Back to Journals » Infection and Drug Resistance » Volume 18
Analysis of the Distribution Characteristics and Changes of Drug Resistance of Pathogens in Patients with Urinary Tract Infection Across Southwest China From 2019 to 2023
Authors Zhong M, Huang X, Liu X, Yu H, Long S
Received 8 January 2025
Accepted for publication 12 March 2025
Published 17 March 2025 Volume 2025:18 Pages 1491—1502
DOI https://doi.org/10.2147/IDR.S512409
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Min Zhong, Xiangning Huang, Xin Liu, Hua Yu, Shanshan Long
Department of Laboratory Medicine, Sichuan Provincial People’s Hospital, University of Electronic Science and Technology of China, Chengdu, 610072, People’s Republic of China
Correspondence: Shanshan Long, Email [email protected] Hua Yu, Email [email protected]
Objective: To analyze the changes in the distribution and drug resistance of pathogenic bacteria causing urinary tract infections in Southwest China from 2019 to 2023, and to provide an accurate scientific basis for empirical clinical use.
Methods: The identification results and drug susceptibility tests of non-duplicate pathogens isolated from urine samples of patients in Sichuan region from 2019 to 2023 were retrospectively analyzed. The results obtained were interpreted with reference to CLSI M100-33th and analyzed with WHONET 5.6 software.
Results: A total of 247295 strains of pathogens were detected, including 188551 gram-negative strains (76.2%). The positive rate of female patients (56.8%) was significantly higher than that of male patients (43.2%). The top five most common urinary pathogens were Escherichia coli (50.5%), Enterococcus faecium (11.5%), Klebsiella pneumoniae (8.5%), Enterococcus faecalis (6.5%), and Proteus mirabilis (2.9%). The resistance rate of E.coli to levofloxacin, cefotaxime and ceftriaxone was higher (> 50%) and had a certain upward trend. The resistance rates of Klebsiella pneumoniae to imipenem and meropenem increased from 7.8% and 9.6% in 2019 to 11.6% and 13.2% in 2023, respectively, much higher than the resistance rates of E. coli to carbapenem antibiotics (< 2%). E. coli, K. pneumoniae and E. cloacae still maintained high activity against tigecycline and polymyxin B. The drug resistance rate of Acinetobacter baumannii to imipenem and meropenem was more than 27.4%. The resistance rates of Enterococcus faecium and Enterococcus faecalis to vancomycin, teicoplanin and linezolid were lower than 3.4%. There was an increasing trend in the detection of CRE-KPN among multidrug-resistant bacteria, and a slight decreasing trend in CRPA and CRAB.
Conclusion: The main pathogens of urinary tract infections were E. coli, E. faecium and K. pneumoniae. The drug resistance rates of main clinically isolated bacteria in urine samples showed a diverse trend. Antibiotics should be rationally selected based on the resistance patterns of the pathogens. At the same time, with the continuous detection of multi-drug resistant bacteria VRE and CRE, we have a long way to go in future drug resistance monitoring.
Keywords: urinary tract infections, pathogenic bacteria distribution, drug resistance
Introduction
Urinary tract infections (UTIs) is one of the most common conditions in both outpatient and inpatient settings worldwide, where it has been noted to affect 150 million people annually.1–3 There are more than 8 million office visits for UTI every year in the United States.4 UTIs are the most common infectious disease in women worldwide, with nearly 50% of women experiencing a UTI at least once a year, and it is the second most common infectious disease in the elderly after pneumonia.5 UTIs cause short-term morbidity such as fever, dysuria, and flank pain, and may also result in long-term renal injury, such as permanent kidney scarring.6 Although most patients suffer only with a varying range of painful and annoying symptoms, the Centers for Disease Control and Prevention (CDC) reports that UTIs contribute to 13,000 deaths every year.7 UTI is easy to relapse, the symptoms are not typical, difficult to cure, early and timely diagnosis and treatment can avoid damage to the kidney.8 The analysis of the distribution and drug resistance of UTI pathogens is beneficial to the rational use of antibiotics.9 However, Studies have found that the distribution and drug resistance of UTI are regional and temporal, and the experience of different countries and regions is only for reference.10 In the Asia-Pacific region, one systematic review found that the resistance rate of E.coli to ceftriaxone, ciprofloxacin, and trimethoprim/sulfamethoxazole (TMP/SMX) was 33–90%, the resistance rate to nitrofurantoin was 2.7–31.4%, and the resistance rate to fosfomycin was 1.8%.11 However, another study found that Klebsiella pneumoniae(K. pneumoniae) isolates in Mexico had poor resistance to amikacin and carbapenems, whereas nitrofurantoin had a median resistance of 52%.12 According to a study in China showed that Escherichia coli(E.coli) had a greater than 50% resistance rate to ciprofloxacin (58.6%), and levofloxacin (51.2%). Low levels of resistance were seen to carbapenems (0.1%-0.7%), piperacillin/tazobactam (0.7%), and nitrofurantoin (1.8%).13 Unfortunately, E. faecium and E. faecalis isolates of UTIs are resistant to vancomycin and linezolid which can lead to a serious and uncontrollable hospital infection.14
Therefore, regular monitoring and understanding the distribution characteristics and drug resistance of pathogenic bacteria in UTIs in different countries and regions is important and necessary for clinical improvement of the effectiveness of early empirical treatment as well as for controlling the growth of drug resistance of pathogenic bacteria.13 In China, studies had reported the distribution and drug resistance rates of pathogenic bacteria with UTIs in the Jiaxing region from 2020 to 2022 and Chongming area of Shanghai in the eastern from 2018 to 2020.9,13 But currently antibiotic resistance and drug sensitivity trends among uropathogens in Southwest China has rarely been reported. Therefore, this study retrospectively analyzed the data on the distribution of pathogenic bacteria and drug sensitivity results of UTIs in 109 hospitals in Southwest China from 2019 to 2023, in order to provide a basis for the rational use of antimicrobial drugs in the clinical treatment of UTIs.
Materials and Methods
Bacterial Isolates
This retrospective study was conducted in 109 healthcare institutions that are members of the Sichuan Bacterial Resistance Surveillance Network in China from January 2019 to December 2023. Ethical approval was obtained from the Institutional Review Board of Sichuan Provincial People’s Hospital, and University of Electronic Science and Technology of China (Number: 2025–21). The ethics committee waived the need for written informed consent provided by participants due to the retrospective nature of this study. Patients’ anonymous information was provided from the microbiology hospital laboratory, which isolated the strains. The study completely followed the principles outlined in the Declaration of Helsinki.
After data review, the identification and drug sensitivity results of 247,295 strains isolated from urine specimens were included in the final analysis, and According to the monitoring protocol, only the first strain of the same bacteria from the same patient was retained.
Bacterial Culture
The same standard microbiological techniques were used to cultivate each sample. Midstream urine was collected in sterile tubes after vulva cleaning and sent to the microbiology laboratory for quantitative incubation within two hours. The urine samples were inoculated onto 5% sheep blood agar, MacConkey, and Chocolate plates using a sterile inoculation loop (10µL). The plates were incubated aerobically for 18–24 hours at 35 °C while the size and shape of the colonies were observed. It was defined as positive for culture if a single gram-negative bacteria reached a concentration of ≥105 CFU/mL or gram-positive bacteria reached a concentration of ≥104 CFU/mL.
Bacterial Identification and Susceptibility Testing
Bacteria identification was carried out in accordance with laboratory standard operating procedures using VITEK system, or MALDI system (bioMérieux, France). The drug susceptibility test was performed by the minimum inhibitory concentration (MIC) test and the Kirby-Bauer (K-B) method.
Interpretation of Results and Quality Control
The MIC value and inhibition circle diameter results were interpreted according to the CLSI M100 33rd edition guideline standard.15 Among them, the judgment standard of tigecycline is recommended by the The United States Food and Drug Administration (FDA).16 The quality control bacteria of drug susceptibility test were: Staphylococcus aureus ATCC25923 and ATCC29213, Escherichia coli ATCC25922, Pseudomonas aeruginosa ATCC27853, Streptococcus pneumoniae ATCC49619 and Haemophilus influenzae ATCC49247. When the results of quality control strains were under control, the results of the study strains could be included in the data analysis.
Statistical Analysis
The susceptibility test results were processed using WHONET5.6 software (WHO, Geneva, Switzerland) and duplicate strains were directly excluded. The specific steps are as follows: (1) Data package import: import all drug susceptibility test results into the WHONET5.6 system, including basic information of patients, information of isolated strains, antibacterial drug names and specific drug susceptibility test results; (2) Analysis type selection: Select different types of analysis in WHONET5.6 according to statistical needs, such as isolated strain information, drug susceptibility analysis, drug resistant bacteria analysis, etc.; (3) Set analysis options: Set the corresponding options according to the type of data to be analyzed, such as selecting the type of antibiotics to be concerned, strain type, etc.; (4) Generate reports; (5) Export data.
Results
Distribution of Pathogenic Bacteria in Urine Samples
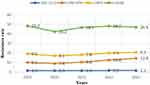
A total of 247295 strains of pathogens were detected in urine samples, including 188551 gram-negative strains (76.2%) and 58744 Gram-positive strains (23.8%). 106,767 isolates were isolated from male patients (43.2%) and 140,528 isolates from female patients (56.8%). The positive rate of isolation in female patients was significantly higher than that in male patients. The positive rate of children under 18 years old was 3.4% (8458/247,295). The detection rate of patients >18 ~ <60 years old was 36.2% (89,581/247,295). The detection rate of patients ≥60 years old was 60.4% (149,256/247,295). The top five bacteria in terms of detection rate were Escherichia coli (50.5%), Enterococcus faecium (11.5%), Klebsiella pneumoniae (8.5%), Enterococcus faecalis (6.5%), and Proteus mirabilis (2.9%), as shown in Tables 1 and 2. The detection trends of the top 5 bacterial pathogens causing UTIs were shown in Figure 1.
 |
Table 1 Distribution of Bacterial Pathogens Isolated From Urine Specimens |
 |
Table 2 Characteristics of Strains Isolated in Different Sex and Age Groups |
 |
Figure 1 Detection trends of the top 5 bacterial pathogens causing UTIs. |
Resistance of Main Gram-Negative Bacteria
Antibiotic Resistance Patterns of Main Enterobacteriaceae Bacteria
E. coli, K. pneumoniae and Proteus mirabilis (P. mirabilis) were the main bacteria isolated from urine samples. E. coli had high sensitivity to amikacin, nitrofurantoin, cefoperazone/sulbactam, piperacillin/tazobactam, the resistance rate was less than 10%, and the change trend in 5 years was not obvious. The drug resistance to quinolone antibiotics, cefazolin, ceftriaxone and cefotaxime was high, and the drug resistance rate was more than 50%, and there was a certain upward trend, as shown in Table 3. The resistance rates of K. Pneumoniae to ceftriaxone and cefotaxime ranged from 41% to 46%, and the resistance rates of imipenem and meropenem increased from 7.8% and 9.6% in 2019 to 11.6% and 13.2% in 2023, respectively, much higher than the resistance rates of E. coli to carbapenems (resistance rates <2%), as shown in Table 4. In addition, the resistance rate of K. pneumoniae to nitrofurantoin (29–34%) was much higher than that of E. coli (2–4%), while the resistance rate of E. coli to levofloxacin (>50%) was much higher than that of K. pneumoniae (<32%). The resistance rate of P. mirabilis to amikacin, meropenem, cefoperazone/sulbactam and piperacillin/tazobactam was low, less than 2%, as shown in Table 5. In 5 years, E. coli, K. pneumoniae and Enterobacter cloacae (E. cloacae) still maintained high activity against tigecycline and polymyxin B, and the drug resistance rate was less than 5.4%.
 |
Table 3 Changing Resistance Rates and Susceptibility Rates of E. coli to Antimicrobial Agents |
 |
Table 4 Changing Resistance Rates and Susceptibility Rates of K. pneumoniae to Antimicrobial Agents |
 |
Table 5 Resistance Rates of E. Cloacae and P. mirabilis to Antimicrobial Agents |
Antibiotic Resistance Patterns of Main Non-Fermentative Bacteria
A total of 6720 strains of Pseudomonas aeruginosa (P. aeruginosa) and 3652 strains of Acinetobacter baumannii (A. baumannii) were isolated, and their resistance rates to the detected antibiotics were low, less than 17%. The resistance rates to imipenem and meropenem were 7.0% and 6.2%, respectively. The lowest resistance rate to polycolistin B was 1.0%, as shown in Table 6. The drug resistance rate of A. baumannii to imipenem and meropenem was more than 27.4%. However, the drug resistance rates to tigecycline and polymyxin B were low, the highest were 3.0% and 0.5%, respectively. The rate of resistance to minocycline was 8.9%, as shown in Table 6.
 |
Table 6 Resistance Rates of P. aeruginosa and A. baumannii to Antimicrobial Agents |
Drug Resistance in Main Gram-Positive Bacteria
Antibiotic Resistance Patterns of Main Enterococcus Spp
A total of 23972 strains (9.7%) of Enterococcus faecium (E. faecium) and 16098 strains (6.5%) of Enterococcus faecalis (E. faecalis) were isolated. The resistance rate of E. faecium to detected antibiotics was significantly higher than that of E. faecalis, especially to ampicillin, levofloxacin, high concentration gentamicin and vancomycin. However, the resistance rate of E. faecalis to linezolid was higher than that of E. faecium. Among them, the resistance rate of E. faecium to penicillins and quinolones was as high as 90%, while Enterococcus was highly sensitive to vancomycin and linezolid, and the resistance rate was less than 4%, as shown in Table 7.
 |
Table 7 Resistance Rates of E. Faecium and E. Faecalis to Antimicrobial Agents |
Antibiotic Resistance Patterns of Main Staphylococcus Spp and Streptococcus Spp
A total of 3130 strains of Staphylococcus aureus (S. aureus) were isolated, accounting for 1.3%, and the detection rate of Methicillin-resistant Staphylococcus aureus (MRSA) was 25.0%. MRSA had high resistance rate to erythromycin, clindamycin and levofloxacin. The resistance rate of MRSA to most tested antimicrobials was significantly higher than that of Methicillin-sensitive Staphylococcus aureus(MSSA), but the resistance to TMP/SMX was lower than that of MSSA. A total of 3272 strains of Streptococcus agalactiae (S. agalactis) were isolated, accounting for 1.3%. In addition to erythromycin, clindamycin and levofloxacin, the resistance rate of S. agalactis was more than 52%, and it was highly sensitive to other tested antibiotics, as shown in Table 8.
 |
Table 8 Resistance Rates of S. aureus and S. agalactiae to Antimicrobial Agents |
Change Trend of Carbapenem-Resistant Bacteria
Among the carbapenem-resistant bacteria detected from 2019 to 2023, the detection rates of CRE-KPN showed an increasing trend, CRPA and CRAB showed a slight decreasing trend, and CRE-ECO remained at a low level, as shown in Figure 2.
Discussion
Through analyzing the data of 247,295 strains of urine pathogens in southwest China from 2019 to 2023, some significant characteristics and trends of drug resistance were found. The results showed that 247295 strains of clinical bacteria isolated from urine samples had the following characteristics: Gram-negative bacteria and positive bacteria were 76.2% and 23.8%, respectively; Gram-negative bacteria were slightly more likely to cause UTIs than Gram-positive bacteria. The results showed certain changes compared with the separation rate in Shanghai, China (61.2% and 30.4%).9 The incidence of urinary tract infection in female patients (56.8%) was more common than that in male patients (43.2%), which was related to the fact that female patients with short and straight urethral opening were more prone to bacterial infection. The data was consistent with the conclusion of the study that the number of females suffering from UTIs was 12,351 (79.6%), which was much higher than the males (3088, 20.4%) in Portugal.17 The number of isolates was the highest in elderly patients aged ≥60 years (60.4%), while the isolation rate in children was the lowest (3.4%), which may be related to the decrease of immunity with the increase of age, the more likely to be hospitalized, invasive urinary tract operations and the use of more antibiotics.18 We found that the top five isolates leading to UTIs remained consistent and the number detected increased year by year, with Enterobacter(64%) being the main cause of UTIs, with E. coli, K. pneumoniae, P. mirabilis, and E. cloacae being the most frequently isolated species, so it is useful to understand their resistance patterns. Studies have reported that E. coli accounts for up to 80% of community-acquired uncomplicated UTIs, these bacteria should be targeted when choosing empirical antibiotics.19
The drug sensitivity results of this study showed that E. coli was highly sensitive to carbapenems, cephalosporins (cefotetan), piperacillin/tazobactam, and the sensitivity rate was more than 90%. Similar findings were made by Niu et al who noted that E. coli had a greater than 50% resistance rate to ceftriaxone, ampicillin, and quinolones and low levels of resistance rate to carbapenems (1%), piperacillin/tazobactam (0.7%), and nitrofurantoin (1.8%).13 One study found that the drug resistance rate of Enterobacteriaceae to third-generation and fourth-generation cephalosporins reached more than 40%, indicating that these agents might not be the optimum medications for empirical UTI therapies in China.20 The resistance rate of E. coli to ceftriaxone in 5 years (51.5–52.7%) was significantly higher than that of ceftazidime (23.9–26.0%). However, the drug sensitivity results in this region showed that Enterobacteriaceae bacteria were still sensitive to the 3rd generation of ceftriaxone, the 3rd generation of ceftriaxone could accelerate the production of ESBLs by some bacteria.20 Therefore, third-generation cephalosporins are not recommended for the treatment of UTIs. Fluoroquinolones, especially ciprofloxacin and levofloxacin, are considered effective antimicrobials against urinary tract pathogens because of the high concentration of the drugs in urine. In this study, it was found that the resistance rate of E. coli to commonly used levofloxacin and ciprofloxacin was as high as 50%, which was significantly higher than the previously reported resistance rate (26.9–28.9%).20 A 5-year data study showed that E. coli remained highly susceptible to nitrofurantoin (>89%), and the antibiotic can continue to be used empirically because it has a significantly higher inhibitory effect on bacteria in urine than in blood in the treatment of UTIs. However, a study in India reported that the resistance rate of E. coli to nitrofurantoin was 78.71%,21 demonstrating that there are considerable regional and national variations in antibiotic resistance patterns. Infectious Diseases Society of America (IDSA) recommended that TMP/SMX are preferred treatment options for uncomplicated cystitis caused by ESBL-E.22 However, the results of this study showed that the overall resistance rates of E. coli and K. pneumoniae to TMP/SMX had little change, but both had reached 39.5%. Therefore, we suggest that the empirical treatment of uncomplicated cystitis in this area should be selected in combination with clinical drug resistance patterns.
Carbapenems can still be considered appropriate for severe infections and can be used as an alternative empirical treatment for UTIs caused by strains of Enterobacteriaceae bacteria that are highly suspected of producing ESBL or AmpC inhibition.22 Although carbapenems are not the drug of choice for simple cystitis and pyelonephritis in women according to IDSA guidelines, they are a good alternative for the treatment of multidrug-resistant gram-negative bacteria that cause UTIs.22 However, with its extensive use in clinical practice, this study found that carbapenem-resistant Enterobacteriales (CRE) of urine isolates increased year by year in the past 5 years, with the highest detection rate of CRKP. Our data showed that the resistance rate of K. pneumoniae isolated from urine samples to carbapenem antibiotics increased from 8.5% in 2019 to 12.8% in 2023. The resistance rate of E. coli to carbapenems was lower than that of K. pneumoniae, and the resistance rate of E. coli to carbapenems remained at 1.3% and the change trend was not obvious.
Nucleic acid or antigen testing should be routinely performed in clinical microbiology laboratories to grasp the specific carbapenase produced by clinical CRE isolates recommended by IDSA.22 Since specific new β-lactam antibiotics were only active to the corresponding carbapenase, it was important to understand the specific carbapenase type produced by clinical CRE strains for clinical treatment selection.22 A nationwide survey in China showed that the main resistance mechanism in 90% of CRE strains was the acquired production of blaKPC-2 and blaNDM.23 Ceftazidime-avibactam, meropenem-vaborbactam, imipenem-cilastatin-relebactam, and cefiderocol were preferred treatment options for pyelonephritis and UTIs caused by CRE based on clinical trials showing non-inferiority of these agents to common comparator agents for UTIs.24–27 This study showed that E. coli and K. pneumoniae had low resistance rates to tigecycline and polycolistin B. However, it was worth noting that in 2023, 1.7% of K. pneumoniae isolates in urine samples were found to be resistant to tigecycline, and 5.4% strains were resistant to polycolistin B, which should attract our attention.
The isolation rate of E.f aecium in the Enterococcus that caused UTIs (9.7%) was higher than that of E. faecalis (6.5%). Studies had shown that indurating catheters can stimulate the formation of Enterococcus biofilm and cause immunological and histological changes in the bladder, which was the main cause of urinary tract infection.28 Surveillance data from our region indicated that E. faecium had a higher rate of resistance to most antimicrobial drugs than E. faecalis, especially to ampicillin, rifampicin, levofloxacin and ciprofloxacin. In the present study, a small number of Enterococcus resistant to vancomycin (<1.3%) and linezolid (<3.6%) were identified. The outbreaks of the hospital-acquired vancomycin-resistant Enterococcal infections had been reported, which caused severe nosocomial infections and were increasing worldwide.29 So it is necessary to strengthen the surveillance, and prevent and control nosocomial infection.
Conclusion
On the whole, E. coli is still the most common pathogen of UTIs, followed by E. faecium and K. pneumoniae. The drug resistance rate of UTIs showed a slow upward trend in the zigzag pattern. Clinicians should timely sampling and collection of urine specimens before starting antibiotics, and treatment decisions should be refined based on the common species and the AST profile of the pathogen in our area. When conditions permit, patients with multi drug-resistant bacteria isolated should be treated in isolation as much as possible to prevent the spread of MDR within the hospital. Meanwhile, in order to better understand the molecular epidemiological characteristics of multi-drug resistant bacteria in this region, further study of these genes as markers of antibiotic resistance is recommended.
Abbreviations
ESBL-E, Extended-spectrum beta-lactamases; CRKP, Carbapenem-resistant Klebsiella pneumoniae; VRE, Vancomycin-resistant Enterococci.
Acknowledgment
We are grateful to all the authors for their contributions to this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Khoshnood S, Heidary M, Mirnejad R, et al. Drug-resistant gram-negative uropathogens: a review. Biomed Pharmacother. 2017;94:982–994. doi:10.1016/j.biopha.2017.08.006
2. Foxman B. Urinary tract infection syndromes: occurrence, recurrence, bacteriology, risk factors, and disease burden. Infect Dis Clin North Am. 2014;28(1):1–13. doi:10.1016/j.idc.2013.09.003
3. O’Brien VP, Hannan TJ, Nielsen HV, et al. Drug and vaccine development for the treatment and prevention of urinary tract infections. Microbiol Spectr. 2016;4(1). doi:10.1128/microbiolspec.UTI-0013-2012
4. Waller TA, Pantin SAL, Yenior AL, et al. Urinary tract infection antibiotic resistance in the United States. Prim Care. 2018;45(3):455–466. doi:10.1016/j.pop.2018.05.005
5. Belete Y, Asrat D, Woldeamanuel Y, et al. Bacterial profile and antibiotic susceptibility pattern of urinary tract infection among children attending Felege Hiwot Referral hospital, Bahir Dar, Northwest Ethiopia. Infect Drug Resist. 2019;12:3575–3583. doi:10.2147/IDR.S217574
6. Wennerstrom M, Hansson S, Jodal U, et al. Primary and acquired renal scarring in boys and girls with urinary tract infection. J Pediatr. 2000;136(1):30–34. doi:10.1016/S0022-3476(00)90045-3
7. Kumar MS, Das AP. Emerging nanotechnology based strategies for diagnosis and therapeutics of urinary tract infections: a review. Adv Colloid Interface Sci. 2017;249:53–65. doi:10.1016/j.cis.2017.06.010
8. Masajtis-Zagajewska A, Nowicki M. New markers of urinary tract infection. Clin Chim Acta. 2017;471:286–291. doi:10.1016/j.cca.2017.06.003
9. Li J, Jiang F, Xie A, Jiang Y. Analysis of the distribution and drug resistance of pathogens in patients with urinary tract infection in the Eastern Chongming area of Shanghai from 2018 to 2020. Infect Drug Resist. 2022;15:6413–6422. doi:10.2147/IDR.S384515
10. Gajdács M, Ábrók M, Lázár A, et al. Increasing relevance of gram-positive cocci in urinary tract infections: a 10-year analysis of their prevalence and resistance trends. Sci Rep. 2020;10(1):17658. doi:10.1038/s41598-020-74834-y
11. Sugianli AK, Ginting F, Parwati I, et al. Antimicrobial resistance among uropathogens in the Asia-Pacific region: a systematic review. JAC Antimicrob Resist. 2021;3(1):dlab003. doi:10.1093/jacamr/dlab003
12. Miranda-Novales M, Flores-Moreno K, López-Vidal Y, et al. Limited therapeutic options in Mexico for the treatment of urinary tract infections. Antibiotics. 2022;11:1656. doi:10.3390/antibiotics11111656
13. Niu X, Hou B, Yang L, et al. Patterns of drug resistance and bacterial pathogen distribution in patients with urinary tract infections in the Jiaxing Region from 2020 to 2022. Infect Drug Resist. 2023;16:5911–5921. doi:10.2147/IDR.S424158
14. Lu X, Wang Y, Guo W, et al. Antibacterial activity of an FtsZ inhibitor celastrol and its synergistic effect with vancomycin against enterococci in vitro and in vivo. Microbiol Spectr. 2023;11(1):e0369922. doi:10.1128/spectrum.03699-22
15. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing. CLSI; 2023.
16. U.S.Food and Drug Administration. FDA-identified interpretive criteria[EB/OL]. 2022. Available from: https://www.fda.gov/drugs/development-resources/tigecycline-injection-products.
17. Jalil M, Naji Al Atbee M. The prevalence of multiple drug resistance Escherichia coli and Klebsiella pneumoniae isolated from patients with urinary tract infections. J Clin Lab Anal. 2022;36(9):e24619. doi:10.1002/jcla.24619
18. Rowe TA, Juthani-Mehta M. Diagnosis and management of urinary tract infection in older adults. Infect Dis Clin North Am. 2014;28(1):75–89. doi:10.1016/j.idc.2013.10.004
19. Kang C, Kim J, Park DW, et al. Clinical practice guidelines for the antibiotic treatment of community-acquired urinary tract infections. Infection & Chemotherapy. 2018;50(1):67–100. doi:10.3947/ic.2018.50.1.67
20. Yang Q, Zhang H, Wang Y, et al. Antimicrobial susceptibilities of aerobic and facultative gram-negative bacilli isolated from Chinese patients with urinary tract infections between 2010 and 2014. BMC Infect Dis. 2017;17(1):192. doi:10.1186/s12879-017-2296-x
21. Prakash D, Saxena RS. Distribution and antimicrobial susceptibility pattern of bacterial pathogens causing urinary tract infection in urban community of Meerut City, India. ISRN Microbiol. 2013;2013:749629. doi:10.1155/2013/749629
22. Tamma PD, Heil EL, Justo JA, et al. Infectious diseases society of America 2024 guidance on the treatment of antimicrobial-resistant gram-negative infections. Clin Infect Dis. 2024. doi:10.1093/cid/ciae403
23. Zhang R, Liu L, Zhou H, et al. Nationwide surveillance of clinical carbapenem-resistant Enterobacteriaceae (CRE) strains in China. EBioMedicine. 2017;19:98–106. doi:10.1016/j.ebiom.2017.04.032
24. Wagenlehner FM, Sobel JD, Newell P, et al. Ceftazidime-avibactam versus doripenem for the treatment of complicated urinary tract infections, including acute pyelonephritis: RECAPTURE, a phase 3 randomized trial program. Clin Infect Dis. 2016;63(6):754–762. doi:10.1093/cid/ciw378
25. Kaye KS, Bhowmick T, Metallidis S, et al. Effect of meropenem-vaborbactam vs piperacillin-tazobactam on clinical cure or improvement and microbial eradication in complicated urinary tract infection: the TANGO I randomized clinical trial. JAMA. 2018;319(8):788–799. doi:10.1001/jama.2018.0438
26. Bassetti M, Echols R, Matsunaga Y, et al. Efficacy and safety of cefiderocol or best available therapy for the treatment of serious infections caused by carbapenem-resistant gram-negative bacteria (CREDIBLE-CR): a randomised, open-label, multicentre, pathogen-focused, descriptive, phase 3 trial. Lancet Infect Dis. 2021;21(2):226–240. doi:10.1016/S1473-3099(20)30796-9
27. Portsmouth S, van Veenhuyzen D, Echols R, et al. Cefiderocol versus imipenem-cilastatin for the treatment of complicated urinary tract infections caused by gram-negative uropathogens: a Phase 2, randomised, double-blind, non-inferiority trial. Lancet Infect Dis. 2018;18(12):1319–1328. doi:10.1016/S1473-3099(18)30554-1
28. Guiton PS, Hannan TJ, Ford B, et al. Enterococcus faecalis overcomes foreign body-mediated inflammation to establish urinary tract infections. Lancet Infect Dis. 2013;81(1):329–339. doi:10.1128/IAI.00856-12
29. Gao W, Howden BP, Stinear TP. Evolution of virulence in Enterococcus faecium, a hospital-adapted opportunistic pathogen. Curr Opin Microbiol. 2018;41:76–82. doi:10.1016/j.mib.2017.11.030
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.