Back to Journals » Infection and Drug Resistance » Volume 18
Analysis of Hospital-Acquired Infections in a Chinese Specialized Rehabilitation Hospital: A Five-Year Surveillance Study (2020-2024)
Received 6 January 2025
Accepted for publication 18 April 2025
Published 7 May 2025 Volume 2025:18 Pages 2377—2388
DOI https://doi.org/10.2147/IDR.S516013
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Oliver Planz
Qianfeng Li,1 Dong Wang,1 Hanyuan Fan2
1Department of Geriatric Rehabilitation, Shenzhen Dapeng New District Nan’ao People’s Hospital, Shenzhen, People’s Republic of China; 2Hospital-Acquired Infection Control department, Shenzhen Dapeng New District Nan’ao People’s Hospital, Shenzhen, People’s Republic of China
Correspondence: Hanyuan Fan, Hospital-acquired infection control department, Shenzhen Dapeng New District Nan’ao People’s Hospital, No. 6 Renmin Road, Nanao Street, Dapeng New District, Shenzhen, 518100, People’s Republic of China, Tel +86-13760331505, Email [email protected]
Objective: Hospital-acquired infections (HAIs) pose significant challenges in rehabilitation hospitals, particularly affecting patients with extended stays and complex medical needs. This study analyzed HAI patterns and risk factors in a Chinese rehabilitation hospital from 2020 to 2024.
Methods: A retrospective observational study was conducted at a tertiary-care rehabilitation hospital with 25 specialized wards. Data collection included patient demographics, clinical parameters, and ward-level characteristics. Statistical analysis employed Poisson and Quasi-Poisson regression models to identify risk factors, with comprehensive diagnostic evaluation.
Results: The study revealed an overall infection rate of 3.64%, representing 385 infections among 10,559 inpatients. The Vegetative State Awakening Department exhibited the highest infection rate at 11.1%, followed by Geriatric Rehabilitation Department (8.2%), and Neuro Rehabilitation Department wards (5.5– 7.0%). Respiratory tract infections were most common (42%), with ventilator-associated pneumonia accounting for 28% of all infections. Statistical analysis identified several significant risk factors through both Poisson and Quasi-Poisson regression models. In the more reliable Quasi-Poisson model that accounted for overdispersion, tracheal intubation emerged as the strongest predictor with a coefficient of 2.02 (p < 0.001), followed by use of glucocorticoids (coefficient: 1.78, p < 0.001). While the initial Poisson model suggested a protective effect of radiation therapy, this effect was not significant in the Quasi-Poisson model.
Conclusion: The study highlights the critical role of tracheal intubation and glucocorticoid use in HAI development within rehabilitation settings. The significant ward-level variability in infection rates suggests the need for tailored infection control strategies. Implementation of targeted interventions focusing on these identified risk factors could help reduce HAI incidence in rehabilitation hospitals.
Keywords: hospital-acquired infections, rehabilitation hospital, risk factors, infection control, healthcare surveillance, China, nosocomial infections, patient safety
Introduction
Hospital-acquired infections (HAIs), also known as nosocomial infections, represent a significant and persistent challenge to patient safety and public health worldwide. These infections occur in patients during the course of receiving healthcare treatment for other conditions and are neither present nor incubating at the time of admission.1 HAIs are associated with increased morbidity and mortality, prolonged hospital stays, and substantial economic burdens on healthcare systems.2,3 Common types of HAIs include bloodstream infections, urinary tract infections, surgical site infections, and pneumonia, each contributing uniquely to patient outcomes and healthcare costs.4 Rehabilitation hospitals, which specialize in restoring patients’ functional abilities following acute medical events such as strokes, spinal cord injuries, and major surgeries, are particularly susceptible to HAIs.5 The nature of rehabilitation care often involves prolonged patient stays, frequent use of medical devices, and intensive physical therapy, all of which can elevate the risk of infection.6 Additionally, patients in rehabilitation settings may have compromised immune systems, advanced age, or underlying chronic conditions, further increasing their vulnerability to infections.7
Effective surveillance and monitoring of HAIs are crucial for implementing timely infection control measures and improving patient outcomes.8 Surveillance systems enable healthcare providers to identify infection trends, evaluate the effectiveness of preventive strategies, and allocate resources efficiently.9 Despite advancements in infection control practices, the incidence of HAIs remains a persistent issue, underscoring the need for continuous monitoring and research.10 This is especially pertinent in specialized settings like rehabilitation hospitals, where the unique patient population and treatment modalities may influence infection dynamics differently compared to general medical wards.11 Several studies have explored the epidemiology of HAIs in various healthcare settings, highlighting key risk factors such as the use of invasive devices, antibiotic resistance, and inadequate hand hygiene.12,13 However, there is a paucity of research focusing specifically on HAIs within rehabilitation hospitals in China, a country with a rapidly expanding healthcare infrastructure and a growing population of elderly patients.14 The unique challenges faced by Chinese rehabilitation hospitals, including resource constraints, varying levels of infection control practices, and diverse patient demographics, necessitate targeted studies to understand and mitigate HAIs effectively.15
Understanding the specific risk factors and infection patterns in Chinese rehabilitation hospitals is essential for developing tailored infection control strategies that address the unique needs of this setting.16 Factors such as the high prevalence of chronic diseases, the intensive use of medical devices, and the extended duration of patient stays in rehabilitation wards may contribute differently to the incidence of HAIs compared to other hospital settings.17 Additionally, cultural and systemic factors within Chinese healthcare facilities, including compliance with infection control protocols and the availability of antimicrobial stewardship programs, play a critical role in shaping infection outcomes.18 This study aims to bridge the existing research gap by conducting a comprehensive analysis of HAIs in a specialized rehabilitation hospital in China from 2020 to 2024. By examining infection rates across different wards and identifying associated risk factors, the research seeks to provide valuable insights into infection dynamics within rehabilitation settings. The findings are expected to inform the development of effective infection control strategies, ultimately enhancing patient safety and care quality in rehabilitation hospitals. Moreover, this study will contribute to the broader understanding of HAIs in specialized healthcare settings, offering evidence-based recommendations that can be generalized to similar contexts both within and beyond China.
Methods
Study Design and Setting
This retrospective observational study was conducted at a specialized rehabilitation hospital in China from January 1, 2020, to December 31, 2024. The hospital is a tertiary-care facility comprising 25 distinct specialized wards, each serving different patient populations and medical needs, with approximately 10,000 inpatients annually. The investigation was designed to leverage existing hospital records to provide comprehensive insights into infection patterns and inform the development of targeted infection control strategies within the rehabilitation setting. The study protocol received approval from the hospital’s Institutional Review Board, and written informed consent was waived due to the retrospective nature of the study and the use of anonymized data in accordance with the Declaration of Helsinki and local regulatory requirements.
Data Collection and Surveillance System
Healthcare-associated infection (HAI) surveillance was conducted according to the National Healthcare Safety Network (NHSN) definitions and criteria through the hospital’s infection surveillance system. A team of six trained infection control practitioners implemented a comprehensive daily monitoring process. The surveillance protocol included systematic reviews of electronic medical records, laboratory results, clinical documentation, regular ward rounds, and direct communication with clinical staff. All suspected infection cases underwent a standardized verification process requiring independent confirmation by two senior infection control specialists with over ten years of experience in healthcare epidemiology.
Clinical and Ward-Level Data Collection
Clinical risk factors were thoroughly documented through a structured protocol developed specifically for this study. The protocol encompassed comprehensive assessment of patient characteristics including demographics, clinical parameters, and potential risk factors for healthcare-associated infections. Demographic data included age (with particular attention to patients over 70 years), gender, and admission source. Clinical characteristics comprised immunological status, mobility conditions, nutritional states (assessed through serum albumin levels, with malnutrition defined as albumin <30 g/L), and the presence of comorbidities such as diabetes. Medical intervention data included surgical procedures within 30 days of admission, mechanical ventilation usage, tracheal intubation, glucocorticoid administration, and radiation therapy protocols. The surveillance system also tracked medical devices including urinary catheters, nasogastric tubes, tracheostomies, and central venous catheters, documenting their duration of use and associated complications. Ward-level data included standardized measures of care level, staff-to-patient ratios, availability of specialized equipment, and complexity of care provided. These characteristics were systematically documented to account for potential ward-specific risk factors that might influence infection rates. Clinical characteristics comprised immunological status, mobility conditions, nutritional states (assessed through serum albumin levels, with malnutrition defined as albumin <30 g/L). Serum albumin was chosen due to its wide - spread use and availability in clinical practice. However, we acknowledge the value of GNRI and G - 8 score in nutritional assessment and will consider incorporating them in future studies.
Statistical Analysis
Statistical analyses were performed using advanced statistical software supporting comprehensive data analysis and modeling capabilities. The analytical approach consisted of several interconnected components designed to examine infection patterns and their associated risk factors systematically. Initial analysis focused on assessing multicollinearity among potential risk factors using Pearson’s correlation coefficients. Variables demonstrating correlation coefficients exceeding 0.8 were identified for potential removal. A systematic variable selection process was implemented to address multicollinearity while maintaining maximum information content. This process resulted in the retention of five key predictors: Surgery, Use of Ventilator, Tracheal Intubation, Use of Glucocorticoids, and Radiation Therapy. The modeling approach employed a hierarchical strategy beginning with a Poisson regression model to examine relationships between new infections and selected risk factors. The model’s goodness-of-fit was evaluated through deviance and Pearson chi-square statistics. Detection of overdispersion (dispersion parameter = 17.88) led to the implementation of a Quasi-Poisson regression model to account for extra-Poisson variation while maintaining the same mean structure but with adjusted variance. Model refinement utilized stepwise selection procedures based on the Akaike Information Criterion (AIC). This process involved iterative evaluation of predictor contributions to model fit, with variables retained based on both statistical significance (p < 0.05) and clinical relevance. The stability of the selected model was assessed through bootstrap resampling with 1000 iterations. Comprehensive model diagnostics included examination of residual patterns, assessment of influential observations using Cook’s distance (threshold: 0.21), and evaluation of model assumptions. Residual analysis examined patterns versus fitted values to assess linearity and homoscedasticity. Scale-location plots evaluated the consistency of residual variance, while normal probability plots assessed residual distribution patterns. The analysis of influential observations identified points with potential disproportionate impact on model parameters. Effect sizes for significant predictors were estimated using incidence rate ratios (IRR) with 95% confidence intervals. For the Quasi-Poisson model, robust standard errors were calculated to account for overdispersion. All statistical tests were conducted as two-sided procedures with a significance level of 0.05. To address potential concerns about multiple testing in our stepwise selection process, we used AIC as the selection criterion, which penalizes model complexity and helps mitigate false positive findings. Additionally, we conducted sensitivity analyses using logistic regression to confirm the consistency of identified risk factors.
Results
Overall Infection Rate and Ward Distribution
Over the five-year period from 2020 to 2024, the specialized rehabilitation hospital in China recorded 385 new infections among 10,559 inpatients, resulting in an overall infection rate of 3.64%. Among the 385 infections recorded, respiratory tract infections were most common (42%), with ventilator-associated pneumonia (VAP) accounting for 28% of all infections. Urinary tract infections (26%), bloodstream infections (18%), and other infection types (14%) comprised the remainder. Infection rates exhibited substantial variability across different hospital wards. The Vegetative State Awakening Department had the highest infection rate at 11.1%, while several specialized units reported 0% infection rates. This distribution is visually depicted in Figure 1. The distribution of pathogens isolated from HAIs is presented in Table 1. Gram-negative bacteria were the predominant pathogens (53.5%), with Pseudomonas aeruginosa (19.0%) being the most common, followed by Escherichia coli (15.3%) and Klebsiella pneumoniae (11.7%). Among Gram-positive bacteria (37.7%), Staphylococcus aureus was the most frequently isolated (17.7%). Fungal pathogens, primarily Candida species, accounted for 8.9% of the isolates. The distribution of pathogens varied by infection site, with P. aeruginosa and S. aureus predominating in respiratory infections, E. coli in urinary tract infections, and coagulase-negative staphylococci and Candida species in bloodstream infections.
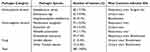 |
Table 1 Distribution of Pathogens Isolated from Hospital-Acquired Infections |
Risk Factor Analysis
Correlation Analysis and Multicollinearity Assessment
Pearson’s correlation analysis revealed exceptionally high correlations among several risk factors, indicating severe multicollinearity within the dataset (Figure 2). Variables such as Immunocompromised Status, Bedridden Condition, Age Over 70, Malnutrition, and Diabetes exhibited correlation coefficients exceeding 0.8, suggesting redundant information that could distort regression estimates. To address this, the caret package’s findCorrelation function was employed, resulting in the exclusion of 14 out of 19 initial risk factors. The final set of predictors retained for model development included Surgery, Use of Ventilator, Tracheal Intubation, Use of Glucocorticoids, and Radiation Therapy (Figure 3).
 |
Figure 2 Correlation Matrix of Risk Factors. Pearson correlation matrix of the selected risk factors, highlighting high correlation coefficients (>0.8) indicative of multicollinearity. |
Regression Analysis
A Poisson regression model was initially fitted to assess the association between new infections and the selected risk factors: Surgery, Use of Ventilator, Tracheal Intubation, Use of Glucocorticoids, and Radiation Therapy. The model’s coefficients are summarized in Table 2. Significant predictors (p < 0.05) include Use of Ventilator, Tracheal Intubation, Use of Glucocorticoids, and Radiation Therapy. Surgery was not found to be a statistically significant predictor.
 |
Table 2 Poisson Regression Model Coefficients |
The dispersion parameter for the Poisson model was calculated to be 17.88, significantly exceeding the expected value of 1, thereby indicating substantial overdispersion. Given the detection of overdispersion, a Quasi-Poisson regression model was subsequently fitted (Table 3). This model confirmed the significance of Tracheal Intubation and Use of Glucocorticoids, while Use of Ventilator and Radiation Therapy were not statistically significant.
 |
Table 3 Quasi-Poisson Regression Model Coefficients |
Stepwise selection using the Akaike Information Criterion (AIC) retained all initial predictors in the Poisson model, reinforcing their collective importance (Table 4). All included predictors were highly significant (p < 0.001), reinforcing their importance in predicting new infections.
 |
Table 4 Stepwise-Selected Poisson Regression Model Coefficients |
Diagnostic Evaluation
Diagnostic plots were generated to assess the adequacy and assumptions of the fitted Poisson model (Figure 4A–D): The Residuals vs Fitted Values plot (Figure 4A) showed residuals scattered randomly around zero, indicating no obvious non-linearity but confirming overdispersion. The Scale-Location Plot (Figure 4B) revealed heteroscedasticity, further supporting the presence of overdispersion. The Cook’s Distance Plot (Figure 4C) identified several observations with Cook’s Distance values exceeding 0.21, suggesting influential observations that may disproportionately affect the model’s estimates. The Normal Q-Q Plot (Figure 4D) indicated deviations from normality in the residuals, consistent with the characteristics of count data models.
Radiation Therapy Effect
Radiation Therapy exhibited a negative association with the number of new infections, suggesting that wards utilizing radiation therapy protocols experienced lower infection rates (Figure 5).
Summary of Significant Predictors
When comparing results across both regression models (Table 5), only Tracheal Intubation (coefficient: 2.02, p < 0.01) and Use of Glucocorticoids (coefficient: 1.78, p < 0.01) remained statistically significant in the more reliable Quasi-Poisson model that accounts for overdispersion. Use of Ventilator and Radiation Therapy, while significant in the Poisson model, did not maintain statistical significance after adjusting for overdispersion. This pattern highlights the importance of accounting for overdispersion in count data analysis to avoid potentially misleading conclusions. The robust significance of tracheal intubation and use of glucocorticoids across both models underscores their critical role as risk factors for hospital-acquired infections in rehabilitation settings. Sensitivity analyses using logistic regression confirmed the consistency of these findings, with both factors remaining statistically significant (p < 0.01 for tracheal intubation; p < 0.01 for glucocorticoid use).
 |
Table 5 Summary of Significant Predictors |
Discussion
This study presents a thorough examination of hospital-acquired infections (HAIs) within a specialized rehabilitation hospital in China over a five-year period (2020–2024). The findings indicate an overall infection rate of 3.64%, with notable variations across different hospital wards. Additionally, the analysis identified critical risk factors associated with HAIs, including the use of ventilators, tracheal intubation, and glucocorticoids, while radiation therapy appeared to be associated with a reduced risk of infection.
The overall HAI rate of 3.64% observed in this study is slightly lower than global estimates, which typically range between 5% and 15% across various healthcare settings.19 This discrepancy may be attributed to the specialized nature of the rehabilitation hospital, where infection control protocols are rigorously implemented due to the high dependency of patients on medical devices and prolonged hospital stays. However, the substantial variability in infection rates across different wards, particularly the Vegetative State Awakening Department exhibiting an 11.1% infection rate, underscores the heterogeneous nature of infection risks within rehabilitation hospitals. Such variability can be influenced by several factors, including patient demographics, underlying medical conditions, and the intensity of medical interventions required in specific wards.20 For instance, wards catering to patients in vegetative states often involve prolonged mechanical ventilation and intensive medical support, which inherently increase the susceptibility to infections. Additionally, variations in staffing ratios, the availability of specialized equipment, and adherence to infection control protocols can significantly impact infection rates.21 Comparative studies have shown that specialized wards, due to their complex patient profiles and intensive care requirements, tend to have higher HAI rates compared to general medical wards.22 The use of ventilators and tracheal intubation emerged as significant predictors of HAIs in both Poisson and Quasi-Poisson regression models. This finding is consistent with existing literature, which identifies mechanical ventilation and invasive airway management as major risk factors for respiratory infections, including ventilator-associated pneumonia (VAP).23 Prolonged use of ventilators can disrupt normal respiratory defenses, facilitating the entry and colonization of pathogens.24 Tracheal intubation compromises the natural barrier of the airway, providing a direct pathway for microorganisms to invade the lower respiratory tract. Moreover, the maintenance and handling of ventilators and intubation equipment can become sources of pathogen transmission if not managed with strict aseptic techniques.25 Studies have demonstrated that stringent protocols for the management of ventilators and endotracheal tubes, such as regular cleaning, timely replacement of equipment, and adherence to hand hygiene practices, are crucial in reducing the incidence of VAP.26 Additionally, implementing ventilator care bundles, which include elements like elevation of the head of the bed, daily sedation interruptions, and spontaneous breathing trials, has been shown to significantly decrease VAP rates.27 Glucocorticoid therapy was identified as a significant risk factor for HAIs, aligning with previous studies that have highlighted the immunosuppressive effects of glucocorticoids.28 In rehabilitation settings, glucocorticoids are often administered to manage inflammation and autoimmune conditions, but their prolonged use can impair both innate and adaptive immune responses, increasing susceptibility to infections.29 Research indicates that patients receiving high doses or long-term glucocorticoid therapy are at a heightened risk of developing infections, including bacterial, viral, and fungal infections.30 The initial Poisson model suggested an association between radiation therapy and decreased risk of HAIs, a finding that contrasts with radiation’s known immunosuppressive effects.31 One plausible explanation is that wards utilizing radiation therapy may adopt more rigorous infection control protocols due to the complexity and high-risk nature of patient care in these units.32 Additionally, patients undergoing radiation therapy are often subjected to close monitoring for adverse effects, which can lead to the early detection and prompt treatment of infections.33 However, this inverse association was not statistically significant in the more reliable Quasi-Poisson model (p = 0.522), indicating that the apparent protective effect was likely a statistical artifact resulting from overdispersion in the data (dispersion parameter = 17.88) rather than a true clinical relationship.34
The identification of specific risk factors such as mechanical ventilation, tracheal intubation, and glucocorticoid use underscores the necessity for targeted infection control interventions in rehabilitation hospitals. Enhanced protocols for the management and maintenance of ventilators and endotracheal tubes, including regular cleaning and timely replacement, are critical in reducing VAP rates.35 Implementing ventilator care bundles that encompass multiple evidence-based practices can significantly lower the incidence of HAIs.36 Moreover, minimizing the use of invasive devices when possible and adopting non-invasive alternatives can substantially reduce infection risks.37 For patients requiring glucocorticoids, strategies such as prophylactic antimicrobial therapy, regular monitoring for infection signs, and optimizing glucocorticoid dosing to the lowest effective level are essential to mitigate infection risks.38 Additionally, the potential protective role of radiation therapy highlights the importance of comprehensive care protocols that integrate infection prevention measures across all therapeutic modalities.39
Despite its strengths, this study has several limitations that must be acknowledged. Firstly, the retrospective design may introduce biases related to the accuracy and completeness of medical records. Although efforts were made to standardize data collection, unmeasured confounders could influence the observed associations. Secondly, the study was conducted in a single specialized rehabilitation hospital, which may limit the generalizability of the findings to other settings with different patient populations and resource levels. Additionally, we were unable to include data on antibiotic-resistant bacteria and prior antibiotic use history, which could potentially influence infection risk. The exclusion of certain risk factors due to multicollinearity may overlook their potential contributions to HAIs, despite their clinical relevance. Future research should aim to replicate these findings in multiple rehabilitation hospitals across different regions to enhance generalizability. Prospective studies incorporating comprehensive data collection on additional potential risk factors, such as specific antibiotic use and detailed patient mobility assessments, would provide a more nuanced understanding of HAI dynamics. Moreover, qualitative studies exploring healthcare providers’ adherence to infection control protocols could identify barriers and facilitators to effective implementation. Investigating the protective mechanisms associated with radiation therapy and other non-traditional interventions could also uncover novel strategies for infection prevention.
Conclusion
This study highlights the critical role of mechanical ventilation, tracheal intubation, and glucocorticoid use in the epidemiology of HAIs within a Chinese rehabilitation hospital. The observed ward-specific variability emphasizes the need for tailored infection control strategies that address the unique challenges of different patient populations and therapeutic interventions. By identifying and mitigating key risk factors, healthcare providers can enhance patient safety, reduce morbidity and mortality associated with HAIs, and alleviate the economic burdens on healthcare systems. Continued surveillance and research are essential to sustain and improve infection control efforts in specialized rehabilitation settings.
Data Sharing Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Ethics Approval and Consent to Participate
The study protocol received approval from the Shenzhen Dapeng New District Nan’ao People’s Hospital’s Institutional Review Board, and written informed consent was waived due to the retrospective nature of the study and the use of anonymized data in accordance with the Declaration of Helsinki and local regulatory requirements.
Funding
This study was supported by the Shenzhen Dapeng New District Medical and Health Group’s 2024 Research Project Fund Support (DPJTKY202405, DPJTKY202408).
Disclosure
All of the authors had no any personal, financial, commercial, or academic conflicts of interest separately for this work.
References
1. Aljamali NM, Al Najim MM. Review in hospital-acquired infection. Int J Adv Eng Res. 2020;20(3):7–20.
2. Stewart S, Robertson C, Pan J, et al. Impact of healthcare-associated infection on length of stay. J Hosp Infect. 2021;114:23–31. doi:10.1016/j.jhin.2021.02.026
3. Gutema G, Håkonsen H, Engidawork E, et al. Antibiotic stewardship in Norway: are strategies for rational use of antibiotics followed in Norwegian healthcare system?medRxiv. 2021. doi:10.1101/2021.02.01.21250947
4. Haque M, Sartelli M, McKimm J, et al. Health care-associated infections – an overview. Infect Drug Resist. 2018;Volume 11:2321–2333. doi:10.2147/IDR.S177247
5. Castellani GB, Maietti E, Leonardi G, et al. Healthcare-associated infections and antimicrobial resistance in severe acquired brain injury: a retrospective multicenter study. Front Neurol. 2023;14:1219862. doi:10.3389/fneur.2023.1219862
6. Bartolo M, Zucchella C, Aabid H, et al. Impact of healthcare-associated infections on functional outcome of severe acquired brain injury during inpatient rehabilitation. Sci Rep. 2022;12(1):5245. doi:10.1038/s41598-022-09351-1
7. Simpson R, Robinson L. Rehabilitation after critical illness in people with COVID-19 infection. Am J Phys Med Rehabil. 2020;99(6):470–474. doi:10.1097/PHM.0000000000001443
8. Takaya S, Hayakawa K, Matsunaga N, et al. Surveillance systems for healthcare-associated infection in high and upper-middle income countries: a scoping review. J Infect Chemother. 2020;26(5):429–437. doi:10.1016/j.jiac.2020.01.001
9. Wloch C, Van Hoek AJ, Green N, et al. Cost–benefit analysis of surveillance for surgical site infection following caesarean section. BMJ Open. 2020;10(7):e036919. doi:10.1136/bmjopen-2020-036919
10. Geraldes C, Tavares L, Gil S, et al. Antibiotic heteroresistance and persistence: an additional aid in hospital acquired infections by Enterococcus spp. Future Microbiol. 2024;19(16):1407–1418. doi:10.1080/17460913.2024.2393003
11. Valmadrid LC, Schwei RJ, Maginot E, et al. The impact of health care provider relationships and communication dynamics on urinary tract infection management and antibiotic utilization for long-term care facility residents treated in the emergency department: a qualitative study. Am J Infect Control. 2021;49(2):198–205. doi:10.1016/j.ajic.2020.07.009
12. Sydnor ERM, Perl TM. Hospital epidemiology and infection control in acute-care settings. Clin Microbiol Rev. 2011;24(1):141–173. doi:10.1128/CMR.00027-10
13. Rodriguez-Acelas AL, de Abreu Almeida M, Engelman B, et al. Risk factors for health care–associated infection in hospitalized adults: systematic review and meta-analysis. Am J Infect Control. 2017;45(12):e149–e156. doi:10.1016/j.ajic.2017.08.016
14. Wang J, Liu F, Tartari E, et al. The prevalence of healthcare-associated infections in mainland China: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2018;39(6):701–709. doi:10.1017/ice.2018.60
15. Stennett J, Hou R, Traverson L, et al. Lessons learned from the resilience of Chinese hospitals to the COVID-19 pandemic: scoping review. JMIRx Med. 2022;3(2):e31272. doi:10.2196/31272
16. Weiner LM, Fridkin SK, Aponte-Torres Z, et al. Vital signs: preventing antibiotic-resistant infections in hospitals—United States, 2014. Am J Transplant. 2016;16(7):2224–2230. doi:10.1111/ajt.13893
17. Zhao X, Wang L, Wei N, et al. Risk factors of health care–associated infection in elderly patients: a retrospective cohort study performed at a tertiary hospital in China. BMC Geriatr. 2019;19:1–6. doi:10.1186/s12877-019-1208-x
18. Luo Y. Hospital infection underreporting rate: an analysis of causes and research on improvement measures. Soc Med Health Manag. 2023;4(4):55–60.
19. Liu X, Long Y, Greenhalgh C, et al. A systematic review and meta-analysis of risk factors associated with healthcare-associated infections among hospitalized patients in Chinese general hospitals from 2001 to 2022. J Hosp Infect. 2023;135:37–49. doi:10.1016/j.jhin.2023.02.013
20. Malheiro R, Gomes AA, Fernandes C, et al. Hospital context determinants of variability in healthcare-associated infection prevalence: multi-level analysis. Microorganisms. 2024;12(12):2522. doi:10.3390/microorganisms12122522
21. Keykha A, Ramezani M, Amini S, et al. Educational challenges of family caregivers of vegetative state patients for home care preparedness: a qualitative content analysis. J Educ Health Promot. 2022;11:345. doi:10.4103/jehp.jehp_1647_21
22. Papazian L, Klompas M, Luyt CE. Ventilator-associated pneumonia in adults: a narrative review. Intensive Care Med. 2020;46(5):888–906. doi:10.1007/s00134-020-05980-0
23. Udompat P, Rongmuang D, Hershow RC. Modifiable risk factors of ventilator-associated pneumonia in non-intensive care unit versus intensive care unit. J Infect Dev Ctries. 2021;15(10):1471–1480. doi:10.3855/jidc.14190
24. Diaconu O, Siriopol I, Poloșanu LI, et al. Endotracheal tube biofilm and its impact on the pathogenesis of ventilator-associated pneumonia. J Crit Care Med. 2018;4(2):50–55. doi:10.2478/jccm-2018-0011
25. Ehrmann S, Barbier F, Demiselle J, et al. Inhaled amikacin to prevent ventilator-associated pneumonia. N Engl J Med. 2023;389(22):2052–2062. doi:10.1056/NEJMoa2310307
26. Klompas M, Branson R, Cawcutt K, et al. Strategies to prevent ventilator-associated pneumonia, ventilator-associated events, and nonventilator hospital-acquired pneumonia in acute-care hospitals: 2022 update. Infect Control Hosp Epidemiol. 2022;43(6):687–713. doi:10.1017/ice.2022.88
27. Ingawale DK, Mandlik SK. New insights into the novel anti-inflammatory mode of action of glucocorticoids. Immunopharmacol Immunotoxicol. 2020;42(2):59–73. doi:10.1080/08923973.2020.1728765
28. Yang Z, Liu J, Zhou Y, et al. The effect of corticosteroid treatment on patients with coronavirus infection: a systematic review and meta-analysis. J Infect. 2020;81(1):e13–e20. doi:10.1016/j.jinf.2020.03.062
29. George MD, Baker JF, Winthrop K, et al. Risk for serious infection with low-dose glucocorticoids in patients with rheumatoid arthritis: a cohort study. Ann Intern Med. 2020;173(11):870–878. doi:10.7326/M20-1594
30. Wang K, Tepper JE. Radiation therapy–associated toxicity: etiology, management, and prevention. CA Cancer J Clin. 2021;71(5):437–454. doi:10.3322/caac.21689
31. Wei W, Zheng D, Lei Y, et al. Radiotherapy workflow and protection procedures during the Coronavirus Disease 2019 (COVID-19) outbreak: experience of the Hubei cancer hospital in Wuhan, China. Radiother Oncol. 2020;148:203–210. doi:10.1016/j.radonc.2020.03.029
32. Mouajou V, Adams K, DeLisle G, et al. Hand hygiene compliance in the prevention of hospital-acquired infections: a systematic review. J Hosp Infect. 2022;119:33–48. doi:10.1016/j.jhin.2021.09.016
33. Conte P, Ascierto PA, Patelli G, et al. Drug-induced interstitial lung disease during cancer therapies: expert opinion on diagnosis and treatment. ESMO Open. 2022;7(2):100404. doi:10.1016/j.esmoop.2022.100404
34. Lee JH, Han G, Fulp WJ, et al. Analysis of overdispersed count data: application to the Human Papillomavirus Infection in Men (HIM) Study. Epidemiol Infect. 2012;140(6):1087–1094. doi:10.1017/S095026881100166X
35. Wan K, Liang H, Yan G, et al. A quality assessment of evidence-based guidelines for the prevention and management of ventilator-associated pneumonia: a systematic review. J Thorac Dis. 2019;11(7):2795. doi:10.21037/jtd.2019.06.56
36. Mastrogianni M, Katsoulas T, Galanis P, et al. The impact of care bundles on ventilator-associated pneumonia (VAP) prevention in adult ICUs: a systematic review. Antibiotics. 2023;12(2):227. doi:10.3390/antibiotics12020227
37. Newton R, Leigh R, Giembycz MA. Pharmacological strategies for improving the efficacy and therapeutic ratio of glucocorticoids in inflammatory lung diseases. Pharmacol Ther. 2010;125(2):286–327. doi:10.1016/j.pharmthera.2009.11.003
38. Venkatesh B, Finfer S, Cohen J, et al. Adjunctive glucocorticoid therapy in patients with septic shock. N Engl J Med. 2018;378(9):797–808. doi:10.1056/NEJMoa1705835
39. Lynch JB, Davitkov P, Anderson DJ, et al. Infectious diseases society of America guidelines on infection prevention for healthcare personnel caring for patients with suspected or known COVID-19 (November 2021). Clin Infect Dis. 2024;78(7):e230–e249. doi:10.1093/cid/ciab953
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Temporal Trends and Projections of Bladder Cancer Burden in China from 1990 to 2030: Findings from the Global Burden of Disease Study
Xiang Z, Ye Z, Ma J, Lin Y, Zhou Y
Clinical Epidemiology 2022, 14:1305-1315
Published Date: 6 November 2022
Epidemiological Trends of Kidney Cancer Along with Attributable Risk Factors in China from 1990 to 2019 and Its Projections Until 2030: An Analysis of the Global Burden of Disease Study 2019
Xu Q, Zhang T, Xia T, Jin B, Chen H, Yang X
Clinical Epidemiology 2023, 15:421-433
Published Date: 28 March 2023





