Back to Journals » Cancer Management and Research » Volume 17
Assessing Mean Glandular Dose in Mammography in Jordan According to American College of Radiology (ACR) Standards
Authors Al Hrout R, Ayasrah M , Noor Azman NZ
Received 20 September 2024
Accepted for publication 28 December 2024
Published 10 January 2025 Volume 2025:17 Pages 11—22
DOI https://doi.org/10.2147/CMAR.S497104
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Lu-Zhe Sun
Rasha Al Hrout,1,2 Mohammad Ayasrah,3 Nurul Zahirah Noor Azman2
1Medical Radiologic Technologies, College of Allied Medical Sciences, Zarqa University, Zarqa, 13132, Jordan; 2School of Physics, Universiti Sains Malaysia, Penang, 11800 Gelugor, Malaysia; 3Department of Allied Medical Sciences, Faculty of Applied Medical Science, Jordan University of Science and Technology, Irbid, 22110, Jordan
Correspondence: Nurul Zahirah Noor Azman, School of Physics, Universiti Sains Malaysia, Gelugor, Pulau Pinang, 11800 Gelugor, Malaysia, Tel +604 653 3668, Email [email protected] Mohammad Ayasrah, Department of Allied Medical Sciences Faculty of Applied Medical Sciences, Jordan University of Science and Technology, P.O. Box 3030, Irbid, 22110, Jordan, Tel +96227201000-26939, Fax +96227201087, Email [email protected]
Introduction: Breast cancer is a significant worldwide health issue, particularly in Jordan, where early detection via mammography is essential for effective disease management. Despite the little radiation risk associated with mammography, it is crucial to monitor radiation exposure to guarantee patient safety. This study intends to assess skin entrance exposure and compute the Mean Glandular Dose (MGD) in mammography units to determine adherence to established criteria and pinpoint areas for enhancement.
Methods: To assess MGD, the study utilized the American College of Radiologists (ACR) phantom alongside a RaySafe X2 MAM dosimeter. Measurements of entrance kerma and half-value layer (HVL) were taken across 25 mammography units in Jordan. The MGD was calculated according to the ACR’s 2018 protocol, which provides a standardized approach to ensure accurate and comparable dose estimations. These measurements were then analyzed against the ACR’s threshold of 3 mGy to assess compliance.
Results: The study found that the average MGD across all units was 2.3 mGy, with individual values ranging from 0.95 to 4.10 mGy. Although 67% of the units maintained MGD values within the ACR threshold, 33% exceeded the recommended limit of 3 mGy. Higher MGD values were particularly common in non-accredited facilities, where the average MGD reached 2.7 mGy, compared to 1.6 mGy in accredited units, suggesting gaps in quality control and adherence to best practices in non-accredited centers.
Conclusion: This study emphasizes the critical role of accreditation and adherence to quality standards in maintaining safe and effective mammography practices. While most mammography units in Jordan meet the ACR’s recommended MGD limits, the elevated dose levels in some non-accredited facilities highlight the need for more rigorous implementation of accreditation standards. Improving compliance with established guidelines will enhance breast cancer screening effectiveness, ultimately supporting better early detection and outcomes for breast cancer in Jordan.
Keywords: patient safety in cancer imaging, mammography quality assurance, mean glandular dose, healthcare accreditation, breast cancer screening, patient safety in cancer imaging, radiation dose optimization in cancer screening
Introduction
Breast cancer continues to be a major health issue globally,1 especially in Jordan, where it is the predominant cancer, constituting 20.8% of all malignancies across genders and 38.5% among females, according to the 2018 Jordan Cancer Registry.2 Mammography is essential for early detection, which has been proven to save treatment costs and fatality rates by up to 20%.3
Mammography is the most reliable screening method and necessitates calibrated and regularly inspected equipment to ensure accurate diagnoses and minimize radiation exposure.4 The Jordan Breast Cancer Program (JBCP) provides annual access to high-quality mammography screening for women aged 40 and older, utilizing minimal radiation doses.5
Screening mammography typically involves two projections: (i) craniocaudal (CC) and (ii) mediolateral oblique (MLO) which can be performed digitally via computed radiography (CR), full field digital mammography (FFDM), or digital breast tomosynthesis (DBT), or analogously using screen film mammography (SFM).6,7
While mammography provides significant benefits, female breast tissue is highly sensitive to ionizing radiation, necessitating a balance between its benefits and potential risks.8,9 Reducing the risk of radiation-induced breast cancer requires accurate measurement of breast dosage.10,11 Mean Glandular Dose (MGD) serves as a critical metric for assessing radiation risk and quality control in mammography, ensuring equipment performance, and maintaining radiation doses at levels as low as reasonably achievable (ALARA).4,12
The accuracy of MGD measurement is influenced by variables including breast thickness, imaging protocols, and the characteristics specific to the equipment used.11,13 Variability in dose levels, influenced by clinical imaging parameters and manufacturer specifications, presents significant challenges.14,15
International guidelines confront these complexities. The Mammography Quality Standards Act (MQSA) and the American College of Radiology (ACR) establish standards in the United States to ensure safety and quality in mammography, specifying a maximum mean glandular dose (MGD) of 3 mGy for a 4.2 cm compressed breast phantom.16,17
Research conducted in various regions demonstrates variability in MGD values. Nigeria reported an average MGD of 0.74 mGy, which is considerably below the international standard of 3 mGy.18 China recorded an average MGD of 1.3 mGy, affected by breast thickness and equipment sensitivity.15 In the MENA region, Saudi Arabia exhibited an average MGD of 1.45 mGy,19 whereas Morocco documented MGDs of 1.34 mGy for CC views and 1.48 mGy for MLO views.20 The findings underscore the significance of standardized practices and quality assurance in mammography.
This study aims to evaluate MGD in Jordan using the ACR phantom and RaySafe X2 MAM dosimeter. By assessing entrance exposure and calculating MGD following the 2018 ACR Digital Mammography QC Manual guidelines, the study seeks to contribute to dose optimization and enhance mammography practices in the region.
Materials and Methods
Collection of Samples and Sampling Region
The study encompassed the collection of mammography machines from various locations across Jordan. The research analyzed 82 operational mammography units in Jordan, of which 30% were accredited by the HCAC. In 2021, of the 96 total units recorded, 56.3% were in the commercial sector, 32.3% in state facilities, 7.2% in military hospitals, and 4.2% in university hospitals, underscoring the preeminence of the private sector in mammography services.
Ethical Approval
The Institutional Review Board (IRB) of the Jordan University of Sciences and Technology has granted ethical approval No. 43/160/2023 date 11/5/2023 for the study, ensuring compliance with ethical standards and the preservation of participants’ rights.
Method of Sampling and Sample Size
The selection of participants involved sending two rounds of Email invitations to 82 mammography facilities. The selection of mammography units used a random sampling technique, encompassing both accredited and non-accredited facilities. This approach aimed to provide a comprehensive and representative sample for the study.
Equipment for Data Collection
Digital Mammography X-Ray Machine
The research assessed 25 mammography machines from multiple manufacturers, encompassing a range of technologies such as CR, FFDM, and DBT. Hologic is the predominant model with 8 units, followed by Siemens with 5 units and GE with 4 units. The additional models included Planmed (3 units), Philips (2 units), Fuji (2 units), and Villa Sistemi (1 unit), reflecting a diverse array of equipment manufacturers. The apparatus employs diverse combinations of molybdenum (Mo), rhodium (Rh), and tungsten (W) targets and filters. Operating at a voltage of 28 kVp, frequently utilized in clinical environments, guarantees consistency across the equipment.
The Pro-MAM Accreditation- FF
This phantom is an ACR-Accredited Full-Field Phantom to evaluate the performance of digital mammographic systems. It simulates a compressed breast measuring 42 mm thick with a composition of 50% glandular and 50% adipose tissue. With dimensions of 311.2×190.5 × 41.3 mm3, the phantom covers the entire image detector area and minimizes scattering.21 It accurately replicates the structure of compressed breasts during clinical examinations, including micro-calcifications, fibrous formations, and tumor-like masses. Additionally, the product holds CE certification and complies with IEC and ACR requirements.
The RaySafe X2 MAM Base and Sensor
The RaySafe X2, consisting of the base unit and MAM sensor from Fluke Biomedical (USA), provides a measurement range from 1 μGy to 99.99 Gy with an associated uncertainty of 5%.22 The RaySafe X2 instrument used in this study was calibrated in advance at the Radiation Application Laboratory of The Royal Scientific Society, adhering to manufacturer guidelines and international dosimetry standards. The calibration was conducted for three target-filter combinations: W/Rh, W/Ag, and W/Al. The Raysafe X2 dosimeter delivered the half-value layer (HVL) measurements for each target-filter combination, as well as the tube potential and tube current-time product readings. All measurements in this calibration were conducted twice to assess repeatability. The 5% uncertainty in the instrument’s measurements is specified by RaySafe, as outlined in the instrument’s manual and specifications sheet, which define this expanded uncertainty in accordance with ISO GUM standards (1995, ISBN 92–67-10,188-9).22
This system accurately measures various radiological factors in a single exposure, such as breast entrance dose (mGy), dose rate, kVp, HVL, exposure length, pulses, and dosage per pulse. The measurements were performed using the automated exposure control (AEC) mode of the digital mammography machine. The RaySafe X2 MAM sensor was placed above the phantom to replicate real clinical exposure settings. To ensure full exposure of the dosimeter, it was placed approximately 4 cm away from the chest-wall boundary of the image receptor, following the guidelines outlined in the Mammography ACR Handbook 2018 for Digital Mammography.23
The Mean Glandular Dose (MGD) Dosimetry
MGD dosimetry plays a vital role in ensuring the safety of mammography radiation. It is accurately determined using standardized processes outlined in the Mammography ACR Handbook 2018 and the important research conducted by Dance et al23. The computation employs a thorough equation (Equation 1):
MGD=K g c s………………………………………. Equation 1
where each variable has a distinct function. K denotes the breast incident air kerma at the upper surface of the phantom, g represents the incident air kerma to MGD conversion factor corresponding to 50% glandularity, c signifies the correction factor for disparities in breast composition from 50% glandularity, and s denotes the correction factor for disparities in X-ray spectra. Dance et al have provided tabular values of g and c in relation to the HVL of X-ray beams.24,25 The procedure involves identifying data points against HVL values, from which the exact values of g and c factors are determined for the digital mammography system under investigation. MGD significantly facilitates the assessment of breast radiation risk during imaging and established diagnostic reference values that contributing to regional and national radiology safety regulations. The conventional MGD established for a typical breast with a compressed thickness of 4.2 cm and a glandular tissue to fat ratio of 50:50 is 3.0 mGy per view.26
Data Analysis
The analysis was conducted utilizing IBM SPSS Statistics 27. Descriptive statistics, such as means, standard deviations, and frequencies, were computed to summarize the data. Inferential statistics, including independent sample t-tests and one-way ANOVA, were utilized to evaluate differences between groups, specifically accredited and non-accredited facilities, as well as to investigate the relationship between MGD and mammography equipment parameters (kVp, mAs, and target filtration).
Statistical analyses were conducted to examine the differences and factors affecting MGD across healthcare institutions, taking into account facility accreditation status. A 95% confidence interval was employed to estimate the true mean MGD values, with statistical tests performed at a significance level (alpha) of 0.05, confirming that assumptions were satisfied. This method offered an in-depth analysis of the distribution and factors influencing MGD values across different contexts.
Results and Discussion
Demography and Respond Rate
Out of the 82 initially targeted mammography facilities, the study achieved a response rate of 30.5%, resulting in the participation of 25 sites. Analysis of the data collected from these 25 mammography centers in Jordan revealed that the majority of machines used for mammograms are located in clinics (76%), with a significant number of them being concentrated in the central area (64%). In addition, the level of private sector participation was significant, accounting for 60% of participation as shown in Figure 1, though only 36% of the centers were accredited.
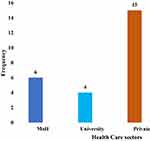 |
Figure 1 Distribution of mammography machines among healthcare sectors. |
Full field digital mammography emerged as the most common type of mammography, accounting for 44.4% of cases in the technical profile as illustrated in Figure 2. The distribution of the target/filter combination was diverse, with Mo/Mo being the most prevalence at 64%, followed by W/Rh at 28%, and Rh/Mo at 8%.
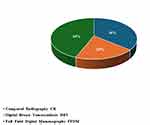 |
Figure 2 Technology profile of mammography units. |
Mean Glandular Dose (MGD)
Measuring MGD directly in clinical settings is challenging, despite its significance in assessing breast cancer risk. Direct measurement of MGD is not feasible; instead, it depends on conversion factors that establish an association between quantifiable dosimetric values and MGD.27 These variables change based on the X-ray spectrum used for the examination, as well as the size and composition of the breast.28,29 Geometrical models of the breast have been established to correlate the measurable value of incident air kerma (in mGy) with MGD.
The most recognized dosimetry approaches for conventional mammography originate from research by Dance et al in the United Kingdom and Wu et al in the United States.28 These systems possess conversion factors specifically tailored for CC projection, a prevalent method in mammography.
Calculations of MGD for mammography are exaggerated by about 30% when basic models are used.30 Phantoms, which mimic the characteristics of the breast are essential for accurately measuring incident air kerma. They provide more reliable QC and make meaningful comparisons between different systems. Nevertheless, the phantoms used in European recommendations, such as those composed of PMMA or PMMA/PE, do not precisely correspond to all breast features,28 particularly for advanced methods such as DBT.31 Nevertheless, these phantoms are deemed enough for quality control purposes. The ACR use a 45 mm thick phantom for quality control testing of digital systems in the United States.32
This estimation process involved utilizing conversion factors provided by Dance et al24 and outlined in the Mammography ACR Handbook 201823 As a result, MGD estimation involved measurements of incident air kerma and HVL, as illustrated in Figure 3. These variables were used in conjunction with tabular conversion factors derived from Monte Carlo simulations to compute MGD.
 |
Figure 3 Example of entrance kerma and HVL readings (A) alongside the sensor image obtained (B) on the ACR phantom Pro-MAM ACR FF (C). |
Table 1 illustrates the range of average entrance dosage (kerma) at the top of the ACR phantom which varied between 3.93 mGy and 17.53 mGy. The mean value obtained was 8.87 mGy, with a standard deviation of 4.42 mGy. The average MGD ranging from 0.95 to 4.10 mGy, with a mean of 2.31 mGy and a standard deviation of 1.02 mGy.
 |
Table 1 Descriptive Statistics of Kerma, HVL, and MGD Obtained in Present Study |
Table 2 displays the range and percentage of MGD values above and below ACR’s MGD, approximately 32% of centers above the maximum allowable (MGD) value of 3.0 mGy as established by the (ACR), with some measurements reaching the level of 4.1 mGy, which is 1.36 times more than the recommended limit.
 |
Table 2 Range and Percentage of MGD Values Above and Below ACR’s MGD |
The findings of the correlation analysis between MGD and the selected equipment parameters (KVP, HVL, and mGy/mAs) are summarized in Table 3. The Pearson correlation analysis indicated a weak negative association between MGD and kVp (r = −0.017) as well as HVL (r = −0.088). Conversely, a slight positive correlation was observed between MGD and mGy/mAs (r = 0.259).
 |
Table 3 Correlation Matrix of Equipment Parameters and MGD |
The Spearman correlation analysis as shown in Table 4 revealed very weak negative correlation was observed between MGD and applied kVp, beam filtration, and mGy per mAs (ρ = −0.057, p = 0.788), HVL (ρ = −0.049, p = 0.815) respectively. Additionally, a weak negative correlation was identified between MGD and mGy per mAs (ρ = −0.087, p = 0.678), with no statistically significant relationship between MGD and tube efficiency.
 |
Table 4 Spearman Correlation Analysis of MGD and Equipment Parameters (kVp, HVL, and mGy per mAs) |
The observed weak and statistically insignificant correlations between MGD and the equipment parameters KVP, HVL, and mGy per mAs in this study highlight the complex interplay of factors affecting glandular dose assessment and optimization in mammography. The theoretical association of KVP and HVL with dose modulation is minimal in correlation with MGD in this analysis,33 indicating that factors such as patient-specific anatomy,34 breast composition,35 and imaging protocols36 are more influential in determining dose levels than equipment-specific parameters alone. The observed negative correlation between MGD and mGy per mAs supports the hypothesis that enhanced tube efficiency, indicated by lower mGy per mAs values, leads to a decrease in radiation dose.37 The observed weak correlation indicates that mGy per mAs alone is inadequate for predicting MGD in clinical practice.
The notable significant positive correlation between HVL and mGy per mAs (ρ = 0.609, p = 0.001) suggests a potential interdependence between these equipment parameters, likely indicating the influence of beam filtration on tube output.38 This finding highlights the significance of examining the interrelationships among equipment parameters in the context of dose optimization efforts. The weak correlations highlight the necessity for a multifactorial approach to dose assessment and optimization in mammography, incorporating patient, equipment, and procedural factors.39
Table 5 presents a range of MGD values observed in studies from the MENA region and globally, highlighting variations in mammography practices and adherence to quality standards. Saudi Arabia reported MGD values ranging from 1.2 to 2.5 mGy, reflecting regulated dose levels.40 Research conducted in Qatar41 and the UAE42 indicated average MGD values of around 1.8 mGy, and 0.80 to 1.8 mGy respectively, consistent with international standards, while Turkey and China reported MGDs within similar ranges.43,44 The present study in Jordan found MGD values ranging from 0.95 to 4.10 mGy, with 32% of centers surpassing the recommended limit of 3.0 mGy. This highlights the need for enhanced QC measures to minimize unnecessary radiation exposure.
 |
Table 5 Comparison of MGD Values in Mammography: Insights from Recent Studies in MENA and Global Regions |
The present study conducted in Jordan found MGD values ranging from 0.95 to 4.10 mGy, with 32% of centers surpassing the recommended limit of 3.0 mGy. Jordan’s findings, when analyzed in an international context, demonstrate alignment with broader trends while also indicating areas for enhancement. These findings suggest a possible need for enhanced QC and strict compliance with international standards in some mammography facilities in Jordan. Nevertheless, the greater proportion of centers beyond the suggested tolerances emphasizes the need of continual monitoring and adjustment to guarantee the safety of patients.
The results underscore the critical importance of accreditation in ensuring superior mammography services. Accredited centers maintained MGDs below 3.0 mGy, in line with international benchmarks. However, among the non-accredited centers, 50% exceeded the maximum ACR limit. This disparity emphasizes the potential influence of accreditation on QA practices and radiation safety. Moreover, private healthcare facilities exhibited a 30% failure rate in meeting ACR guidelines, highlighting the need for consistent QA procedures across sectors. Stringent quality control techniques in medical imaging guarantee excellent results through rigorous analysis and enhancement.47 Assessing MGD in mammography is essential for risk evaluation, system architecture, and reducing radiation exposure while attaining optimal outcomes.48
For women aged over 40 in Jordan, the JBCP endeavors to offer top-tier screening mammography while minimizing radiation exposure risks. The JBCP is committed to the establishment of unified quality assurance (QA) protocols and guidelines for mammography equipment, training, and referral systems. This commitment ensures excellence in screening and diagnostic results while simultaneously minimizing potential adverse effects such as radiation exposure, overdiagnosis, underdiagnosis, and unnecessary interventions.5 The HCAC is responsible for enforcing the Breast Imaging Units Certification Standards (BIUCS) for mammography QC. This involves adhering to nationally agreed-upon standards to keep high-quality screening and diagnostic outcomes.49 Presently, there are 33 mammography centers accredited by HCAC.50
The distribution of accreditation status, based on the MGD limit set by the ACR is listed in Table 6. All evaluated and accredited mammography centers maintained MGDs below 3.0 mGy, in line with international quality benchmarks. However, among the non-accredited centers (N=16), half of them surpassed the maximum ACR limit. This underscores potential variations in QA practices and emphasizes the need of accreditation to ensure radiation safety and achieve optimal imaging results.
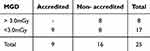 |
Table 6 Distribution of MGD Above and Below 3.0 mGy According to Accreditation Status |
It is evident that the MGD for non-accredited mammography centers (2.7mGy) was approximately double compared to accredited centers (1.6mGy). as depicted in Table 7.
 |
Table 7 MGD Statistics by Accreditation Status |
The significant difference in MGD between non-accredited and accredited mammography centers underscores the potential influence of accreditation in ensuring patient safety and effective radiation dosage management. The results underscore the critical need for accreditation in guaranteeing superior mammography services. To enhance this effect, various tactics may be implemented. Providing financial incentives and subsidies, including the elimination of fees for first accreditation, may encourage additional institutions to comply with the necessary requirements. Customized training programs for imaging specialists can improve compliance with QA guidelines, guaranteeing uniformity in practice. Moreover, public awareness initiatives highlighting the safety and quality benefits of accredited mammography centers may enhance the demand for such services. Implementing these measures would enhance accreditation initiatives, resulting in enhanced patient safety and superior diagnostic outcomes.
Furthermore, the variation in low MGD rates, which reflects the effectiveness of quality management, reveals significant disparities among various sectors. Table 8 illustrates the significant role of university hospitals in achieving and sustaining low MGD rates, with an average MGD of 2 mGy. University centers demonstrate compliance with international guidelines, with none of their mammography equipment exceeding the 3 mGy dosage limit established by the ACR, showcasing a dedication to maintain elevated levels of QC and radiation safety in healthcare institutions affiliated with universities.
 |
Table 8 Distribution of MGD Level Limits Above and Below ACR Limit Among Health Sectors in Jordan |
However, a more complex understanding arises when examining the private health care sector closely. Although the average MGD for all mammography machines in this sector is below 3 mGy, it is noteworthy that 30% (5 machines) of the 15 machines do not match the ACR guidelines, indicating a substantial failure rate of 30%. The MoH centers exhibited the highest incidence of failure and the highest average MGD of 2.84 mGy (Table 9). Specifically, 50% (6 out of 12 centers) of their equipment exceeded the 3 mGy limit. This disparity underscores the potential differences in QA procedures across various healthcare sectors and emphasizes the importance of consistently adhering to international standards to ensure optimal imaging outcomes and patient safety.
 |
Table 9 MGD Statistics by Health Care Sector in Jordan |
Conclusion
This study underscores the critical necessity to lower MGD levels in mammography centers in Jordan, as one-third of these centers surpass the recommended thresholds. Accredited centers that strictly follow ACR guidelines demonstrate the effectiveness of Jordan’s certification program. Significant disparities in MGD levels among various healthcare sectors, particularly the superior performance of university hospitals and the higher failure rates in MoH facilities, highlight the need for further investigation.
A national strategy that incorporates mandatory accreditation, endorsed by the JBCP, could significantly address these disparities and improve patient safety. Essential steps encompass the standardization of mammography protocols, the implementation of continuous quality assurance procedures, and the provision of regular training for radiology personnel to enhance dose management.
Collaborative efforts involving stakeholders from accredited and non-accredited centers are essential for comprehensive improvements in mammography practices. By prioritizing the reduction of MGD levels alongside the maintenance of high-quality imaging, Jordan can achieve optimal imaging results and improve breast cancer screening and treatment, thereby enhancing public health and patient safety nationwide.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding author Mohammad Ayasrah, PhD upon request.
Acknowledgments
We would like to extend our deepest gratitude to the management of the Jordan Breast Cancer Program (JBCP) for their significant assistance in supplying us with QC equipment. We express sincere appreciation to all the members of the participating mammography centers whose cooperation and dedication played a crucial role in the effective implementation of this research.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors did not receive support from any organization for the submitted work, to assist with the preparation of this manuscript, or for conducting this study. No funds, grants, or other support was received.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. Ferlay J, Colombet M, Soerjomataram I, et al. Cancer statistics for the year 2020: an overview. Int J Cancer. 2021. doi:10.1002/ijc.33588
2. MoH J Jordan Cancer Registry: cancer Incidence in Jordan – 2018. Ministry of Health; 2018. Available From: https://moh.gov.jo/ebv4.0/root_storage/ar/eb_list_page/%D8%A7%D9%84%D8%AA%D9%82%D8%B1%D9%8A%D8%B1_%D8%A7%D9%84%D8%B3%D9%86%D9%88%D9%8A_%D9%84%D8%A7%D8%B5%D8%A7%D8%A8%D8%A7%D8%AA_%D8%A7%D9%84%D8%B3%D8%B1%D8%B7%D8%A7%D9%86_%D8%A7%D9%84%D9%85%D8%B3%D8%AC%D9%84%D8%A9_%D9%81%D9%8A_%D8%A7%D9%84%D8%A7%D8%B1%D8%AF%D9%86_%D9%84%D8%B9%D8%A7%D9%85_2018.pdf.
3. Christiansen SR, Autier P, Støvring H. Change in effectiveness of mammography screening with decreasing breast cancer mortality: a population-based study. Eur J Public Health. 2022;32(4):630–635. doi:10.1093/eurpub/ckac047
4. Gonzalez-Ruiz A, Mendoza HIS, Cuevas CLS, et al. An evaluation of the present status of quality assurance program implementation in digital mammography facilities in a developing country. J Radiol Prot. 2022;42(4):041506. doi:10.1088/1361-6498/aca0fe
5. Jordan Breast Cancer Program JJBCPB, Breif JBCP. 2023. Available From: https://www.jbcp.jo/about/15.
6. Hovda T, Tsuruda K, Hoff SR, Sahlberg KK, Hofvind S. Radiological review of prior screening mammograms of screen-detected breast cancer. Eur Radiol. 2021;31(4):2568–2579. doi:10.1007/s00330-020-07130-y
7. Suleiman ME, Brennan PC, Ekpo E, Kench P, McEntee MF. Integrating mammographic breast density in glandular dose calculation. Br J Radiol. 2018;91(1085):20180032. doi:10.1259/bjr.20180032
8. Di Maria S, van Nijnatten TJA, CRLPN J, Vedantham S, Dietzel M, Vaz P. Understanding the risk of ionizing radiation in breast imaging: concepts and quantities, clinical importance, and future directions. Eur J Radiol. 2024;181:111784. doi:10.1016/j.ejrad.2024.111784
9. Hooshmand S, Reed W, Suleiman M, Brennan P. A review of screening mammography: the benefits and radiation risks put into perspective. J Med Imaging Radiat Sci. 2021;53. doi:10.1016/j.jmir.2021.12.002
10. Aşlar E, Şahiner E, Polymeris GS, Meriç N. Feasibility of determining Entrance Surface Dose (ESD) and mean glandular dose (MGD) using OSL signal from BeO dosimeters in mammography. Radiat Phys Chem. 2020;177:109151. doi:10.1016/j.radphyschem.2020.109151
11. Norweck JT, Seibert JA, Andriole KP, et al. ACR–AAPM–SIIM Technical Standard for Electronic Practice of Medical Imaging. J Digit Imaging. 2013;26(1):38–52. doi:10.1007/s10278-012-9522-2
12. Abraham A, Sanghera KP, Gheisari F, et al. Is Radiation-Induced Cardiac Toxicity Reversible? Prospective Evaluation of Patients With Breast Cancer Enrolled in a Phase 3 Randomized Controlled Trial. Int J Radiat Oncol Biol Phys. 2022;113(1):125–134. doi:10.1016/j.ijrobp.2022.01.020
13. Wigati KT, Marshall NW, Lemmens K, et al. On the relevance of modulation transfer function measurements in digital mammography quality control. J Med Imag. 2021;8(2):023505. doi:10.1117/1.JMI.8.2.023505
14. Suliman M II, Mahadi A S, et al. Average Glandular Dose (AGD) and Radiation Dose Optimization in Screen-Film and Digital X-ray Mammography. Appl Sci. 2023;13(21):11901. doi:10.3390/app132111901
15. Du X, Wang J, Zhu BL. Estimated Average Glandular Dose for 1,828 Mammography Procedures in China: a Multicenter Study. Biomed Environ Sci. 2019;32(4):242–249. doi:10.3967/bes2019.034
16. Bhumika NM, Mishra S, Arjun M, Venkatesh MP. Navigating the mammography quality standard act in USA: role of US FDA and future scopes of regulation-A narrative review. J Med Imaging Radiat Sci. 2024;55(4). doi:10.1016/j.jmir.2024.04.013
17. Trinate R Quantitative Evaluation of Image Quality for Dedicated Cone-Beam Breast Computerized Tomography. M.S. The University of Arizona; 2023. Available From: https://www.proquest.com/docview/2856208698/abstract/20B1DD95D29E4C29PQ/1.
18. Josephine J, Christian NC, Zira JD, et al. Estimation of Mean Glandular Doses for Patients Undergoing Mammography Examination in Some Selected Centers in. Vol. 3. Lagos State, Nigeria; 2020.
19. Albahiti S. How Much Radiation Are Women in Saudi Arabia Receiving from Mammography? A Review. Int J Biomed. 2024;14(2):235–239. doi:10.21103/Article14(2)_RA5
20. Tahiri Z, Talbi M, Mansouri ME, et al. Radiation exposure in routine mammography screening: a large observational cross-sectional study in Morocco. Radioprotection. 2024;59(2):104–110. doi:10.1051/radiopro/2024010
21. Project. Pro-MAM ACR FF. Diagnomatic Pro-project DP. 2023. Availabe From: https://diagnomatic.com/devices/pro-mam-accreditation-ff.
22. RaySafe. RaySafe X2 Specifications. Published online 2024. Availble From: https://www.raysafe.com/sites/default/files/5200078-11.2_RaySafe_X2_Specifications_EN.pdf.
23. Berns EA, Pfeiffer DE, Butler PF, et al. Quality Control Manual: 2018 Digital Mammography. ACR. 2018. Available from: https://www.acr.org/-/media/ACR/Files/Clinical-Resources/QC-Manuals/Mammo_QCManual.pdf.
24. Dance DR, Skinner CL, Young KC, Beckett JR, Kotre CJ. Additional factors for the estimation of mean glandular breast dose using the UK mammography dosimetry protocol. Phys Med Biol. 2000;45(11):3225. doi:10.1088/0031-9155/45/11/308
25. Dance DR. Monte-Carlo calculation of conversion factors for the estimation of mean glandular breast dose. Phys Med Biol. 1990;35(9):1211. doi:10.1088/0031-9155/35/9/002
26. Vajuhudeen Z. Mean glandular dose | radiology Reference Article | radiopaedia.org. Radiopaedia. doi:10.53347/rID-79640
27. Teoh KC, Manan HA, Mohd Norsuddin N, Rizuana IH. Comparison of Mean Glandular Dose between Full-Field Digital Mammography and Digital Breast Tomosynthesis. Healthcare. 2021;9(12):1758. doi:10.3390/healthcare9121758
28. Dance DR, Sechopoulos I. Dosimetry in x-ray-based breast imaging. Phys Med Biol. 2016;61(19):R271–R304. doi:10.1088/0031-9155/61/19/R271
29. Jamal N, Ng KH, McLean D. A study of mean glandular dose during diagnostic mammography in Malaysia and some of the factors affecting it. Br J Radiol. 2003;76(904):238–245. doi:10.1259/bjr/66428508
30. Bouwman R, Diaz O, Engen R, et al. Phantoms for quality control procedures in digital breast tomosynthesis: dose assessment. Phys Med Biol. 2013;58:4423–4438. doi:10.1088/0031-9155/58/13/4423
31. Baldelli P, Chevalier M, Bosmans H QUALITY CONTROL IN DIGITAL BREAST TOMOSYNTHESIS (DBT). protocol presented at: 2023; Availabe from: https://www.efomp.org/uploads/f5990c7d-37ad-469d-b37d-74618756b257/QUALITY%20CONTROL%20IN%20DIGITAL%20BREAST%20TOMOSYNTHESIS%20(DBT)_F2.pdf.
32. Reis C, Pascoal A, Sakellaris T, Koutalonis M. Quality assurance and quality control in mammography: a review of available guidance worldwide. Insights Imag. 2013;4(5):539–553. doi:10.1007/s13244-013-0269-1
33. Williams MB, Raghunathan P, More MJ, et al. Optimization of exposure parameters in full field digital mammography. Med Phys. 2008;35(6):2414–2423. doi:10.1118/1.2912177
34. Tromans CE, Highnam R, Morrish O, et al. Patient Specific Dose Calculation Using Volumetric Breast Density for Mammography and Tomosynthesis. Breast Imaging. 2014:158–165. doi:10.1007/978-3-319-07887-8_23
35. Ferrauche G, Tramontin G, Massera RT, Tomal A. Impact of fibroglandular tissue distribution and breast shape in voxelized breast models for dosimetry in mammography. Phys Med Biol. 2023;68(7):074003. doi:10.1088/1361-6560/acbefd
36. Chang TY, Wu J, Liu PY, Liu YL, Luzhbin D, Lin HC. Using Breast Tissue Information and Subject-Specific Finite-Element Models to Optimize Breast Compression Parameters for Digital Mammography. Electronics. 2022;11(11):1784. doi:10.3390/electronics11111784
37. Fitton I, Tsapaki V, Zerbib J, et al. Two-Dimensional Mammography Imaging Techniques for Screening Women with Silicone Breast Implants: a Pilot Phantom Study. Bioengineering. 2024;11(9):884. doi:10.3390/bioengineering11090884
38. Shrestha S, Vedantham S, Karellas A. Towards Standardization of X-ray Beam Filters in Digital Mammography and Digital Breast Tomosynthesis: monte Carlo simulations and analytical modelling. Phys Med Biol. 2017;62(5):1969–1993. doi:10.1088/1361-6560/aa58c8
39. Adelodun M, Anyanwu E. Comprehensive risk management and safety strategies in radiation use in medical imaging. Int J Front Med Surg Res. 2024;6. doi:10.53294/ijfmsr.2024.6.1.0039
40. Albeshan SM, Alhulail AA, Almuqbil MM. Reporting average glandular dose and its associations with age and exposure parameters. Radiat Phys Chem. 2024;223:112004. doi:10.1016/j.radphyschem.2024.112004
41. Al-Naemi HM, Taha OB, Al-attar AO, et al. Evaluation of Mean Glandular Dose from Digital Mammography Exams at Qatar and Compared with International Guidelines Levels. J Adv Med Med Res. 2016:1–9. doi:10.9734/BJMMR/2016/23129
42. Abdulwahid Noor K, Mohd Norsuddin N, Abdul Karim MK, Che Isa IN, Alshamsi W. Estimating Local Diagnostic Reference Levels for Mammography in Dubai. Diagn Basel Switz. 2023;14(1):8. doi:10.3390/diagnostics14010008
43. Parmaksız A, Ataç GK, Bulur E, İnal T, Alhan A. AVERAGE GLANDULAR DOSES AND NATIONAL DIAGNOSTIC REFERENCE LEVELS IN MAMMOGRAPHY EXAMINATIONS IN TURKEY. Radiat Prot Dosimetry. 2020;190(1):100–107. doi:10.1093/rpd/ncaa080
44. Xu H, Yue B, Cheng J, et al. A Survey of Mean Glandular Doses and Suggestions on National Diagnostic Reference Levels for Digital Mammography in China. Health Phys. 2024. doi:10.1097/HP.0000000000001853
45. Ahmed Shaker Hegian Z, Moh’d Abu Tahoun L, Ramli RM, Noor Azman NZ. The relationship between mean glandular dose and compressed breast thickness specified for Jordan. Radiat Prot Dosimetry. 2024;200(1):25–31. doi:10.1093/rpd/ncad259
46. Asadollahzadeh N, Razavi S, Zare MH. A survey on mean glandular dose in mammography examination and the factors affecting it in Shahid Sadoughi Hospital, Yazd, Iran. Radiat Prot Dosimetry. 2024;200(9):809–821. doi:10.1093/rpd/ncae121
47. Larson DB, Boland GW. Imaging Quality Control in the Era of Artificial Intelligence. J Am Coll Radiol JACR. 2019;16(9 Pt B):1259–1266. doi:10.1016/j.jacr.2019.05.048
48. Patel V, Sindhwani G, Gupta M, et al. A Comprehensive Approach Towards Quality and Safety in Diagnostic Imaging Services: our Experience at a Rural Tertiary Health Care Center. J Clin Diagn Res JCDR. 2017;11(8):TC10–TC16. doi:10.7860/JCDR/2017/29545.10354
49. HCAC. Breast Imaging Units Certification Standards. Breast Imaging Units Certification Standards. 2023. Available from: https://hcac.jo/en-us/Accreditation/Breast-Imaging-Units-Certification-Standards.
50. JBCP. Situational Analysis Reports for 2021. Jordan Breast Canc Prog. 2021.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Perceived Barriers and Facilitators to Breast Cancer Screening Among Women in Saudi Arabia
AlAbdulKader A, Gari D, Al yousif G, Alghamdi A, AlKaltham S, AlDamigh F, AlEisawi Y, AlGhamdi A, Al-Hayek O, AlMudhi A
Breast Cancer: Targets and Therapy 2023, 15:505-513
Published Date: 25 July 2023

