Back to Journals » Journal of Pain Research » Volume 18
Analysis of Electroacupuncture Parameters for Irritable Bowel Syndrome: A Data Mining Approach
Received 12 August 2024
Accepted for publication 10 April 2025
Published 23 April 2025 Volume 2025:18 Pages 2175—2189
DOI https://doi.org/10.2147/JPR.S483750
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Houman Danesh
Yang Tang,1,* Xiao Tang,1,* Qiao Wen2
1Yongchuan Hospital of Traditional Chinese Medicine, Chongqing Medical University, Chongqing, People’s Republic of China; 2Acupuncture and Tuina School, Chongqing College of Traditional Chinese Medicine, Chongqing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qiao Wen, Acupuncture and Tuina School, Chongqing College of Traditional Chinese Medicine, No. 61 Puguobao Road, Bi Cheng Street, Bishan District, Chongqing, 402760, People’s Republic of China, Tel +8615528385250, Email [email protected]
Purpose: Irritable bowel syndrome (IBS), a prevalent functional bowel disorder, has increasingly seen acupuncture incorporated into its clinical management. Despite this, a comprehensive summary of electroacupuncture (EA) stimulation parameters and acupoint prescriptions tailored for IBS remains absent. This study endeavors to identify effective EA parameters for IBS through data mining methodologies.
Methods: To retrieve randomized controlled trials (RCTs) on EA for IBS published between 2013 and 2024, a comprehensive search was conducted across nine databases. EA parameters from eligible studies were extracted and evaluated for quality using the Cochrane’s risk of bias tool (RoB 2). Descriptive statistics were computed using MS-Excel®. Association rule analysis was undertaken in SPSS Modeler, whereas complex network analysis and co-occurrence network analyses were performed using Gephi and Origin, respectively.
Results: A total of 30 RCTs involving 2906 participants were included. All included studies exhibit a low to high risk of bias. Key methodologic weaknesses are mainly attributed to insufficient randomization and lack of blinding. The frequently reported EA stimulation parameters were a frequency of 2 hz, using either dilatational or continuous waves, with a treatment duration of 30 minutes, a 4-week course, and once daily treatment. Across 32 acupoint prescriptions, 27 acupoints were identified, with the stomach and bladder meridians being the most frequently targeted. Acupoints ST25, ST37, and ST36 were most frequently used. The most supported combination of acupoints could be (ST25→ST37); k-core hierarchical analysis of complex networks revealed the core acupoints for IBS treatment, including ST25, ST37, ST36, SP6, LR3, BL25, LI11 and RN4.
Conclusion: A regimen combining dilatational/continuous waves, 2 hz, a 30-minute stimulus, a 4-week course, and the acupoint combination (ST25→ST37) may serve as a primary EA protocol for IBS. However, methodological constraints may undermine the robustness of these findings. Therefore, the clinical application of these therapeutic modalities requires further validation.
Keywords: data mining, electroacupuncture stimulation parameters, acupoint selection rules, association rule analysis
Introduction
Irritable bowel syndrome (IBS) is a functional gastrointestinal disorder characterized by recurrent abdominal pain, discomfort, and alterations in bowel habits.1 As one of the most common medical disorders encountered by the healthcare system, it affects 11.2% of the general population.2 While not life-threatening, its chronic relapsing symptoms significantly increase healthcare costs and impair quality of life (QOL). It can be estimated that the QOL impairments of patients with IBS are comparable to those of patients with diabetes mellitus and end-stage renal disease.3 The limited efficacy of conventional medical treatments for IBS has prompted increasing interest in complementary therapies.
Acupuncture has been shown to have promising effects on IBS.4 The possible biological mechanisms underlying acupuncture for IBS include regulation of gastrointestinal dynamics, inhibition of visceral hypersensitivity, modulation of “gut-brain axis”, immune function and intestinal flora.5–7 As an improved variant of acupuncture approach, electroacupuncture (EA) as a combination of electrical stimulation and acupuncture has been widely used to treat IBS. Several clinical trials showed the efficacy and safety of EA in improving IBS symptoms and QOL.8,9 For example, Zhao et al found that a four-week EA regimen was effective in improving abdominal distension, defecation frequency, difficulty in defecation, and irregular stool features among IBS patients.10 Despite evidence for the efficacy of EA in IBS, there is currently a lack of research examining the main EA parameters for IBS. From the perspective of Traditional Chinese Medicine (TCM), selecting appropriate EA parameters is crucial for achieving satisfactory therapeutic effects. Therefore, research into EA parameters for IBS is required to identify effective EA protocols, which is conducive to optimizing future treatment strategies.
Data mining has emerged as a vital tool for extracting valuable insights from vast amounts of incomplete, noisy, fuzzy, and random practical application data, allowing researchers to uncover potentially useful information and knowledge that is difficult to detect manually.11 Structured databases (eg, clinical trial repositories, electronic health records), literature reviews, transactional records, and experimental datasets12,13 serve as common sources of evidence for data mining. Literature reviews, in particular, synthesize findings from published studies, enabling researchers to identify patterns, trends, and any emerging consensus within a field.14 Compared to database or individual participant data analysis — which rely on raw, granular data — literature reviews offer a cost-effective and time-efficient alternative for hypothesis generation and contextualization of findings. However, they are not devoid of limitations, such as publication bias or methodological heterogeneity in primary study designs.15 Data mining based on clinical data can identify potential EA parameters for efficient management of IBS, enabling precise clinical decision-making.
The object of this research was to summarize the stimulation parameters of EA and acupoint prescriptions for IBS using data mining techniques. It is hypothesized that mining of clinical EA intervention data pertaining to IBS will reveal critical parameter combinations (eg, stimulation frequency, duration, acupoint prescriptions) that correlate with improved symptom relief and QOL outcomes. These findings will furnish an evidence-based framework to optimize EA protocols.
Methods
Data Sources and Search Strategy
Nine electronic literature databases (PubMed, Cochrane Library, Embase, Web of Science, OVID, PubScholar, China National Knowledge Infrastructure, Chongqing VIP, and Wanfang) were scanned for studies on EA for IBS published between January 2013 and December 2024. Studies were restricted to those published in English and Chinese. The search strategy used subject terms related to acupuncture and IBS, such as electroacupuncture, electrical stimulation, and irritable bowel syndrome. The PubMed search strategy was as follows: ((Acupuncture [MeSH Terms]) OR (acupuncture therapy OR acupuncture treatment OR acupuncture treatments OR electroacupuncture OR electrical stimulation OR acupuncture, ear OR meridians OR acupunctur* OR acupoints)) AND ((Irritable Bowel Syndrome [MeSH Terms]) OR (irritable bowel syndromes OR mucous colitis OR mucous colitides OR syndrome, irritable bowel OR syndromes, irritable bowel OR irritable colon OR colitis, mucous OR colitides, mucous)). The search strategy was modified for each database.
Inclusion Criteria
Exclusion Criteria
Data Screening
Two independent investigators (TY, TX) screened studies against eligibility criteria. After removing duplicates, irrelevant studies through title/abstract screening were excluded. Then, full texts of remaining studies were retrieved and subjected to a further screening process to determine their eligibility. Any disagreements during the data screening process were resolved through discussions between the two investigators or in consultation with a third investigator (WQ).
Data Extraction and Quality Assessment
Microsoft Excel® 2016 software was used to create the database. One investigator (TY) extracted detailed information from all eligible studies, including the title, first author’s name, publication year, participant characteristics (including total number, gender, group allocation, and diagnostic standard), main outcomes, EA parameters (eg, current frequency, waveform, frequency of treatment, stimulation duration), and frequency of acupoint prescription. After data entry, another investigator (TX) proofread the data for accuracy. Cochrane’s risk of bias tool version 2 (RoB 2) was utilized for evaluating the risk of bias of included RCTs. The risk-of-bias judgments for each domain were categorized as “low risk of bias”, “some concerns”, or “high risk of bias”.22
Data Analysis
Descriptive statistics were calculated using MS-Excel® 2016. The Apriori algorithm in SPSS Modeler 18.0 was used for association rule analysis of EA stimulation parameters and acupoint prescriptions. Complex network analysis was conducted using Gephi 0.9.2. The co-occurrence network diagram of acupoints was generated using Origin 2021 software. The k-core hierarchical analysis algorithm was used to obtain the core degree of the nodes of EA stimulation parameters and acupoint prescriptions and identify the core combination of parameters for EA treatment of IBS.
Results
Eligible Studies
A total of 733 records were retrieved from the databases. Following the exclusion of 273 duplicates, the title and abstract of 460 studies were screened, resulting in the exclusion of 411 studies. Subsequently, 49 studies progressed to full-text screening, with an additional 19 studies being excluded due to non-compliance with inclusion criteria. Ultimately, 30 studies were included in the final analysis. The PRISMA flow diagram (Figure 1) provides a concise summary of the search and screening process.
 |
Figure 1 PRISMA flow diagram of literature search and screening process. Adapted from Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021; 372 :n71. Creative Commons.23 |
The risk-of-bias assessments categorized the included RCTs into three groups: low risk (3.33%), some concerns (63.3%), and high risk (33.3%). The high-risk categorization was primarily due to blinding of participants, whereas concerns were raised regarding incomplete outcome data, insufficient blinding of outcome assessment, and allocation concealment. These assessment results are depicted in Figures 2 and 3.
 |
Figure 2 Risk of bias graph. |
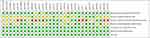 |
Figure 3 Risk of bias assessment. |
Study Characteristics
Among the 30 studies, 2906 participants were included. Concerning IBS subtypes, 70% (21 studies)9,10,24–42 concentrated on irritable bowel syndrome with diarrhea (IBS-D), 13.33% (4 studies)43–46 on irritable bowel syndrome with constipation (IBS-C), 6.67% (2 studies)47,48 on both IBS - C and IBS-D, 3.33% (1 study)49 on multiple subtypes, and 6.67% (2 studies)50,51 were unspecified. For diagnostic criteria, 76.67% (23 studies)9,10,24–35,43–45,47–50 used Rome III, 23.33% (7 studies)36–42,46,48,51 used Rome IV. Regarding gender, 86.67% (26 studies)24–36,38–46,49–51 included both genders, 6.67% (2 studies)37,48 included only females, and 10% (3 studies)9,10,47 were unspecified. The detailed characteristics of the studies are presented in Tables 1 and S1.
 |
Table 1 Study Characteristics |
EA Stimulation Parameters Analysis
EA Frequency
A total of 14 EA frequencies were reported in 24 studies, ranging from 1 to 100 hz. The most frequently used EA frequencies were 2 hz (25%), 20 hz (16.67%), 25 hz (8.33%), and 2/100 hz (8.33%). The results are shown in Figure 4A.
EA Waveforms
Three waveforms were identified in 26 studies, including dilatational wave (42.31%), continuous wave (38.46%), and intermittent wave (19.23%). The results are illustrated in Figure 4B.
Treatment Duration
A total of four treatment durations were documented in 30 studies, including 30 minutes (90%), 25 minutes (3.34%), 15 minutes (3.33%), and 60 minutes (3.33%). The results are depicted in Figure 4C.
Course of EA Therapy
A total of seven treatment frequencies were reported in 29 studies, ranging from 3 weeks to 12 weeks. The most common duration was 4 weeks (72.41%), followed by 6 weeks (6.90%), 3 weeks (6.90%), 10 weeks (3.45%),12 weeks (3.45%), 22 days (3.45%), and 30 days (3.45%). The results are illustrated in Figure 4D.
Frequency of Treatment
A total of six treatment frequencies were reported in 30 studies. The most frequently used treatment frequencies were once a day (60%), three times a week (20%), and twice a day (10%). The results are shown in Figure 4E.
Acupoint and Meridian Analysis
Frequency of Meridian Analysis
Nine meridians were identified across 32 acupoint prescriptions for EA treatment of IBS. The meridian distribution analysis showed that the stomach meridian was the most frequently used (61 times, 52.99%), followed by the bladder meridian (9 times, 7.69%), and the spleen meridian (8 times, 6.84%). The cumulative frequency of the top three meridian accounts for 67.52% of the total use. The results are summarized in Table 2.
 |
Table 2 Frequency of Meridian Application for IBS Treatment |
Frequency of Acupoint Analysis
Twenty-seven acupoints were documented across 32 acupoint prescriptions for EA treatment of IBS, with a total frequency of 117 times. The acupoints that have been used more than five times were ST25, ST37, ST36, SP6, LR3, and BL25. The cumulative frequency of the top five acupoints accounts for 66.65% of the total use. Specific point analysis found that the most commonly used specific points were the Front Mu point and the Lower He-Sea Points (Table 3).
 |
Table 3 Frequency of Acupoint Application for IBS Treatment (Top 5) |
Association Rule Analysis
Association Rule Analysis for EA Stimulation Parameters
For the EA parameters, a total of 11 association rules were generated using the Apriori algorithm. The minimum support level was set to 20, the minimum confidence level was set to 80, the maximum number of antecedents was two, and the maximum number of lift-hand sides was set to one. The top five combinations with the highest support were (Treatment duration = 30 min →Course of EA therapy = 4 weeks), (Treatment duration = 30 min→Frequency of treatment = Once a day), (Treatment duration = 30 min→Frequency of treatment = Once a day and Course of EA therapy = 4 weeks), (Treatment duration = 30 min→Frequency of treatment = Once a day and Subtypes = IBS-D), (Subtypes = IBS-D→Waveform = Dilatational wave) (Table 4).
 |
Table 4 Association Rule Analysis for EA Stimulation Parameters |
The further to explore the core EA parameters for IBS with EA, all EA parameters were selected to establish a k-core network. The results showed that the core EA parameters were dilatational/continuous waves, 2 hz, treatment duration of 30 minutes, course of 4 weeks, and frequency of treatment of once a day. The results are shown in Figure 5.
Association Rule Analysis for a Combination of Acupoints
For a combination of acupoints, a total of eight association rules were identified using the Apriori algorithm. The minimum support level was set to 20, the minimum confidence level was set to 80, and the maximum number of antecedents was two. The top five combinations with the highest support were (ST25→ST37), (ST25→ST36 and ST37), (ST37→ST36 and ST25), (ST36→SP6), (ST37→SP6) (Table 5). The compatibility diagram of acupoints used in EA treatment of IBS is shown in Figure 6. The k-core hierarchical analysis revealed the core acupoints selected for EA treatment of IBS were ST25, ST37, ST36, SP6, LR3, BL25, LI11 and RN4. The results are shown in Figure 7.
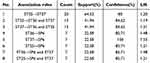 |
Table 5 Association Rule Analysis for a Combination of Acupoints |
 |
Figure 7 Diagram illustrating the k-core network of acupoints used in acupuncture treatment of IBS. |
Discussion
Currently, there are various EA parameters for the treatment of IBS with no uniform standard. This study identified the most frequently reported EA stimulation parameters and acupoint prescriptions of EA for IBS through multi-dimensional analysis. Furthermore, the rules covering combinations of core EA parameters were summarized to provide references for IBS treatment.
Selection of EA Stimulation Parameters
Our results indicated that the EA frequencies for treating IBS range from 1 to 100 hz, with 2 hz (25%), 20 hz (16.67%), 25 hz (8.33%), and 2/100 hz (8.33%) being most frequently reported in the included studies. Frequencies of 2 hz, 20 hz, and 100 hz were identified as the standard setting for low, medium, and high-frequency EA stimulus, respectively. EA-induced opioid peptide release is widely recognized as a crucial mechanism of EA analgesia.52 Different opioid receptors respond specifically to different EA frequencies. EA with a low frequency promotes the release of enkephalin. EA with a high frequency promotes the release of dynorphin. Medium-frequency EA may facilitate the simultaneous release of enkephalin, β-endorphin, and dynorphin.53,54 Moreover, a recent study has demonstrated that EA with different frequencies alleviates chronic visceral pain in IBS rats via divergent gut microbiota and metabolic pathways.55
The waveform emerges as a pivotal parameter in all electrical stimulations. The findings indicate that the dilatational wave is the most prevalent waveform reported. Characterized by alternating sparse and dense pulses, this waveform exhibits reduced adaptive responses when compared to continuous and intermittent waves. Furthermore, dilatational waves may enhance blood and lymphatic circulation, thereby modulating tissue nutritional metabolism.56 When selecting EA waveforms, consideration should be given to IBS subtypes and the underlying etiology of pain. For instance, continuous waveforms have been shown to enhance cerebral activation associated with pain modulation,57 whereas dilatational waves can decrease corticotropin-releasing factor levels, thus regulating gut-brain interactions.58 Clinical trials involving IBS patients demonstrated that waveform efficacy may differ according to symptom subtype. Specifically, dilatational waves have achieved symptom relief in patients with IBS-D by deducing visceral hypersensitivity,42 whereas intermittent waves have exhibited favorable outcomes in patients with IBS-C by enhancing colonic motility.43,46
The frequency of EA treatment for IBS, as reported in the included studies, most commonly involves once-daily sessions. Typically, the severity of symptoms dictates the frequency of treatment, with adjustments needed according to the disease stage. During acute exacerbations, daily sessions may offer swift relief of symptoms, whereas maintenance therapy twice weekly could help prevent recurrence during remission phases.29,59 A recent meta-analysis of acupuncture’s dose-effect in treating functional gastrointestinal disorders found more frequent (about 24) sessions led to optimal outcomes, especially for severe cases.60
With regard to treatment duration, our findings indicate that 30 minutes is the most prevalent duration used in those studies examined. Barlas et al found that, when compared to 20-minute or 40-minute EA stimulation, a 30-minute duration elicits the most significant analgesic effects in healthy individuals.61 Results from an animal experiment have further indicated that a 30-minute duration is significantly more effective than 10 - minute and 20 -minute durations in promoting the recovery of damaged colon mucosa.62 Consequently, an EA stimulus duration of approximately 30 minutes was recommended to ensure an analgesic effect. The overall therapeutic outcome was determined by the combination of multiple EA parameters, which may require individualization in clinical practice through an assessment of the IBS patient’s symptom type and severity.
Selection of Acupoint and Meridian
Acupoint compatibility is one of the important factors considered in achieving ideal therapeutic effects of acupuncture. The frequency of acupoint analysis revealed that ST25, ST37, ST36, SP6, LR3, and BL25 were the high-frequency acupoints for acupuncture treatment of IBS. Notably, these acupoints focus on the stomach meridian, spleen meridian, liver meridian, and bladder meridian. Based on Zangfu-meridian theory, these acupoints belong or are related to the gastrointestinal tract.
The association rule analysis of acupoint combinations implied that the pairing (ST25→ST37) exhibits the highest support. In the context of TCM, both ST25 and ST37 are affiliated with the stomach meridian. Specifically, ST25, situated in the abdomen, serves as the Front Mu point of the large intestine, whereas ST37, positioned in the lower leg, functions as the Lower He-Sea point of the same meridian. The synergistic integration of these two acupoints holds promise for effectively regulating intestinal function. Anatomically, the innervation territories of ST25 and ST37 overlap with those of the spinal nerve segments innervating the gastrointestinal tract. EA stimulation at these points was found to upregulate the occludin expression, ameliorate visceral hypersensitivity, and modulate P2X3 receptors in the colon and associated dorsal root ganglia of rats with IBS exhibiting visceral pain.63 Furthermore, EA applications at ST25 and ST37 enhance gut motility and butyrate production in mouse models of constipation.64 Complex network analysis indicated a focus on abdominal local acupoints, emphasizing the combination of distant-local acupoints and Shu-Mu acupoints. The selection of acupoints follows meridian theory, clinical experience, and consensus among experts in acupuncture and IBS. The core acupoints identified — ST25, ST37, ST36, SP6, LR3, BL25, LI11 and RN4 — may serve as a potential basis for acupuncture prescriptions in IBS treatment, pending further clinical validation.
The limitations of this study can be outlined as follows. Firstly, the methodological quality of the incorporated studies may have affected the reliability of the findings. Discrepancies in outcome measurement methodologies and incomplete documentation of EA parameters, such as waveform specifics and stimulation intensity, hindered the standardization of the data. It is advisable for future clinical trials to adhere strictly to reporting guidelines.65,66 Secondly, potential heterogeneity within the data mining process — encompassing variations in the interpretation of parameter definitions (for instance, the term “dilatational wave” being interpreted differently across studies) and the presence of confounding factors (such as concurrent therapies) — could undermine the generalizability of the identified parameter combinations. Thirdly, the restricted number of studies included rendered subgroup analyses for IBS subtypes. Lastly, the underlying mechanism responsible for the synergies observed among EA parameters remains elusive, thereby necessitating further mechanistic investigations.
Conclusion
An EA frequency of 20 hz, employing dilatational waves or continuous wave, with a treatment duration of 30 minutes, course of 4 weeks, and a treatment frequency of once daily, has been commonly applied in the management of IBS. Acupoints ST25, ST37, ST36, SP6, LR3, BL25, LI11 and RN4 can be regarded as pivotal selections for future clinical applications. Although this study provides clarity on parameter selection, the limitations inherent in the trial design — such as inadequate randomization and insufficient blinding of participants — underscore the imperative for large-scale, multicenter RCTs to corroborate the findings and refine IBS therapy.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work is supported by grants from the National Natural Science Foundation of China (No. 82405571), the Chongqing Natural Science Foundation Project (No. CSTB2023NSCQ-BHX0058) and Chongqing Science, Technology Bureau and Health Commission Joint Medical Research Project (No. 2023QNXM053), and the Science and Technology Research Program of Chongqing Municipal Education Commission (No. KJ QN202315132).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chey WD, Kurlander J, Eswaran S. Irritable bowel syndrome: a clinical review. JAMA. 2015;313(9):949–958. doi:10.1001/jama.2015.0954
2. Enck P, Aziz Q, Barbara G, et al. Irritable bowel syndrome. Nat Rev Dis Primers. 2016;2:16014. doi:10.1038/nrdp.2016.14
3. Mönnikes H. Quality of life in patients with irritable bowel syndrome. J Clin Gastroenterol. 2011;45 Suppl:S98–101. doi:10.1097/MCG.0b013e31821fbf44
4. Qi L-Y, Yang J-W, Yan S-Y, et al. Acupuncture for the treatment of diarrhea-predominant irritable bowel syndrome: a pilot randomized clinical trial. JAMA Network Open. 2022;5(12):e2248817–e2248817. doi:10.1001/jamanetworkopen.2022.48817
5. Zhang G, Zhang T, Cao Z, et al. Effects and mechanisms of acupuncture on diarrhea-predominant irritable bowel syndrome: a systematic review. Front Neurosci. 2022;16:918701. doi:10.3389/fnins.2022.918701
6. Yue-ying M, Zhou H, Zi-yi C, et al. Acupuncture and moxibustion for irritable bowel syndrome: an umbrella systematic review. J Integr Med. 2024;22(1):22–31. doi:10.1016/j.joim.2023.12.001
7. Zhang B, Shi H, Cao S, et al. Revealing the magic of acupuncture based on biological mechanisms: a literature review. Biosci Trends. 2022;16(1):73–90. doi:10.5582/bst.2022.01039
8. Ma YY, Hao Z, Chen ZY, et al. Acupuncture and moxibustion for irritable bowel syndrome: an umbrella systematic review. J Integr Med. 2024;22(1):22–31. doi:10.1016/j.joim.2023.12.001
9. Zhao JM, Lu JH, Yin XJ, et al. Comparison of electroacupuncture and moxibustion on brain-gut function in patients with diarrhea-predominant irritable bowel syndrome: a randomized controlled trial. Chin J Integr Med. 2015;21(11):855–865. doi:10.1007/s11655-015-2049-x
10. Zhao JM, Lu JH, Yin XJ, et al. Comparison of electroacupuncture and mild-warm moxibustion on brain-gut function in patients with constipation-predominant irritable bowel syndrome: a randomized controlled trial. Chin J Integr Med. 2018;24(5):328–335. doi:10.1007/s11655-018-2838-0
11. Hemlata S, Shalini S, Seema G. A brief overview on data mining survey. 2011; Available from: https://api.semanticscholar.org/CorpusID:40682865.
12. Han J, Kamber M, Pei J. Data mining: concepts and techniques. Third Edition. 2011.
13. Sim I. Mobile devices and health. N Engl J Med. 2019;381(10):956–968. doi:10.1056/NEJMra1806949
14. Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91–108. doi:10.1111/j.1471-1842.2009.00848.x
15. Riley RD, Lambert PC, Abo-Zaid G. Meta-analysis of individual participant data: rationale, conduct, and reporting. BMJ. 2010;340(feb05 1):c221. doi:10.1136/bmj.c221
16. Drossman DA. The functional gastrointestinal disorders and the Rome II process. Gut. 1999;45(Suppl 2):Ii1–5. doi:10.1136/gut.45.2008.ii1
17. Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006;130(5):1377–1390. doi:10.1053/j.gastro.2006.03.008
18. Drossman DA, Hasler WL. Rome IV-functional GI disorders: disorders of gut-brain interaction. Gastroenterology. 2016;150(6):1257–1261. doi:10.1053/j.gastro.2016.03.035
19. Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monito ring irritable bowel syndrome and its progress. Aliment. Pharmacol. Ther. 1997;11(2):395–402. doi:10.1046/j.1365-2036.1997.142318000.x
20. Patrick DL, Drossman DA, Frederick IO, DiCesare J, Puder KL. Quality of life in persons with irritable bowel syndrome: development and validation of a new measure. Dig Dis Sci. 1998;43(2):400–411. doi:10.1023/a:1018831127942
21. Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997;32(9):920–924. doi:10.3109/00365529709011203
22. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;
23. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
24. Wu Y, Gao J. Clinical study of acupuncture therapy for diarrhea-predominant irritable bowel syndrome in 30 patients. J External Ther Traditional Chin Med. 2013;22(05):38–39.
25. Li H, Pei L, Zhou J, J-h S. Controlled observation on the efficacy of acupuncture and western medicine on diarrhea-type irritable bowel syndrome. World J Acupuncture - Moxibustion. 2013;23(2):11–16. doi:10.1016/S1003-5257(13)60037-9
26. Shi X, Li X, Liu L, et al. Ziwu Liuzhu acupuncture treatment of irritable bowel syndrome. Shaanxi J Traditional Chin Med. 2015;36(11):1516–1518.
27. Cui B. Clinical Curative Effect Observation on Treatment of Diarrhea Type Irritable Bowel Syndrome (Liver Stagnation and Spleen Deficiency)For Electroacupuncture Combined With Regulation of Mental Therapy [Dissertation]. Heilongjiang University of Chinese Medicine; 2015.
28. Wang W, Cui B. Clinical observation of invigorating the spleen and regulating the acupuncture for treating diarrhea type irritable bowel syndrome with electroacupuncture. HEILONGJIANG Medl J. 2015;39(04):405–406.
29. Zheng H, Li Y, Zhang W, et al. Electroacupuncture for patients with diarrhea-predominant irritable bowel syndrome or functional diarrhea: a randomized controlled trial. Medicine (Baltimore). 2016;95(24):e3884. doi:10.1097/md.0000000000003884
30. Zhong F, Cao Y, Luo R, et al. Clinical evaluation of electroacupuncture at the lower he-points and he-points for diarrhea-predominant irritable bowel syndrome. J Anhui Univ Chin Med. 2018;37(02):68–71.
31. Zhang G. The Clinical Research of Electro-Acupuncture With Warm Needling Method on Treating IBS-D [Dissertation]. Guangzhou University of Chinese Medicine; 2018.
32. Zhang C, Guo L, Wang Y, Zhang L, Chang T. Electroacupuncture combined with qibei mixture for diarrhea-predominant irritable bowel syndrome: a randomized controlled trial. World J Acupuncture - Moxibustion. 2018;28(1):19–24. doi:10.1016/j.wjam.2018.03.002
33. Zhong F, Cao Y, Luo R, et al. Clinical effect of electroacupuncture at He-Mu acupoint combination in treatment of diarrhea-predominant irritable bowel syndrome. J Hunan Univ Chin Med. 2018;38(04):435–438.
34. Mak AD-P, Chung VCH, Yuen SY, et al. Noneffectiveness of electroacupuncture for comorbid generalized anxiety disorder and irritable bowel syndrome. J Gastroenterol Hepatol. 2019;34(10):1736–1742. doi:10.1111/jgh.14667
35. Wu D, Peng T, Rong P, et al. Clinical effects of concha auriculae electroacupuncture in the treatment of diarrhea irritable bowel syndrome. World J Traditional Chin Med. 2021;16(11):1721–1725.
36. Hu P, Sun K, Li H, et al. Transcutaneous electrical acustimulation improved the quality of life in patients with diarrhea-irritable bowel syndrome. Neuromodulation. 2022;25(8):1165–1172. doi:10.1016/j.neurom.2021.10.009
37. Li G, Ma J, Wu H, et al. Clinical efficacy of acupuncture and moxibustion in treatment of female patients with IBS-D and the regulatory effect on serum MDA and T-AOC. World J Traditional Chin Med. 2022;17(03):344–348.
38. Sun Y, Wang S, Yu T, et al. Tiaoshen acupuncture method combined with electroacupuncture for diarrhea-type irritable bowel syndrome: a randomized controlled trial. Chin Acupuncture & Moxibustion. 2021;41(01):13–16. doi:10.13703/j.0255-2930.20191220-k0001
39. Chen X, Tang M, Wu H, et al. Clinical study on electro-acupuncture at auricular vagus nerve for diarrhea-predominant irritable bowel syndrome. J New Chin Med. 2022;54(08):184–187. doi:10.13457/j.cnki.jncm.2022.08.043
40. Feng W. Clinical Study on Spirit-Regulating Acupuncture With Electroacupuncture in the Treatment of Irritable Bowel Syndrome [Dissertation]. Guangzhou University of Chinese Medicine; 2022.
41. Zhang X. Clinical Effect Observation of Electroacupuncture in the Treatment of Diarrhea-Predominant Irritable Bowel Syndrome [Dissertation]. Tianjin University of Traditional Chinese Medicine; 2022.
42. Zhan D, Liu J, Xu Y, et al. Observation on the efficacy of Tiao Shen Jian Pi acupuncture combined with electroacupuncture in the treatment of irritable bowel syndrome-diarrheal and its effect on mast cell activation. Shanghai J Acupuncture Moxibustion. 2024;43(06):594–598. doi:10.13460/j.issn.1005-0957.2024.06.0594
43. Peng S, Yang J, Shi T, et al. Clinical evaluation of electroacupuncture therapy for constipation-predominant irritable bowel syndrome. Chin J Integrated Tradition Western Med Digestion. 2013;21(08):426–428.
44. Pei L, Zhu L, Sun J, et al. Constipation predominant irritable bowel syndrome treated with acupuncture for regulating the mind and strengthening the spleen: a randomized controlled trial. Chin Acupuncture & Moxibustion. 2015;35(11):1095–1098. doi:10.13703/j.0255-2930.2015.11.003
45. Mao W. Observation on Electroacupuncture in the Treatment ofIrritable Bowel Syndrome With Predominant Constipation [Dissertation]. Hubei University of Chinese Medicine; 2018.
46. Huang Z, Lin Z, Lin C, et al. Transcutaneous electrical acustimulation improves irritable bowel syndrome with constipation by accelerating colon transit and reducing rectal sensation using autonomic mechanisms. Am J Gastroenterol. 2022;117(9):1491–1501. doi:10.14309/ajg.0000000000001882
47. Lu Z, Yin X, Teng W, et al. Comparative effect of electroacupuncture and moxibustion on the expression of substance P and vasoactive intestinal peptide in patients with irritable bowel syndrome. J Tradit Chin Med. 2015;35(4):402–410. doi:10.1016/s0254-6272(15)30116-3
48. Chen X. The Clinical Study on Treatment of Abdominal Pain Symptoms of Irritable Bowel Syndrome by Electroacupuncture at Local Point or Remote Point [Dissertation]. Guangzhou University of Chinese Medicine; 2016.
49. Shi Y, Chen YH, Yin XJ, et al. Electroacupuncture versus Moxibustion for Irritable Bowel Syndrome: a Randomized, Parallel-Controlled Trial. Evid Based Complement Alternat Med. 2015;2015:361786. doi:10.1155/2015/361786
50. Sun YZ, Song J. Therapeutic observation of acupuncture at Jiaji (EX-B2) for irritable bowel syndrome. Journal Article Shanghai Journal of Acupuncture and Moxibustion [Shang Hai Zhen Jiu Za Zhi]. 2015;34(9):856–857.
51. Yang L, Wang X, Li B, et al. Effect of acupuncture on the acupoint pain threshold in patients with irritable bowel syndrome. Shanghai J Acupuncture Moxibustion. 2018;37(09):1030–1036. doi:10.13460/j.issn.1005-0957.2018.09.1030
52. Wang Q, Li Z, Nie D, et al. Low-frequency electroacupuncture exerts antinociceptive effects through activation of POMC neural circuit induced endorphinergic input to the periaqueductal gray from the arcuate nucleus. Mol Pain. 2024;20:17448069241254201. doi:10.1177/17448069241254201
53. Han JS. Acupuncture: neuropeptide release produced by electrical stimulation of different frequencies. Trends Neurosci. 2003;26(1):17–22. doi:10.1016/s0166-2236(02)00006-1
54. Chen P, Xu H, Zhang R, et al. Dose-effect relationship between electroacupuncture with different parameters and the regulation of endogenous opioid peptide system. World J Acupuncture-Moxibustion. 2024;34(01):9–15.
55. Chang X, Wang L, Sun H, Wang Z, Yang Z, Chen S. Electroacupuncture at different frequencies improves visceral pain in IBS rats through different pathways. Neurogastroenterol Motil. 2024;36(10):e14874. doi:10.1111/nmo.14874
56. Liang Y, Zhou J, Sun J, et al. The dose-effect relationship of electroacupuncture analgesia and its stimulus parameters: progress in the last 3 decades. World J Acupuncture-Moxibustion. 2023;33(01):12–19. doi:10.1016/j.wjam.2022.12.001
57. Chu WC, Wu JC, Yew DT, et al. Does acupuncture therapy alter activation of neural pathway for pain perception in irritable bowel syndrome?: a comparative study of true and sham acupuncture using functional magnetic resonance imaging. J Neurogastroenterol Motil. 2012;18(3):305–316. doi:10.5056/jnm.2012.18.3.305
58. Chen Y, Zhao Y, Luo DN, Zheng H, Li Y, Zhou SY. Electroacupuncture regulates disorders of gut-brain interaction by decreasing corticotropin-releasing factor in a rat model of IBS. Gastroenterol Res Pract. 2019;2019:1759842. doi:10.1155/2019/1759842
59. Liu Z, Yan S, Wu J, et al. Acupuncture for chronic severe functional constipation: a randomized trial. Ann Intern Med. 2016;165(11):761–769. doi:10.7326/m15-3118
60. Gong S, Yu X, Yang J, Huang D, Yu S, Yang S. The dose-effect relationship of acupuncture in the treatment of functional gastrointestinal disorders: a meta-regression of randomized controlled trials. Eur J Int Med. 2024;71:102406. EarlyAccessDate = OCT 2024, Article-Number = 102406.doi:10.1016/j.eujim.2024.102406
61. Barlas P, Ting SL, Chesterton LS, Jones PW, Sim J. Effects of intensity of electroacupuncture upon experimental pain in healthy human volunteers: a randomized, double-blind, placebo-controlled study. Pain. 2006;122(1–2):81–89. doi:10.1016/j.pain.2006.01.012
62. Yan L, Ji L, Qi C, et al. Study on optimum acupuncture parameter for “changbingfang” by orthogonal design. Chin J Basic Med Traditional Chin Med. 2015;21(01):80–82. doi:10.19945/j.cnki.issn.1006-3250.2015.01.035
63. Zhang F, Ma Z, Weng Z, et al. P2X(3) receptor in primary afferent neurons mediates the relief of visceral hypersensitivity by electroacupuncture in an irritable bowel syndrome rat model. Gastroenterol Res Pract. 2020;2020:8186106. doi:10.1155/2020/8186106
64. Xu MM, Guo Y, Chen Y, Zhang W, Wang L, Li Y. Electro-acupuncture promotes gut motility and alleviates functional constipation by regulating gut microbiota and increasing butyric acid generation in mice. J Integr Med. 2023;21(4):397–406. doi:10.1016/j.joim.2023.05.003
65. Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 Explanation and Elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;
66. MacPherson H, Altman DG, Hammerschlag R, et al. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. Acupunct Med. 2010;28(2):83–93. doi:10.1136/aim.2009.001370
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




