Back to Journals » Therapeutics and Clinical Risk Management » Volume 21
Application of Perioperative Nursing Based on Enhanced Recovery After Surgery (ERAS) Principles in Patients Undergoing Total Knee Arthroplasty
Received 6 January 2025
Accepted for publication 5 April 2025
Published 31 May 2025 Volume 2025:21 Pages 829—839
DOI https://doi.org/10.2147/TCRM.S515992
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Juan Huang,1 Guoqing Wu,2 Xiaohong Li1
1Department of Orthopedics, Dazhou Central Hospital, Dazhou City, Sichuan Province, 635000, People’s Republic of China; 2Department of Medical Insurance Management, Dazhou Central Hospital, Dazhou City, Sichuan Province, 635000, People’s Republic of China
Correspondence: Juan Huang, Department of Orthopedics,Dazhou Central Hospital, No. 61 Tongchuan North Road, Tongchuan District, Dazhou City, Sichuan Province, 635000, People’s Republic of China, Email [email protected]
Background: Enhanced Recovery After Surgery (ERAS) principles have gained widespread adoption in perioperative care to optimize recovery and reduce complications. Total knee arthroplasty (TKA) patients benefit significantly from ERAS-guided strategies, which minimize surgical stress and accelerate postoperative recovery. This study evaluates the application of perioperative nursing care based on ERAS principles and its impact on TKA patients.
Methods: A retrospective analysis was conducted on prospectively maintained data of 312 patients who underwent TKA between January 2023 and December 2023. Of these, 158 patients received perioperative nursing care based on ERAS principles, while 154 received standard nursing care. The ERAS-based perioperative nursing protocol included preoperative education, intraoperative fluid optimization, postoperative pain management, and early mobilization strategies. Clinical data, including postoperative complications, length of hospital stay, and patient satisfaction, were collected and compared between the two groups using statistical methods.
Results: Patients in the ERAS-based nursing group exhibited significantly better outcomes compared to the standard care group. Postoperative complications, such as deep vein thrombosis and infections, were reduced (4.4% vs 11.7%, P< 0.05), and the average length of hospital stay was shorter (5.6 ± 1.8 days vs 8.3 ± 2.4 days, P< 0.001). Patient satisfaction scores were notably higher in the ERAS group (94.3% vs 78.6%, P< 0.001). Multivariate analysis identified perioperative nursing based on ERAS principles as an independent factor for improved recovery.
Conclusion: Perioperative nursing care guided by ERAS principles significantly improves clinical outcomes in TKA patients, reducing complications and hospital stay while enhancing patient satisfaction. This study supports the broader implementation of ERAS protocols in perioperative nursing to optimize surgical care outcomes.
Keywords: enhanced recovery after surgery, perioperative nursing, total knee arthroplasty, patient outcomes, complication reduction, early mobilization, pain management, nursing protocols
Introduction
Total knee arthroplasty (TKA) is a widely performed surgical procedure that significantly improves the quality of life for patients suffering from advanced knee osteoarthritis and other degenerative joint diseases.1–3 However, despite its benefits, TKA is associated with substantial perioperative challenges, including postoperative pain, complications such as infections or deep vein thrombosis, and prolonged recovery periods.4,5 Enhanced Recovery After Surgery (ERAS) principles, initially developed for colorectal surgery, have been increasingly applied to orthopedic procedures, including TKA, to address these challenges and improve patient outcomes.6,7
ERAS principles encompass a comprehensive, multidisciplinary approach that integrates preoperative, intraoperative, and postoperative strategies aimed at reducing surgical stress, optimizing recovery, and enhancing overall patient satisfaction.8 Evidence from previous studies highlights the benefits of ERAS protocols. For instance, Kehlet and Wilmore9 identified the reduction of surgical stress and inflammation as central to ERAS success, particularly in improving postoperative recovery trajectories. Similarly, Salamanna et al10 conducted a review which concluded that ERAS protocols can improve recovery in orthopedic surgeries, reducing length of hospital stay (LOS) and readmission rates. The successful application of ERAS relies heavily on effective perioperative nursing care, which is instrumental in facilitating patient education, managing postoperative pain, and promoting early mobilization.11 Nurses play a pivotal role in implementing ERAS protocols. According to Auyong et al12 perioperative nursing strategies that focus on individualized care plans significantly enhance patient adherence to ERAS protocols, leading to better clinical outcomes. In contrast, Ripollés-Melchor et al13 pointed out that inconsistent nursing practices and lack of standardized protocols can undermine the effectiveness of ERAS interventions, resulting in variable patient outcomes. ERAS is a multimodal perioperative care pathway aimed at optimizing recovery and reducing postoperative complications. ERAS protocols typically involve several key interventions, including preoperative education, intraoperative fluid management, postoperative pain control using multimodal analgesia, early mobilization within 24 hours post-surgery, and nutritional support to facilitate healing. The goal of ERAS is to minimize surgical stress, enhance recovery, and improve patient outcomes by standardizing and optimizing perioperative care.
Our hypothesis is that the application of ERAS principles in patients undergoing total knee arthroplasty (TKA) will lead to improved postoperative outcomes, including reduced hospital stay, lower complication rates, and enhanced patient satisfaction compared to standard care. Despite the potential of ERAS to enhance patient outcomes, a notable gap remains in standardized perioperative nursing protocols tailored specifically to TKA patients. Addressing this gap is crucial to ensuring consistent and effective implementation of ERAS principles in clinical practice. This study aims to evaluate the impact of perioperative nursing care based on ERAS principles on clinical outcomes in TKA patients. By focusing on the integration of preoperative education, intraoperative support, and postoperative rehabilitation, this research seeks to provide evidence-based insights into optimizing nursing protocols and improving patient care in TKA.
Materials and Methods
Patient Selection Study Design and Participants
This retrospective cohort study was designed to assess the impact of perioperative nursing care based on Enhanced Recovery After Surgery (ERAS) principles on the outcomes of patients undergoing total knee arthroplasty (TKA). The study included adult patients (18 years or older) who underwent TKA between January 2023 and December 2023. Inclusion criteria were: (1) patients aged 18 years or older, (2) primary TKA performed due to degenerative joint diseases, and (3) complete clinical data availability. Exclusion criteria included: (1) revision TKA procedures, (2) significant comorbidities that could influence outcomes (eg, severe cardiovascular or renal diseases) that might complicate the postoperative course and confound the analysis of perioperative nursing interventions, (3) patient refusal to follow postoperative care protocols, (4) low educational levels or inability to comprehend the ERAS protocol. Patients with controlled chronic conditions, such as hypertension and diabetes, were not excluded and participated in the ERAS pathway under close medical supervision. The study was approved by the Ethics Committee of Dazhou Central Hospital and conducted in accordance with the Declaration of Helsinki (Approval Number: 202305061354). Informed consent was obtained from all participants. This study was conducted following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines to ensure the completeness and transparency of reporting.
ERAS-Based Perioperative Nursing Interventions
Patients were admitted prior to the day of surgery to allow for thorough preoperative preparation, including patient education, anesthesia evaluation, and optimization of perioperative care. Patients in the ERAS group received comprehensive perioperative nursing interventions aligned with Enhanced Recovery After Surgery (ERAS) principles.
Preoperative Education
Nursing staff conducted structured educational sessions twice a week for two weeks before surgery; Patients and their families were provided with a detailed “TKA Recovery Guide”, covering preoperative preparation, pain management techniques, early mobilization importance, and potential complications; Sessions included interactive Q&A and hands-on demonstrations, such as using walkers or crutches.
Intraoperative Fluid Optimization
Nurses collaborated with anesthesiologists to maintain intraoperative fluid balance; Advanced monitoring tools were used to track patients’ fluid status, ensuring optimal hydration while avoiding fluid overload; Individualized protocols were applied based on patient-specific factors, including body weight and comorbidities.
Postoperative Pain Management
A multimodal approach was implemented, combining regional anesthesia (eg, femoral nerve blocks), non-opioid analgesics (eg, acetaminophen, NSAIDs), and patient-controlled analgesia (PCA) for breakthrough pain; Nurses closely monitored pain levels using validated scales, such as the Visual Analog Scale (VAS), adjusting interventions as needed. Postoperative pain levels were assessed using the VAS, which ranged from 0 (no pain) to 10 (worst pain imaginable). Pain scores were recorded on postoperative Days 1 and 3. Quality of life was evaluated using the Short Form-36 (SF-36) Health Survey, which consists of physical and mental component scores, and the EuroQol-5 Dimension (EQ-5D) index, which measures general health status and recovery outcomes. Both assessments were conducted at the time of hospital discharge and during follow-up.
Early Mobilization Strategies
Mobilization began within 24 hours post-surgery under nursing supervision; Nurses guided patients through light exercises, such as ankle pumps, isometric quadriceps contractions, and assisted walking with aids; Physiotherapists collaborated with nurses to develop individualized exercise plans to restore joint mobility and strength.
Nutritional Support
Postoperative nutrition was emphasized, with early oral intake encouraged to promote recovery; Nurses provided dietary advice, including protein-rich and easily digestible meals, to support wound healing and energy restoration.
Proactive Monitoring and Complication Prevention
Nurses regularly assessed for signs of complications, including deep vein thrombosis (DVT), using ultrasound and clinical observation; Preventive measures, such as compression stockings and anticoagulants, were administered according to protocol.
Standard Care
Patients in the standard care group received conventional nursing interventions commonly practiced for TKA patients.
Basic Preoperative Preparation
Routine instructions were provided on the day before surgery, including fasting requirements and hygiene practices; No additional educational materials or interactive sessions were offered.
Intraoperative Care
Standard fluid management was performed based on conventional clinical guidelines without individualized optimization.
Postoperative Pain Management
Pain control relied primarily on opioid-based medications administered as needed; Minimal use of multimodal analgesia strategies.
Postoperative Mobilization
Mobilization was initiated on postoperative day two or three, depending on the patient’s condition; Basic exercises were demonstrated once daily without a structured or individualized plan.
Nutritional Support
Postoperative dietary advice was limited to general recommendations, and oral intake was delayed until bowel function returned.
Monitoring and Complication Management
Nurses monitored patients routinely but without proactive protocols for complication prevention; Compression stockings were applied, but advanced assessments for DVT or other complications were not routinely performed.
Patient Satisfaction Score
Patient satisfaction was assessed using a validated questionnaire that measured aspects such as pain management, nursing care, and overall recovery. Patients rated their satisfaction on a scale from 1 (very dissatisfied) to 5 (very satisfied). The overall satisfaction score was calculated as the average of the individual responses. Satisfaction was categorized as “satisfied” (≥4) or “not satisfied” (<4) based on the average score.
Data Collection and Outcome Measures
Clinical data were retrospectively collected from electronic medical records and independently verified by two researchers to ensure accuracy. Primary outcomes included the length of hospital stay, postoperative complications (eg, infections, deep vein thrombosis), and patient satisfaction scores. Secondary outcomes focused on readmission rates and recovery milestones, such as time to independent ambulation and the ability to perform activities of daily living (ADLs).
Physiological System Monitoring
Postoperative complications were categorized and analyzed across key physiological systems: Circulatory System: Monitoring of blood pressure, heart rate, and any cardiovascular events; Urinary System: Evaluation of urine output, renal function, and occurrence of urinary tract infections; Digestive System: Assessment of gastrointestinal complications, nutritional intake, and bowel function; Coagulation System: Analysis of thrombotic events, such as deep vein thrombosis, and coagulation profiles.
Data Analysis
Descriptive statistics were utilized to summarize baseline characteristics and clinical outcomes. Continuous variables, such as the duration of hospital stay, were analyzed using t-tests or non-parametric methods, while categorical variables, such as complication rates, were compared using chi-square or Fisher’s exact tests. To analyze factors associated with shorter hospital stays, a binary classification was applied, defining a short hospital stay as ≤5 days based on the median hospital stay in the study population. The multivariable logistic regression model included the following variables: ERAS-based care, presence of preoperative comorbidities, age (>65 years), BMI (>30 kg/m²), baseline pain score (VAS >7), hypertension, diabetes, preoperative albumin levels (<40 g/L), smoking history, and history of previous knee surgery. To avoid multicollinearity, early mobilization was excluded from the multivariable model, as it is an inherent component of ERAS-based care. Multivariable regression analysis was performed to adjust for potential confounding factors, including age, gender, and comorbidities. Statistical analyses were conducted using SPSS 25.0 (IBM, Armonk, NY, USA), with a significance threshold of P<0.05. Data visualizations were created using R (version 4.0.5) and GraphPad Prism (version 8.0).
Results
Baseline Information of TKA Patients with ERAS-Based Perioperative Nursing and Standard Care
The inclusion and exclusion criteria are detailed in Figure 1. A total of 312 patients undergoing total knee arthroplasty (TKA) were included, with 158 receiving ERAS-based perioperative nursing and 154 receiving standard care. Both groups were comparable in terms of baseline characteristics, including gender distribution, age, body mass index (BMI), pre-existing comorbidities (eg, diabetes, hypertension), and American Society of Anesthesiologists (ASA) physical status classification (P > 0.05).
 |
Figure 1 Inclusion and exclusion table for patients undergoing total knee arthroplasty. |
Notably, the ERAS group had a slightly higher proportion of patients with ASA Class II (62.5% vs 58.4%) and preoperative joint stiffness (51.9% vs 48.1%) compared to the standard care group. However, these differences were not statistically significant. The median values for systolic blood pressure, diastolic blood pressure, heart rate, and body temperature were also similar between the two groups (Table 1).
 |
Table 1 Baseline Characteristics of TKA Patients |
Univariate and Multivariate Analyses of Factors Associated with Shorter Hospital Stay in TKA Patients
Logistic regression analyses were performed to identify significant predictors. In the univariate analysis, factors significantly associated with a shorter hospital stay included ERAS-based perioperative nursing (P<0.001, OR=3.012, 95% CI: 2.214–4.099), early mobilization within 24 hours postoperatively (P<0.001, OR=2.658, 95% CI: 1.957–3.611), and the absence of preoperative comorbidities (P=0.021, OR=1.583, 95% CI: 1.071–2.340). Other variables, such as gender, age, and BMI, were not significantly associated with shorter hospital stays (P > 0.05). After adjusting for potential confounders in the multivariate analysis, ERAS-based perioperative nursing (P<0.001, OR=3.312, 95% CI: 2.316–4.737) and early mobilization within 24 hours (P<0.001, OR=2.472, 95% CI: 1.766–3.461) remained independently associated with shorter hospital stays, whereas the absence of preoperative comorbidities was not a significant independent predictor (P=0.076). These findings highlight the critical roles of ERAS-based nursing and early mobilization in facilitating shorter recovery times for TKA patients (Table 2).
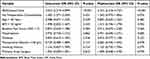 |
Table 2 Univariate and Multivariate Logistic Regression Analysis for Shorter Hospital Stay (≤5 Days) |
Complications in TKA Patients Receiving ERAS-Based Perioperative Nursing Versus Standard Care
The incidence of postoperative complications differed significantly between the ERAS and standard care groups. Patients in the ERAS group had fewer complications, Deep vein thrombosis (2.5% vs 8.4%, P=0.018), Postoperative infections (1.3% vs 7.1%, P=0.011), Delayed wound healing (0.6% vs 6.5%, P=0.005), Patients in the ERAS group also had significantly shorter hospital stays (5.6 ± 1.8 days vs 8.3 ± 2.4 days, P<0.001). Furthermore, their pain scores measured by the Visual Analog Scale (VAS) on postoperative days 1 and 3 were significantly lower (Day 1: 3.8 ± 1.2 vs 5.4 ± 1.5, P<0.001; Day 3: 2.6 ± 0.8 vs 4.1 ± 1.2, P<0.001).
No significant differences were observed in urinary, gastrointestinal, or coagulation-related complications between the two groups (Table 3). Multivariable logistic regression was performed to assess the association between ERAS-based nursing and the overall complication rate. The results showed that ERAS-based perioperative nursing was independently associated with a significantly lower risk of complications (OR = 0.42, 95% CI: 0.27–0.68, P < 0.001). (Table 4).
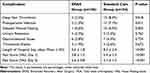 |
Table 3 Postoperative Complications in TKA Patients |
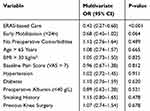 |
Table 4 Multivariable Logistic Regression Analysis for Overall Complications |
Comparison of Clinical Recovery Outcomes between ERAS-Based and Standard Care Groups
Patients in the ERAS group achieved functional recovery milestones significantly faster than those in the standard care group. The time to first ambulation was notably shorter in the ERAS group (24.3 ± 5.6 hours vs 48.7 ± 7.2 hours, P<0.001), patient satisfaction scores were substantially higher (94.3% vs 78.6%, P<0.001), and they achieved independent walking with assistive devices earlier (3.2 ± 0.9 days vs 5.1 ± 1.2 days, P<0.001). Furthermore, the readmission rate was significantly lower in the ERAS group (6.3% vs 12.9%, P=0.024). (Table 5).
 |
Table 5 Functional Recovery and Patient Satisfaction Outcomes |
Patient-Reported Functional Recovery and Quality of Life Outcomes
Patients in the ERAS group demonstrated superior self-reported functional recovery and quality of life compared to those in the standard care group. The SF-36 physical component scores were significantly higher in the ERAS group (75.4 ± 10.2 vs 68.3 ± 11.5, P<0.001), as were the SF-36 mental component scores (78.6 ± 9.8 vs 72.4 ± 10.3, P<0.001). The EQ-5D index also favored the ERAS group (0.87 [0.82–0.91] vs 0.79 [0.73–0.85], P=0.015). Furthermore, a higher proportion of patients in the ERAS group returned to work or normal activities within the follow-up period (79.1% vs 66.2%, P=0.041) (Table 6).
 |
Table 6 Patient-Reported Outcomes Comparing ERAS and Standard Care Groups |
Discussion
Total knee arthroplasty (TKA) is considered a major surgical procedure in orthopedics, associated with significant risks such as postoperative infections, deep vein thrombosis, and prolonged recovery periods. As highlighted in recent RCT,14 the complexity of TKA surgery can conceal several critical complications, necessitating the use of evidence-based perioperative strategies to minimize risks. Enhanced Recovery After Surgery (ERAS) protocols have been increasingly recognized as a key intervention in optimizing recovery, reducing complications, and improving long-term functional outcomes in patients undergoing TKA.
TKA is also a common surgical procedure aimed at improving the quality of life for patients with severe joint disease.15–18 However, optimizing recovery and minimizing complications remain key challenges in perioperative care. Our study demonstrates that ERAS-based perioperative nursing significantly improves recovery metrics, reduces complications, and enhances patient satisfaction compared to standard care. These findings are consistent with growing evidence supporting the use of ERAS principles in surgical nursing.
One of the primary findings of our study is the significant reduction in postoperative complications in the ERAS group, including deep vein thrombosis, infections, and delayed wound healing. This reduction underscores the effectiveness of ERAS protocols in mitigating perioperative risks. Salamanna et al10 reported similar results, finding that ERAS protocols reduced complication rates and enhanced functional recovery in orthopedic surgery. Noba et al19 demonstrated that the introduction of ERAS protocols in liver resection was both safe and feasible, reducing LOS and complication risks without increasing mortality or readmission rates, while significantly cutting hospital costs. Tazreean et al20 highlighted that early mobilization, a key component of the ERAS pathway, helps counteract the adverse physiological effects of surgical stress and immobilization. The improved outcomes in our study may be attributed to comprehensive nursing interventions, such as early mobilization, personalized pain management, and preoperative patient education, which are core components of the ERAS protocol. In addition to fewer complications, patients in the ERAS group achieved faster recovery milestones, including earlier ambulation and shorter hospital stays. Compared to standard care, the ERAS group’s hospital stays were reduced by nearly 3 days on average (5.6 ± 1.8 days vs 8.3 ± 2.4 days, P<0.001). This reduction not only decreases medical costs but also alleviates the psychological and emotional burden on patients and their families. These findings align with a meta-analysis by Sauro et al21 which reported that the application of ERAS guidelines in various conditions was associated with reduced hospital stays and complications. Recent studies have further validated the benefits of ERAS protocols in orthopedic surgery. Research has shown that ERAS significantly reduces hospital length of stay and readmission rates, particularly when multimodal pain management and early mobilization are effectively implemented. Furthermore, some systematic review highlighted that ERAS pathways not only reduce complications but also contribute to improved long-term functional recovery and patient satisfaction.22,23 These findings align with our results, reinforcing the importance of ERAS as a standardized approach for perioperative nursing care in TKA.
Our study also highlights significant improvements in patient-reported outcomes in the ERAS group. Patients in this group reported higher scores in both the physical and psychological components of the SF-36 and better overall health status as measured by the EQ-5D index. Similarly, Zhang et al24 demonstrated that ERAS significantly improved ROM, SF-36 BP, and SF-36 PF scores. Additionally, a higher proportion of ERAS patients returned to work or daily activities during the follow-up period, reflecting the holistic benefits of ERAS-based perioperative nursing. These findings underscore the importance of integrating patient-centered care into surgical protocols to achieve optimal outcomes. Our findings align with previous studies investigating ERAS pathways in orthopedic surgery within China. Wei et al25 demonstrated that an ERAS protocol applied to TKA via the midvastus approach resulted in a similar reduction in hospital stay and improved functional recovery, supporting our results. Wu et al26 explored ERAS in TKA patients with hemophilia A, confirming that ERAS is safe and feasible even in complex patient populations, reinforcing the broader applicability of these protocols. Zhang evaluated a fast-track surgery approach combined with a nursing pathway in THA,27 reporting shorter hospital stays and improved rehabilitation outcomes, which is consistent with our findings on the role of perioperative nursing in enhancing recovery.
However, our study is not without limitations. First, the retrospective design limits the ability to establish causal relationships between ERAS interventions and improved outcomes. Second, the study was conducted at a single institution, which may affect the generalizability of the findings. Future research should focus on multicenter, prospective studies to validate these results and explore their applicability across different healthcare settings. Furthermore, demographic and geographic differences, such as variations in healthcare access and population characteristics, may influence the effectiveness of ERAS protocols. Exploring these factors in future research will help refine care protocols and expand the applicability of ERAS-based perioperative nursing. Lastly, one limitation of this study is the variability in compliance with certain ERAS components. While the protocol recommended early mobilization within 24 hours, this was achieved in 87.3% of patients in the ERAS group, with a mean ambulation time of 24.3 ± 5.6 hours. Compliance with multimodal pain management was 94.1%, while 98.7% of patients completed preoperative education, and 92.5% adhered to nutritional support recommendations. While overall adherence was high, minor deviations in mobilization timing may have influenced recovery outcomesOur findings highlight the need for evidence-based guidelines to ensure consistent and effective application of ERAS principles. The development of standardized nursing protocols could further optimize recovery and improve outcomes for TKA patients.
Despite these limitations, our study has several strengths, including a relatively large sample size, a real-world evaluation of ERAS implementation, and a focus on perioperative nursing interventions that have not been extensively studied in previous research. Moving forward, future research should focus on conducting multicenter prospective studies and randomized controlled trials to validate our findings. Additionally, exploring modifications to ERAS protocols tailored to specific patient populations, such as elderly or high-risk individuals, could further optimize recovery and patient outcomes.
Conclusion
In summary, our study demonstrates that ERAS-based perioperative nursing significantly improves postoperative recovery and patient outcomes in TKA patients. These interventions not only reduce complication rates and shorten hospital stays but also enhance patient satisfaction and quality of life. These findings provide compelling evidence for integrating ERAS principles into perioperative nursing care.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval and Consent to Participation
Written informed consent was obtained from all participants. This research was performed in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Dazhou Central Hospital.
Acknowledgments
Thanks to the nurses in the department for their help with the project.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Fortier LM, Rockov ZA, Chen AF, Rajaee SS. Activity recommendations after total hip and total knee arthroplasty. J Bone Joint Surg Am Vol. 2021;103(5):446–455. doi:10.2106/JBJS.20.00983
2. Gränicher P, Mulder L, Lenssen T, Scherr J, Swanenburg J, de Bie R. Prehabilitation improves knee functioning before and within the first year after total knee arthroplasty: a systematic review with meta-analysis. J Orthop Sports Phys Ther. 2022;52(11):709–725. doi:10.2519/jospt.2022.11160
3. Oussedik S, Abdel MP, Victor J, Pagnano MW, Haddad FS. Alignment in total knee arthroplasty. Bone Joint J. 2020;102-b(3):276–279. doi:10.1302/0301-620X.102B3.BJJ-2019-1729
4. Lavand’homme PM, Kehlet H, Rawal N, Joshi GP. Pain management after total knee arthroplasty: procedure specific postoperative pain management recommendations. Eur J Anaesthesiol. 2022;39(9):743–757. doi:10.1097/EJA.0000000000001691
5. Lavie LG, Fox MP, Dasa V. Overview of total knee arthroplasty and modern pain control strategies. Curr Pain Headache Rep. 2016;20(11):59. doi:10.1007/s11916-016-0592-6
6. Morrell AT, Layon DR, Scott MJ, Kates SL, Golladay GJ, Patel NK. Enhanced recovery after primary total hip and knee arthroplasty: a systematic review. J Bone Joint Surg Am Vol. 2021;103(20):1938–1947. doi:10.2106/JBJS.20.02169
7. Ripollés-Melchor J, Abad-Motos A, Díez-Remesal Y, et al. Association between use of enhanced recovery after surgery protocol and postoperative complications in total hip and knee arthroplasty in the postoperative outcomes within enhanced recovery after surgery protocol in elective total hip and knee arthroplasty study (POWER2). JAMA Surgery. 2020;155(4):e196024. doi:10.1001/jamasurg.2019.6024
8. Scott MJ, Baldini G, Fearon KC, et al. Enhanced Recovery After Surgery (ERAS) for gastrointestinal surgery, part 1: pathophysiological considerations. Acta anaesthesiologica Scandinavica. 2015;59(10):1212–1231. doi:10.1111/aas.12601
9. Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg. 2002;183(6):630–641. doi:10.1016/S0002-9610(02)00866-8
10. Salamanna F, Contartese D, Brogini S, et al. Key components, current practice and clinical outcomes of ERAS programs in patients undergoing orthopedic surgery: a systematic review. J Clin Med. 2022;11(14):4222. doi:10.3390/jcm11144222
11. Wainwright TW, Gill M, McDonald DA, et al. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery After Surgery (ERAS(®)) society recommendations. Acta orthopaedica. 2020;91(1):3–19. doi:10.1080/17453674.2019.1683790
12. Auyong DB, Allen CJ, Pahang JA, Clabeaux JJ, MacDonald KM, Hanson NA. Reduced length of hospitalization in primary total knee arthroplasty patients using an updated Enhanced Recovery After Orthopedic Surgery (ERAS) pathway. J Arthroplasty. 2015;30(10):1705–1709. doi:10.1016/j.arth.2015.05.007
13. Ripollés-Melchor J, Carli F, Coca-Martínez M, Barbero-Mielgo M, Ramírez-Rodríguez JM, García-Erce JA. Committed to be fit. The value of preoperative care in the perioperative medicine era. Minerva anestesiologica. 2018;84(5):615–625. doi:10.23736/S0375-9393.18.12286-3
14. Coviello M, Abate A, Ippolito F, et al. Continuous cold flow device following total knee arthroplasty: myths and reality. Medicina. 2022;58(11):1537.
15. Karasavvidis T, Pagan Moldenhauer CA, Haddad FS, Hirschmann MT, Pagnano MW, Vigdorchik JM. Current Concepts in Alignment in Total Knee Arthroplasty. J Arthroplasty. 2023;38(7 Suppl 2):S29–s37. doi:10.1016/j.arth.2023.01.060
16. Matassi F, Pettinari F, Frasconà F, Innocenti M, Civinini R. Coronal alignment in total knee arthroplasty: a review. J Orthop Traumatol. 2023;24(1):24. doi:10.1186/s10195-023-00702-w
17. Mosher ZA, Bolognesi MP, Malkani AL, Meneghini RM, Oni JK, Fricka KB. Cementless total knee arthroplasty: a resurgence-who, when, where, and how? J Arthroplasty. 2024;39(9s2):S45–s53. doi:10.1016/j.arth.2024.02.078
18. Pagan CA, Karasavvidis T, Cohen-Rosenblum AR, Hannon CP, Lombardi AV Jr, Vigdorchik JM. Technology in total knee arthroplasty in 2023. J Arthroplasty. 2024;39(9s2):S54–s59. doi:10.1016/j.arth.2024.07.028
19. Noba L, Rodgers S, Chandler C, Balfour A, Hariharan D, Yip VS. Enhanced Recovery After Surgery (ERAS) reduces hospital costs and improve clinical outcomes in liver surgery: a systematic review and meta-analysis. J Gastrointest Surg. 2020;24(4):918–932. doi:10.1007/s11605-019-04499-0
20. Tazreean R, Nelson G, Twomey R. Early mobilization in enhanced recovery after surgery pathways: current evidence and recent advancements. J Comp Eff Res. 2022;11(2):121–129. doi:10.2217/cer-2021-0258
21. Sauro KM, Smith C, Ibadin S, et al. Enhanced recovery after surgery guidelines and hospital length of stay, readmission, complications, and mortality: a meta-analysis of randomized clinical trials. JAMA Network Open. 2024;7(6):e2417310. doi:10.1001/jamanetworkopen.2024.17310
22. Brigato P, De Salvatore S, Oggiano L, et al. Enhanced recovery after surgery for adolescent idiopathic scoliosis: a revised systematic review and meta‑analysis. Spine Deform. 2025;13(3):647–665. doi:10.1007/s43390-025-01040-z
23. Phillips KG, Galloway A, Grossi EA, et al. Integrating quality metrics with enhanced recovery pathways in coronary artery bypass grafting. Semin Thorac Cardiovasc Surg. 2025;37(1):48–57. doi:10.1053/j.semtcvs.2025.01.002
24. Zhang Q, Chen Y, Li Y, et al. Enhanced recovery after surgery in patients after hip and knee arthroplasty: a systematic review and meta-analysis. Postgrad Med J. 2024;100(1181):159–173. doi:10.1093/postmj/qgad125
25. Wei B, Tang C, Li X, et al. Enhanced recovery after surgery protocols in total knee arthroplasty via midvastus approach: a randomized controlled trial. BMC Musculoskelet Disord. 2021;22(1):856. doi:10.1186/s12891-021-04731-6
26. Wu Y, Xue H, Zhang W, Wu Y, Yang Y, Ji H. Application of enhanced recovery after surgery in total knee arthroplasty in patients with haemophilia A: a pilot study. Nurs Open. 2021;8(1):80–86. doi:10.1002/nop2.605
27. Zhang C, Xiao J. Application of fast-track surgery combined with a clinical nursing pathway in the rehabilitation of patients undergoing total hip arthroplasty. J Int Med Res. 2020;48(1):300060519889718. doi:10.1177/0300060519889718
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

