thoracoscopy. The puncture point, 1–1.5 cm lateral to the sympathetic nerve chain, was chosen, and a single-use scalp needle with an extension tube was used to puncture through the parietal pleura. The needle was advanced 0.5 cm, and after confirming no blood, cerebrospinal fluid, or gas during aspiration, local anesthetic was slowly injected. The pleura would bulge, and the local anesthetic enveloped by the pleura can be seen spreading towards the head and tail, indicating a successful paravertebral nerve block in the corresponding segment.19
Both groups received injections of 10 mL 0.75% ropivacaine at the T4 and T7 paravertebral spaces.
Outcomes
Primary Outcome
Due to differences in the timing of nerve block administration between the two groups, we chose to evaluate the primary outcome by measuring the cumulative sufentanil equivalents from the beginning of the manipulation of the lungs in operation to 24h postoperatively.
Secondary Outcomes
Other analgesic measures included the average NRS scores for incision and intrathoracic pain at rest and during coughing, assessed over 24 hours. Additional outcomes included sensory block dermatome regions, analgesic consumption, TPVB procedure time, plasma ropivacaine concentration, State-Trait Anxiety Inventory (STAI), postoperative recovery indicators, nerve block complications (such as paravertebral hematoma, vascular puncture, nerve injury, infection, hypotension/hypertension, respiratory depression, allergic reactions, pneumothorax, and toxic reactions to local anesthetics), and postoperative adverse reactions (such as atelectasis, pneumonia, pleural effusion requiring drainage, and pneumothorax). Patient satisfaction with analgesic methods was evaluated at 48 hours postoperatively using an 11-point scale (range, 0 to 10), where a score of 0 indicates “entirely dissatisfied” and a score of 10 means “fully satisfied”. Symptoms of anxiety were assessed using the Chinese version of the STAI, which is known for its high reliability and validity.24 The STAI includes two subscales: STAI-S (State Anxiety) and STAI-T (Trait Anxiety), each with 20 items to measure anxiety as a general trait or temporary state. Responses are recorded on a 4-point Likert scale (1 to 4), with reverse scoring for negatively worded items. Scores range from 20 (no anxiety) to 80 (extreme anxiety).25,26 In addition, emergence agitation was assessed using the Riker Sedation–Agitation Scale during the recovery period. The Riker Sedation-Agitation Scale (RSAS) is divided into seven levels, with scores ranging from 1 to 7, where higher scores indicate more severe agitation.27
The definition of pneumothorax in this study comprises two aspects: TPVB-related pneumothorax and surgery-related pneumothorax. TPVB-related pneumothorax is characterized by a positive needle suction test, as well as an air-over-water phenomenon in direct view when expanding the patient’s lungs after three trocars were inserted in the chest cavity. Surgery-related pneumothorax is diagnosed through postoperative X-ray examination. Quantification of nerve blocking effect: Cold sensation was assessed with ice and compared with the contralateral area until there was no change. We defined each intercostal skin as a “dermatome region”. We defined sensory blocks in at least two dermatome regions as successful.28 We recorded the time from needle puncture to the end of the injection. We performed sensory tests within 24 hours of surgery. Adverse hemodynamic events trigger interventions: hypotension (SBP < 90 mmHg, DBP < 50 mmHg, or ≥ 20% MAP decrease), treated with ephedrine; hypertension (SBP > 160 mmHg, DBP > 110 mmHg, or ≥ 20% increase), treated with urapidil. Tachycardia (HR > 120 bpm) receives esmolol or causal treatments. Desaturation (SpO2 < 95%), respiratory depression (SpO2 < 95% or respiratory rate < 8 bpm for more than 1 minute), airway obstruction, or apnea were managed by lifting the lower jaw and/or providing pressure-assisted ventilation via a facemask.
Ropivacaine Concentration
A 2 mL radial artery blood sample was collected 0, 5, 10, 15, 30, 45, 60, and 90 minutes after paravertebral block in heparin-containing tubes and centrifuged at a speed of 2500 rpm for 15 minutes; the supernatant was stored in a refrigerator at −80°C. UPLC-MS/MS determined the concentration of ropivacaine in arterial blood samples.
UPLC-MS/MS: Plasma samples were centrifuged at 13000 rpm for 10 minutes. A 100 uL supernatant was transferred to a 1.5 mL centrifuge tube, to which 10μL lidocaine (500ng/mL) was added as an internal standard, along with 300μL acetonitrile. The mixture was vortexed for 2 minutes and then centrifuged at a speed of 13000 rpm for 10 minutes. The supernatant was collected, diluted 1:1 with ultrapure water, and used for UPLC-MS/MS analysis. The chromatographic conditions were as follows: Chromatography column: ACQUITY UPLC BEH C18 column (2.1mm x 50 mm, 1.7 μm); column temperature: 40°C; flow rate: 0.4 mL/min; injection volume: 2μL; mobile phase: 0.1% formic acid, acetonitrile; elution time: 2 minutes. Mass spectrometry conditions were as follows: multiple reaction monitoring (MRM) modes; desolvation gas flow: N2, flow rate 1000 L/hour; temperature: 600°C; ion source temperature: 150°C.29,30
The UPLC-MS/MS method used in this experiment has been validated through recovery rate, matrix effect, precision, and stability.
Sample Size Estimation
Based on previous pretrial results, the cumulative sufentanil equivalents were 32.4±5.1 µg for the U group and 33.3±5.8 µg for the D group. Taking into account existing literature,31 as well as discussions with statistical and clinical experts, we set the non-inferiority margin at 5µg,28 deeming it clinically acceptable as it reflects real-world clinical conditions and effectively prevents inappropriate type II error rates. To achieve 90% statistical power and a significance level of 0.025, 27 patients per group are required, totaling 54 patients. Considering a potential 20% data loss, the final required sample size is 68 patients.
Statistical Analysis
All analyses were conducted using R statistical software (http://www.R-project.org, The R Foundation) and Free Statistics version 1.3. Normality and homogeneity of variance were assessed using the Shapiro–Wilk and Levene’s tests, respectively. Continuous variables with normal distribution are presented as mean ± standard deviation and compared using independent t-tests. Skewed variables are expressed as median (P25, P75) and compared using the U rank-sum test. Categorical data are presented as numbers (percentages) and compared using the chi-square or Fisher’s exact test. Repeated measures ANOVA was used for intra-group comparisons. Mauchly’s test assessed sphericity and the Shapiro–Wilk test checked the normality of residuals. If sphericity was violated, the Greenhouse-Geisser correction was applied to adjust the degrees of freedom, ensuring result robustness. A significance level of P<0.05 was set. Cumulative sufentanil equivalents were used to evaluate the non-inferiority of DTPVB compared to UTPVB, with the upper limit of the mean difference within Δ (5) under α = 0.025 and β = 0.1 indicating “non-inferiority”.
Results
We initially assessed 77 patients for eligibility, with 6 not meeting the inclusion criteria and 3 declining to participate. Consequently, 68 patients were randomly assigned and received the study intervention. All preoperative, intraoperative, and postoperative assessments were completed. However, one patient was excluded due to withdrawal, leaving 67 patients for analysis. The detailed flowchart is presented in Figure 1.
 |
Figure 1 Consolidated Standards of Reporting Trials (CONSORT) Flowchart describing patients progress through the study. |
Demographic and Surgical Data
Patient characteristics and surgical details are presented in Table 1, revealing no significant differences between the groups. All patients underwent unilateral thoracoscopic lung surgery, including wedge resection, segmentectomy, lobectomy, or combined procedures. In Group D and Group U, 19 and 15 patients, respectively, underwent lung wedge resection.
 |
Table 1 Patient Demographic and Surgical Parameters |
Cumulative Sufentanil Equivalents and Postoperative Pain Management
The two groups showed similar cumulative sufentanil equivalents from the beginning of the manipulation of the lungs in operation to 24 hours postoperatively. Group D consumed 35.0±6.1 μg, and Group U consumed 33.2±5.6 μg (Table 2). The difference between groups (Group D minus Group U) was 1.79 (95% CI −1.07, 4.65), with the upper limit of the 95% CI being (4.65), within the predefined non-inferiority margin of 5 μg(Δ), as depicted in Figure 2. Supplementary Figure S1 illustrates the average NRS at various time points postoperatively. Supplementary Table S1 provides additional details on rescue analgesia and PCIA pump usage at 24 and 48 hours, none of which were statistically significantly different.
 |
Table 2 Comparison of Intraoperative Data and Anesthesia-Related Data |
Intraoperative Data and Anesthesia-Related Data
As shown in Table 2, Group D had a significantly shorter average operation time (1.57 mins) compared to Group U (3.66 mins). Additionally, Group D had a lower SAI score (39.6±3.6) than Group U (46.6±5.2), indicating a statistical difference (P=0.001). We also studied the dispersion of ropivacaine and the change in the sensory block area over time in both groups. In Group D, the highest position of local anesthetic diffusion was at T1 (T1, T2), and the lowest was at T9 (T8, T9). In contrast, in Group U, the highest position of local anesthetic diffusion was at T3 (T2, T4), and the lowest was at T10 (T9, T10) (Table 2). Sensory blockade distribution was assessed using the ice method at 30 minutes, 6 hours, 12 hours, and 24 hours postoperatively. At 12 hours, the median blockade level was 2 in Group D and 3 in Group U. By 24 hours, some patients in Group U still retained one sensory block dermatome region, as shown in Supplementary Figure S2.
Supplementary Figure S3 illustrates stable hemodynamics during lung manipulation in surgery and the awakening phase, with no significant differences between the two groups. Table S1 reveals no disparities in the recovery time of spontaneous respiration, extubation time, and postoperative PACU observation duration. Additionally, Supplementary Table S1 highlights no distinctions between the groups in terms of postoperative time to first cough, cough frequency at 24 hours, time to first ambulation, and total hospital stay. Furthermore, patients in Group D reported higher satisfaction with the analgesic method than those in Group U (P=0.001). However, doctors’ satisfaction evaluations for the two pain relief methods showed no significant difference.
Adverse Events
The incidence of intraoperative hypotension was comparable between the two groups, with 7 cases in Group D and 4 cases in Group U requiring vasopressor intervention. Among these, 3 cases in Group D and 1 case in Group U required more than two doses of vasopressors. No itching or drowsiness was observed in either group. There were no significant differences in postoperative nausea, vomiting, lung infection, atelectasis, or oxygenation index on the first day. Two cases of paravertebral hematoma and pneumothorax occurred in Group U, and one case each in Group D. Postoperative drainage volume was 147.5 mL (48.75, 255) in Group D and 112.5 mL (57, 240) in Group U, with no significant difference. Specific details are presented in Table 3.
 |
Table 3 Monitoring and Profiling Adverse Events |
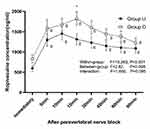
Plasma Ropivacaine Concentrations
In Group D, ropivacaine consistently had higher average plasma concentrations than in Group U, with a significant difference at 15 minutes (P=0.024). Both groups showed significant time effects (P<0.001). Even after 90 minutes of TPVB, the average plasma concentration of ropivacaine in Group D (1225.6±668.4ng/mL) remained higher than in Group U (1082.7±638.5ng/mL), as shown in Figure 3. Although Group D had a higher average plasma peak concentration (Cmax) of ropivacaine compared to Group U (2054.4±1281.5 ng/mL vs 1683.8±909.4 ng/mL), the difference was not statistically significant. Post hoc analysis indicated that, compared to UTPVB, DTPVB led to a more pronounced reduction in MAP 10 and 15 minutes after nerve block. Additionally, both methods resulted in a decrease in heart rate (HR) at 15 minutes post-TPVB, as shown in Supplementary Figure S4.
Discussion
In this prospective randomized controlled study, the analgesic effect of DTPVB was no worse than that of UTPVB from the beginning of intraoperative lung procedures to 24 hours after surgery. The cumulative use equivalent of sufentanil was comparable between the two TPVB methods, and the distance between the non-inferiority threshold and the upper threshold of the primary outcome indicated the non-inferiority of DTPVB. There were also no significant differences in other secondary outcomes, including additional analgesic consumption, NRS score, intraoperative and postoperative hemodynamic changes, evaluation of recovery, nerve block-related complications, and adverse drug reactions. Our results also showed that DTPVB was easy to operate and reduced puncture time. Moreover, because DTPVB was administered after general anesthesia, patients reported higher satisfaction with analgesic modalities and lower SAI scores. Therefore, we suggest that DTPVB can be an effective alternative to UTPVB in patients undergoing VATS lung surgery intraoperatively and 24 hours after surgery. Notably, the plasma concentration of ropivacaine at all time points of DTPVB exceeded UTPVB, and the peak plasma concentration of Ropivacaine reached the threshold of potential central nervous system toxicity in two patients receiving DTPVB. Although there were no clinical local anesthetic drug toxicity events in the study, it is still necessary to be vigilant about local anesthetic drug toxicity.
As a prerequisite for the non-inferiority trial, TPVB surpasses control groups (intercostal nerve block, erector spinae plane block, serratus anterior plane block, retrolaminar block, or local infiltration analgesia) in analgesic efficacy 24 hours post-VATS lung surgery, as the study indicated.32 However, UTPVB may still have a failure of analgesia because UTPVB usually requires skilled ultrasound guidance technology, and the patient’s obesity, anxiety, and other factors will also lead to poor imaging. There is a possibility of paravertebral hematoma, pneumothorax, and other complications.33–35 Since the failure of analgesia may have an adverse effect on patient prognosis, surgeons should consider other local analgesia methods with the same effect in the face of failure or inability to perform UTPVB. Our study supports that the surgeon-led DTPVB technique is safe and effective and can be used as an alternative method when UTPVB is not performed or cannot be performed.
In our study, we hypothesized that the analgesic effect of surgeon-performed DTPVB via transpleural puncture is not inferior to UTPVB. Although the DTPVB technique has previously been successfully applied for postoperative analgesia in single-port pulmonary wedge resection and thoracolaparoscopic esophagectomy, there is insufficient research comparing UTPVB and DTPVB, and there is a lack of adequate data to support the widespread adoption of this technique. To our knowledge, this randomized controlled trial is the largest study to date comparing the thoracoscopically guided transpleural DTPVB technique with the ultrasound-guided percutaneous UTPVB technique. DTPVB is performed under direct thoracoscopic vision by inserting a scalp needle through the parietal pleura, 1–1.5 cm lateral to the sympathetic chain.19 This procedure is simple and rapid and achieves a diffusion effect similar to UTPVB through a single injection at the same site. In contrast, UTPVB often requires multiple adjustments to reach the target location. Additionally, in DTPVB, patient factors such as obesity, perioperative anxiety, or the ability to cooperate during interscapular block are not limiting factors. This should be considered an advantage of DTPVB, as these factors are associated with higher block failure rates in UTPVB. However, the main limitation of DTPVB is the reduced or absent visualization of the paravertebral area due to poor lung isolation or pleural adhesions. Consequently, we implemented rigorous screening for these patients at the beginning of the trial. When UTPVB or DTPVB cannot be performed due to technical issues, poor lung isolation, or pleural adhesions, alternative analgesic methods should be considered. These options include the use of intravenous opioids (such as morphine or fentanyl), non-steroidal anti-inflammatory drugs (NSAIDs), and PCIA pumps.36 Additionally, depending on the specific circumstances, epidural analgesia, local infiltration anesthesia, or other regional nerve block techniques (eg, intercostal nerve block or serratus anterior nerve block) may be considered.32,36,37
In addition, this trial found that the plasma ropivacaine concentration peaked 15 minutes after DTPVB, and the average ropivacaine plasma concentration at each time point was higher than UTPVB. This may be related to the slow leakage of ropivacaine through the puncture site and the absorption of local anesthetic in the chest cavity. Although we are careful of this phenomenon during the administration of the drug, the negative pressure after closing the chest may still cause it to penetrate the chest from the puncture site. Previous studies have also shown that parietal pleural injury can increase the plasma concentration of local anesthetics.38,39 This may also explain the faster decline of sensory block dermatome in group D six hours after surgery. However, it is not clear whether the anesthetic drugs in the pleural cavity also play an analgesic role or merely lead to an increase in peak concentration. In this trial, two patients in the D group had plasma Cmax of Ropivacaine reaching 5.5 μg/mL and 6.2 μg/mL. A study has shown that mild CNS toxicity symptoms appeared at a ropivacaine plasma concentration of 1–2 μg/mL in healthy volunteers.40 However, another study found that no toxic symptoms were observed even at a maximum concentration of 4.2 μg/mL of ropivacaine.41 Knudsen K et al reported that the toxic central nervous system reaction occurred at 4.3 (3.4–5.3) μg/mL during intravenous administration of ropivacaine.42,43 Ropivacaine predominantly binds to plasma proteins (primarily α1-acid glycoprotein) at 94%, leaving 6% free.44 In this trial, two patients post-DTPVB peaked at 5.5–6.2 μg/mL plasma. Their calculated free concentrations (330–372 ng/mL) fall within the CNS toxicity range (300–900 ng/mL).42 Although no typical toxic effects of local anesthetic drugs were observed, the toxic effects of local anesthetic drugs still need to be vigilant.
In the post-analysis, a significant difference in MAP occurred 10 and 15 minutes after TPVB. Both groups experienced a temporary MAP decrease post-block. The decrease of MAP in group D from the basal value was more obvious than that in group U, which we believe may be attributed to the following three factors: (1) DTPVB directly penetrating the wall pleura at 1–1.5 cm lateral to the sympathetic chain, which was closer to the sympathetic chain and more accessible to block, or even completely block, the sympathetic chain; (2) part of local anesthetics leaked from the paravertebral space into the thoracic cavity, and the absorption rate of ropivacaine was accelerated, which in turn inhibit the circulation. Although we did not find any cases of local anesthetic poisoning, this may be due to the influence of general anesthetic drug masking; (3) the high-pressure area of the pleural wrap is closer to the intervertebral foramen during DTPVB injection, and there is a greater likelihood of infiltration into the epidural. The high concentration of ropivacaine is more likely to pass through sparse tissues and potential interstitial space.
Our study has a few limitations. First, it was conducted in a single center and only included patients undergoing multi-port VATS lung surgery. Therefore, we must be cautious about extending the conclusions to a broader context. Second, the anesthesiologists and patients knew the intervention types that could introduce bias. However, both groups were unaware of the alternative intervention, and patient-reported outcomes, like STAIS and satisfaction assessments, were self-recorded, reducing bias to some extent. Third, more research is vital to determine the ideal ropivacaine concentration and dosage for DTPVB, evaluating its pain-relieving effects in thoracic surgery. Finally, we did not conduct a questionnaire 30 days or longer after surgery to assess the long-term outcome of chronic pain after surgery.
Conclusion
In this study, the DTPVB technique performed by the surgeon through pleural puncture was not inferior to the UTPVB performed by the anesthesiologist in terms of opioid consumption in the 24 hours after pulmonary surgery. However, when performing DTPVB with high concentrations of ropivacaine, greater vigilance for local anesthetic toxicity is necessary compared to UTPVB.
Data Sharing Statement
The datasets generated and/or analyzed during the current study are available from either of the two corresponding authors upon reasonable request.
Acknowledgment
We express our gratitude to the patients who participated in this study, as well as the physicians and nurses in the post-anesthesia care unit (PACU).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This project is supported by the Zhejiang Medical and Health Science and Technology Project (Project No. 2023KY2378).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bendixen M, Jørgensen OD, Kronborg C, Andersen C, Licht PB. Postoperative pain and quality of life after lobectomy via video-assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: a randomised controlled trial. Lancet Oncol. 2016;17(6):836–844. doi:10.1016/S1470-2045(16)00173-X
2. Ikeda N. Updates on minimally invasive surgery in non-small cell lung cancer. Curr Treat Options Oncol. 2019;20(2):16. doi:10.1007/s11864-019-0614-9
3. Zhu M, Fu XN, Chen X. Lobectomy by video-assisted thoracoscopic surgery (VATS) for early stage of non-small cell lung cancer. Front Med. 2011;5(1):53–60. doi:10.1007/s11684-011-0121-2
4. Boffa DJ, Kosinski AS, Furnary AP, et al. Minimally invasive lung cancer surgery performed by thoracic surgeons as effective as thoracotomy. J Clin Oncol. 2018;36(23):2378–2385. doi:10.1200/JCO.2018.77.8977
5. Sun K, Liu D, Chen J, et al. Moderate-severe postoperative pain in patients undergoing video-assisted thoracoscopic surgery: a retrospective study. Sci Rep. 2020;10(1):795. doi:10.1038/s41598-020-57620-8
6. Whitson BA, Groth SS, Duval SJ, Swanson SJ, Maddaus MA. Surgery for early-stage non-small cell lung cancer: a systematic review of the video-assisted thoracoscopic surgery versus thoracotomy approaches to lobectomy. Ann Thorac Surg. 2008;86(6):2008–2016. discussion 2016-2018. doi:10.1016/j.athoracsur.2008.07.009
7. Lim E, Batchelor T, Dunning J, et al. Video-assisted thoracoscopic or open lobectomy in early-stage lung cancer. NEJM Evid. 2022;1(3):EVIDoa2100016. doi:10.1056/EVIDoa2100016
8. Elsayed HH, Moharram AA. Tailored anaesthesia for thoracoscopic surgery promoting enhanced recovery: the state of the art. Anaesth Crit Care Pain Med. 2021;40(2):100846. doi:10.1016/j.accpm.2021.100846
9. Zorrilla-Vaca A, Rice D, Brown JK, et al. Sustained reduction of discharge opioid prescriptions in an enhanced recovery after thoracic surgery program: a multilevel generalized linear model. Surgery. 2022;171(2):504–510. doi:10.1016/j.surg.2021.08.039
10. Davies RG, Myles PS, Graham JM. A comparison of the analgesic efficacy and side-effects of paravertebral vs epidural blockade for thoracotomy--a systematic review and meta-analysis of randomized trials. Br J Anaesth. 2006;96(4):418–426. doi:10.1093/bja/ael020
11. Gulbahar G, Kocer B, Muratli SN, et al. A comparison of epidural and paravertebral catheterisation techniques in post-thoracotomy pain management. Eur J Cardiothorac Surg. 2010;37(2):467–472. doi:10.1016/j.ejcts.2009.05.057
12. Li XL, Zhang J, Wan L, Wang J. Efficacy of single-shot thoracic paravertebral block combined with intravenous analgesia versus continuous thoracic epidural analgesia for chronic pain after thoracotomy. Pain Physician. 2021;24(6):E753–E759.
13. Hong B, Lim C, Kang H, et al. Thoracic paravertebral block with adjuvant dexmedetomidine in video-assisted thoracoscopic surgery: a randomized, double-blind study. J Clin Med. 2019;8(3):352. doi:10.3390/jcm8030352
14. Abd-Elshafy SK, Abdallal F, Kamel EZ, et al. Paravertebral dexmedetomidine in video-assisted thoracic surgeries for acute and chronic pain prevention. Pain Physician. 2019;22(3):271–280.
15. Wang R, Huang X, Wang Y, Akbari M. Non-pharmacologic approaches in preoperative anxiety, a comprehensive review. Front Public Health. 2022;10:854673. doi:10.3389/fpubh.2022.854673
16. Yeung JH, Gates S, Naidu BV, Wilson MJ, Gao Smith F. Paravertebral block versus thoracic epidural for patients undergoing thoracotomy. Cochrane Database Syst Rev. 2016;2(2):CD009121. doi:10.1002/14651858.CD009121.pub2
17. Kosiński S, Fryźlewicz E, Wiłkojć M, Ćmiel A, Zieliński M. Comparison of continuous epidural block and continuous paravertebral block in postoperative analgaesia after video-assisted thoracoscopic surgery lobectomy: a randomised, non-inferiority trial. Anaesthesiol Intensive Ther. 2016;48(5):280–287. doi:10.5603/AIT.2016.0059
18. Pace MM, Sharma B, Anderson-Dam J, Fleischmann K, Warren L, Stefanovich P. Ultrasound-guided thoracic paravertebral blockade: a retrospective study of the incidence of complications. Anesth Analg. 2016;122(4):1186–1191. doi:10.1213/ANE.0000000000001117
19. Hu L, Xu X, Tian H, He J. Effect of single-injection thoracic paravertebral block via the intrathoracic approach for analgesia after single-port video-assisted thoracoscopic lung wedge resection: a randomized controlled trial. Pain Ther. 2021;10(1):433–442. doi:10.1007/s40122-020-00231-y
20. Hu L, Xu X, Shen W, He J. Feasibility and effectiveness of multi-injection thoracic paravertebral block via the intrathoracic approach for analgesia after thoracoscopic-laparoscopic esophagectomy. Esophagus. 2021;18(3):513–521. doi:10.1007/s10388-020-00807-9
21. Miller’s basics of anesthesia. Eur J Anaesthesiol. 2024;41(2):153–154. doi:10.1097/EJA.0000000000001943
22. Ma Y, Li B, Sun L, et al. A prospective randomized comparison of the efficacy of standard antiviral therapy versus ultrasound-guided thoracic paravertebral block for acute herpes zoster. Ann Med. 2022;54(1):369–378. doi:10.1080/07853890.2022.2031267
23. Zhao Y, Zheng S, Cai N, et al. Utility of artificial intelligence for real-time anatomical landmark identification in ultrasound-guided thoracic paravertebral block. J Digit Imaging. 2023;36(5):2051–2059. doi:10.1007/s10278-023-00851-8
24. Ma WF, Liu YC, Chen YF, Lane HY, Lai TJ, Huang LC. Evaluation of psychometric properties of the Chinese mandarin version state-trait anxiety inventory Y form in Taiwanese outpatients with anxiety disorders. J Psychiatr Ment Health Nurs. 2013;20(6):499–507. doi:10.1111/j.1365-2850.2012.01945.x
25. Ruffinengo C, Versino E, Renga G. Effectiveness of an informative video on reducing anxiety levels in patients undergoing elective coronarography: an RCT. Eur J Cardiovasc Nurs. 2009;8(1):57–61. doi:10.1016/j.ejcnurse.2008.04.002
26. Reck C, Zimmer K, Dubber S, Zipser B, Schlehe B, Gawlik S. The influence of general anxiety and childbirth-specific anxiety on birth outcome. Arch Womens Ment Health. 2013;16(5):363–369. doi:10.1007/s00737-013-0344-0
27. Jo JY, Jung KW, Kim HJ, et al. Effect of total intravenous anesthesia vs volatile induction with maintenance anesthesia on emergence agitation after nasal surgery: a randomized clinical trial. JAMA Otolaryngol Head Neck Surg. 2019;145(2):117–123. doi:10.1001/jamaoto.2018.3097
28. Xu ZZ, Li X, Chen BL, et al. A randomised controlled trial of the non-inferiority of erector spinae plane block vs. thoracic paravertebral block for laparoscopic nephro-ureterectomy. Anaesthesia. 2023;78(4):442–448. doi:10.1111/anae.15959
29. Chen Y, Cai Y, Ye Y, et al. Single and repeated intrapleural ropivacaine administration: a plasma concentration and pharmacodynamics study. J Pain Res. 2021;14:785–791. doi:10.2147/JPR.S295913
30. Chen S, Ma J, Wang X, Zhou Q. Simultaneous determination of ropivacaine and 3-hydroxy ropivacaine in cerebrospinal fluid by UPLC-MS/MS. Biomed Res Int. 2020;2020(1):8844866. doi:10.1155/2020/8844866
31. Chenesseau J, Fourdrain A, Pastene B, et al. Effectiveness of surgeon-performed paravertebral block analgesia for minimally invasive thoracic surgery: a randomized clinical trial. JAMA Surg. 2023;158(12):1255–1263. doi:10.1001/jamasurg.2023.5228
32. Sandeep B, Huang X, Li Y, Xiong D, Zhu B, Xiao Z. A comparison of regional anesthesia techniques in patients undergoing video-assisted thoracic surgery: a network meta-analysis. Int J Surg. 2022;105:106840. doi:10.1016/j.ijsu.2022.106840
33. Naja Z, Lönnqvist PA. Somatic paravertebral nerve blockade. Incidence of failed block and complications. Anaesthesia. 2001;56(12):1184–1188. doi:10.1111/j.1365-2044.2001.2084-2.x
34. Richardson J, Lönnqvist PA, Naja Z. Bilateral thoracic paravertebral block: potential and practice. Br J Anaesth. 2011;106(2):164–171. doi:10.1093/bja/aeq378
35. Lönnqvist PA, MacKenzie J, Soni AK, Conacher ID. Paravertebral blockade. Failure rate and complications. Anaesthesia. 1995;50(9):813–815. doi:10.1111/j.1365-2044.1995.tb06148.x
36. Feray S, Lubach J, Joshi GP, Bonnet F, Van de Velde M. PROSPECT guidelines for video-assisted thoracoscopic surgery: a systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia. 2022;77(3):311–325. doi:10.1111/anae.15609
37. Moorthy A, Ní Eochagáin A, Dempsey E, et al. Postoperative recovery with continuous erector spinae plane block or video-assisted paravertebral block after minimally invasive thoracic surgery: a prospective, randomised controlled trial. Br J Anaesth. 2023;130(1):e137–e147. doi:10.1016/j.bja.2022.07.051
38. Fagenholz PJ, Bowler GM, Carnochan FM, Walker WS. Systemic local anaesthetic toxicity from continuous thoracic paravertebral block. Br J Anaesth. 2012;109(2):260–262. doi:10.1093/bja/aes126
39. Komatsu T, Sowa T, Kino A, Fujinaga T. The importance of pleural integrity for effective and safe thoracic paravertebral block: a retrospective comparative study on postoperative pain control by paravertebral block. Interact Cardiovasc Thorac Surg. 2015;20(3):296–299. doi:10.1093/icvts/ivu395
40. Mather LE, Copeland SE, Ladd LA. Acute toxicity of local anesthetics: underlying pharmacokinetic and pharmacodynamic concepts. Reg Anesth Pain Med. 2005;30(6):553–566. doi:10.1016/j.rapm.2005.07.186
41. Salonen MH, Haasio J, Bachmann M, Xu M, Rosenberg PH. Evaluation of efficacy and plasma concentrations of ropivacaine in continuous axillary brachial plexus block: high dose for surgical anesthesia and low dose for postoperative analgesia. Reg Anesth Pain Med. 2000;25(1):47–51. doi:10.1016/s1098-7339(00)80010-3
42. Knudsen K, Beckman Suurküla M, Blomberg S, Sjövall J, Edvardsson N. Central nervous and cardiovascular effects of i.v. infusions of ropivacaine, bupivacaine and placebo in volunteers. Br J Anaesth. 1997;78(5):507–514. doi:10.1093/bja/78.5.507
43. Stewart J, Kellett N, Castro D. The central nervous system and cardiovascular effects of levobupivacaine and ropivacaine in healthy volunteers. Anesth Analg. 2003;97(2):412–416. doi:10.1213/01.ANE.0000069506.68137.F2
44. Hansen TG. Ropivacaine: a pharmacological review. Expert Rev Neurother. 2004;4(5):781–791. doi:10.1586/14737175.4.5.781
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.