Back to Journals » Journal of Pain Research » Volume 18
Articaine Needle - Free Anesthesia Vs Conventional Anesthesia in Root Canal Treatment of Irreversible Pulpitis in Permanent Teeth: A Prospective Study on Anesthetic Efficacy and Effects on Pain
Authors Qian S, Meng Z, Zhang H, Li K, Zhang F, Zhang S, Liu J, Zhou Z
Received 13 January 2025
Accepted for publication 8 April 2025
Published 21 April 2025 Volume 2025:18 Pages 2115—2125
DOI https://doi.org/10.2147/JPR.S514944
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr David Keith
Suhui Qian,1,* Ziying Meng,2,* Haiyan Zhang,1 Kaicheng Li,1 Fei Zhang,1 Sen Zhang,1 Jianfei Liu,1 Zhou Zhou1
1Department of Stomatology, Huaibei People’s Hospital, Huaibei, Anhui, People’s Republic of China; 2Stomatology Department of Suixi County Hospital, Huaibei, Anhui, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhou Zhou, Email [email protected]
Objective: This study aimed to compare the anesthetic efficacy of articaine needle-free anesthesia with conventional lidocaine nerve block anesthesia for root canal treatment in permanent teeth with irreversible pulpitis.
Methods: In this prospective clinical trial, 94 patients were randomly allocated to receive either articaine needle-free anesthesia (n=47) or lidocaine nerve block anesthesia (n=47). Anesthetic effectiveness was evaluated through onset time, success rate, and visual analog scale (VAS) pain scores during crown opening and pulp removal procedures. Secondary outcomes included hemodynamic stability (heart rate, systolic and diastolic blood pressure) and incidence of adverse reactions.
Results: The articaine group exhibited significantly faster anesthesia onset (7.62± 1.28 minutes vs 9.35± 2.04 minutes, p< 0.05) and higher success rate (93.62% vs 80.85%, p< 0.05). Patients receiving articaine reported significantly lower pain scores during crown opening (4.31± 1.13 vs 5.48± 1.06) and pulp removal (3.18± 1.07 vs 4.26± 1.12) (both p< 0.05). Both groups maintained comparable hemodynamic stability throughout the procedure (p> 0.05), with no significant difference in adverse reaction rates (11.49% vs 10.64%, p> 0.05).
Conclusion: Articaine needle-free anesthesia demonstrates superior clinical performance compared to conventional lidocaine nerve block, offering faster onset, improved success rate, and enhanced pain control during root canal treatment of irreversible pulpitis, while maintaining equivalent safety parameters. These findings support its adoption as an effective alternative for dental anesthesia in endodontic procedures.
Keywords: articaine needle-free anesthesia, conventional anesthesia, irreversible pulpitis, root canal treatment, effects, pain, impact
Introduction
Irreversible pulpitis is a common dental pulp disease caused by irreversible pathological damage to the pulp tissue due to bacterial infection or other stimuli.1 Typical clinical manifestations include spontaneous pain, nocturnal pain, and exacerbated pain upon thermal stimulation, severely affecting patients’ daily lives and psychological well-being.2,3 If left untreated, the condition may progress to involve periapical tissues, leading to more severe periodontal and systemic health issues.4 Thus, early accurate diagnosis and effective treatment are crucial for controlling disease progression, alleviating pain, and preserving the affected teeth. Root canal therapy is the preferred treatment for irreversible pulpitis. By thoroughly removing infected tissue within the pulp chamber and root canals, followed by proper disinfection and filling, this therapy effectively controls infection and restores tooth function.5,6 However, the complex procedures involved in root canal treatment, including accessing and cleaning the pulp chamber, often induce significant pain in patients due to procedural stimulation.7 This pain not only impacts the patient’s treatment experience and compliance but also exacerbates dental anxiety.8 Therefore, optimizing anesthetic techniques to reduce procedural pain has become a critical area of clinical research.
Currently, conventional lidocaine nerve block anesthesia remains the most commonly used anesthetic technique in root canal treatment. By injecting the anesthetic locally to block nerve conduction, it alleviates procedural pain to some extent.9,10 However, this method requires needle injection for drug delivery, which can increase psychological stress for patients with needle phobia or heightened pain sensitivity.11 Additionally, needle insertion may cause mechanical damage to local tissues or infection, further contributing to procedural discomfort.12 With the advent of needle-free technology, new developments in dental anesthesia have emerged. Needle-free anesthesia utilizes high-pressure devices to deliver anesthetic agents directly into subcutaneous tissues without the need for needle insertion, offering advantages such as rapid onset, minimally invasive delivery, and increased comfort.13,14 Among needle-free anesthetics, articaine has garnered attention for its high lipid solubility and rapid diffusion.15 Articaine, an amide-type local anesthetic, is characterized by its fast onset, high anesthetic depth, and prolonged duration, making it a promising option in dental anesthesia.16,17 However, systematic studies on the use of articaine needle-free anesthesia in treating irreversible pulpitis remain limited, and its specific advantages in pain management require further investigation. This study retrospectively analyzed the outcomes of root canal therapy for irreversible pulpitis patients receiving different anesthesia methods. The aim was to provide scientific evidence for optimizing clinical anesthetic protocols for irreversible pulpitis and to support the broader application of needle-free anesthesia technology in dental procedures.
Materials and Methods
Ethics Approval and Consent to Participate
This study was approved by the ethics committee of Huaibei People’s Hospital. All the methods were carried out in accordance with the Declaration of Helsinki. All participants provided written informed consent prior to their inclusion in the study.
Study Subjects
This analysis examined the clinical data of 94 patients diagnosed with irreversible pulpitis and undergoing root canal treatment in our hospital from January 2022 to April 2024. Patients were randomly allocated into the control group (receiving conventional lidocaine nerve block anesthesia) and the test group (receiving articaine needle - free anesthesia). Randomization was performed using a computer - generated random number sequence in SPSS 22.0 software. Each patient was assigned a unique random number between 1 and 94. Those with random numbers in the range of 1–47 were placed in the control group, while those with numbers from 48–94 were placed in the test group. Inclusion criteria: (1) Patients meeting the diagnostic criteria for irreversible pulpitis of the mandibular first molar, characterized by acute onset, spontaneous and paroxysmal pain, exacerbation with hot or cold stimulation, temperature sensitivity, occasional nocturnal pain, inability to localize the pain, unilateral cheek pain without radiation to the contralateral side. Diagnosis was confirmed via X-rays and oral radiography, with clear assessment of pain intensity. (2) Aged between 18 and 65 years, with full civil capacity, capable of understanding and cooperating with anesthesia and treatment procedures. (3) Good general health without severe systemic diseases (eg, uncontrolled hypertension, diabetes, heart disease) that would preclude tolerance to dental treatment. (4) No history of allergies to local anesthetics (eg, articaine, lidocaine). (5) No prior root canal treatment or history of failed dental anesthesia. (6) Voluntary participation in the study with informed consent, with a clear understanding of the study’s objectives, potential risks, and benefits. Exclusion criteria: (1) Severe periapical periodontitis or other complications rendering immediate root canal treatment infeasible. (2) Severe tooth structure damage requiring extraction. (3) Allergic reactions or contraindications to the drugs or equipment used in the study. (4) Coagulopathy, severe cardiopulmonary diseases, or other systemic conditions precluding tolerance to anesthesia or dental treatment. (5) Pregnant or breastfeeding women. (6) Severe anxiety, phobias, or other psychological disorders preventing cooperation during treatment. (7) Cognitive impairments or communication difficulties that prevent accurate reporting of symptoms or cooperation in assessments. (8) Participation in other related clinical trials. This study was approved by the Huaibei People’s Hospital Medical Ethics Committee (Approval No. KQ-MZ24017) and conducted in strict adherence to the ethical standards of the Declaration of Helsinki.
Anesthesia Methods
Control Group
The control group received conventional lidocaine nerve block anesthesia using 2% lidocaine injection (Shanxi Jinxi Double Crane Pharmaceutical Co., Ltd., National Drug Approval No. H11022295). The specific steps were as follows: Patients were seated, identity confirmed, contraindications excluded, and communication conducted to alleviate tension. Oral preparation was performed using 0.2% chlorhexidine mouthwash to ensure cleanliness at the injection site. The injection site was selected based on the tooth to be treated. A 2% lidocaine solution (1.0–1.8 mL) was prepared using a sterile disposable syringe, with dosage adjusted according to the patient’s weight and treatment needs. The injection point was located using a periodontal probe or palpation. The needle was slowly inserted into the target tissue, ensuring that the needle tip did not enter a blood vessel. The solution was injected slowly while monitoring the patient’s reaction to avoid discomfort from rapid drug diffusion. Anesthesia was tested 3–5 minutes post-injection using a blunt instrument to assess the anesthetized area. If pain persisted, additional solution was administered. Patients were monitored for systemic reactions, including heart rate (HR), blood pressure, and local responses, to prevent allergic reactions or other adverse effects.
Observation Group
The observation group received needle-free articaine anesthesia using 4% articaine injection (Septodont, Imported Drug Registration No. H20110264) delivered via needle-free injection equipment for local infiltration anesthesia. The procedure was as follows: Patient identity was confirmed, and contraindications to the medication and needle-free equipment were excluded. Oral preparation was the same as in the control group. A needle-free injector (high-pressure jet injector) was loaded with 4% articaine solution (1.7 mL). The device’s spray pressure and dosage were adjusted according to the target tooth. The injection point was identified based on the anatomical location of the tooth. The nozzle of the needle-free injector was placed against the injection site, ensuring complete contact with the tissue to prevent drug leakage. The solution was administered via high-pressure jet injection over 3–5 seconds. Anesthesia was tested 2–3 minutes post-injection using a blunt instrument. If the effect was insufficient, additional injections were performed. Systemic reactions, including HR, blood pressure, and local responses, were monitored to avoid allergic reactions or other adverse effects.
Observation Indicators
Anesthesia Effect
Onset time of anesthesia: Measured using a pulp vitality tester. The tooth surface was isolated with cotton rolls and dried with an air syringe. The pulp vitality tester, coated with conductive paste, was applied to the buccal surface of the tooth at the apical third. When patients reported sensations of acidity, numbness, or pain, the operation was stopped, and the time recorded. Measurements were taken at 1 - minute intervals post - anesthesia until a maximum reading of 80 with no subjective sensation was achieved.
- Depth of anesthesia: Evaluated by pain levels measured before anesthesia, during pulpal access, and during pulpectomy using a visual analog scale (VAS), scored from 0 to 10. Lower VAS scores indicate a greater depth of anesthesia.
- Duration of anesthesia: Recorded from the time of achieving an adequate level of anesthesia (as determined by the absence of pain response to the pulp vitality tester) until the reappearance of pain or sensation during the procedure or within a specified post - treatment observation period (set as 60 minutes in this study).
- Anesthesia success rate: Calculated as (Complete pain relief + Mild pain cases) / Total cases × 100%. Complete pain relief is defined as no pain during pulpal access, crown, or root removal; Mild pain is no pain during pulpal access but slight pain during deep crown or root removal; Severe pain is slight pain during pulpal access and significant pain during root removal but tolerable for completing treatment”.
The assessment of the anesthetic effect was carried out by 3 trained and calibrated examiners. To ensure standardization, all examiners participated in a calibration session before the study. During the calibration, they were required to assess a set of 20 pre - defined cases independently, and the inter - examiner reliability was calculated using Cohen’s kappa. The kappa values for the three examiners were 0.85, 0.83, and 0.87 respectively, all of which exceeded the threshold of 0.8.
The local anesthetic (LA) was administered by 5 experienced dentists. All dentists had at least 10 years of experience in dental anesthesia and were trained in the specific techniques of both conventional lidocaine nerve block anesthesia and articaine needle - free anesthesia used in this study. Before the study, they underwent a training session on the standardized administration procedures for both anesthesia methods.
Pain at Different Time Points
Pain was assessed before anesthesia, during pulpal access, and during pulpectomy using a visual analog scale (VAS), scored from 0 to 10, where higher scores indicated greater pain intensity. In addition to the VAS, observational scales that assess pain-related behaviors (eg, facial expressions, body movements) or physiological markers (eg, heart rate variability, cortisol levels) could be used alongside self-reported measures to provide a more objective assessment of pain.
HR Levels at Different Time Points
HR was measured using an automatic electronic sphygmomanometer before anesthesia, during pulpal access, and during pulpectomy.
Blood Pressure Levels at Different Time Points
Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured using an automatic electronic sphygmomanometer before anesthesia, during pulpal access, and during pulpectomy.
Adverse Reactions
Adverse reactions during anesthesia and the postoperative observation period, including dizziness, headache, nausea, vomiting, abnormal blood pressure, HR irregularities, and peripheral nerve damage, were recorded by hospital staff.
Long-Term Effectiveness and Complications Assessment
To comprehensively evaluate the long-term treatment outcomes, we implemented a standardized 12-month follow-up protocol with the following measurement methods: (1) Periapical Healing Assessment: Digital periapical radiographs (Schick CDR system) were obtained at 6 and 12 months. Two blinded endodontists independently scored healing using the periapical index (PAI). Complete healing defined as PAI score ≤2 with normal periodontal ligament space. (2) Neurological Function Testing: Two-point discrimination measured with calibrated Von Frey filaments. Light touch sensitivity assessed using standardized nylon monofilaments. Persistent paresthesia defined as abnormal responses persisting >6 months. (3) Clinical Symptom Monitoring: Patients maintained daily symptom diaries for 3 months. Monthly telephone interviews conducted by research assistants. Recurrent pain episodes verified through clinical examination. Structural Integrity Evaluation: Teeth examined under 4× magnification for cracks/fractures. Bite force measurements using T-scan digital occlusal analysis.
Statistical Analysis
The sample size for this study was determined based on a power analysis. We estimated that a sample size of 94 patients (with 47 in each group) would be sufficient to detect a clinically significant difference in anesthetic effectiveness between the articaine needle - free anesthesia group and the conventional lidocaine nerve block anesthesia group. To minimize potential biases in outcome assessment, the study implemented a single-blind design. The clinicians administering the anesthesia were aware of the treatment allocation due to the nature of the interventions (needle-free vs conventional injection). However, the three trained examiners who evaluated anesthetic efficacy and pain outcomes were blinded to group assignments during data collection and analysis. Additionally, patients were not informed about which anesthetic method they received to reduce reporting bias in pain assessments. The power analysis was conducted using G*Power 3.1 software with the following assumptions: a significance level (α) of 0.05, a power (1 - β) of 0.80, and an expected effect size of 0.5. The expected effect size of 0.5 was based on a previous similar study, which investigated the difference in anesthesia success rates between different anesthesia methods in dental procedures. GraphPad Prism 8 was used for graphing, and SPSS 22.0 for data processing. Categorical data were expressed as percentages (%) and analyzed using the χ²-test. Continuous data were expressed as ( ) and analyzed using an independent-sample t-test for between-group comparisons, paired t-tests for within-group comparisons, and repeated measures ANOVA for multiple time-point comparisons between groups. A p-value < 0.05 was considered statistically significant.
) and analyzed using an independent-sample t-test for between-group comparisons, paired t-tests for within-group comparisons, and repeated measures ANOVA for multiple time-point comparisons between groups. A p-value < 0.05 was considered statistically significant.
Results
Comparison of Basic Information
The gender, age, body mass index (BMI), disease duration, proportions of percussion pain, chewing pain, radiating pain in the maxillofacial region, and comorbidities were comparable between the two groups (P > 0.05), as shown in Table 1.
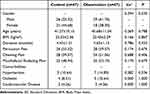 |
Table 1 Comparison of Clinical Information (mean±SD, n [%]) |
Comparison of Anesthetic Effects
The induction time of anesthesia was (9.35 ± 2.04) in the control group and (7.62 ± 1.28) in the observation group. The observation group showed a shorter induction time than the control group (P < 0.05), as shown in Figure 1. Among the 47 patients in the control group, 16 experienced complete pain relief, 22 experienced mild pain, and 9 experienced severe pain. In the observation group, 25 experienced complete pain relief, 20 experienced mild pain, and 2 experienced severe pain. The success rate of anesthesia in the observation group (93.62%) was higher than in the control group (80.85%) (P < 0.05), as shown in Figure 2.
 |
Figure 1 Comparison of Anesthesia Induction Time (mean±SD, min). |
 |
Figure 2 Comparison of Anesthesia Success Rate [n (%)]. Note: Compared with the control group, *P < 0.05. |
The duration of anesthesia in the control group was (45.23 ± 8.56) minutes, while in the observation group it was (50.15 ± 7.89) minutes. Although the difference did not reach statistical significance (P > 0.05), there was a trend towards a longer duration of anesthesia with articaine needle - free anesthesia.
The success rate of anesthesia in the observation group (93.62%) was higher than in the control group (80.85%) (P < 0.05), further demonstrating the superior anesthetic efficacy of articaine needle - free anesthesia.
Comparison of Pain Scores at Different Time Points
The VAS scores before anesthesia, during unroofing, and during pulpectomy were (7.53 ± 0.72, 5.48 ± 1.06, 4.26 ± 1.12) in the control group and (7.62 ± 0.81, 4.31 ± 1.13, 3.18 ± 1.07) in the observation group. The differences in group effects (F = 4.765), time effects (F = 6.581), and interaction effects (F = 5.437) between the two groups were significant (P < 0.05). Within-group comparisons showed that VAS scores during unroofing and pulpectomy were lower than those before anesthesia, and scores during pulpectomy were lower than those during unroofing (P < 0.05). Between-group comparisons showed no significant differences in pre-anesthesia VAS scores (P > 0.05), but VAS scores during unroofing and pulpectomy were lower in the observation group than in the control group (P < 0.05), as shown in Figure 3.
Comparison of HR Levels at Different Time Points
The HR values before anesthesia, during unroofing, and during pulpectomy were (75.27 ± 5.43, 76.15 ± 4.89, 75.52 ± 4.68) in the control group and (75.38 ± 5.16, 75.89 ± 4.74, 75.27 ± 5.32) in the observation group. There were no significant differences in group effects (F = 0.814), time effects (F = 1.012), or interaction effects (F = 0.939) (P > 0.05), as shown in Figure 4.
 |
Figure 4 Comparison of HR Levels at Different Time Points (mean±SD, beats/min). |
Comparison of SBP and DBP Levels at Different Time Points
There were no significant differences in group effects (SBP: F = 0.715; DBP: F = 0.918), time effects (SBP: F = 0.846; DBP: F = 0.786), or interaction effects (SBP: F = 0.781; DBP: F = 0.827) (P > 0.05), as shown in Tables 2 and 3.
 |
Table 2 Comparison of SBP Levels at Different Time Points (mean±SD, mmHg) |
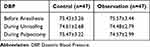 |
Table 3 Comparison of DBP Levels at Different Time Points (mean±SD, mmHg) |
Comparison of Adverse Reactions
The incidence of adverse reactions was 10.64% in the control group and 14.89% in the observation group, with no significant difference (P > 0.05), as shown in Table 4.
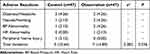 |
Table 4 Comparison of Adverse Reactions [n (%)] |
Long-Term Treatment Outcomes and Complications
The 12-month follow-up data (87.2% retention rate) revealed significant differences in long-term outcomes (Table 5).
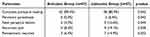 |
Table 5 Comparative 12-Month Outcomes (n [%]) |
Discussion
Irreversible pulpitis is a common pulp disease characterized by irreversible damage to the pulp tissue, often accompanied by severe spontaneous pain, significantly impacting patients’ quality of life.18,19 Root canal therapy, as the main treatment for this condition, relies on effective anesthesia management for its successful implementation. However, traditional anesthesia methods face challenges such as slow onset, inadequate pain relief, and patient discomfort caused by the procedure,20 highlighting the need for more efficient and comfortable anesthesia techniques. In recent years, articaine needle-free infiltration anesthesia has gained attention for its rapid onset and high comfort level. This study aims to analyze the application effects of articaine needle-free anesthesia in the root canal treatment of irreversible pulpitis, exploring its mechanism of action and potential clinical value to provide scientific evidence for optimizing pulpitis treatment.
The data from this study indicate that patients receiving articaine needle-free anesthesia (observation group) had significantly shorter anesthesia onset times compared to those receiving conventional lidocaine nerve block anesthesia (control group), with a significantly higher anesthesia success rate in the observation group (P < 0.05). This advantage can be attributed to the molecular properties of articaine and the unique mechanism of needle-free anesthesia. The high lipid solubility and low protein-binding rate of articaine enable it to penetrate tissue barriers quickly, acting directly on sodium ion channels in nerve fibers to rapidly block nerve signal transmission.21 Furthermore, needle-free anesthesia, through high-pressure jet technology, distributes the drug evenly within the tissue, avoiding uneven drug distribution associated with traditional needle injections,22 thereby enhancing the stability and success rate of anesthesia. This is particularly significant in complex root canal treatments, where rapid and effective anesthesia is essential for alleviating patient discomfort and improving procedural efficiency. Pain management remains a core issue in the treatment of pulpitis.23 The results of this study show that the VAS scores of the observation group were significantly lower than those of the control group at different postoperative time points, with pain gradually alleviating over time. This indicates that articaine needle-free anesthesia is more effective in controlling intraoperative pain. This outcome may be related to the following factors:(1) Drug Mechanism Advantage: Articaine rapidly and efficiently blocks nerve impulse transmission, achieving profound anesthesia in a short time and providing prolonged pain relief.24 (2) Comfort of Needle-Free Technology: Traditional needle injections may induce psychological fear and additional pain, while needle-free technology avoids discomfort related to needle punctures through high-pressure jet injection, enabling a more relaxed experience for patients, especially those sensitive to pain.25 (3) Uniform Drug Distribution: Needle-free anesthesia ensures comprehensive drug coverage, reducing the likelihood of incomplete pain control in localized areas, further enhancing pain relief.26 In terms of vital sign stability, the study shows no significant differences in HR, SBP, and DBP indicators at different time points between the two groups (P > 0.05). This suggests that both articaine needle-free anesthesia and lidocaine nerve block anesthesia maintain physiological stability during treatment. However, it should be emphasized that needle-free anesthesia technology may further reduce psychological stress during treatment by minimizing mechanical stimulation and psychological anxiety, which is particularly important for patients with significant anxiety or nervousness. Although the needle-free technique did not significantly affect vital signs in this study, its potential to indirectly improve the treatment experience warrants further investigation.
Regarding safety, there was no significant difference in the incidence of adverse reactions between the two groups (P > 0.05). This indicates that while enhancing the effectiveness of anesthesia, articaine needle-free infiltration anesthesia does not increase safety risks. Furthermore, studies27 suggest that articaine is rapidly metabolized by plasma esterases, differing from other local anesthetics that rely on liver metabolism. This characteristic reduces the risk of systemic adverse reactions caused by drug accumulation. However, the high-pressure jet used in needle-free anesthesia may cause slight mechanical tissue damage or temporary discomfort,28 necessitating optimization of technical parameters during clinical practice to further minimize risks.
This study confirms the superiority of articaine needle-free infiltration anesthesia in the root canal treatment of irreversible pulpitis. Its rapid onset, high success rate, and excellent pain control capability offer a new option for dental anesthesia.
Several variables may influence anaesthesia success rates. There are conditions that may help to predict a patient’s pain during endodontic procedures. These conditions could be overcome either by employing methods such as premedication with a non-steroidal anti-inflammatory drug prior to the treatment visit or by using supplementary techniques before or during the treatment. However, investigators need to be more careful when reporting details of their studies to reduce concerns regarding their study bias.29 A prior study showed that articaine is more effective than lidocaine for local anaesthesia of teeth with irreversible pulpitis undergoing root canal treatment. There is limited evidence that injection of articaine is less painful, has more rapid onset and has fewer adverse events compared with lidocaine.30 Moreover, the efficacy of 4% articaine with 1:100,000 epinephrine has been found to be better than 2% lidocaine with 1:80,000 epinephrine, as only 0.8 mL of 4% articaine with 1:100,000 epinephrine was effectively used as compared to 1.6 mL of 2% lidocaine with 1:80,000 epinephrine. Furthermore, females experience more pain as compared to males.31,32
However, the study has certain limitations, such as a limited sample size, single-center study design, and potential impacts of individual patient differences on the results. Therefore, future research should include multicenter, large-sample randomized controlled trials to further validate the generalizability and reliability of the findings. Additionally, attention should be given to the following aspects: (1) Impact of Individual Patient Factors: Investigate the potential influence of factors such as age, gender, and psychological state on the efficacy of needle-free anesthesia. (2) Applicability to Different Conditions: Assess the application of articaine needle-free infiltration anesthesia in other dental conditions, such as complex root canal treatments or implant surgeries. (3) Individual variations in pain perception: The study did not account for individual differences in pain perception, which can significantly influence Visual Analog Scale (VAS) scores. Factors such as psychological state, cultural background, and prior pain experiences may affect subjective pain reporting, potentially introducing bias into the results.
The findings of this study have several important clinical implications for the management of irreversible pulpitis and the broader field of dental anesthesia. Firstly, the significantly shorter onset time of articaine needle-free anesthesia (7.62 ± 1.28 minutes) compared to conventional lidocaine nerve block anesthesia (9.35 ± 2.04 minutes) suggests that this method can expedite the initiation of root canal treatment. In clinical practice, this means that patients can experience pain relief more quickly, reducing their anxiety and discomfort during the waiting period. This is particularly beneficial in emergency dental settings where rapid pain management is critical.
Secondly, the higher anesthesia success rate in the observation group (93.62%) compared to the control group (80.85%) indicates that articaine needle-free anesthesia is more reliable in achieving effective pain control during root canal procedures. This is crucial for ensuring that patients do not experience breakthrough pain during treatment, which can lead to procedural interruptions, increased patient distress, and potentially compromised treatment outcomes. The improved success rate also suggests that articaine needle-free anesthesia may reduce the need for supplemental anesthesia, which is often required in cases where traditional anesthesia fails to provide adequate pain relief.
Thirdly, the lower VAS pain scores in the observation group during crown opening and pulp removal (4.31 ± 1.13 and 3.18 ± 1.07, respectively) compared to the control group (5.48 ± 1.06 and 4.26 ± 1.12) highlight the superior pain control provided by articaine needle-free anesthesia. This reduction in intraoperative pain is not only beneficial for patient comfort but also for the overall efficiency of the procedure. Patients who experience less pain are more likely to remain cooperative and still during treatment, allowing the dentist to perform the procedure more smoothly and with greater precision. This can lead to better clinical outcomes and a reduced risk of complications.
Moreover, the absence of significant differences in heart rate (HR) and blood pressure (SBP and DBP) between the two groups suggests that articaine needle-free anesthesia does not compromise hemodynamic stability. This is particularly important for patients with cardiovascular conditions or those who are at risk of stress-induced physiological changes during dental procedures. The stability of vital signs during treatment further supports the safety profile of articaine needle-free anesthesia, making it a viable option for a wide range of patients, including those with systemic health concerns.
Finally, the comparable incidence of adverse reactions between the two groups (10.64% in the control group vs 11.49% in the observation group) indicates that articaine needle-free anesthesia does not increase the risk of complications. This is reassuring for both clinicians and patients, as it suggests that the benefits of needle-free anesthesia can be achieved without compromising safety. The most common adverse reactions, such as dizziness and nausea, were mild and transient, further supporting the clinical feasibility of this technique.
Conclusion
In summary, the results of this study demonstrate that articaine needle-free anesthesia offers several clinical advantages over traditional lidocaine nerve block anesthesia in the treatment of irreversible pulpitis. The shorter onset time, higher success rate, and superior pain control provided by articaine needle-free anesthesia can significantly enhance the patient experience, improve procedural efficiency, and reduce the risk of intraoperative complications. These findings suggest that articaine needle-free anesthesia should be considered as a first-line option for patients undergoing root canal treatment, particularly those with dental anxiety or systemic health concerns. Future research should focus on validating these findings in larger, multicenter studies and exploring the potential applications of needle-free anesthesia in other dental procedures.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zheng Y, Chen XJ, Wang Q. [One-way membrane decompression for vital pulp therapy in irreversible pulpitis: a case report]. Zhonghua Kou Qiang Yi Xue Za Zhi. 2024;59(1):85–88. doi:10.3760/cma.j.cn112144-20230912-00154 Dutch
2. Xiao W, Shi WT, Wang J. [Study of vital inflamed pulp therapy in immature permanent teeth with irreversible pulpitis and apical periodontitis]. Zhonghua Kou Qiang Yi Xue Za Zhi. 2022;57(3):287–291. doi:10.3760/cma.j.cn112144-20211223-00563 Dutch
3. Hewitt B, Coffman C. Update on Endodontic, Restorative, and Prosthodontic Therapy. Vet Clin North Am Small Anim Pract. 2022;52(1):185–220. doi:10.1016/j.cvsm.2021.09.003
4. El Karim IA, Duncan HF, Fouad AF, et al. Effectiveness of full pulpotomy compared with root canal treatment in managing teeth with signs and symptOms indicative of irreversible pulpitis: a protocol for prospectiVE meta-analysis of individual participant data of linked randomised clinical trials (PROVE). Trials. 2023;24(1):807. doi:10.1186/s13063-023-07836-6
5. Koçer A, Dönmez Özkan H, Turk T. Postoperative pain intensity and incidence following single visit root canal treatment with different obturation techniques: a randomized clinical trial. PeerJ. 2022;10:e13756. doi:10.7717/peerj.13756
6. Dhyani VK, Chhabra S, Sharma VK, et al. A randomized controlled trial to evaluate the incidence of postoperative pain and flare-ups in single and multiple visits root canal treatment. Med J Armed Forces India. 2022;78(Suppl 1):S35–s41. doi:10.1016/j.mjafi.2020.03.010
7. Santos JM, Pereira JF, Marques A, et al. Vital pulp therapy in permanent mature posterior teeth with symptomatic irreversible pulpitis: a systematic review of treatment outcomes. Medicina. 2021;57(6):573. doi:10.3390/medicina57060573
8. Atesci AA, Topaloglu-Ak A, Turan E, et al. Evaluation of postoperative pain following single-visit root canal treatment with rotary and reciprocal ni-ti file systems in children. Medicina. 2021;58(1):50. doi:10.3390/medicina58010050
9. Laham A, Clouet R, Del Valle GA, et al. Anaesthetic efficacy and influence on cardiovascular parameters change of intraosseous computerised anaesthesia versus inferior alveolar nerve block anaesthesia in acute irreversible pulpitis of mandibular molars: study protocol for a prospective randomised controlled trial. Trials. 2022;23(1):979. doi:10.1186/s13063-022-06915-4
10. Chang QK, Gao C, Shen M-L, et al. [Different concentration of lidocaine used for an exodontia of the impacted mandibular third molar]. Shanghai Kou Qiang Yi Xue. 2020;29(5):499–503. Dutch
11. Albar NH, Maganur PC, Alsaeedi AA, et al. Effectiveness of a needle-free local anesthetic technique compared to the traditional syringe technique for the restoration of young permanent molars: a single-blind randomized clinical trial. J Clin Pediatr Dent. 2024;48(6):107–116.
12. Gandhi N, Shah N, Wahjuningrum DA, et al. Evaluation of pulpal anesthesia and injection pain using IANB with pre-heated, buffered and conventional 2% lignocaine in teeth with symptomatic irreversible pulpitis-a randomized clinical study. PeerJ. 2022;10:e14187. doi:10.7717/peerj.14187
13. Yilmaz N, Baygin O, Tuzuner T, et al. Determination of the effect of two different methods of dental anesthesia on pain level in pediatric patients: a cross-over, randomized trial. Niger J Clin Pract. 2022;25(11):1853–1863. doi:10.4103/njcp.njcp_289_22
14. Gao Q, Noël G, Der Khatchadourian Z, et al. Needle-free injection: dental infiltration anesthesia. Int J Pharm. 2021;604:120765. doi:10.1016/j.ijpharm.2021.120765
15. Batista da Silva C, Volpato MC, Muniz BV, et al. Promising potential of articaine-loaded poly(epsilon-caprolactone) nanocapules for intraoral topical anesthesia. PLoS One. 2021;16(2):e0246760. doi:10.1371/journal.pone.0246760
16. Afkhami F, Pirmoazen S, Ardestani A, et al. Comparative evaluation of anesthetic efficacy of inferior alveolar nerve block and inferior alveolar nerve block plus buccal or lingual infiltration using articaine in mandibular molars with irreversible pulpitis: a preliminary prospective randomized single-blind clinical trial. Quintessence Int. 2021;52(9):820–826. doi:10.3290/j.qi.b1864321
17. Vasil’ev YL, Rabinovich SA, Dydykin SS, et al. [Evaluation of the effectiveness of the compression method for infiltration anesthesia of the mandibular molars]. Stomatologiia. 2021;100(1):60–66. doi:10.17116/stomat202110001160
18. Zhang N, Kang Q, Cheng Y. Pulpotomy for teeth with irreversible pulpitis in immature permanent teeth: a retrospective case series study. Sci Rep. 2024;14(1):6395. doi:10.1038/s41598-024-56975-6
19. Ather A, Patel B, Gelfond JAL, et al. Outcome of pulpotomy in permanent teeth with irreversible pulpitis: a systematic review and meta-analysis. Sci Rep. 2022;12(1):19664. doi:10.1038/s41598-022-20918-w
20. Chaitanya M, Bhawalkar A, Bagchi A, et al. Comparative analysis of post-operative pain relief and healing outcomes between single-visit and multiple-visit root canal therapy: a tertiary care study. J Pharm Bioallied Sci. 2024;16(Suppl 3):S2388–s2390. doi:10.4103/jpbs.jpbs_281_24
21. Anisimova NY, Anisimova EN, Ryazancev NA, et al. [Comparative analysis of 2% and 4% articaine solution efficacy and safety for the local anesthesia]. Stomatologiia. 2021;100(5):25–29. doi:10.17116/stomat202110005125
22. Calixto GMF, Muniz BV, Castro SR, et al. Mucoadhesive, thermoreversible hydrogel, containing tetracaine-loaded nanostructured lipid carriers for topical, intranasal needle-free anesthesia. Pharmaceutics. 2021;13(11):1760. doi:10.3390/pharmaceutics13111760
23. Abbasi H, Saqib M, Maqsood A, et al. The effectiveness of single antibiotic paste nitrofurantoin V/S double antibiotic paste in alleviation of post-operative pain of patients suffering from symptomatic irreversible pulpitis-A randomized controlled trial. SAGE Open Med. 2024;12:20503121231220794. doi:10.1177/20503121231220794
24. Anisimova EN, Anisimova NY, Ryazancev NA, et al. [Preventive analgesia for the improvement of local anesthesia efficacy in treatment of acute pulpitis in molars]. Stomatologiia. 2021;100(3):30–34. doi:10.17116/stomat202110003130
25. Akyüz O, Ergün M. The effectiveness of jet (Needle-Free) injector to provide anesthesia in child circumcision under local anesthesia. J Invest Surg. 2022;35(1):44–48. doi:10.1080/08941939.2020.1817635
26. Belevcikli M, Altan H, Demir O. Effect of the new needle-free injection system on pain perception and dental anxiety during anesthesia: randomized controlled split-mouth study. J Dent Anesth Pain Med. 2023;23(1):1–8. doi:10.17245/jdapm.2023.23.1.1
27. Anisimova EN, Anisimova NU, Erilin EA, et al. [Comparative effectiveness of periodontal methods of anesthesia in the treatment of dental caries]. Stomatologiia. 2021;100(2):40–43. doi:10.17116/stomat202110002140
28. Brunton PA, McLean M, Vedagiri S, et al. Jet injection needle-free dental anaesthesia: initial findings. J Dent. 2022;122:104165. doi:10.1016/j.jdent.2022.104165
29. Parirokh M, Paul VA. Present status and future directions-Mechanisms and management of local anaesthetic failures. Int Endodontic J. 2022;55(Suppl 4):951–994. doi:10.1111/iej.13697
30. Nagendrababu V, Duncan HF, Whitworth J, et al. Is articaine more effective than lidocaine in patients with irreversible pulpitis? An umbrella review. Int Endodontic J. 2020;53(2):200–213. doi:10.1111/iej.13215
31. Syed GA, Mulay SA. Comparative evaluation of anesthetic efficacy of 4% articaine and 2% lidocaine for buccal infiltration in adult patients with irreversible pulpitis of maxillary first molar: a prospective randomized study. Contemp Clin Dent. 2022;13(1):61–68. PMID: 35466294; PMCID: PMC9030316. doi:10.4103/ccd.ccd_710_20
32. Dai XY, Lou HD, Wang XY, et al. [A preliminary study on the short-term effectiveness and safety of sublingual immunotherapy-spray for patients with respiratory allergy]. Zhonghua Yu Fang Yi Xue Za Zhi. 2024;58(12):1921–1925. doi:10.3760/cma.j.cn112150-20240921-00761 Wolof
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


