Back to Journals » Infection and Drug Resistance » Volume 18
Analysis of Clinical Characteristics and the Effect of Symptomatic Supportive Treatment for Severe Neonatal Enterovirus Infection
Authors Xuan Z, Wang T, Li N, Tang Z
Received 30 November 2024
Accepted for publication 8 May 2025
Published 22 May 2025 Volume 2025:18 Pages 2629—2636
DOI https://doi.org/10.2147/IDR.S507842
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Zhe Xuan,1 Ting Wang,1 Ning Li,1 Ziqian Tang2
1Department of Neonatology, Zhuzhou Central Hospital, Zhuzhou, Hunan, 412000, People’s Republic of China; 2Department of Obstetrics and Gynecology, Zhuzhou Central Hospital, Zhuzhou, Hunan, 412000, People’s Republic of China
Correspondence: Ziqian Tang, Email [email protected]
Objective: To retrospectively analyze cases of neonatal enterovirus (EV) infection, identify risk factors for severe infection, pathological characteristics, and prognostic differences, and provide a basis for early identification of high-risk neonates.
Methods: Neonates diagnosed with EV infection and admitted to Zhuzhou Central Hospital between January 2020 and December 2023 were included in the study. Based on disease severity, they were divided into a mild infection group (n = 149) and a severe infection group (n = 44). Data on demographic characteristics, clinical manifestations, laboratory findings, treatment methods, and prognosis were collected and statistically analyzed using SPSS 26.0.
Results: Compared to the mild infection group, the severe infection group had lower gestational age (36.61 vs 38.50 weeks, P < 0.001) and higher preterm birth rates (P < 0.05). They presented earlier with higher incidences of rash, respiratory symptoms, and sepsis-like signs (all P < 0.05). Severe cases had significantly higher rates of pneumonia, myocarditis, necrotizing hepatitis, and DIC (all P < 0.001), with a mortality rate of 54.55% (P < 0.001). Laboratory findings showed more thrombocytopenia, coagulation dysfunction, and organ injury markers in the severe group (all P < 0.001). Mild cases required mainly non-invasive treatment, while severe cases had high mortality despite intensive interventions. Among survivors, 50% required long-term neurological rehabilitation.
Conclusion: Severe neonatal EV infection is closely associated with preterm birth and perinatal infection, characterized by thrombocytopenia, coagulation dysfunction, and multiple organ damage. Early monitoring of high-risk neonates, especially preterm infants, should be reinforced. For neonates presenting within the first seven days of life with rash or respiratory distress accompanied by a rapid decline in platelet count, intensive care should be promptly initiated. Further research is needed to explore targeted antiviral therapies and immune modulation strategies.
Keywords: neonate, enterovirus, severe infection, symptomatic supportive treatment, retrospective study
Introduction
Enteroviruses (EVs), as important members of the Picornaviridae family, encompass various serotypes, including coxsackieviruses, echoviruses, polioviruses, and enterovirus 71 (EV71). These viruses are transmitted through the digestive and respiratory tracts, leading to a broad spectrum of clinical manifestations ranging from asymptomatic infections to severe neurological diseases, myocarditis, and other life-threatening conditions.1,2 Although EV infections can affect individuals of all age groups, neonates, due to their immature immune systems, represent a high-risk population, with case fatality rates for severe infections reaching 10%-25%.3 Global epidemiological data indicate significant regional differences in the distribution of EV infections: outbreaks in temperate regions (eg, North America and Europe) peak during summer and autumn, whereas in tropical countries (eg, Southeast Asia and sub-Saharan Africa), infections occur year-round, with underdiagnosis rates exceeding 40% due to limited medical resources.4 These disparities underscore the urgent need to establish universal management strategies for neonatal EV infections.
Neonatal EV infections often present with nonspecific clinical manifestations, making them difficult to distinguish from bacterial sepsis, which leads to delayed diagnosis. The atypical symptoms primarily stem from the unique immunological deficiencies of neonates: 1) Impaired innate immune response – Neonates exhibit inadequate activation of Toll-like receptor (TLR3/7/8) signaling pathways, resulting in significantly reduced interferon-α/β production (only 15–20% of adult levels). Consequently, early inflammatory biomarkers such as C-reactive protein (CRP) and interleukin-6 (IL-6) lack specificity in neonatal EV infections.5 2) Immature adaptive immunity – The neutralizing antibodies passively acquired from the mother are significantly lower in preterm infants (<28 weeks of gestational age), with antibody titers being only 30% of those observed in full-term infants. This deficiency weakens the ability to control viral replication and dissemination.6 Moreover, the disease progression in neonates is markedly “hyper-acute”, with approximately 50% of severe cases deteriorating into multi-organ failure within 12–24 hours after fever onset, whereas in adults, a similar progression typically takes 48–72 hours. This rapid clinical course further shortens the diagnostic window and increases the risk of fatal outcomes.7
Clinicians face dual challenges in managing neonatal EV infections: 1) Diagnostic limitations – Although reverse transcription-polymerase chain reaction (RT-PCR) is the gold standard for EV detection, approximately 65% of neonatal intensive care units (NICUs) worldwide lack routine access to this test, particularly in low-income regions. As a result, physicians often rely on bacterial culture exclusion methods, which require 48–72 hours, delaying appropriate antiviral interventions.8 2) Uncertainty in treatment protocols – Current international guidelines emphasize symptomatic supportive care (eg, inotropic support for cardiac function and anticonvulsant therapy for encephalitis). However, there is no consensus on key management decisions, such as the optimal timing for mechanical ventilation, intensity of interventions, and adaptation strategies in resource-limited settings. These discrepancies have led to significant intercenter variations in mortality rates (ranging from 12% to 34%).9 For instance, a multicenter study found that, in sub-Saharan Africa, the lack of vasoactive drugs resulted in a 2.3-fold higher mortality rate in neonates with EV-associated myocarditis compared to developed countries.10
Although previous studies have explored the clinical characteristics of neonatal EV infections, systematic analyses of severe cases and evaluations of supportive treatment efficacy remain limited. This study aims to retrospectively analyze the clinical manifestations, laboratory findings, and their correlation with disease severity in severe neonatal EV infections, while also assessing the impact of different supportive treatment strategies on patient outcomes. The key contributions of this study include: 1) Providing a clearer clinical classification system to help physicians identify high-risk cases at an early stage, thereby optimizing monitoring and treatment decisions. 2) Evaluating the efficacy of different supportive treatment strategies, offering clinical evidence for more precise management approaches for severe neonatal EV infections. 3) Identifying key factors influencing disease progression, laying the foundation for future development of targeted antiviral therapies and immunomodulatory interventions.
In summary, this study addresses a critical gap in the clinical characterization and treatment strategies for severe neonatal EV infections, providing an important reference for optimizing neonatal EV infection management on a global scale. Through an in-depth investigation, we aim to offer stronger scientific evidence for clinical practice, ultimately improving patient outcomes, reducing mortality rates, and enhancing treatment effectiveness.
Materials and Methods
Study Population
This study was designed as a retrospective analysis. Neonatal cases diagnosed with enterovirus (EV) infection admitted to Zhuzhou Central Hospital between January 2020 and December 2023 were included. After applying strict inclusion criteria, 193 cases were registered and recorded, documenting demographic characteristics, clinical presentations, laboratory findings, treatments, and outcomes. The neonates were initially grouped based on disease severity into a mild infection group (n=149) and a severe infection group (n=44) for comparative analysis of clinical features. This study adhered to the principles of the Declaration of Helsinki and was approved by the Ethics Committee of Zhuzhou Central Hospital, with a waiver of informed consent from guardians. Informed consent was waived due to the minimal risk to subjects. Data was handled with confidentiality.
Inclusion and Exclusion Criteria
Inclusion Criteria
The study included singleton neonates born at Zhuzhou Central Hospital within 72 hours of birth with clinically or laboratory-confirmed EV infection.11 EV RNA presence was confirmed via reverse transcription-polymerase chain reaction (RT-PCR) testing of stool, blood, or cerebrospinal fluid (CSF).
Exclusion Criteria
Neonates with concurrent infections from other pathogens, or those with perinatal asphyxia, intraventricular hemorrhage, epileptic encephalopathy, genetic metabolic disorders, or severe cardiopulmonary diseases, were excluded.
Grouping Criteria
General infection was defined as the presence of symptoms such as fever without focus, rash, aseptic meningitis (cerebrospinal fluid cell count >25×106/L, negative CSF culture, and exclusion of bacterial infection), liver dysfunction, coagulation abnormalities, or myocardial damage. Severe infection was defined as the occurrence of multi-organ dysfunction, including respiratory failure, septic shock, renal failure, heart failure, or necrotizing hepatitis, requiring intensive care unit (ICU) treatment.
Related Concepts and Definitions of Complications
- Necrotizing Hepatitis: Defined as an elevation of alanine aminotransferase (ALT) levels exceeding three times the normal value, accompanied by thrombocytopenia.
- Definitions of Hepatic Dysfunction, Coagulation Disorders, Myocardial Injury, Disseminated Intravascular Coagulation (DIC), Myocarditis, Respiratory Failure, Heart Failure, Renal Failure, Premature Infants, and Full-term Infants are based on the 5th edition of Practical Neonatology.
- Infection Exposure History: Defined as close contact within two weeks prior to disease onset with individuals exhibiting gastrointestinal or respiratory symptoms, or fever, suggesting potential infection exposure.
Data Collection
Clinical data of all enrolled infants were collected, including:
- General Information: Gender, gestational age at birth, birth weight, Apgar score, mode of delivery, presence of premature rupture of membranes (PROM), onset time of symptoms, age at hospital admission, and history of infection exposure.
- Disease Diagnosis and Treatment Course: Infants suspected of having infectious diseases or confirmed enterovirus infections underwent lumbar puncture to determine whether there was concurrent intracranial infection. Enterovirus testing was performed on cerebrospinal fluid (CSF). Clinical manifestations involving the gastrointestinal and respiratory systems, as well as other symptoms, were recorded. The treatment process, including the use of vasoactive drugs, blood products, ventilatory support, and extracorporeal membrane oxygenation (ECMO), was documented.
- Laboratory and Imaging Examinations: Upon admission, laboratory tests included white blood cell count, hemoglobin, platelet count, high-sensitivity C-reactive protein (hs-CRP), liver and kidney function tests, blood gas and electrolyte analysis, creatine kinase-MB (CK-MB), cerebrospinal fluid (CSF) routine tests, CSF biochemical analysis, CSF culture, and imaging studies such as chest X-ray, electrocardiogram (ECG), echocardiography, abdominal ultrasound (liver, gallbladder, spleen, and pancreas), brain MRI, and electroencephalography (EEG).
- Clinical Outcomes:
① Death during hospitalization or shortly after discharge.
② Survival.
Enterovirus Pathogen Detection
RT-PCR method was used to test the feces, blood, or cerebrospinal fluid of the children. Feces, cerebrospinal fluid, or blood specimens were collected and mixed with 1 mL of 0.9% sodium chloride solution. RNA was extracted using an automated nucleic acid extractor (Zhejiang Biotech Co., Ltd., Shanghai, China). RT-PCR was performed using a detection kit (Zhejiang Biotech Co., Ltd., Shanghai, China) to detect enteroviruses. The RT-PCR was conducted in the ABIStepOnePlus system under the following conditions: 50°C for 15 minutes, 95°C for 5 minutes, 94°C for 15 seconds, and 55°C for 45 seconds, for 40 cycles. Samples with a Ct value less than 35.0 were identified as positive.
Statistical Analysis
Data analysis was performed using SPSS version 26.0. Quantitative data were expressed as mean ± standard deviation (±s) and analyzed using t-tests. Categorical data were expressed as percentages (%) and analyzed using chi-square (χ²) tests. A P value of <0.05 was considered statistically significant.
Results
Comparison of Clinical Characteristics of Neonatal Enterovirus Infections
As shown in Table 1, compared with the mild infection group, neonates in the severe infection group had a lower gestational age at birth and a higher proportion of preterm births (P < 0.05). There were no significant differences between the two groups in terms of gender or birth weight (P > 0.05).
 |
Table 1 Comparison of Clinical Characteristics of Neonatal Enterovirus Infections |
Infants in the severe infection group had an earlier onset of illness and a higher incidence of rash, respiratory symptoms, and sepsis-like manifestations such as reduced feeding, crying, and movement (P < 0.05). However, there was no significant difference in the incidence of vomiting and diarrhea between the two groups (P > 0.05).
The incidence of pneumonia, myocarditis, necrotizing hepatitis, and disseminated intravascular coagulation (DIC) was significantly higher in the severe infection group compared to the mild infection group (P < 0.05). The mortality rate in the severe infection group was 54.55%, which was significantly higher than that in the mild infection group (P < 0.05).
Comparison of Laboratory Tests Between the Mild Infection Group and the Severe Infection Group
For high-sensitivity C-reactive protein (hs-CRP) > 20 mg/L, 11 cases (7.38%) were observed in the mild infection group, while no cases (0%) were found in the severe infection group, with a statistically significant difference (P = 0.044).
For white blood cell count (WBC) > 15×109/L, the incidence was higher in the severe infection group (22.73%) compared to the mild infection group (10.74%), but the difference did not reach statistical significance (P = 0.071).
Thrombocytopenia (<100×109/L) was a major characteristic of the severe infection group, occurring in 84.09% of cases, whereas only 2.68% of cases in the mild infection group showed this condition, with an extremely significant difference (P < 0.001).
For prothrombin time (PT) prolongation > 30s, the incidence was 84.09% in the severe infection group, significantly higher than 2.01% in the mild infection group (P < 0.001).
The incidence of elevated CK-MB (>48 U/L) was 54.55% in the severe infection group, far exceeding 10.74% in the mild infection group, with a significant difference (P < 0.001).
Finally, ALT > 40 U/L was observed in 68.18% of cases in the severe infection group, compared to only 5.37% in the mild infection group, with a significant difference (P < 0.001).
These results suggest that the severe infection group exhibited significant abnormalities in multiple laboratory parameters, particularly in thrombocytopenia, PT prolongation, CK-MB elevation, and ALT elevation, indicating a more severe disease condition. See Table 2 for details.
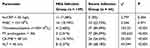 |
Table 2 Comparison of Laboratory Tests Between the Mild Infection Group and the Severe Infection Group |
Comparison of Treatment Methods, Complications, and Outcomes
The mild infection group primarily received non-invasive treatment, such as physical cooling and oral rehydration. Only 2 cases (1.4%) progressed to severe infection and required escalation to intensive care treatment. Compared to the severe infection group, the mild infection group did not require respiratory support, vasoactive drugs, or blood purification, and antibiotic selection was more conservative (ceftriaxone vs broad-spectrum combination antibiotics).
Regarding complications, the mild infection group mainly exhibited self-limiting symptoms (eg, diarrhea, rash) without leading to organ failure. In contrast, core complications of the severe infection group (MODS, necrotizing hepatitis) developed in only 1.4% of patients in the mild infection group, highlighting the importance of early identification and intervention in reducing the risk of disease progression.
In terms of clinical outcomes, the survival rate in the mild infection group was 100%, whereas only 45% of patients in the severe infection group survived, demonstrating the extremely high mortality rate associated with severe infection. Additionally, the incidence of long-term sequelae was very low in the mild infection group (only 2 cases with mild motor impairment), whereas 50% of survivors in the severe infection group required long-term neurological rehabilitation. See Tables 3 and 4.
 |
Table 3 Treatment Methods, Complications, and Clinical Outcomes in the Mild Infection Group (n=149) |
 |
Table 4 Complications, Treatment, and Clinical Outcomes in the Severe Infection Group (n=44) |
Discussion
Neonatal enterovirus (EV) infection is a significant threat to neonatal health, with highly heterogeneous clinical manifestations. While mild cases are self-limiting, severe cases can rapidly progress to multiple organ dysfunction syndrome (MODS) with a high mortality rate. This study retrospectively analyzed 193 cases of neonatal EV infection, identifying risk factors, pathological features, and prognostic differences in severe infections, providing valuable insights for early identification of high-risk neonates.
The study found that the average gestational age in the severe infection group (36.61 weeks) was significantly lower than in the mild infection group (38.50 weeks), with a higher proportion of preterm infants (15.9% vs 9.4%), consistent with the findings of Nouwen et al,12 who reported that “for each week of gestational age reduction, the risk of severe EV infection increases by 1.3 times.” Preterm infants have an immature immune system, with defects in both innate immune responses (eg, interferon secretion capacity) and adaptive immunity (T-cell function),13 leading to delayed viral clearance and increased susceptibility to systemic dissemination. Notably, 77.3% of severe cases presented within the first seven days of life, suggesting that perinatal vertical transmission or nosocomial infection may be the primary route of spread. Davila-Calderon et al14 found through maternal-neonatal paired sequencing that EV can be transmitted via the placenta or birth canal, and neonates with vertical transmission are more likely to develop liver failure (OR = 4.2), which corresponds with the 70.45% incidence of necrotizing hepatitis observed in the severe group in this study.
Additionally, laboratory analysis showed that 84.09% of the severe group had thrombocytopenia (<100×109/L), accompanied by prolonged PT (84.09%) and a high incidence of DIC (31.82%). This phenomenon may be related to EV’s direct attack on megakaryocytes and liver sinusoidal endothelial cells. Wu et al15 demonstrated in vitro that EV-A71 downregulates thrombopoietin receptor expression in megakaryocytes, inhibiting platelet production. Meanwhile, liver damage leads to decreased synthesis of coagulation factors (eg, II, VII, IX, X), forming a “dual-hit” effect. Interestingly, in this study, the proportion of patients with hs-CRP >20 mg/L was lower in the severe group than in the mild group (0% vs 7.38%). This finding aligns with the mechanism proposed by Harvala et al,16 suggesting that severe EV infection may suppress the IL-6 pathway, leading to an attenuated CRP response, which implies that CRP alone is not a reliable severity marker.
The proportion of severe cases with elevated CK-MB reached 54.55%, and 54.54% developed heart failure. EV invades myocardial cells via the SCARB2 receptor,17 triggering mitochondrial apoptosis. Animal models have shown that EV infection leads to a tenfold upregulation of TNF-α expression in myocardial cells, inducing contractile protein degradation and calcium dysregulation,18 which explains why 84.09% of severe cases required vasoactive drugs (dopamine/epinephrine). Additionally, 68.18% of severe cases had elevated ALT, with 70.45% developing necrotizing hepatitis. Autopsy studies have demonstrated that EV infection results in extensive eosinophilic necrosis and CD8+ T-cell infiltration in liver tissues,8 indicating that both direct viral cytopathic effects and cellular immune responses contribute to the pathology. In this study, nine surviving cases showed liver enzyme recovery after treatment with N-acetylcysteine, likely due to its ability to inhibit the NF-κB pathway and reduce oxidative stress damage.19 Although this study did not include specific encephalitis markers, 50% of the 20 surviving severe cases required neurological rehabilitation, suggesting that EV may cause subclinical neurological damage by disrupting the blood-brain barrier. Randolph et al20 found that EV68 infection upregulates matrix metalloproteinase-9 (MMP-9), which degrades the tight junction protein ZO-1, potentially explaining the delayed onset of motor impairments.
This study showed that mechanical ventilation (84.09%) and blood purification (20.45%) were significantly more common in the severe group, yet the mortality rate remained 54.55%. This finding is consistent with the multicenter study by Ikuse et al,21 which reported a mortality rate of 52.8%, highlighting the limitations of current supportive treatments. In recent years, the antiviral drug Pocapavir has demonstrated the ability to reduce viral loads by 2.5 log in Phase II clinical trials,22 but its safety in neonates remains unverified. Regarding coagulation dysfunction, this study set the platelet transfusion threshold at <50×109/L, but recent guidelines recommend maintaining PLT >80×109/L in cases of concurrent DIC,23 which may be an area for future improvement in prognosis.
This study has several limitations: (1) The single-center retrospective design may introduce selection bias. (2) Viral genotyping was not performed, despite different serotypes (eg, CV-A6, EV-A71) exhibiting varying pathogenicity. (3) The study lacks data on cytokine profiles and other mechanistic investigations. Future research should conduct multicenter prospective cohort studies incorporating metagenomic sequencing and immunological profiling to establish early warning models. Additionally, maternal vaccination (eg, EV-A71 vaccine) as a preventive measure against vertical transmission warrants further investigation.
Conclusion
Severe neonatal EV infection is closely associated with preterm birth and perinatal infection, characterized by thrombocytopenia, coagulation dysfunction, and multiple organ damage. Clinicians should enhance early monitoring of high-risk neonates, particularly preterm infants, and promptly initiate intensive care for those developing rashes or respiratory distress with a rapid decline in platelet counts within the first seven days of life. Further exploration of targeted antiviral therapies and immunomodulatory strategies is warranted.
Data Sharing Statement
All data generated or analysed during this study are included in this published article.
Disclosure
The authors declare that they have no competing interests.
References
1. Jubelt B, Lipton HL. Enterovirus/picornavirus infections. Handb Clin Neurol. 2014;123:379–416. doi:10.1016/B978-0-444-53488-0.00018-3
2. Xie Z, Khamrin P, Maneekarn N, et al. Epidemiology of enterovirus genotypes in association with human diseases. Viruses. 2024;16(7):1165. doi:10.3390/v16071165
3. Ang PY, Chong CWH, Alonso S. Viral determinants that drive Enterovirus-A71 fitness and virulence. Emerg Microbes Infect. 2021;10(1):713–724. doi:10.1080/22221751.2021.1906754
4. Huang HI, Shih SR. Neurotropic enterovirus infections in the central nervous system. Viruses. 2015;7(11):6051–6066. doi:10.3390/v7112920
5. Ho BC, Yang PC, Yu SL. MicroRNA and pathogenesis of enterovirus infection. Viruses. 2016;8(1):11. doi:10.3390/v8010011
6. Lukashev AN, Koroleva GA, Lashkevich VA, et al. [Enterovirus 71: epidemiology and diagnostics]. Zh Mikrobiol Epidemiol Immunobiol. 2009;3:110–116. Danish
7. Yoshida H. [Human enterovirus]. Nihon Rinsho. 2003;61(Suppl 3):463–467. Danish
8. Thibaut HJ, De Palma AM, Neyts J. Combating enterovirus replication: state-of-the-art on antiviral research. Biochem Pharmacol. 2012;83(2):185–192. doi:10.1016/j.bcp.2011.08.016
9. Pérez-Martínez Z, Álvarez-Argüelles ME, Rojo-Alba S, et al. Incidence of enterovirus in patients with acute gastroenteritis. Eur J Clin Microbiol Infect Dis. 2021;40(10):2185–2190. doi:10.1007/s10096-021-04275-6
10. Nguyen TT, Chiu C-H, Lin C-Y, et al. Efficacy, safety, and immunogenicity of an inactivated, adjuvanted enterovirus 71 vaccine in infants and children: a multiregion, double-blind, randomised, placebo-controlled, Phase 3 trial. Lancet. 2022;399(10336):1708–1717. doi:10.1016/S0140-6736(22)00313-0
11. Ho HY. Special issue “enteroviruses 2021”. Viruses. 2022;14(2).
12. Nouwen LV, Breeuwsma M, Zaal EA, et al. Modulation of nucleotide metabolism by picornaviruses. PLoS Pathog. 2024;20(3):e1012036. doi:10.1371/journal.ppat.1012036
13. Wang L, Wang J, Wang L, et al. Anti-enterovirus 71 agents of natural products. Molecules. 2015;20(9):16320–16333. doi:10.3390/molecules200916320
14. Davila-Calderon J, Li M-L, Penumutchu SR, et al. Enterovirus evolution reveals the mechanism of an RNA-targeted antiviral and determinants of viral replication. Sci Adv. 2024;10(7):eadg3060. doi:10.1126/sciadv.adg3060
15. Wu W, Li B, Xie T. Children with severe enterovirus A71 infection. BMC Pediatr. 2023;23(1):172. doi:10.1186/s12887-023-03980-9
16. Harvala H, Broberg E, Benschop K, et al. Recommendations for enterovirus diagnostics and characterisation within and beyond Europe. J Clin Virol. 2018;101:11–17. doi:10.1016/j.jcv.2018.01.008
17. Chuang YY, Huang YC. Enteroviral infection in neonates. J Microbiol Immunol Infect. 2019;52(6):851–857. doi:10.1016/j.jmii.2019.08.018
18. Singanayagam A, Moore C, Froude S, et al. Increased reports of severe myocarditis associated with enterovirus infection in neonates, United Kingdom, 27 June 2022 to 26 April 2023. Euro Surveill. 2023;28(39). doi:10.2807/1560-7917.ES.2023.28.39.2300313
19. Yang X, Duan L, Zhan W, et al. Enterovirus B types cause severe infection in infants aged 0–3 months. Virol J. 2023;20(1):5. doi:10.1186/s12985-023-01965-9
20. Randolph AG. Enterovirus D68 reemerges globally as a severe pathogen targeting children. Pediatr Crit Care Med. 2016;17(11):1088–1089. doi:10.1097/PCC.0000000000000961
21. Ikuse T, Aizawa Y, Kachikawa R, et al. Detection of enterovirus D68 among children with severe acute respiratory infection in Myanmar. J Microbiol Immunol Infect. 2024;57(2):238–245. doi:10.1016/j.jmii.2024.01.001
22. Novikov DV, Melentev DA. [Enteroviral (Picornaviridae: enterovirus) (nonpolio) vaccines]. Vopr Virusol. 2022;67(3):185–192. Bislama. doi:10.36233/0507-4088-111
23. Tomatis Souverbielle C, Erdem G, Sánchez PJ. Update on nonpolio enterovirus and parechovirus infections in neonates and young infants. Curr Opin Pediatr. 2023;35(3):380–389. doi:10.1097/MOP.0000000000001236
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

