Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 17
Antibiotic Prophylaxis in Patients with Joint Prostheses: Variability in Dentists’ Practices and the Need for Guidance
Received 6 March 2025
Accepted for publication 7 May 2025
Published 11 May 2025 Volume 2025:17 Pages 209—215
DOI https://doi.org/10.2147/CCIDE.S526588
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Christopher E. Okunseri
Mohamed Rahhali,1,2 Majid Sakout1,2
1Department of Conservative Dentistry and Endodontics, Faculty of Dentistry, Mohammed V University, Rabat, Morocco; 2Service of Conservative Dentistry and Endodontics, Mohammed V Military Hospital of Rabat, Rabat, Morocco
Correspondence: Mohamed Rahhali, Faculty of Dentistry, Mohammed V University, Madinat Al Irfane, Rabat, Morocco, Tel +212662222918, Email [email protected]
Background and Objective: With increasing life expectancy, the incidence of degenerative and inflammatory joint diseases continues to rise. These conditions are major indications for orthopedic prostheses, which pose risks of postoperative complications, particularly infections of orthopedic prostheses (IPO). Dental infections have been considered a potential source of these infections, and recommendations regarding the use of antibiotic prophylaxis (AP) during dental procedures have evolved over time. Current guidelines discourage the routine use of AP. This study aims to assess the knowledge, attitudes, and practices (KAP) of private-sector dentists in the cities of Rabat, Temara, and Salé (Morocco) regarding the dental management of patients with orthopedic prostheses, particularly the use of AP.
Methodology: An anonymous 21-question survey was distributed to 310 dentists practicing in these cities. The collected responses were analyzed using JamoviR software (version 2.3.25), with a significance threshold set at p < 0.05. Chi-square and Fisher’s exact tests were employed to compare different groups.
Results: Out of 310 distributed questionnaires, 102 valid responses were retained (response rate: 32.9%). Among respondents, 53.9% considered patients with joint prostheses at risk of infection, yet only 47.1% reported prescribing AP. Female practitioners and those with over 20 years of experience were significantly more likely to prescribe AP (p=0.047 and p=0.002, respectively). Dentists who did not consult guidelines or attend professional conferences were also more prone to prescribing AP during endodontic procedures (p=0.017 and p=0.018).
Conclusion: This study reveals inconsistent knowledge and practices among dentists regarding AP use for patients with joint prostheses. Given the misalignment with current guidelines and the influence of outdated sources of information, targeted educational interventions and updated clinical guidelines are urgently needed to promote evidence-based practices. Clear, standardized guidelines are also essential to prevent the unjustified overprescription of antibiotics and to address the growing concern of antimicrobial resistance.
Keywords: joint prostheses, dentistry, antibiotic prophylaxis, knowledge, attitudes, practices
Introduction
With global increases in life expectancy, the prevalence of degenerative and inflammatory joint diseases is rising, leading to a growing number of orthopedic surgeries. In 2022 alone, approximately 28.3 million such surgeries were performed globally,1 and knee arthroplasty is projected to reach 3.48 million procedures annually in the United States by 2030.2 These surgeries are not without complications, the most severe being prosthetic joint infections (PJI), which are difficult to manage and potentially linked to oral infections.
Historically, antibiotic prophylaxis (AP) before dental procedures was widely recommended for patients with joint prostheses, based on the assumption that transient bacteremia could lead to PJIs. However, recent guidelines from international organizations such as the American Dental Association (ADA), American Academy of Orthopaedic Surgeons (AAOS), and European Federation of Periodontology (EFP) have shifted away from this approach. They now advise against routine AP, recommending instead an individualized assessment of infection risk.3–5 Despite this, clinical practices remain inconsistent and often rely on outdated information.
The literature presents conflicting findings: while some studies suggest a correlation between invasive dental procedures and PJIs, others report no statistically significant association.6–9 These discrepancies, combined with concerns about antibiotic resistance and unnecessary medication, highlight the importance of evaluating real-world clinical practices.
In Morocco, national guidelines regarding AP use in dentistry remain unclear, and little is known about how private-sector dentists handle these cases. This study addresses this gap by assessing the knowledge, attitudes, and practices (KAP) of dentists in Rabat, Temara, and Salé regarding AP for patients with joint prostheses. Understanding these practices can inform future educational interventions, policy development, and guideline standardization at the national level.
Methods
This is a KAP (Knowledge, Attitudes, and Practices) study conducted between August 1, 2022, and February 6, 2023. An anonymous 21 question survey, distributed via Google Forms, was sent to 310 dentists in Rabat, Temara, and Salé, Morocco. A convenience sampling method was chosen due to limited access to a complete registry of dentists and logistical constraints. While this approach may introduce selection bias, it allowed for timely data collection from a representative subset of urban dental practitioners.The questionnaire was pretested during a calibration phase with 10 final-year dental students to assess clarity, coherence, and time of completion. Feedback from this phase was used to reword ambiguous items, standardize terminology, and improve the flow of questions. This refinement enhanced content validity and helped reduce potential response bias. Following calibration, specific adjustments were made to clarify clinical scenarios and align terminology with common dental practice.Only fully completed questionnaires were included in the final analysis. Incomplete responses were excluded to maintain data integrity. The full questionnaire is provided as Supplementary Material.
The collected data were then entered into JamoviR software (version 2.3.25) for statistical analysis, with a significance level set at p<0.05. Chi-square and Fisher’s exact tests were employed to compare different groups. No formal power calculation was performed. However, a sample of over 100 respondents was deemed sufficient to detect medium effect sizes (Cohen’s w = 0.3) at 80% power and α = 0.05, consistent with the exploratory nature of the study.
Results
Out of 106 collected responses, four were excluded due to missing mandatory fields, yielding 102 valid responses and a participation rate of 32.9%. Among participants, gender distribution was equal (51 men, 51 women), with a predominance of general practitioners (75.5%). Among the 25 specialists, 30.8% were orthodontists and 7.7% were conservative dentistry specialists.
The dominant age group was 25–35 years, comprising 52.9% of the sample, while those over 55 years old accounted for only 13.7%. Additionally, 44.1% had five years or fewer of professional experience. The demographic characteristics of the sample are summarized in Table 1.
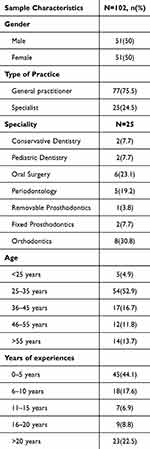 |
Table 1 Demographic Characteristics of the Sample |
A total of 53.9% of participants considered patients with orthopedic prostheses at infectious risk, and 76.5% reported having managed such patients for dental procedures. AP was prescribed in 47.1% of cases. Table 2 summarizes the clinical situations in which AP was systematically prescribed.
 |
Table 2 Procedures for Which AP Was Systematically Used |
The most commonly prescribed antibiotic was amoxicillin at a dosage of 2g in 25.5% of cases. Among dentists prescribing AP, 70.8% administered it one hour before the procedure. Factors influencing AP prescription are summarized in Table 3.
 |
Table 3 Factors Influencing the Use of AP |
Compared to similar studies conducted in India,10 Canada,11 and the United States,12 the AP prescription rate among Moroccan dentists was relatively lower. This may reflect better adherence to recent recommendations among younger professionals or a variation in educational curricula. These findings emphasize the need for clearer national guidelines in Morocco, aligned with international standards, to unify clinical decision making across regions.
The observed gender difference in AP prescription may reflect divergent risk perception or differences in training exposure. However, the underlying causes remain unclear and warrant further exploration. More experienced dentists may rely on earlier acquired habits or outdated sources of information, as continuing education appears to be underutilized.
Discussion
In dentistry, the management of patients with joint prostheses has been a widely debated topic. Prosthetic joint infections (PJI) can occur at various stages post-surgery, and it has been suggested that infectious foci of dental origin may increase the risk of these complications.
Over time, guidelines regarding the management of these patients have evolved significantly, ranging from systematic antibiotic prophylaxis (AP) to its contraindication, with some recommendations advocating selective indication for patients presenting with specific risk factors. The lack of strong evidence supporting AP and the existence of presumed cases of dental-origin infections have prevented the establishment of definitive guidelines on this subject. Current data remain insufficient to justify the routine use of AP in these patients, leading recommendations to favor an individualized decision-making process based on a risk-benefit analysis, considering the patient’s associated comorbidities.4–9
In our study, 47.1% of dentists reported using AP for patients with joint prostheses. However, our findings do not align with similar studies conducted elsewhere. Studies by Rela et al (2021) in India,10 Teixeira et al,12 Spittle et al,13 and Colterjohn et al11 reported AP prescription rates of 60%, 76.1%, 72%, and 71.5%, respectively. This discrepancy may be attributed to the younger age group in our sample, which is more likely to have been trained based on recent guidelines discouraging systematic AP use. A statistically significant correlation (p=0.002) was observed, showing that dentists with more than 20 years of experience prescribed AP more frequently than their less experienced counterparts, consistent with findings by Epstein et al.14
Additionally, female practitioners were more likely to prescribe AP than male dentists (p=0.047), possibly due to a greater sense of security associated with antibiotic coverage.
Regarding sources of information used by our sample for the management of patients with joint prostheses, 62.7% of dentists reported relying on initial professional training, while 64.7% consulted the treating orthopedic surgeon. Conversely, continuing education (30.4%), scientific society guidelines (31.4%), and conference participation (15.7%) were less frequently cited as primary sources of information. As a result, outdated recommendations continue to influence clinical decisions, leading to the persistent use of AP. A statistically significant difference (p=0.017) was observed between dentists who did not consider official recommendations as a primary source of information and those who systematically prescribed AP for endodontic treatments.
Invasive dental procedures such as subgingival caries treatment, rubber dam placement, matrix system application, and endodontic therapy are associated with transient bacteremia. However, this does not justify the routine use of AP in patients with joint prostheses.
According to a study by Kao et al,15 invasive dental treatments were not associated with an increased risk of PJI in patients who had undergone hip or knee arthroplasty. Moreover, prophylactic antibiotic use did not reduce infection risk. Instead, underlying comorbidities, such as chronic pulmonary disease and chronic liver disease, were identified as independent risk factors for prosthetic joint infections.
In our sample, 65.2% of dentists reported using AP for subgingival or proximal caries treatment, with 28.3% applying it systematically and 36.9% prescribing it only for high-risk patients. These findings contrast with those of Palmer,16 where only 13.5% of practitioners prescribed AP in similar cases. Furthermore, 27.3% of our sample reported using AP for occlusal caries treatment, likely due to the perception that subgingival procedures induce a higher risk of bacteremia than occlusal restorations.
Similarly, in our study, the use of AP in endodontic procedures was found to be diagnosis-dependent. Dentists more frequently prescribed AP for infectious endodontic conditions such as acute serous cellulitis (70.7%), collected cellulitis (65.9%), and acute apical periodontitis with abscess formation (73.7%), compared to inflammatory conditions such as pulpitis (50%) and early-stage acute apical periodontitis (57.1%). These findings differ from those of Rela et al10 and Palmer et al,16 where 92% and 17.2% of dentists, respectively, systematically prescribed AP for orthograde endodontic treatment.
A study by Springer et al17 found no significant association between invasive dental procedures and PJI, further questioning the justification for AP in patients with joint prostheses. Considering the costs, potential side effects, risks of antibiotic resistance, and unnecessary exposure, routine AP use should be reconsidered.18
Although a statistically significant gender-based difference was observed, the practical impact of this finding remains uncertain and should be interpreted with caution.
Dentists with over 20 years of experience may not have benefited from recent updates or may lack access to structured continuing education resources. Cultural or institutional inertia may also contribute to the persistence of outdated practices.
These findings highlight the need for targeted policies to reinforce continuing education, particularly on evolving AP guidelines. Dental education curricula should integrate updated infection risk frameworks in collaboration with orthopedic specialists.
This study has limitations, including potential self-reporting bias, as participants may overstate guideline adherence. Moreover, the sample is limited to urban areas in Morocco, which may not represent rural or other regional contexts.
Conclusion
This KAP study reveals a low level of knowledge among dentists regarding the management of patients with joint prostheses, along with inconsistent attitudes and practices influenced by factors such as gender, years of experience, and information sources. Despite current guidelines contraindicating the routine use of antibiotic prophylaxis (AP) in these patients, many practitioners continue to rely on outdated recommendations. This misalignment highlights the urgent need for targeted educational interventions and updated, evidence-based clinical guidelines.
Clear and standardized national guidelines are essential to prevent the unjustified overprescription of antibiotics and to address the rising concern of antimicrobial resistance. Dentists must also be made aware of the limited benefits and potential risks associated with unnecessary AP use, and the importance of lifelong oral hygiene to reduce bacterial load and prevent postoperative infections.
To promote consistent, guideline-concordant care, we recommend that national health authorities implement mandatory continuing education modules and that collaborative initiatives be established between dental and orthopedic societies. These joint efforts will help harmonize professional understanding of infection risks and ensure improved patient outcomes across disciplines.
Ethical/Copyright Corrections
This study did not undergo review by an institutional review board or ethics committee, as it was not deemed necessary given the nature of the research. The questionnaire was sent to practitioners with a clear explanation of the study’s objectives and assurance of participant anonymity. Participation was entirely voluntary, and informed consent was implied through the completion and return of the questionnaire.
Funding
There is no funding to report.
Disclosure
None of the authors reported any disclosures.
References
1. Orthopedic Surgery – global Trends & Opportunities. Research and Markets. Life Science Intelligence. 2018;4825313.
2. Steven K, Kevin O, Edmund L, Fionna M, Michael H. Projections of Primary and Revision Hip and Knee Arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. doi:10.2106/00004623-200704000-00012
3. Florschutz Anthony V, Parslez Brian S, Shapiro Irving M. Capturing orthopaedic surgical site infection data and assessing dental recommendations with respect to total joint arthroplasty. J Am Acad Orthop Surg. 2015;23:S55–9. doi:10.5435/JAAOS-D-14-00419
4. Heather Y, Joel H, Mark HE, Price Connie S. Dental disease and periprosthetic joint infection. J Bone Joint Surg Am. 2014;96(2):162–168. doi:10.2106/JBJS.L.01379
5. Nixil. Prescription des antibiotiques en pratique bucco-dentaire. AFSSAPS juillet. 2011;2011:1.
6. Shah Neel B, Tande Aaron J, Robin P, Berbari Elie F. Anaerobic prosthetic joint infection. Anaerobe. 2015;36:1–8. Epub 2015 Sep 1. PMID: 26341272. doi:10.1016/j.anaerobe.2015.08.003.
7. Canovas F, Dagneaux L. Quality of life after total knee arthroplasty. Orthop Traumatol Surg Res. 2018;104(1S):S41–S46. Epub 2017 Nov 26. PMID: 29183821. doi:10.1016/j.otsr.2017.04.017.
8. LaPorte DM, Waldman BJ, Mont MA, Hungerford DS. Infections associated with dental procedures in total Hip arthroplasty. J Bone Joint Surg Brit. 1999;81:56–59. doi:10.1302/0301-620X.81B1.0810056
9. American Dental Association. American Academy of Orthopedic Surgeons: antibiotic prophylaxis for dental patients with total joint replacements. J Am Dent Assoc. 2003;134(7):895–899. doi:10.14219/jada.archive.2003.0289
10. Rela R, Sejao AV, Singh A. Antibiotic Prescribing Knowledge, Awareness, and Attitude of Dental Surgeons Practicing in the Urban Indian Population. J Pharm Bioallied Sci. 2021;13(Suppl 2):S1637–S1641. doi:10.4103/jpbs.jpbs_394_21
11. Tristan C, de Beer J, Danielle P, Nazar Z, Mitch W. Antibiotic prophylaxis for dental procedures at risk of causing bacteremia among post-total joint arthroplasty patients: a survey of Canadian orthopaedic surgeons and dental surgeons. J Arthroplasty. 2014;29(6):1091–1097. doi:10.1016/j.arth.2013.11.024
12. Teixeira Erica C, Warren John J, McKernan Susan C, McQuistan Michelle R, Fang Q. Prescribing practices for antibiotic prophylaxis in patients with prosthetic joints. Spec Care Dentist. 2020;40(2):198–205. doi:10.1111/scd.12450
13. Spittle Lea S, Muzzin Kathleen B, Campbell Patricia R, DeWald Janice P, Francisco R-H. Current prescribing Practices for Antibiotic Prophylaxis: a Survey of Dental Practitioners. J Contemporary Dental Pract. 2017;18(7):559–566. doi:10.5005/jp-journals-10024-2084
14. Epstein Joel B, Sandra C, Le Nhu D. A survey of antibiotic use in dentistry. J Am Dent Assoc. 2000;131(11):1600–1609. doi:10.14219/jada.archive.2000.0090
15. Feng-Chen K, Yao-Chun H, Wen-Hui C, Jiun-Nong L, Ying-Ying L, Yuan-Kun T. Prosthetic Joint Infection Following Invasive Dental Procedures and Antibiotic Prophylaxis in Patients With Hip or Knee Arthroplasty. Infect Control Hosp Epidemiol. 2017;38(2):154–161. Epub 2016 Nov 9. PMID: 27825396. doi:10.1017/ice.2016.248.
16. Palmer NA, Pealing R, Ireland RS, Martin MV. A study of prophylactic antibiotic prescribing in National Health Service general dental practice in England. Br Dent J. 2000;189(1):43–46. PMID: 10967824. doi:10.1038/sj.bdj.4800597.
17. Springer Bryan D, Baddour Larry M, Lockhart Peter B, Thornhill Martin H. Antibiotic Prophylaxis for Prosthetic Joint Patients Undergoing Invasive Dental Procedures: time for a Rethink? J Arthroplasty. 2022;37(7):1223–1226. Epub 2022 Feb 11. PMID: 35158002. doi:10.1016/j.arth.2022.02.014.
18. Thornhill Martin H, Gibson Teresa B, Cory P, et al. Quantifying the risk of prosthetic joint infections after invasive dental procedures and the effect of antibiotic prophylaxis. J Am Dent Assoc. 2023;154(1):43–52.e12. Epub 2022 Dec 2. PMID: 36470690. doi:10.1016/j.adaj.2022.10.001.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Health Literacy Among University Students in Shaanxi Province of China: A Cross-Sectional Study
Wu S, Shao B, Wang G
Risk Management and Healthcare Policy 2023, 16:865-878
Published Date: 11 May 2023
Knowledge, Attitudes, and Practices Among Patients with Systemic Lupus Erythematosus Toward Disease Management and Biologic Therapy
Liu X, Song Y, Wan L, Du R
Journal of Multidisciplinary Healthcare 2024, 17:937-947
Published Date: 2 March 2024
Knowledge, Attitudes, and Practices Among Elderly CHD Patients Towards Self-Perceived Health Abilities
Ren L, Li Z, Wu J, Duan L, Gao J
Journal of Multidisciplinary Healthcare 2024, 17:1999-2011
Published Date: 1 May 2024
Knowledge, Attitudes, and Practices Among Community Populations Toward Long COVID in China
He N, Tunala S, Wu R, Zhao C, Wuren T, Hushuud C
International Journal of General Medicine 2024, 17:4455-4463
Published Date: 1 October 2024
Knowledge, Attitudes, and Practices Regarding Swallowing Disorders Among General Practitioners
Zou M, Zhu X, Li J, Yu H, Guo P
International Journal of General Medicine 2025, 18:1555-1567
Published Date: 18 March 2025

