Back to Journals » Vascular Health and Risk Management » Volume 21
AQP1 Affects Necroptosis by Targeting RIPK1 in Endothelial Cells of Atherosclerosis
Authors Wang P, Zheng L , Yang Y , Yue X, Liu J, Fan K, Zhou H, Dong H
Received 23 September 2024
Accepted for publication 1 March 2025
Published 20 March 2025 Volume 2025:21 Pages 139—152
DOI https://doi.org/10.2147/VHRM.S487327
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Pietro Scicchitano
Ping Wang,1,* Lin Zheng,1,* Yusi Yang,2,* Xinyang Yue,1 Jie Liu,3 Keyi Fan,1 Haonan Zhou,4 Honglin Dong1
1Department of Vascular Surgery, The Second Hospital of Shanxi Medical University, Taiyuan, People’s Republic of China; 2Department of Cardiology, Third Hospital of Shanxi Medical University, Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences Tongji Shanxi Hospital, Taiyuan, People’s Republic of China; 3Department of Cardiac Surgery, The Second Hospital of Hebei Medical University, Shijiazhuang, People’s Republic of China; 4Department of Vascular Surgery, Third Hospital of Shanxi Medical University, Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences Tongji Shanxi Hospital, Taiyuan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Honglin Dong, The Second Hospital of Shanxi Medical University, Taiyuan, People’s Republic of China, Email [email protected]
Purpose: Aquaporin 1 (AQP1), a transmembrane water channel protein, has been implicated in the regulation of necroptosis. However, its specific role in atherosclerotic plaque stability through the modulation of necroptosis remains unclear. Therefore, in this study, we aim to investigate whether AQP1 influences necroptosis in atherosclerosis by binding to receptor-interacting serine/threonine-protein kinase 1 (RIPK1) and decreasing the expression of receptor-interacting serine/threonine-protein kinase 3 (RIPK3) and mixed lineage kinase domain-like pseudokinase (MLKL).
Patients and Methods: The gene expression of AQP1 and necroptosis-associated genes significantly differ between atherosclerosis and normal groups. Genes linked to necroptosis were screened to influence the AS identified by weighted gene coexpression network analysis (WGCNA). Then we collected femoral atherosclerosis and normal aortic samples, further conducted single-cell sequencing and spatial transcriptomic methods to confirm the potential function and pathway of AQP1 in endothelial cells. Meanwhile, we overexpressed AQP1 in ox-LDL-treated endothelial cells in vitro.
Results: Firstly, via single-sample Gene Set Enrichment Analysis (ssGSEA) scores, we found that necroptosis plays the most important role among all ways of programmed cell death in two kinds of atherosclerosis. AQP1, RIPK1, RIPK3 and MLKL express differently in normal and atherosclerosis tissue by differentially expressed gene (DEG) analysis and Western Blot (WB). WGCNA analysis indicates that AQP1, MLKL and RIPK3 were significantly related to the AS. The area under the curve of the above hub genes was greater than 0.8 (AQP1 0.946, RIPK1 0.908, RIPK3 0.988, MLKL 0.863). We found AQP1 highly enriched in endothelial cells (ECs) by single-cell analysis. We sequenced the samples by spatial transcriptome and found that AQP1 was also mainly enriched in ECs both in expression and spatial location. With AQP1 overexpression in ECs, it significantly inhibited the expression of MLKL and RIPK3 and stimulated EC proliferation.
Conclusion: Our study identified that AQP1 suppresses atherosclerotic necroptosis by inhibiting the expression of RIPK3 and MLKL in ECs which might indicates that AQP1 plays a role in atherosclerosis. This new mechanism contributes to improving the diagnostic, prognostic, and therapeutic outcomes of atherosclerosis.
Keywords: plaque, carotid atherosclerosis, necroptosis, mechanism
Introduction
Atherosclerosis is a chronic inflammatory disease characterized by the accumulation of lipids and immune cells within the arterial wall, leading to plaque formation.1 The stability of these atherosclerotic plaques is a critical factor in the prevention of adverse cardiovascular events such as stroke and myocardial infarction.2 Recent studies have highlighted the role of programmed cell death mechanisms, including pyroptosis and necroptosis, in the progression and destabilization of atherosclerotic plaques.3–5 Pyroptosis, an inflammatory form of cell death, has been implicated in endothelial dysfunction and vulnerable plaques.6 Similarly, necroptosis contributes to the formation of necrotic cores within plaques, exacerbating their instability.7
Aquaporin 1 (AQP1), a transmembrane water channel protein, has been extensively studied in various diseases, where it has been shown to influence cell proliferation, migration, and apoptosis.8 Notably, AQP1 has been implicated in the regulation of necroptosis pathways. For instance, AQP1 has been shown to interact with receptor-interacting protein kinase 1 (RIPK1), a key mediator of necroptosis, suggesting a role in modulating cell death pathways.9
In the context of atherosclerosis, emerging evidence suggests that AQP1 may play a role in plaque development and stability.10,11 However, the specific mechanisms by which AQP1 influences atherosclerotic processes remain unclear. Given the established involvement of necroptosis in plaque instability and the regulatory role of AQP1 in necroptosis observed in other studies, it is plausible that AQP1 may modulate plaque stability through similar pathways in atherosclerosis.
Therefore, this study aims to investigate the role of AQP1 in atherosclerotic plaque stability, with a particular focus on its potential interaction with necroptosis pathways. By elucidating the molecular mechanisms underlying AQP1’s involvement in plaque destabilization, we hope to identify novel therapeutic targets for the prevention of acute cardiovascular events associated with atherosclerotic disease.
Materials and Methods
Datasets
Atherosclerosis samples of GSE100927 gene expression data were retrieved from the GEO (http://www.ncbi.nlm.nih.gov/geo) database. By using the limma R package, differentially expressed genes (DEGs) between carotid atherosclerosis (CA) and control groups were found (|log2FC| > 1 and P < 0.05).12
Construction of Co-Expression Network
Genes linked to differently enriched cell types were filtered using weighted gene co-expression network analysis (WGCNA). Then, a clustering tree map of samples was built to find and remove outliers based on the profiles of gene expression and sample attributes, WGCNA was performed. In consideration of the sample size, we selected 17 as the soft threshold in accordance with WGCNA guidelines. The selected soft threshold was used to construct networks. The genetic dendrogram as well as modular color were calculated using the degree of differences. A topological overlapping matrix was created by transforming the adjacency matrix. The original module was further isolated through the use of dynamic tree cutting. To determine the most relevant module related to the sample characteristics, the Pearson correlation coefficient between the module eigengenes and the sample traits was determined.
Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) Analysis
R 3.6.3 org.hs.eg.db package and the clusterProfiler package are used to conduct analyses of GO and KEGG pathway enrichment of the intersection between genes in the modules with P<0.05 and DEGs13
Sample Treatment and Collection
Four patients who had severe artery stenosis in the femoral artery and one patient who underwent heart coronary bypass operation were assembled. In accordance with the recommendations for the diagnosis and treatment of lower extremity arterial blockage,14 the patients had perioperative anticoagulation and anti-thrombocyte medication prior to surgery. The ethics committee authorized the sample collection strategy and exclusion standard, No. (2022) YX No (006).
Data Origination and Data Preparation
The Seurat object for the artery sample was produced with the Seurat package in R (version 3.1.1).15 We eliminated any cells that contained fewer than 500 genes, more than 50% mitochondria. The “NormalizeData” and “ScaleData” functions in Seurat were used to normalize and scale the count matrix, respectively.
Identification of Cell Types
Seurat’s “FindVariableFeatures” function was used to determine the top 2000 highly variable genes, and the “RunPCA” function determined the top 20 principal components based on the top 2000 highly variable genes. All cell clusters were clustered using the uniform manifold approximation and projection (UMAP) algorithm, which had a solution of 0.6. The “SingleR” approach for automatic cell annotation annotated every cell cluster using the “HumanPrimaryCellAtlasData” and “BlueprintEncodeData” databases as a guide.
Analysis of Spatial Transcriptomics
In order to identify particular spatial features connected to the effectiveness of immunotherapy, spatial transcriptomics (ST) with multiplexed immunofluorescence, and the single-cell RNA sequencing of atherosclerotic obliterans patients were performed.
Western Blotting
Tissues with human carotid atherosclerosis were used to extract proteins. The Bicinchoninic Acid test (Beyotime, China) was used to measure the concentrations of proteins. In summary, NuPage 4–12% Bis-Tris Gels, manufactured by Novex Life Technologies located in Carlsbad, CA, USA., were used to separate samples of lysate weighing 25 μg. Sanying (Wuhan, China) supplied the primary antibodies against MLKL (1: 500; ab184718) and AQP1 (1:5000; ab12281). Servicebio (Wuhan, China) provided GAPDH (1: 2000, GB15002) and RIPK3 (1: 2000, ab255705). Densitometric analysis of Western blot bands was performed using ImageJ software. Briefly, the acquired blot images were converted to 8-bit grayscale, and the regions corresponding to the target and loading control proteins were selected to measure their integrated density. Background subtraction was applied to correct for non-specific signals. The expression levels of the target proteins were normalized to those of the loading control proteins by calculating the ratio of their integrated densities. The normalized data were then imported into GraphPad Prism software for statistical analysis and graphical representation. Statistical significance was determined using ANOVA, with a p-value of <0.05 considered significant.
Cell Culture
The American Type Culture Collection provided the endothelial cells, which were then cultivated in DMEM supplemented with 10% fetal bovine serum, 100 U/mL penicillin, and streptomycin at 37°C in an incubator with 5% CO2.
Cell Transfection and Treatment
Polymerase chain reaction (PCR) was used to amplify the entire AQP1 sequence, and pcDNA-NEAT1 overexpression plasmids were created after the sequence was subcloned into pcDNA3.1 vectors (Invitrogen; Thermo Fisher Scientific, Inc). Following the manufacturer’s guidance, cells were transfected using Lipofectamine 2000 reagent, which was purchased from Invitrogen. Biosynthesis Biotechnology supplied ox-LDL, which was used to treat endothelial cells at various doses (0, 100, 200, and 300 µg/mL) for a duration of 48 hours in order to investigate its effects.
Reverse Transcription‑quantitative Polymerase Chain Reaction Assay
TSINGKE provided TRIzol® reagent, which was used to extract total RNA extraction in compliance with the manufacturer’s instructions. RT was used to create cDNA specimens using U6 and Glyceraldehyde-3-Phosphate Dehydrogenase (GAPDH) as the internal reference after the concentration and purity of the RNA specimens were measured. Forward (F)/reverse (R) primers were premixed into a solution to create a PCR solution. Following preparation, the mixture was put on an RT-PCR apparatus to be amplified by PCR. The primer sequences are shown in Table 1.
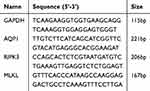 |
Table 1 Primer Pairs and Primer Sequence Required for the Experiment |
Cell Counting Kit-8 (CCK-8) Assay
96-well culture plates (5 × 103 /well) were seeded with endothelial cells in corresponding amounts. Add 100 µL of DMEM medium to each well. A Cell Counting Kit-8 was used to quantify the proliferation of the cells at 0, 24, 48, and 72 hours. Following the addition of 10 μL of CCK8 solution to each well, the cells were incubated for two hours at 37°C. Ultimately, the absorbance of each well was measured using a microplate reader.
Colony Formation Assay
The transfected ECs (Endothelial Cells) were seeded in a 6-well plate and cultured in complete media for 14 days. Following this, they were immobilized with methanol and colored with a 0.1% crystal violet solution (Merck KGaA) that was kept at room temperature for 10 minutes. Ultimately, colonies with a minimum of 50 cells were measured using an Olympus inverted microscope.
Cell Apoptosis Assays
Using the Annexin Fluorescein Isothiocyanate (FITC) Annexin V and Propidium Iodide (PI) Apoptosis Kit that were purchased from GeneCodex in compliance with the manufacturer’s instructions, cells that were going through apoptosis were investigated. In summary, the collected cells were reconstituted in 100 µL of 1X binding buffer, and then a dyeing solution comprising 5 µL of PI and 5 µL of Anne xin V FITC was introduced. Following mixing, the cells were left out of the light and incubated for 15 minutes at room temperature. Afterward, using a flow cytometric device provided by Agilent, apoptotic cells were counted before 400 µL of 1X binding buffer was added.
Results
Bulk Analysis of Two Types of Atherosclerosis
To better ascertain which method of cell death is crucial to the etiology of atherosclerosis in various cases of atherosclerosis, we obtained data of carotid and femoral plaques, downloaded from GEO, comprising 27 femoral arteries and 28 carotid arteries. The gene expression patterns of the carotid and femoral transcriptomes were analyzed. We discovered variations in gene expression between atherosclerosis and normal groups. The atherosclerosis group includes femoral and carotid atherosclerosis. We discovered that genes associated with necroptosis were significantly elevated in atherosclerosis and barely expressed in the normal artery. There was a substantial difference (p < 0.05, |log2FC| > 0.5) in the expression of TNF, FASLG, and Receptor-interacting serine/threonine-protein kinase 3 (RIPK3) (Figure 1A). Moreover, the necroptosis pathway exhibited the greatest t-value by observing Single-sample Gene Set Enrichment Analysis(ssGSEA) scores of femoral and carotid arteries (Figure 1B).
Identification of High Expression of Necroptosis Key Regulated Genes in Atherosclerosis
AQP1 has long been considered as a water pathway protein on the endothelial cell membrane, but recent research indicates that AQP1 may control the rate at which necroptosis advances. It can inhibit the key molecule of necroptosis, RIPK1, thereby weakening the killing effect of downstream Receptor-interacting serine/threonine-protein kinase 3 (RIPK3) and Mixed lineage kinase domain-like pseudokinase (MLKL) on cells. Therefore, to confirm the AQP1 function to regulate necroptosis in atherosclerosis, we first examined the expression of AQP1, RIPK1, RIPK3 and MLKL in atherosclerotic and normal tissues. We downloaded the expression matrix of the GEO dataset including carotid and femoral atherosclerotic patients as well as carotid artery and femoral artery samples. Healthy arteries free of atherosclerotic lesions were obtained from organ donors. The carotid atherosclerosis and femoral samples from carotid and femoral endarterectomy surgery are made up of atherosclerotic plaques.
GSE100927 was analyzed and there were 758 differentially expressed genes found between CA and healthy individuals. Among them, 337 upregulated and 113 downregulated were found relative to normal samples (Figure 2a and b). The expression levels of AQP1, RIPK1, RIPK3 and MLKL in atherosclerosis were shown in boxplots (Figure 2c-f). We have drawn heatmaps of AQP1, RIPK1, RIPK3 and MLKL in Figure 2g, which more clearly and directly shows the expression of the four genes in each sample. The blue color is the atherosclerotic sample group, and the red color is the normal group. The expressions of RIPK1, RIPK3, and MLKL, which initiate necroptosis, are significantly upregulated, while AQP1 decreased.
The Four Genes are Identified to Have a Strong Correlation with the Atherosclerosis Stability
We paired the expression matrix with the disease statuses of the samples. The 43 samples were categorized based on whether atherosclerosis plaque is stable in supplemental file 1 for the trait heatmap and sample dendrogram. The soft threshold power was adjusted to 17 to create a weighted network using scale-free topology criteria, which is when the curve initially arrived at R2 = 0.85 (supplemental file 2). Two modules were found using the dynamic tree-cutting technique, as illustrated in Figure 3a. After connecting the modules to traits, high correlations with the disease status characteristic (stable atherosclerosis plaque or not) were discovered, as shown in Figure 3b. Given that the turquoise and blue modules had a value of p<0.05, it was determined that they were clinically significant and qualified for further analysis. AQP1 is in the turquoise module that has been significantly downgraded. RIPK3 and MLKL are both in the blue module that has been significantly positive correlation. Thus, by correlation analysis of WGCNA, we found that the expression of AQP1 was shown to be associated with the carotid atherosclerosis stability and expressions of RIPK3, MLKL, and RIPK1 are positively linked with the level of development of carotid vulnerable plaque.
In order to assess the diagnostic value of predictor genes for individuals with stable samples or vulnerable atherosclerotic lesions, a receiver operating characteristic (ROC) curve evaluation was carried out. The area under the curve of AQP1 was 0.946, RIPK1 was 0.908, RIPK3 was 0.988, and MLKL was 0.863. (Figure 3c) Therefore, in addition to being linked to clinical outcomes, AQP1, RIPK1, and MLKL have a strong prognostic value for atherosclerosis stability. Meanwhile, the result of Western Blot also demonstrates that AQP1 significantly decreased in carotid atherosclerosis (Figure 3d).
AQP1 Mainly Expresses on Endothelial Cells in Femoral and Carotid Atherosclerosis Plaques
To further determine the mechanism of AQP1-mediated necroptosis, we have to clarify which kinds of cells AQP1 plays a role. Therefore, we analyzed the cellular composition of carotid and femoral atherosclerosis, as well as the cellular location where the necroptosis pathway mainly occurs using single-cell and Spatial Transcriptomics (ST) analysis.
AQP1 Expression in Carotid Atherosclerosis
With the use of the genome map for marker genes, the expression of the genes for each celltype was calculated. The patient’s 47,351 cells were collected. Principal component analysis was used to determine the variation in gene expression in all cells. With the use of graph-based clustering of the relevant main components (n=8), the cells were further divided into cell-type groups. Figure 4a displays the thirty-one groups that were displayed using UMAP.
The top 50 expressed genes (fold change) for each cluster were matched to defined markers. As a result, we identified cell clusters that were easily attributed to well-established cell lineages using common marker genes. 13 cell types were found, comprising Monocyte, Macrophage (monocyte−derived), Common Myeloid Progenitors, NK cell, CD4+T cell, B cell (Plasma cells, Naive and memory B cells), Osteoblasts, Endothelial cell, vascular smooth muscle cells (VSMCs), Tissue stem cell (Figure 4c). All cell markers are shown in the supplementary file 3.
Figure 4b shows the clustering distribution of different samples. GSM4837524, GSM4837526 and GSM4837528 belong to the normal group. GSM4837523, GSM4837525 and GSM4837527 are carotid atherosclerotic plaques. As can be seen, the expression of the other three genes was not obvious, but AQP1 was significantly accumulated in endothelial cells, VSMCs, and mesenchymal cells, and the expression of endothelial cells was more than the other two genes (Figure 4d-e).
AQP1 Expression and Location in the Femoral Atherosclerosis Plaque
To further determine which cells AQP1 mainly expresses in femoral atherosclerosis, we collected disease and normal samples from clinical patients for single-cell sequencing. During a femoral endarterectomy, disease samples from femoral-artery plaques were collected. The normal aorta sample was obtained from heart coronary bypass operations. All these samples were obtained during the operation, swiftly put in the tissue storage solution and submitted right away for single-cell and spatial transcriptome sequencing.
With the use of the genome map for marker genes, the expression of the genes for each cell was determined. The patient’s 13,512 cells were collected. Principal component analysis was employed to determine the variation in gene expression in all cells. With the use of graph-based clustering of the relevant main components, the cells were further divided into cell-type groups. Figure 5a displays the 20 groups that were displayed using UMAP.
Each cluster’s top 50 expressed genes (fold change) were compared to established markers. As a result, by employing common marker genes, we identified cell clusters that were easily attributed to well-established cell lineages. Smooth muscle cell (TAGLN, CNN1, ACTA2), endothelial cells (PECAM1, VWF, CDH5), T/NK Cell (CD3D, CD3E, NKG7, PRF1), B Cell (CD79A, CD19, CD79B), Monocytes and macrophages (CD68, CD163, CD14), fibroblasts (DCN, PDGFRA, PDGFRB), DC (CST3, HLA-DPA1, HLA-DQA1), Foam cells (TREM2, APOC1, GPNMB) (Figure 5B). Figure 5c displays each celltype that merges normal and atherosclerosis samples displayed using UMAP. In the distribution of each cell type on the UMAP in both samples, immune cells of the atherosclerosis sample like T/NK cells, monocytes, macrophages, DC and B cells are more than the normal sample, yet fibroblasts significantly reduced (Figure 5d).
Our sequencing data showed that AQP1 was still highly expressed in femoral atherosclerotic endothelial cells (Figure 5e). In order to further confirm our hypothesis, we performed spatial transcriptome analysis. In total, we examined the transcriptomes with 1,526 UMIs/ point and 1,288 genes/point. Based on the characteristics of gene expression at each site and distribution, we identified 9 types of cells on the entire spatial plane (Figure 5f-g). According to the expression levels of the top 10 specific genes of 9 types of cells, seven cell types were identified, including endothelial cells, T/NK Cell, Monocytes and macrophages, SMC, B Cell, fibroblasts and DC (Figure 5h). We mapped the primary location of AQP1 in pathological tissue sections of plaques. It was also found that AQP1 was mainly enriched in endothelial cells (Figure 5i).
We performed differently expressed gene analysis of all celltypes between normal and atherosclerosis groups (Figure 5j). The up-regulated genes in each cell type were performed GOKEGG enrichment analysis (supplementary file 4). Among all celltypes, only endothelial cells enriched the necroptosis signaling pathway in the environmental signals (Table 2). Genes involved in these necroptosis pathways were found to be highly expressed in endothelial cells: JAK1, GLUL, IL1B, CFLAR, TNFSF10, H2AZ1, MACROH2A1, TNFAIP3, CYBB, TNFRSF10B, IL33, FTH1, BIRC3, BIRC2, PYCARD, CHMP1B, FTL, BAX (P<0.0001), What’s more, many ways of cell death in endothelial cells were enriched, including Apoptosis, Endocytosis, Ferroptosis.
 |
Table 2 The Top ten Pathways of Endothelial Cells in KEGG Enrichment Results |
Constructing Injury Models of Endothelial Cells and Identification of AQP1 Downregulation in Endothelial Cells
Oxidized low-density lipoprotein (ox-LDL) induced endothelial cells to construct vascular endothelial cell injury models. Endothelial cells were treated with 0, 100, 200 and 300μg/ mL ox-LDL for 48h. CCK8 and Lactate Dehydrogenase (LDH) were used to detect cell viability cell supernatant respectively. ox-LDL inhibited cell viability and increased the degree of cell damage in a dose-dependent manner (Figures 6a-b). Based on the results, we selected 300μg/mL as the optimal working concentration of ox-LDL. Endothelial cells treated with 300μg/mL ox-LDL showed a reduction in AQP1 expression (Figure 6c-d). Therefore, AQP1 truly significantly reduces in inflammation ECs, which indicates AQP1 plays a role in the suppression in ECs of atherosclerosis.
AQP1 Overexpression Decreases the Necroptosis and Triggers the Proliferation of ox‑LDL‑induced Endothelial Cells
To investigate whether AQP1 can regulate the key genes of necroptosis——RIPK3 and MLKL, we overexpressed the expression of AQP1 in ox-LDL treated ECs, we first demonstrated that AQP1 was successfully overexpressed by Western Blot and qRT-PCR (Figure 7a-b). The findings of the Western Blot and qRT-PCR demonstrated that AQP1 suppresses MLKL and RIPK3 expression at the mRNA level (Figures 7c-d) and Western Blot (Figure 7e-g). The CCK-8 experiment demonstrated that AQP1 upregulation enhances endothelial-cell proliferation (Figure 7h). The comparison of 0h,24h, 48h and 72h was put into supplementary file 5. Furthermore, the flow cytometric experiment demonstrated that endothelial cells treated with AQP1 overexpression saw a reduction in apoptosis in comparison to the control group (Figure 7i). The colony-formation assay demonstrated that AQP1 significantly increased the survival rate of endothelial cells after overexpression compared with the normal group (Figure 7j).
Discussion
Necroptosis is a regulated form of necrosis characterized by its inflammatory nature, distinct from apoptosis. This process is mediated by receptor-interacting protein kinases, particularly RIPK1 and RIPK3, which, upon activation, phosphorylate mixed lineage kinase domain-like protein (MLKL). Phosphorylated MLKL translocates to the plasma membrane, causing its rupture and the subsequent release of intracellular pro-inflammatory contents. Recent studies have implicated necroptosis in various human diseases, including inflammatory conditions and atherosclerosis. For instance, Karunakaran et al16 demonstrated that key necroptotic factors, RIPK3 and MLKL, are present and active in human atherosclerotic plaques. They observed that patients with unstable conditions, such as those presenting with stroke or transient ischemic attacks, exhibited higher levels of these factors compared to patients with stable disease.16 These findings underscore the importance of investigating the role of necroptosis in atherosclerosis to enhance plaque stability and improve patient outcomes.
AQP1 is a transmembrane protein that facilitates the transport of water and small solutes across cell membranes in response to osmotic gradients. Predominantly expressed in endothelial and epithelial cells, AQP1 plays a crucial role in maintaining water homeostasis. Beyond its traditional role, recent research has linked AQP1 to various pathologies, including cerebral ischemia and cardiovascular diseases.17 Notably, AQP1 has been identified in human atherosclerotic vascular lesions, and its deficiency has been associated with exacerbated atherosclerosis in mouse models. This suggests that AQP1 may have a protective role in vascular health.10 In the context of cell death mechanisms, AQP1 has been shown to interact with RIPK1. Specifically, AQP1 binds to the D324 site of RIPK1, promoting its cleavage and inactivation, thereby inhibiting both RIPK1/RIPK3/MLKL-mediated necroptosis and RIPK1/caspase-8/caspase-3-mediated apoptosis. This interaction highlights a potential regulatory role of AQP1 in cell death pathways.9
Our study builds upon these findings by exploring the expression and function of AQP1 in atherosclerosis. We observed that AQP1 expression is reduced in atherosclerotic tissues, while necroptosis-related genes are upregulated, correlating with disease progression. Single-cell analysis revealed that AQP1 is highly expressed in endothelial cells. Functional assays demonstrated that overexpression of AQP1 in endothelial cells treated with oxidized ox-LDL led to a significant decrease in the expression of MLKL and RIPK3, enhanced cell proliferation, and reduced apoptosis. These results suggest that AQP1 may confer protective effects against endothelial cell necroptosis, thereby contributing to plaque stability. Previous studies have indicated that oxidative stress can induce necroptosis in endothelial cells.18 For example, microvascular endothelial cells can undergo necroptosis initiated by RIPK3 under oxidative stress conditions.19 This implies that similar mechanisms may be operative in the endothelial cells involved in atherosclerosis.
In summary, our study uncovers a novel pathway wherein AQP1 interacts with RIPK1, facilitating its cleavage and thereby suppressing necroptotic signaling in atherosclerosis. This preliminary investigation enhances our understanding of AQP1’s role in the progression of atherosclerosis and offers potential therapeutic avenues targeting this pathway.
However, further research is warranted to identify additional components or adaptors of the AQP1–RIPK1 complex and to elucidate the mechanisms by which AQP1 recruits caspase-8 following its binding to RIPK1. While we observed that the knockdown of AQP1 in endothelial cells led to increased expression of key proteins in the autophagy pathway, specifically RIPK3 and MLKL, indicating that AQP1 may influence autophagy beyond its role as a water channel protein, we did not further validate whether AQP1 directly binds to RIPK1. Additionally, our study lacks in vivo experiments to confirm the impact of AQP1 on the RIPK1/RIPK3/MLKL pathway in a pathological context. Future research should focus on in vivo validation of AQP1’s role and explore whether modulation of this pathway through small molecule inhibitors or gene therapy can ameliorate symptoms in animal models, ultimately assessing its potential in clinical applications.
Conclusions
In addition to aquaporins, AQP1 might also be involved in the inhibition of necroptosis in atherosclerosis. Through bioinformatic analysis, this paper proved that AQP1 plays a key role in the pathogenesis of necroptosis in atherosclerosis. Then vitro experiments further demonstrated that AQP1 may inhibit the production of RIPK3 and MLKL in ox-LDL treated endothelial cells.
Abbreviations
AQP1, Aquaporin 1; AS, atherosclerosis; RIPK1, receptor-interacting serine/threonine-protein kinase 1; RIPK3, receptor-interacting serine/threonine-protein kinase 3; MLKL, mixed lineage kinase domain-like pseudokinase; EC, endothelial cell; CA, carotid atherosclerosis; GEO, Gene Expression Omnibus; WGCNA, weighted gene co-expression network analysis; ssGSEA, single-sample gene set enrichment analysis; AUC, area under the curve; DEG, differentially expressed gene; GO, Gene Ontology; KEGG, Kyoto Encyclopedia of Genes and Genomes; PCD, programmed cell death; PCR, polymerase chain reaction; ST, spatial transcriptomics; VSMC, vascular smooth muscle cell; CCK-8, Cell Counting Kit-8; LDH, lactate dehydrogenase; ox-LDL, oxidized low-density lipoprotein; ROC, receiver operating characteristic; UMAP, uniform manifold approximation and projection; FITC, fluorescein isothiocyanate; PI, propidium iodide GAPDH, glyceraldehyde-3-phosphate dehydrogenase.
Ethics Approval and Informed Consent
The study was carried out in compliance with the Declaration of Helsinki, and approved by the Ethics Committee of Shanxi Medical University. The patients provided informed consent. The ethics number is No. (2022) YX No. (006).
Acknowledgments
The authors would like to thank the BIOINFOR-MEDICAL CENTRE at the Second Hospital of Shanxi Medical University for academic instruction and manuscript revision.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Research Project of Shanxi Provincial Health Commission (2023XG034).
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Skenteris NT, Hemme E, Delfos L, et al. Mast cells participate in smooth muscle cell reprogramming and atherosclerotic plaque calcification. Vascul Pharmacol. 2023;150:107167. doi:10.1016/j.vph.2023.107167
2. Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics-2023 update: a report from the American Heart Association. Circulation. 2023;147:e93–e621. doi:10.1161/cir.0000000000001123
3. Puylaert P, Roth L, Van Praet M, et al. Effect of erythrophagocytosis-induced ferroptosis during angiogenesis in atherosclerotic plaques. Angiogenesis. 2023. doi:10.1007/s10456-023-09877-6
4. Fidler TP, Xue C, Yalcinkaya M, et al. The AIM2 inflammasome exacerbates atherosclerosis in clonal haematopoiesis. Nature. 2021;592:296–301. doi:10.1038/s41586-021-03341-5
5. Kluck GEG, Qian AS, Sakarya EH, Quach H, Deng YD, Trigatti BL. Apolipoprotein A1 protects against necrotic core development in atherosclerotic plaques: PDZK1-dependent high-density lipoprotein suppression of necroptosis in macrophages. Arterioscler Thromb Vasc Biol. 2023;43:45–63. doi:10.1161/ATVBAHA.122.318062
6. Shamas S, Rahil RR, Kaushal L, et al. Pyroptosis in endothelial cells and extracellular vesicle release in atherosclerosis via NF-kappaB-Caspase-4/5-GSDM-D pathway. Pharmaceuticals. 2024;17:1568. doi:10.3390/ph17121568
7. Puylaert P, Zurek M, Rayner KJ, De Meyer GRY, Martinet W. Regulated necrosis in atherosclerosis. Arterioscler Thromb Vasc Biol. 2022;42:1283–1306. doi:10.1161/ATVBAHA.122.318177
8. Guo Z, Zhang H, Liu X, et al. Water channel protein AQP1 in cytoplasm is a critical factor in breast cancer local invasion. J Exp Clin Cancer Res. 2023;42:49. doi:10.1186/s13046-023-02616-1
9. Yin Z, Chen W, Yin J, et al. RIPK1 is a negative mediator in aquaporin 1-driven triple-negative breast carcinoma progression and metastasis. NPJ Breast Cancer. 2021;7:53. doi:10.1038/s41523-021-00261-5
10. Wintmo P, Johansen SH, Hansen PBL, et al. The water channel AQP1 is expressed in human atherosclerotic vascular lesions and AQP1 deficiency augments angiotensin II-induced atherosclerosis in mice. Acta Physiol. 2017;220:446–460. doi:10.1111/apha.12853
11. Shanahan CM, Connolly DL, Tyson KL, et al. Aquaporin-1 is expressed by vascular smooth muscle cells and mediates rapid water transport across vascular cell membranes. J Vasc Res. 1999;36:353–362. doi:10.1159/000025674
12. Ritchie ME, Phipson B, Wu D, et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43:e47–e47. doi:10.1093/nar/gkv007
13. Yu G, Wang LG, Han Y, He, He Q-Y. clusterProfiler: an R package for comparing biological themes among gene clusters. OMICS. 2012;16:284–287. doi:10.1089/omi.2011.0118
14. Liu C. Guidelines for the treatment of arteriosclerotic obliterans of the lower extremities. Chin J Pract Surg. 2008;28:923–924.
15. Zhang Z, Salisbury D, Sallam T. Long Noncoding RNAs in atherosclerosis: JACC review topic of the week. J Am Coll Cardiol. 2018;72:2380–2390. doi:10.1016/j.jacc.2018.08.2161
16. Karunakaran D, Geoffrion M, Wei L, et al. Targeting macrophage necroptosis for therapeutic and diagnostic interventions in atherosclerosis. Sci Adv. 2016;2:e1600224. doi:10.1126/sciadv.1600224
17. Gomes D, Agasse A, Thiébaud P, Delrot S, Gerós H, Chaumont F. Aquaporins are multifunctional water and solute transporters highly divergent in living organisms. Biochim Biophys Acta. 2009;1788:1213–1228. doi:10.1016/j.bbamem.2009.03.009
18. Zhao W, Feng H, Sun W, Liu K, Lu JJ, Chen X. Tert-butyl hydroperoxide (t-BHP) induced apoptosis and necroptosis in endothelial cells: roles of NOX4 and mitochondrion. Redox Biol. 2017;11:524–534. doi:10.1016/j.redox.2016.12.036
19. Faust H, Lam LM, Hotz MJ, Qing D, Mangalmurti NS. RAGE interacts with the necroptotic protein RIPK3 and mediates transfusion-induced danger signal release. Vox Sang. 2020;115:729–734. doi:10.1111/vox.12946
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.








