Back to Journals » Infection and Drug Resistance » Volume 17
Association Between COVID-19 and Diabetes Management Indices in Japanese Type 2 Diabetes Mellitus Patients: A Single-Center, Retrospective Study
Authors Furumachi K , Kagatsume T, Higuchi A, Kozaru M, Kumagai E, Hosohata K
Received 19 June 2024
Accepted for publication 23 August 2024
Published 29 August 2024 Volume 2024:17 Pages 3759—3767
DOI https://doi.org/10.2147/IDR.S475917
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Kazuhiro Furumachi,1 Tatsuki Kagatsume,2 Akari Higuchi,2 Mariko Kozaru,2 Etsuko Kumagai,1 Keiko Hosohata2
1Department of Nephrology, Kenwakai Hospital, Nagano, Japan; 2Education and Research Center for Clinical Pharmacy, Faculty of Pharmacy, Osaka Medical and Pharmaceutical University, Osaka, Japan
Correspondence: Keiko Hosohata, Education and Research Center for Clinical Pharmacy, Faculty of Pharmacy, Osaka Medical and Pharmaceutical University, Osaka, Japan, Tel +81-72-690-1271, Fax +81-72-690-1023, Email [email protected]
Purpose: The aim of the study was to determine the association between coronavirus disease 2019 (COVID-19) infection and diabetes management indices in patients with type 2 diabetes mellitus.
Patients and Methods: A single-center, retrospective, observational study of patients with type 2 diabetes mellitus at Kenwakai Hospital (Nagano, Japan) was conducted. Data of 95 patients (mean age, 72 ± 12 years; men, 67.4%) who visited between March 1, 2019 and February 28, 2022 were obtained from the hospital’s electronic information system. COVID-19 was diagnosed by a chemiluminescent enzyme immunoassay (CLEIA).
Results: There was no association between COVID-19 infection and age, sex, hemodialysis treatment status, or the Charlson Comorbidity Index. After adjustment for possible confounding factors, the incidence of COVID-19 infection was significantly correlated with HbA1c ≥ 7.0% (odds ratio [OR], 5.51; 95% confidence interval [CI], 1.30– 23.26).
Conclusion: The results suggest an association between high HbA1c levels and COVID-19 infection in patients with type 2 diabetes mellitus. Appropriate management of diabetes mellitus, focusing on HbA1c levels, may help prevent COVID-19 infection and severe disease after infection.
Keywords: Type 2 diabetes mellitus, COVID-19, risk factors, HbA1c, Japanese
Introduction
Diabetes mellitus increases the risk of infectious diseases, regardless of whether it is type 1 or 2.1 In particular, poor glycemic control can lead to increased susceptibility to infection due to decreased phagocytic and bactericidal functions of polymorphonuclear neutrophils and decreased complement binding to antigen-antibody complexes,2–5 increased susceptibility to severe infections,6 and increased risks of hospitalization and death.7–9 Epidemics of SARS (2003) and H1N1 influenza (2009) have shown that a history of diabetes mellitus is an independent factor that increases the risks of hospitalization and severe illness,10–12 and vaccination is recommended to prevent severe illness caused by viral infections.13 Similarly, for the COVID-19 pandemic since 2020, a history of diabetes mellitus was found to increase the risk of severe disease,14 whereas no consistent trend has emerged regarding the impact of diabetes mellitus on the risk of COVID-19 infection itself. Reports from Europe, the United States, and China have shown no clear difference in the prevalence of diabetes mellitus in COVID-19-infected patients compared with control populations.15,16 In Japan, the prevalence of diabetes mellitus in hospitalized patients with COVID-19 infection was similar to the prevalence in the same age group in the general population;17 therefore, we cannot definitively say that diabetes mellitus increases the risk of COVID-19 infection. In addition, which baseline information, including type 2 diabetes indices, is the most associated with COVID-19 infection has yet to be clarified. The aim of this study was to retrospectively examine the association between type 2 diabetes mellitus and the risk of COVID-19 infection using real-world clinical data.
Materials and Methods
Subjects and Data Collection
This was a retrospective, observational, cohort study, which was approved by the Ethics Committee of Kenwakai Hospital (No. 2023004) and Osaka Medical and Pharmaceutical University (No. 2323–061) and was conducted in accordance with the Declaration of Helsinki. The Ethics Committee waived the need for informed consent from patients because of the retrospective and anonymous nature of the study. Data of eligible patients (≥20 years) with type 2 diabetes mellitus who visited Kenwakai Hospital (Nagano, Japan) between March 1, 2019 and February 28, 2022 were collected. The data of patients without information on HbA1c (n = 1), body mass index (BMI) (n = 6), or smoking status (n = 21), as well as of patients who did not receive continuous treatment with antidiabetic agents (n = 53), were excluded. Finally, the remaining 95 patients were included in the present analyses (Figure 1).
 |
Figure 1 Flow chart of the study cohort. |
In daily practice, COVID-19 was diagnosed by a chemiluminescence enzyme immunoassay (CLEIA). The CLEIA test reagent (Lumipulse SARS-CoV-2 Ag kit) and analyzer (LUMIPULSE G600II) were supplied by Fujirebio (Osaka, Japan). Electronic medical charts were used to collect data of patients infected and not infected with COVID-19. The collected data included demographic data, clinical laboratory data, vital signs, diagnosis, and medication history. As a surrogate marker for insulin resistance, the triglyceride-glucose (TyG) index was calculated as follows: ln(fasting TG [mg/dL] × fasting glucose [mg/dL]/2).18
Outcome
The primary outcome was defined as infection with COVID-19 during the observation period.
Statistical Analysis
Continuous variables are expressed as means ± standard deviation (SD). Logistic regression models were used to examine the associations between the risk of COVID-19 infection and patients’ characteristics. Significance was defined as a P-value <0.05 (two-tailed). All statistical analyses were performed using JMP 13 (SAS Institute, Cary, NC, USA).
Results
Patients’ Characteristics
Table 1 shows the characteristics of the study patients. Of the 95 patients, 67.4% were men. The mean age was 72.1 ± 11.6 years; 14 (14.7%) patients were in the age group <60 years, 20 (21.1%) were aged 60–69 years, 19 (20.0%) aged 70–74 years, 18 (18.9%) aged 75–79 years, 13 (13.7%) aged 80–84 years, and 11 (11.6%) aged 85 years or older. The mean BMI was 22.6 ± 3.2 kg/m2; the BMI was under 18.5 kg/m2 in 10 (10.5%) patients, 18.5–24.9 kg/m2 in 66 (69.5%) patients, and above 25.0 kg/m2 in 1 (1.0%) patient. Of the study patients, 9 (9.5%) were classified as smokers, and 66 (69.5%) were on maintenance dialysis due to chronic kidney disease (CKD). Mean systolic blood pressure (BP) was 147.3 ± 26.3 mmHg; systolic BP was under 140 mmHg in 36 (37.9%) patients and above 140 mmHg in 58 (61.1%) patients. Mean diastolic BP was 77.7 ± 15.6 mmHg; diastolic BP was under 90 mmHg in 75 (78.9%) patients and above 90 mmHg in 19 (20.0%) patients. Mean total cholesterol was 145.6 ± 31.1 mg/dL; total cholesterol was under 175 mg/dL in 67 (70.5%) patients, and above 175 mg/dL in 12 (12.6%). The mean triglyceride level was 136.0 ± 82.2 mg/dL; the triglyceride level was under 150 mg/dL in 60 (63.2%) patients and above 150 mg/dL in 28 (29.5%) patients. The median value of the Charlson Comorbidity index was 8 (6–9), with 46 (48.4%) patients having a value under 8 and 49 patients (51.6%) above 8. Mean HbA1c was 6.7 ± 0.9%; HbA1c was under 7.0% in 64 (67.4%) patients and above 7.0% in 31 (32.6%) patients. The mean serum glucose was 175.7 ± 58.8 mg/dL; serum glucose was under 126 mg/dL in 13 (13.7%) patients and above 126 mg/dL in 82 (86.3%) patients. The mean TyG index was 9.2 ± 0.7, with 33 (34.7%) patients having a value under 9 and 55 (57.9%) above 9.
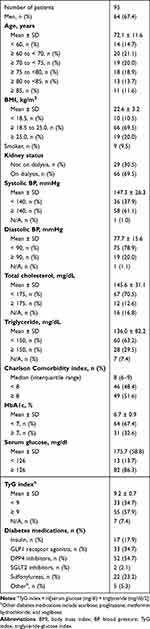 |
Table 1 Baseline Characteristics of Study Patients |
Drug therapy was prescribed as follows: insulin, 17 (17.9%); GLP1 receptor agonists, 33 (34.7%); DPP4 inhibitors, 52 (54.7%); SGLT2 inhibitors, 2 (2.1%); sulfonylureas, 22 (23.2%); other, 5 (5.3%). The most commonly prescribed agents were DPP4 inhibitors (54.7%), followed by GLP1 receptor agonists (34.7%) and sulfonylureas (23.2%). Of the 95 patients, 13 (13.7%) were diagnosed with COVID-19 infection by CLEIA for the SARS-CoV-2 virus. Of the 13 patients who tested positive for COVID-19 infection, 10 had mild infection (76.9%), and 3 had moderate infection (23.1%).
Factors Associated with the Primary Outcome
Tables 2 and 3 show the odds ratios for infection with COVID-19. Univariate regression analysis showed no significant differences in age, sex, dialysis medication, systolic BP, diastolic BP, total cholesterol, triglyceride, Charlson Comorbidity index, BMI, HbA1c, serum glucose, or TyG index with COVID-19 infection (Table 2). After adjusting for relevant factors (age, sex, smoking status, dialysis medication, and Charlson Comorbidity index), multivariate logistic regression analysis identified HbA1c as being significantly and independently correlated with COVID-19 infection (OR: 5.51, 95% CI: 1.30–23.26, P = 0.020; Table 3).
 |
Table 2 Univariate Logistic Regression Analysis for the Infection with COVID-19 |
 |
Table 3 Multivariate Logistic Regression Analysis for the Infection with COVID-19 |
Discussion
In the present study, high HbA1c levels were significantly correlated with COVID-19 infection after adjusting for possible confounding factors (age, sex, smoking, dialysis medication, and Charlson Comorbidity index). To the best of our knowledge, this is the first study to identify the potential relevance of HbA1c to COVID-19 infection in Japanese patients.
HbA1c is the result of nonenzymatic modification of red blood cells by exposure to hyperglycemia, and it is a stable indicator reflecting chronic hyperglycemia.19 Hyperglycemia may be a factor in determining COVID-19 morbidity because neutrophils adhere to endothelial cells, chemotaxis and bactericidal activity are reduced, and complement activity is decreased due to glycosylation.3 The present results are consistent with these reports, and it is important to maintain appropriate diabetes management indices to help prevent COVID-19 infection.
Whether appropriate control of diabetes management indices is associated with the incidence of COVID-19 infection in diabetic patients remains unclear,20 but there have been several reports of an association between severe disease and death. For example, a retrospective study showed that HbA1c of 7.0% or higher was associated with higher severity of pulmonary involvement and mortality from COVID-19 infection,21 and an observational, cross-sectional study showed an increased risk of hospitalization in adult type 1 diabetic patients with median HbA1c of 8.6%.22 Regarding COVID-19-related mortality, a whole-population study indicated that patients with HbA1c of 10.0% or higher showed an increased mortality rate regardless of whether they had type 1 or 2 diabetes mellitus; particularly in patients with type 2 diabetes mellitus, the mortality rate increased significantly with increasing HbA1c.23 A cohort study in England demonstrated that, in comparison with non-diabetic patients, an increased risk of COVID-19-related mortality was observed with HbA1c ≥7.5%, but diabetic patients with HbA1c <7.5% also exhibited a significantly higher risk of death.24 In an analysis of diabetic patients infected with COVID-19 in the United States, the mean HbA1c level was 7.5%, and although 33.1% of patients died, the association was not significant. However, since being on insulin therapy was correlated with the risk of death, insulin therapy and obesity, reflecting the duration of long-term diabetes, have been reported to be risk factors.25
As for BMI, a meta-analysis showed that higher values are associated with more severe COVID-19 infection in all age groups, especially elderly persons.26 In the present results, the independent association of BMI with the risk of COVID-19 infection in diabetes populations was U-shaped, with a nadir at BMI of 18.5–24.9 kg/m2. This is in agreement with a report that the relationship between BMI and COVID-19-related mortality was U-shaped, with a significant increase in the risk of death for both type 1 and type 2 diabetes mellitus patients at BMI <20 kg/m2 and BMI >40 kg/m2 in a population-based cohort study of people with diagnosed diabetes mellitus.27 Regarding fasting blood glucose levels, some studies reported an increased risk of severe COVID-19 infection in diabetic patients with levels >180 mg/dL. For example, fasting plasma glucose levels of 200 mg/dL or higher are a significant predictor of 28-day mortality,28 and understanding and achieving good control of hyperglycemia is important for improving the prognosis. However, an observational study reported that HbA1c and mean blood glucose levels were not associated with severe disease.29 As for hypoglycemic medications, there is no known causal relationship with the risk of developing severe COVID-19 infection, but there are reports that insulin, DPP-4 inhibitor, and metformin use were associated with the prognosis.30–37 In addition, risk factors for severe COVID-19 infection in diabetic patients were reportedly correlated with a history of cardiovascular disease, chronic kidney disease, obesity, cerebrovascular disease, and patient background, including male, older age, race, and social poverty,17,23,24 and combined factors are likely to increase the risk of severe COVID-19 infection. Patients with type 2 diabetes mellitus, metabolic syndrome, and obesity exhibited altered systolic and diastolic functions on echocardiography after SARS-CoV-2 virus infection due to an increased inflammatory burden. This change is related to the degree of pre-existing metabolic disorders and the degree of inflammation.
Similarly, the risk of COVID-19 in diabetic patients is likely to be affected by diabetes management indices, in addition to various factors such as patient background, and appropriate management may lead to the prevention of morbidity, reduced severity of disease, and improvement of the prognosis.
Limitations
This study had some limitations. First, this was a retrospective study with a relatively small population. Second, all data were from one hospital in Japan and did not include non-diabetic patients, so the findings may not be generalizable to other populations. Finally, genetic factors should be considered, because gene mutations such as FOXP4, ABO, TAC4, DPP9, and IFNAR2 are associated with COVID-19 infection.38–41 Recently, it has been reported that the DOCK2 gene mutation doubles the risk of severe disease in 10% of East Asians, including Japanese.42 Therefore, future studies of the effects of various genetic variants on the diagnosis and severity of COVID-19 in patients are warranted.
Conclusion
There was an association between HbA1c and COVID-19 infection in diabetic patients. Appropriate diabetes management, focusing particularly on HbA1c, is considered important to decrease the risk of COVID-19 infection and, ultimately, to prevent severe disease after infection. Further studies with larger populations are needed to confirm the present findings and assess the utility of risk factors for COVID-19 infection in Japanese patients.
Data Sharing Statement
All data relevant to the study are included in the article.
Acknowledgments
The authors would like to sincerely thank all investigators for their help and support.
Funding
This work was supported by JSPS KAKENHI (grant no. JP21K06722).
Disclosure
All authors report no competing interests associated with this work.
References
1. Abramson N, Melton B. Leukocytosis: basics of clinical assessment. Am Family Phys. 2000;62(9):2053–2060.
2. Kim JH, Park K, Lee SB, et al. Relationship between natural killer cell activity and glucose control in patients with type 2 diabetes and prediabetes. J Diabetes Invest. 2019;10(5):1223–1228. doi:10.1111/jdi.13002
3. Casqueiro J, Casqueiro J, Alves C. Infections in patients with diabetes mellitus: a review of pathogenesis. Indian J Endocrinol Metab. 2012;16(Suppl1):S27–36. doi:10.4103/2230-8210.94253
4. Jafar N, Edriss H, Nugent K. The effect of short-term hyperglycemia on the innate immune system. Am J Med Sci. 2016;351(2):201–211. doi:10.1016/j.amjms.2015.11.011
5. Chovancova Z. Secondary immunodeficiency as a consequence of chronic diseases. Vnitrni lekarstvi. 2019;65(2):117–124. [Sekundarni imunodeficience jako nasledek chronickych onemocněni]. doi:10.36290/vnl.2019.024
6. van Crevel R, van de Vijver S, Moore DAJ. The global diabetes epidemic: what does it mean for infectious diseases in tropical countries? Lancet Diabetes Endocrinol. 2017;5(6):457–468. doi:10.1016/S2213-8587(16)30081-X
7. Uzu T, Sawaguchi M, Maegawa H, Kashiwagi A, Shiga Microalbuminuria Reduction Trial G. Reduction of microalbuminuria in patients with type 2 diabetes: the Shiga Microalbuminuria Reduction Trial (SMART). Diabetes Care. 2007;30(6):1581–1583. doi:10.2337/dc06-2493
8. McAlister FA, Majumdar SR, Blitz S, Rowe BH, Romney J, Marrie TJ. The relation between hyperglycemia and outcomes in 2471 patients admitted to the hospital with community-acquired pneumonia. Diabetes Care. 2005;28(4):810–815. doi:10.2337/diacare.28.4.810
9. Lepper PM, Ott S, Nuesch E, et al. Serum glucose levels for predicting death in patients admitted to hospital for community acquired pneumonia: prospective cohort study. BMJ. 2012;
10. Yang JK, Feng Y, Yuan MY, et al. Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet Med. 2006;23(6):623–628. doi:10.1111/j.1464-5491.2006.01861.x
11. Yang JK, Lin SS, Ji XJ, Guo LM. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta diabetologica. 2010;47(3):193–199. doi:10.1007/s00592-009-0109-4
12. Allard R, Leclerc P, Tremblay C, Tannenbaum TN. Diabetes and the severity of pandemic influenza A (H1N1) infection. Diabetes Care. 2010;33(7):1491–1493. doi:10.2337/dc09-2215
13. Dos Santos G, Tahrat H, Bekkat-Berkani R. Immunogenicity, safety, and effectiveness of seasonal influenza vaccination in patients with diabetes mellitus: a systematic review. Hum Vaccines Immunother. 2018;14(8):1853–1866. doi:10.1080/21645515.2018.1446719
14. Fadini GP, Morieri ML, Longato E, Avogaro A. Prevalence and impact of diabetes among people infected with SARS-CoV-2. J Endocrinol Invest. 2020;43(6):867–869. doi:10.1007/s40618-020-01236-2
15. Pugliese G, Vitale M, Resi V, Orsi E. Is diabetes mellitus a risk factor for coronavirus disease 19 (COVID-19)? Acta diabetologica. 2020;57(11):1275–1285. doi:10.1007/s00592-020-01586-6
16. Wang L, Gao P, Zhang M, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA. 2017;317(24):2515–2523. doi:10.1001/jama.2017.7596
17. Matsunaga N, Hayakawa K, Terada M, et al. Clinical epidemiology of hospitalized patients with coronavirus disease 2019 (COVID-19) in Japan: report of the COVID-19 Registry Japan. Clinical Infect Dis. 2021;73(11):e3677–e3689. doi:10.1093/cid/ciaa1470
18. Simental-Mendia LE, Rodriguez-Moran M, Guerrero-Romero F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord. 2008;6(4):299–304. doi:10.1089/met.2008.0034
19. Seino Y, Nanjo K, Tajima N, et al.; Committee of the Japan Diabetes Society on the Diagnostic Criteria of Diabetes M. Report of the committee on the classification and diagnostic criteria of diabetes mellitus. J Diabetes Invest. 2010;1(5):212–228. doi:10.1111/j.2040-1124.2010.00074.x.
20. Lim S, Bae JH, Kwon HS, Nauck MA. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol. 2021;17(1):11–30. doi:10.1038/s41574-020-00435-4
21. Lu X, Cui Z, Pan F, et al. Glycemic status affects the severity of coronavirus disease 2019 in patients with diabetes mellitus: an observational study of CT radiological manifestations using an artificial intelligence algorithm. Acta diabetologica. 2021;58(5):575–586. doi:10.1007/s00592-020-01654-x
22. O’Malley G, Ebekozien O, Desimone M, et al. COVID-19 hospitalization in adults with Type 1 diabetes: results from the T1D exchange multicenter surveillance study. J Clin Endocrinol Metab. 2021;106(2):e936–e942. doi:10.1210/clinem/dgaa825
23. Barron E, Bakhai C, Kar P, et al. Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study. Lancet Diabetes Endocrinol. 2020;8(10):813–822. doi:10.1016/S2213-8587(20)30272-2
24. Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–436. doi:10.1038/s41586-020-2521-4
25. Agarwal S, Schechter C, Southern W, Crandall JP, Tomer Y. Preadmission diabetes-specific risk factors for mortality in hospitalized patients with diabetes and coronavirus disease 2019. Diabetes Care. 2020;43(10):2339–2344. doi:10.2337/dc20-1543
26. Malik VS, Ravindra K, Attri SV, Bhadada SK, Singh M. Higher body mass index is an important risk factor in COVID-19 patients: a systematic review and meta-analysis. Environ. Sci. Pollut. Res. Int. 2020;27(33):42115–42123. doi:10.1007/s11356-020-10132-4
27. Holman N, Knighton P, Kar P, et al. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study. Lancet Diabetes Endocrinol. 2020;8(10):823–833. doi:10.1016/S2213-8587(20)30271-0
28. Yang P, Wang N, Wang J, Luo A, Gao F, Tu Y. Admission fasting plasma glucose is an independent risk factor for 28-day mortality in patients with COVID-19. J Med Virol. 2021;93(4):2168–2176. doi:10.1002/jmv.26608
29. Ling P, Luo S, Zheng X, Cai G, Weng J. Elevated fasting blood glucose within the first week of hospitalization was associated with progression to severe illness of COVID-19 in patients with preexisting diabetes: a multicenter observational study. J Diabet. 2021;13(1):89–93. doi:10.1111/1753-0407.13121
30. Wargny M, Potier L, Gourdy P, et al. Predictors of hospital discharge and mortality in patients with diabetes and COVID-19: updated results from the nationwide CORONADO study. Diabetologia. 2021;64(4):778–794. doi:10.1007/s00125-020-05351-w
31. Chen Y, Yang D, Cheng B, et al. Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication. Diabetes Care. 2020;43(7):1399–1407. doi:10.2337/dc20-0660
32. Mirani M, Favacchio G, Carrone F, et al. Impact of comorbidities and glycemia at admission and dipeptidyl peptidase 4 inhibitors in patients with Type 2 diabetes with COVID-19: a case series from an academic hospital in Lombardy, Italy. Diabetes Care. 2020;43(12):3042–3049. doi:10.2337/dc20-1340
33. Cariou B, Hadjadj S, Wargny M, et al. Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study. Diabetologia. 2020;63(8):1500–1515. doi:10.1007/s00125-020-05180-x
34. Perez-Belmonte LM, Torres-Pena JD, Lopez-Carmona MD, et al. Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COVID-19 in association with glucose-lowering drugs: a nationwide cohort study. BMC Med. 2020;18(1):359. doi:10.1186/s12916-020-01832-2
35. Sardu C, D’Onofrio N, Balestrieri ML, et al. Outcomes in patients with hyperglycemia affected by COVID-19: can we do more on glycemic control? Diabetes Care. 2020;43(7):1408–1415. doi:10.2337/dc20-0723
36. Wang J, Cooper JM, Gokhale K, et al. Association of metformin with susceptibility to COVID-19 in people with Type 2 diabetes. J Clin Endocrinol Metab. 2021;106(5):1255–1268. doi:10.1210/clinem/dgab067
37. Oh TK, Song IA. Metformin use and risk of COVID-19 among patients with type II diabetes mellitus: an NHIS-COVID-19 database cohort study. Acta diabetologica. 2021;58(6):771–778. doi:10.1007/s00592-020-01666-7
38. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in china: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi:10.1001/jama.2020.2648
39. Rao S, Baranova A, Cao H, Chen J, Zhang X, Zhang F. Corrigendum to: genetic mechanisms of COVID-19 and its association with smoking and alcohol consumption. Briefings Bioinf. 2021;22(6). doi:10.1093/bib/bbab357
40. Muhammad JS, Siddiqui R, Khan NA. COVID-19: is there a link between alcohol abuse and SARS-CoV-2-induced severe neurological manifestations? ACS Pharmacol. Transl. Sci. 2021;4(2):1024–1025. doi:10.1021/acsptsci.1c00073
41. Pairo-Castineira E, Clohisey S, Klaric L, et al. Genetic mechanisms of critical illness in COVID-19. Nature. 2021;591(7848):92–98. doi:10.1038/s41586-020-03065-y
42. Namkoong H, Edahiro R, Takano T, et al. DOCK2 is involved in the host genetics and biology of severe COVID-19. Nature. 2022;
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

