Back to Journals » Journal of Pain Research » Volume 18
Analgesic Quality Improvement in Paravertebral Blocks for Pediatric Nuss Procedure: An Exploratory Report on the Effects of Perineural Combined Glucocorticoids
Authors Donham RN, Jin E, Caty MG, Thomas DA, Yuan C, Hollingsworth K, Zhang X, Yanez ND, Li J
Received 23 October 2024
Accepted for publication 23 January 2025
Published 27 January 2025 Volume 2025:18 Pages 489—496
DOI https://doi.org/10.2147/JPR.S502600
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Karina Gritsenko
Rebecca N Donham,1,* Evan Jin,2,* Michael G Caty,3 Donna-Ann Thomas,2 Claire Yuan,4 Kamren Hollingsworth,2 Xuewei Zhang,2 N David Yanez,5 Jinlei Li2,*
1Alabama College of Osteopathic Medicine, Dothan, AL, USA; 2Department of Anesthesiology, Yale University School of Medicine, New Haven, CT, USA; 3Department of Surgery, Yale University School of Medicine, New Haven, CT, USA; 4Harvard University, Cambridge, MA, USA; 5Department of Anesthesiology, Duke University School of Medicine, Durham, NC, USA
*These authors contributed equally to this work
Correspondence: Jinlei Li, Department of Anesthesiology, Yale University School of Medicine, 20 York Street, New Haven, CT, 06510, USA, Tel +1 (475) 434-4038, Email [email protected]
Purpose: Pectus excavatum repair using the Nuss procedure is associated with significant postoperative opioid consumption even in the presence of a continuous thoracic paravertebral block.
Patients and Methods: A CQI project was initiated by adding combined glucocorticoids as perineural adjuvants to continuous thoracic paravertebral block. An electronic health record review of patients undergoing Nuss procedures by a single surgeon at a major academic children’s hospital from June 2013 to December 2021 was performed with no patients excluded. The patients received pre-incision continuous bilateral T4 paravertebral blocks preoperatively either with plain ropivacaine (standard group, N = 34) or with a combination of dexamethasone sodium phosphate (DXP) and methylprednisolone acetate (MPA) in addition to ropivacaine (experimental group, N = 10). The primary outcome studied was postoperative opioid consumption measured by oral morphine milligram equivalents (MME).
Results: A total of 44 patients were included in the final analysis. The experimental group had 72% lower postoperative opioid usage than the standard group during the hospitalization (p < 0.001) with comparable pain scores and hospital length of stay and no increase in wound dehiscence or other complications.
Conclusion: The addition of dexamethasone sodium phosphate and methylprednisolone acetate to continuous paravertebral blocks significantly decreased postoperative opioid consumption while maintaining comfort pain scores.
Keywords: Nuss procedure, paravertebral, dexamethasone, methylprednisolone acetate
A Letter to the Editor has been published for this article.
A Response to Letter by Mr Li has been published for this article.
Introduction
Pectus excavatum, an abnormal concavity of the chest wall, may be surgically corrected in adolescents with the Nuss procedure. A recent survey of academic children’s hospitals in the United States showed that there is no consensus on how to effectively manage the significant postoperative pain associated with the Nuss procedure.1 Several regional anesthetic techniques have been explored, including continuous thoracic epidural analgesia (EA), continuous thoracic paravertebral nerve block (TPVB), and continuous erector spinae plane block (ESPB).2 Epidural analgesia appears to provide the best pain relief, but it carries the risk of failed block, upper extremity neurologic deficits, hemodynamic instability, and increased hospital length of stay.1,3 Continuous TPVB and ESPB with local anesthetics represent alternatives to EA but are thought to be suboptimal in terms of analgesic effects.1,4
Nonparticulate dexamethasone sodium phosphate (DXP) and particulate methylprednisolone acetate (MPA) are commonly used to prolong single injection neuraxial and peripheral nerve blocks.5,6 Previous studies by this group showed that a single dose of perineural DXP and MPA before the threading of nerve block catheters decreased the requirement of local anesthetics without changes in pain scores or opioid consumption in lower extremity fascia plane blocks.7 In addition, as compared to perineural DXP alone, the addition of MPA to DXP further decreases postoperative opioid consumption in knee surgery.5 Utilizing a single surgeon’s historical data over 8 years, this current study examined retrospectively whether the addition of a single dose of DXP and MPA via TPVB improved the quality of analgesia from the TPVB in pediatric Nuss procedure. The specific aim is to investigate the effects of perineural DXP and MPA combination on the analgesic quality of paravertebral blocks measured by opioid-reducing effect. The working hypothesis was that patients who received the glucocorticoid adjuncts DXP and MPA would have reduced in-hospital opioid usage as compared to those without. The primary outcome studied was postoperative total opioid consumption over the course of the entire hospitalization.8 Secondary outcomes included patient-reported visual analogue scale (VAS) pain scores on a numeric rating scale from 0 to 10, antiemetics usage, length of hospital stay, time between patient discharge and first physical therapy session, and 90-day complications including rates of re-operation, emergency room visit or hospital readmission.
Materials and Methods
Data Source / Patient Population
Yale University institutional review board exempt data extraction was performed from the electronic medical record at an academic children’s hospital for patients who underwent Nuss Bar surgery by the same surgeon (MGC) from June 2013 to December 2021. Data extracted included the Haller index (a measure of the degree of concavity of the chest wall), age, sex, body mass index (BMI), operative duration, total postoperative opioid usage over the course of the hospitalization reported in morphine milligram equivalents (MME), administration of antiemetics, patient-reported VAS pain score, time between patient discharge and first physical therapy session (a marker of patient’s ability to exercise during recovery), 90 days re-operation and emergency room visits. Also recorded were serum glucose values for the patients who had them taken.
Standard group patients (N = 34) received continuous bilateral T4 TPVB without any glucocorticoid adjuncts placed preoperatively, while the experimental group (N = 10) patients received one-time perineural DXP and MPA glucocorticoid combination in TPVB right before the continuous TPVB catheters were placed preoperatively. In addition to the TPVB, a small percentage of patients in both the standard group (N = 2) and the intervention group (N = 6) received additional bilateral T4 single-shot ESP blocks. The patients in the glucocorticoid group were primarily patients having surgery between late 2019 and 2021, during which a perineural glucocorticoids protocol was in place in the study institute. There were no other additional changes in pain management protocol for patients in the study duration.
Ultrasound-Guided Bilateral TPVB and ESPB Techniques
TPVBs were placed in a preoperative procedure room with patients placed in either a sitting or prone position after standard American Society of Anesthesiologists (ASA) monitors were placed and were sedated with 2mg midazolam and 100 μg Fentanyl intravenously. The T4-T5 paravertebral space on one side was identified using a curvilinear, low-frequency ultrasound probe (Sonosite X-Porte, Bothell, WA, USA) in the paramedian sagittal orientation. Using sterile technique and skin infiltration with 0.5 mL 1% lidocaine local anesthetic, a short bevel insulated nerve block needle (Contiplex® Tuohy, 18G, 4-inch, B. Braun Medical USA, Bethlehem, PA, USA) was advanced in-plane under direct visualization until it reached the target paravertebral space. Then, a weight-based bolus dose of local anesthetic (usually 0.2% ropivacaine) was injected into the space. If glucocorticoids (5 mg DXP and 40 mg MPA) were administered, they were mixed with the bolus local anesthetic before injection. A catheter (Perifix® catheter, 20G, B. Braun Medical USA, Bethlehem, PA, USA) was then threaded into the paravertebral space. The same was repeated on the contralateral side.
Eight of the 44 patients received a single-shot, bilateral ESPB in addition to the PVB bolus and catheter placement. For these patients, the same curvilinear, low-frequency ultrasound probe was placed in a paramedian sagittal orientation at T4-T5 interspace, the transverse process with the overlying erector spinae muscle was identified. A weight-based bolus dose with local anesthetics, as well as 2.5 mg DXP and 20 mg MPA, was given once needle contact was made with the transverse process. The provider then proceeded to paravertebral catheter placement as described above. The same was repeated on the contralateral side.
Upon arrival in the operating room, general anesthesia was induced in both groups with intravenous fentanyl 3 μg/kg, propofol 2.5 mg/kg, and rocuronium 0.6 mg/kg. After tracheal intubation, general anesthesia was maintained with sevoflurane at 1–1.5 MAC in both groups, with intermittent fentanyl and morphine in response to surgical stimulation. All patients received glycopyrrolate and neostigmine reversing neuromuscular blockade before extubation.
Once in the post-anesthesia care unit (PACU), a continuous infusion was started for each TPVB catheter at 0.2% ropivacaine at 5 mL/hr. Patients were placed on multimodal analgesia with acetaminophen, diazepam, gabapentin, and ketorolac (ketorolac only if approved by the surgical team). Patients with more tolerable pain received oxycodone by mouth at a dose of 5–10 mg every 3 hours (q3h) as needed with morphine IV 30 mcg/kg q3h for breakthrough pain. Patients with greater pain received morphine patient-control analgesia (PCA) pumps with 20 mcg/kg dose with a 10-minute lockout. The acute pain service evaluated the paravertebral catheters every day and gave 5 mL bolus doses of 0.2% ropivacaine if needed, in addition to the continuous infusion dose of 0.2% ropivacaine captured in the electronic record. The paravertebral catheters were typically removed on postoperative day four.
Statistical Analysis
Statistical analysis analyses were performed using bivariate and adjusted group-level comparisons. Quantitative variables (eg, Haller Index, BMI, age, and surgery duration) were compared between the study groups (ie, patients receiving glucocorticoids and patients not receiving glucocorticoids) using Welch’s unequal variance t-test. Comparisons of categorical variables (eg, sex) were performed using chi-square tests or two-sided Fisher’s Exact tests. Formal comparisons between the two study groups were made by adjusting for potential confounding factors.
All outcomes, except for total hospital MME consumption, were analyzed using linear regression and incorporated robust (sandwich) standard error estimates. For total hospital MME consumption, we performed linear regression on the logarithm transformation of the outcome and back transformed the estimates to interpret geometric mean estimates. All statistical tests and confidence intervals are two-sided. Serum glucose values were recorded sparingly so no formal statistical analysis was performed with regard to them.
Results
The study population was a relatively homogenous group of adolescents, with the standard and experimental groups displaying no significant difference in the recorded baseline characteristics of Haller index, age, sex, BMI, ASA physical status and surgery duration (Table 1).
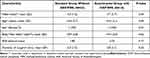 |
Table 1 Baseline Characteristics of Study Subjects |
Regression analysis showed that the primary outcome of postoperative opioid consumption in the experimental group with glucocorticoids was statistically lower than that in standard group (Figure 1).
Adjustments were made for age, sex, BMI, Haller index, and duration of surgery as covariates. Those that received the experimental block had a geometric mean total hospitalization MME that was 72% lower than the patients that received the standard block, a highly statistically significant result (P-value < 0.001). The 95% confidence interval suggests that patients that received the experimental block might have a lower geometric mean (43% to 86% lower than the standard block therapy) (Table 2).
 |
Table 2 Perioperative and Postoperative Outcomes |
The significant reduction in postoperative opioid consumption did not appear to affect patient’s self-reported minimum, average or maximum pain levels (Table 2). Additionally, the days from discharge to first physical therapy session were not found to be statistically significant nor was there a significant difference in patient’s post-operative return to the operating room (OR) and emergency room (ER). Antiemetic administration was comparable between the experimental and standard groups.
Serum glucose levels were inconsistently obtained in the patients likely due to low concern for the laboratory value preoperatively or postoperatively (Table 3). Only 7 patients had both pre-operative and post-operative glucose values. Of these, only 3 patients had higher postoperative values and they all belonged to the non-steroid group.
 |
Table 3 Serum Glucose Values |
Discussion
This single-center single-surgeon historical retrospective cohort study showed a significant reduction in opioid usage with comparable pain scores in patients who received the bilateral continuous TPVB with MPA and DXP versus those who did not. The study also showed that the inclusion of DXP and MPA into peripheral nerve blocks was not associated with any detectable adverse events such as hyperglycemia, delayed wound healing, increase in hospital length of stay, a return to the ER or OR, or a delay on the initiation of outpatient physical therapy. As far as we know, this is the first contribution to the literature assessing the impacts of glucocorticoids on continuous TPVB for pediatric Nuss procedure.
Glucocorticoids such as DXP and MPA are commonly used as local anesthetic adjuvants in single injection epidural injections and peripheral nerve blocks for chronic pain management. The mechanism is multi-factorial including direct effects on nerves that result in the downregulation of inflammatory mediators and indirect effects through systemic absorption. The study provides insight into the use of particulate glucocorticoids in peripheral nerve blocks (PNB) outside of chronic pain management into perioperative acute pain management. DXP has been shown to increase the duration of analgesia from a bolus dose by approximately 4–6 hours.9 Particulate glucocorticoids like MPA are thought to provide a slow-onset but long-acting depot of glucocorticoid at the target nerve.10,11 Unfortunately, this study cannot comment on the additive effect of particulate glucocorticoids as there was no comparison between patients who received particulate glucocorticoids versus those that just received the more commonly used non-particulate glucocorticoids like DXP. We started this CQI project based on previous success by this group using combined non-particulate and particulate glucocorticoids (which decrease local anesthetic requirement through continuous nerve block catheters, pain scores and opioid consumption for 48–72 hours)5,7,12 rather than non-particulate glucocorticoids alone (which prolong nerve blocks for only a fraction of a single day).13 However, the apparent safety of particulate glucocorticoids in this population gives promise for a future study making such a comparison.
Glucocorticoid adjuncts are mostly recognized for increasing the duration of analgesia from single injection peripheral nerve block. Our study indicated that in the presence of a continuous TPVB catheter that provides a continuous infusion of local anesthetic to the nerve, glucocorticoids may have an added effect of additional reduction of postoperative opioid consumption.10,14 This is consistent with previous findings from this group of investigators that decreased patient-control demand doses of local anesthetic infusion through the continuous nerve block catheter when glucocorticoid adjuncts were used.5,7 Taken together, these studies support the idea that glucocorticoid use augments the quality of the analgesia in not only single injection but also continuous peripheral nerve blocks.
The strategy of employing regional blocks with steroid adjuncts may provide an alternative to the current long-acting therapy for pain management after Nuss procedure – cryoablation. Cryoablation is the use of thermally conducted cold needles to destroy surrounding tissue and small nerves in an effort to provide long-term analgesia. Cryoablation has been shown to be beneficial for pain relief in patients who undergo the Nuss procedures; however, it is also associated with significant complications such as Nuss hardware malalignment, permanent loss of thoracic sensation, chronic neuropathic pain, and pneumothorax. Patients who received cryoablation also had an associated increased odds ratio of slipped bars requiring reoperation.15–19
The limitations of this study include the small sample size, which may make the results difficult to generalize as shown in the scatter plot that in the “standard” group there are 3 obvious outliers (>3K on the MME log scale) suggesting either block failure or partial failure or the low concentration of local anesthetics (0.2% ropivacaine) not strong enough for certain patients and additional effects from steroids made the block much stronger. Nonetheless, due to the large range of total hospital MME consumption, we performed linear regression on the logarithm transformation of the outcome and back transformed the estimates to interpret geometric mean estimates. In addition, the study did include all patients within the specified time frame with accessible medical records making the sample at least more representative. The retrospective study design also creates possibilities for confounding even in a relatively young and healthy patient population. It is important to note that patients in the non-glucocorticoid group had their procedures mostly from 2013 to 2019, while patients in the glucocorticoid group had their procedures from 2019 to 2021 (the practice of routinely adding glucocorticoid adjuncts began in 2019), but there have been no significant changes in multimodal analgesia. It may also be speculated that greater awareness of opioid side effects over the course of the study period may have contributed to patients later in the study period receiving fewer opioid medications, but the similar pain scores and length of hospital stays during the study period argue against these. The supervising providers giving the nerve blocks experienced mild changes over the course of the study, and they all came from a subspecialty group within the academic practice that specializes in regional anesthesia procedures. This single surgeon has not modified his surgical techniques in the study duration either. Additionally, the retrospective design did not allow for standardized collection of certain outcome measures. Pain scores may have only been recorded when patients were in most pain and asking for pain medication. This lack of standardized reporting may explain the lack of difference between the groups in terms of pain scores. Boluses of local anesthetic through the indwelling TPVB catheters were also not recorded so its effect on the opioid administration could not be quantified. Additionally, variations in practitioner preference allowed for the administration of ESPB in some patients, with a greater proportion in the glucocorticoid group. It may be argued that the ESPB exerts its analgesic effect through spread into the paravertebral space and may be of no benefit when added to a TPVB, which is supported by current literature.20,21 However, it cannot be ignored that a large proportion of patients in the intervention group received this extra block and could be a confounding factor. For example, one might say that due to the relative ease and reduced risk of ESPB the people performing the blocks may have had greater success with ESPB than with the TPVB.
Despite the limitations detailed above, it is noteworthy that interests in less invasive alternatives to EA such as TPVB and ESPB in Nuss procedure have generated promising yet suboptimal results.4,22–25 Our study is the first designed to augment TPVB’s analgesic effects by using glucocorticoids as local anesthetic adjuvants. Future directions would be to compare the efficacy and safety of continuous TPVB or ESPB with epidural analgesia, as well as single injection TPVB or ESPB vs continuous epidural analgesia in the presence of glucocorticoids, preferably in a prospectively randomized control study.
Conclusion
This study showed that a combination of DXP and MPA in TPVB yielded a significant decrease in opioid intake in Nuss Bar pediatric patients without significant adverse effect on post-operative recovery.
Ethics Approval and Informed Consent
Given the retrospective nature of the research, on May 4th, 2022, Yale’s Human Research Protection Program Institutional Review granted a waiver of HIPAA authorization and informed consent from patients were not required for access to medical record and use of protected health information (HIC 2000032821). With Yale University institutional review board approval, data was extracted from the electronic medical record at an academic children’s hospital. All data were immediately de-identified once the initial data collection were complete to maintain patient data confidentiality and compliance with the Declaration of Helsinki.
Funding
This work was funded in part by the Foundation for Anesthesia Education and Research - FAER MSARF through a grant to the Yale Department of Anesthesiology for Rebecca Donham (MSARF-10-01/2022). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors have no relevant financial or non-financial interests to disclose for this work.
References
1. Muhly WT, Beltran RJ, Bielsky A, et al. Perioperative management and in-hospital outcomes after minimally invasive repair of pectus excavatum: a multicenter registry report from the society for pediatric anesthesia improvement network. Anesth Analg. 2019;128(2):315–327. doi:10.1213/ANE.0000000000003829
2. Lee JM, Gee E, Liu CA. Anesthesia for innovative pediatric surgical procedures. Anesthesiol Clin. 2020;38(3):493–508. doi:10.1016/j.anclin.2020.06.004
3. Mavi J, Moore DL. Anesthesia and analgesia for pectus excavatum surgery. Anesthesiol Clin. 2014;32(1):175–184. doi:10.1016/j.anclin.2013.10.006
4. Walter CM, Lee CS, Moore DL, et al. Retrospective study comparing outcomes of multimodal epidural and erector spinae catheter pain protocols after pectus surgery. J Pediatr Surg. 2022;58(3):397–404. doi:10.1016/j.jpedsurg.2022.06.017
5. Toro-Pagan NM D, Dai F, Banack T, et al. Perineural methylprednisolone depot formulation decreases opioid consumption after total knee arthroplasty. J Pain Res. 2022;15:2537–2546. doi:10.2147/JPR.S378243
6. Pino CS, Rathmell JC. Chapter 92: interventional Management of Chronic Pain. In: Longnecker DE, Mackey SC, Newman MF, Sandberg WS, Zapol WM, editors. Anesthesiology.
7. Baldev K, Dai F, Barrett C, et al. Glucocorticoid minimizes local anesthetic infusion requirement through adductor canal block and improves perioperative prosthetic joint range of motion in total knee arthroplasty. PLoS One. 2022;17(1):e0261949. doi:10.1371/journal.pone.0261949
8. Opioid Equianalgesic Dosing Chart(ed)^(eds), 2018.
9. Desai N, Kirkham KR, Albrecht E. Local anaesthetic adjuncts for peripheral regional anaesthesia: a narrative review. Anaesthesia. 2021;76(Suppl 1):100–109. doi:10.1111/anae.15245
10. Rijsdijk M, van Wijck AJ, Kalkman CJ, Yaksh TL. The effects of glucocorticoids on neuropathic pain: a review with emphasis on intrathecal methylprednisolone acetate delivery. Anesth Analg. 2014;118(5):1097–1112. doi:10.1213/ANE.0000000000000161
11. Li J, Li L, Zhang X, et al. Paravertebral block with compound betamethasone in laparoscopic cholecystectomy: a double-blind randomized controlled trial. Cureus. 2019;11(10):e6023. doi:10.7759/cureus.6023
12. Li J, Dai F, Ona Ayala KE, Zhou B, Schonberger RB, Sharma A. Transmuscular quadratus lumborum and lateral femoral cutaneous nerve block in total hip arthroplasty. Clin J Pain. 2021;37(5):366–371. PMID: 33577193; PMCID: PMC8035232.doi:10.1097/AJP.0000000000000923
13. Kirkham KR, Jacot-Guillarmod A, Albrecht E. Optimal dose of perineural dexamethasone to prolong analgesia after brachial plexus blockade: a systematic review and meta-analysis. Anesth Analg. 2018;126(1):270–279. PMID: 28922230.doi:10.1213/ANE.0000000000002488
14. Zorrilla-Vaca A, Li J. Dexamethasone injected perineurally is more effective than administered intravenously for peripheral nerve blocks: a meta-analysis of randomized controlled trials. Clin J Pain. 2018;34(3):276–284. doi:10.1097/AJP.0000000000000519
15. Green CR, de Rosayro AM, Tait AR. The role of cryoanalgesia for chronic thoracic pain: results of a long-term follow up. J Natl Med Assoc. 2002;94(8):716–720.
16. Sujka J, Benedict LA, Fraser JD, Aguayo P, Millspaugh DL, St Peter SD. Outcomes using cryoablation for postoperative pain control in children following minimally invasive pectus excavatum repair. J Laparoendosc Adv Surg Tech A. 2018;28(11):1383–1386. doi:10.1089/lap.2018.0111
17. Chidambaran V, Garcia VF, Brown RL. Are We Ready for Cryoablation in Children Undergoing Nuss Procedures? Anesth Analg. 2022;134(4):881–884. doi:10.1213/ANE.0000000000005857
18. Freezing Out Pain: Intercostal Cryoablation Is Improving Pectus Excavatum Recovery(Ed)^(Eds). Cleveland Clinic; 2024.
19. Sun RC, Mehl SC, Anbarasu CR, et al. Intercostal cryoablation during Nuss procedure: a large volume single surgeon’s experience and outcomes. J Pediatr Surg. 2021;56(12):2229–2234. doi:10.1016/j.jpedsurg.2021.03.006
20. Chin KJ, El-Boghdadly K. Mechanisms of action of the erector spinae plane (ESP) block: a narrative review. Can J Anaesth. 2021;68(3):387–408. doi:10.1007/s12630-020-01875-2
21. Zhang L, Hu Y, Liu H, et al. Analgesic efficacy of combined thoracic paravertebral block and erector spinae plane block for video-assisted thoracic surgery: a prospective randomized clinical trial. Med Sci Monit. 2023;29(e940247). PMID: 37408302; PMCID: PMC10334846. doi:10.12659/MSM.940247
22. Bliss Jr DP Jr, Strandness TB, Derderian SC, Kaizer AM, Partrick DA. Ultrasound-guided erector spinae plane block versus thoracic epidural analgesia: postoperative pain management after Nuss repair for pectus excavatum. J Pediatr Surg. 2022;57(2):207–212. doi:10.1016/j.jpedsurg.2021.10.030
23. Hall Burton DM, Boretsky KR. A comparison of paravertebral nerve block catheters and thoracic epidural catheters for postoperative analgesia following the Nuss procedure for pectus excavatum repair. Paediatr Anaesth. 2014;24(5):516–520. doi:10.1111/pan.12369
24. Ren Y, Zheng T, Hua L, Zhang F, Ma Y, Zhang J. The effect of ultrasound-guided erector spinae plane block versus thoracic epidural block on postoperative analgesia after nuss surgery in paediatric patients: study protocol of a randomized non-inferiority design trial. J Pain Res. 2021;14:3047–3055. doi:10.2147/JPR.S332078
25. Loftus PD, Elder CT, Russell KW, et al. Paravertebral regional blocks decrease length of stay following surgery for pectus excavatum in children. J Pediatr Surg. 2016;51(1):149–153. doi:10.1016/j.jpedsurg.2015.10.037
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


