Back to Journals » Journal of Inflammation Research » Volume 18
Association Between Serum Uric Acid to High-Density Lipoprotein Cholesterol Ratio and Pneumonia After Endovascular Treatment of Vertebrobasilar Artery Occlusion
Authors Lan W, Yuan K , Xiao L, Qiu F, Sun W , Xu L, Cao H, Zhu W, Du M, Liu X
Received 19 August 2024
Accepted for publication 18 February 2025
Published 26 February 2025 Volume 2025:18 Pages 2899—2908
DOI https://doi.org/10.2147/JIR.S492095
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Wenya Lan,1,2,* Kang Yuan,3,* Lulu Xiao,3 Feng Qiu,1 Wen Sun,4 Lili Xu,1 Hui Cao,1 Wusheng Zhu,3 Mingyang Du,1 Xinfeng Liu2
1Department of Cerebrovascular Disease Treatment Center, the Affiliated Brain Hospital of Nanjing Medical University, Nanjing Brain Hospital, Nanjing, People’s Republic of China; 2Department of Neurology, Affiliated Jinling Hospital, Nanjing Medical University, Nanjing, People’s Republic of China; 3Department of Neurology, Affiliated Jinling Hospital, Medical School of Nanjing University, Nanjing, 210002, People’s Republic of China; 4Stroke Center and Department of Neurology, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei, Anhui, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Mingyang Du, Department of Cerebrovascular Disease treatment Center, the Affiliated Brain Hospital of Nanjing Medical University, Nanjing Brain Hospital, Nanjing, People’s Republic of China, Tel +862582296590, Email [email protected] Xinfeng Liu, Department of Neurology, Jinling Hospital, Nanjing Medical University, No. 305 East Zhongshan Road, Nanjing, Jiangsu Province, 210000, People’s Republic of China, Tel +862584801861, Fax +862584805169, Email [email protected]
Background: The uric acid to high-density lipoprotein cholesterol ratio (UHR) is a novel marker of inflammation and metabolism. We aimed to explore the association of UHR with pneumonia after endovascular thrombectomy (EVT) in patients with vertebrobasilar artery occlusion (VBAO).
Methods: We retrospectively enrolled participants diagnosed with acute VBAO treated with EVT within 24 hours of estimated occlusion time from the multicenter PERSIST study. The primary outcome was pneumonia within 7 days after EVT according to the Pneumonia in Stroke Consensus Group recommendations. We utilized the restricted cubic spline curve to explore the dose–response relationship between UHR and pneumonia. We used multivariable logistic regression models to assess the association between UHR and the risk of pneumonia after EVT and verified the findings in subgroup analysis.
Results: Three hundred and seventy-eight patients were enrolled in this study, and 236 (62.4%) were diagnosed with pneumonia. In multivariable models, a higher UHR was associated with an increased risk of pneumonia after EVT (odds ratio [OR], 1.05; 95% confidence interval [CI], 1.01– 1.10; P = 0.020; tertile 3 versus tertile 1: OR, 2.09; 95% CI, 1.15– 3.82; P = 0.016). The dose–response relationship indicated that UHR was linearly associated with the risk of pneumonia (P = 0.888). The association between UHR and pneumonia remained significant in different subgroups.
Conclusion: This study demonstrated that a higher UHR was associated with an increased risk of pneumonia in VABO patients treated with EVT. Further studies were warranted to verify the prognostic values of UHR in pneumonia after EVT.
Keywords: pneumonia, vertebrobasilar artery occlusion, stroke, thrombectomy, uric acid to high-density lipoprotein cholesterol ratio
Introduction
Endovascular treatment (EVT) is considered an effective therapeutic approach for acute ischemic stroke due to vertebrobasilar artery occlusion (VBAO), which accounts for 10% to 20% of large artery occlusion strokes.1–3 Although EVT has significantly improved clinical outcomes for patients with VBAO compared with optimal medical management, approximately 50% of these patients still do not achieve functional independence after 90 days, due to factors such as advanced age, a higher 24-h NIHSS and incomplete recanalization.4–6 Pneumonia is a frequent complication in ischemic stroke, particularly in those with posterior circulation stroke and dysphagia, and it is a significant factor contributing to poor clinical outcomes.7–10 Previous studies indicated that the incidence of pneumonia in patients with VBAO was approximately 70% and was significantly associated with early mortality.11 Hence, it is important to identify biomarkers that could predict pneumonia in VBAO patients after EVT at an early stage, facilitating the recognition of high-risk patients and enabling timely intervention.
The uric acid (UA) to high-density lipoprotein cholesterol (HDL) ratio (UHR) is a novel marker of inflammation and metabolism recently proposed in studies.12,13 UA can activate the natural immune response by acting as damage-associated molecular patterns and initiating innate immunity.14–16 Conversely, HDL is an active lipid in the immune response and has a protective effect on infections.17–19 As the ratio of UA to HDL, UHR may serve as a predictive marker for pneumonia risk in stroke patients. Previous studies reported that elevated UHR was associated with a reduced risk of osteoporosis.20 Patients with atrial fibrillation and non-alcoholic fatty liver disease exhibited higher UHR levels than healthy populations.21 UHR was associated with insulin resistance and metabolic disorders, particularly in patients with type 2 diabetes.22 However, few studies had evaluated the prognostic value of UHR for pneumonia after EVT. Thus, we conducted a multicenter study to investigate the hypothesis that UHR was associated with pneumonia risk in VBAO patients treated with EVT.
Methods
Data that supported the findings of this study are available from the corresponding authors upon reasonable request.
Study Population
From December 2015 to December 2018, we enrolled participants diagnosed with acute VBAO from the PERSIST study, which was a retrospective, multicenter study conducted at 21 stroke centers in 13 provinces of China (ChiCTR2000033211). Details of the PERSIST study have been described in previous studies.23–25 We included patients according to the following criteria: (1) ≥18 years; (2) diagnosed as acute symptomatic VBAO on computed tomographic angiography (CTA), magnetic resonance angiography (MRA), or digital subtracted angiography (DSA); and (3) treated with EVT within 24 hours of estimated occlusion time. The exclusion criteria were: (1) had pre-stroke mRS score >2; (2) had anterior circulation stroke; (3) had aneurysms or arteriovenous malformation; (4) had missing UA and HDL and imaging information; (5) had chronic inflammatory diseases or autoimmune diseases; (6) pregnancy or lactation. This study was approved by the Ethics Committee of The First Affiliated Hospital of USTC. Patient consent was waived due to the retrospective nature. This study was conducted in accordance with the ethical standards for patient confidentiality and the principles outlined in the 1964 Declaration of Helsinki.
Data Collection
Demographic data, medical history, laboratory results, and imaging information were retrospectively collected from the medical records. Stroke severity was assessed with the National Institute of Health Stroke Scale (NIHSS) score. Consciousness was assessed with the Glasgow Coma Scale (GCS). Stroke subtype was classified according to the Trial of Org 10172 in Acute Stroke Treatment (TOAST) criteria. All imaging files were independently reviewed by two neurologists who were blinded to this study. The occlusion site was classified as a basilar artery, vertebral artery, and vertebrobasilar artery occlusion. Cerebral ischemia was assessed with the posterior circulation-Alberta Stroke Program Early CT Score (PC-ASPECTS). Collateral status was assessed with the American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology (ASITN/SIR) score. Successful reperfusion status was defined as the modified Thrombolysis in Cerebral Infarction (mTICI) scale 2b or 3. The blood samples were collected on admission including routine blood and blood chemistry. UHR was calculated with the following equations: serum UA (mg/dL)/HDL (mg/dL).13
EVT
EVT was carried out using mechanical thrombectomy with stent retrievers or thromboaspiration, balloon angioplasty, intra-arterial thrombolysis, stenting, or a combination of these techniques. The selection of specific EVT techniques was determined by the neurointerventionists, guided by local protocols and the preferences of the patients or their legal representatives at each institution.
Primary Outcome
Pneumonia within 7 days after EVT was defined according to the criteria published by the Pneumonia in Stroke Consensus Group:26 (1) at least 1 of the following criteria: a. fever (>38°C) with no other recognized cause; b. leukopenia (<4000 white blood cell/mm3) or leukocytosis (>12000 white blood cell/mm3); c. for adults aged ≥70 years, altered mental status with no other recognized cause; (2) at least 2 of the following criteria: a. new onset of purulent sputum, or change in character of sputum over a 24 h period, or increased respiratory secretions, or increased suctioning requirements; b. new onset or worsening cough, or dyspnea, or tachypnea (respiratory rate > 25/min); c. rales, crackles, or bronchial breath sounds; d. worsening gas exchange. (3) and ≥2 serial chest radiographs with at least 1 of the following criteria: new or progressive and persistent infiltrate, or consolidation, or cavitation. Pneumonia was then classified as community-acquired pneumonia and hospital-acquired pneumonia.
Statistical Analysis
Categorical variables were presented as numbers (percentages), and continuous variables were presented as mean ± standard deviation or median (interquartile range, [IQR]) according to the normality in the Kolmogorov–Smirnov test. Categorical variables were compared with chi-square tests or Fisher’s exact tests and continuous variables were compared with t test or Mann–Whitney U-test as appropriate. Multiple imputation with chain equations was used to deal with missing values.
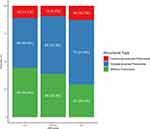
We categorized UHR into low (<9.97%), medium (9.97%–14.61%), and high levels (≥14.61%) by tertiles, and presented the distribution of pneumonia types across different UHR levels. We utilized the multivariable logistic regression models to evaluate the association between UHR and pneumonia after EVT in VBAO with adjustment for potential confounders. Model 1 was adjusted for age and gender. Model 2 was adjusted for age, gender, systolic blood pressure, diastolic blood pressure, hypertension, diabetes mellitus, coronary heart disease, hyperlipidemia, atrial fibrillation, smoking, and stroke types. Model 3 was adjusted for variables with P <0.10 in the univariable analysis using the backward selection method, as well as for variables previously identified as predictors of pneumonia in prior research.
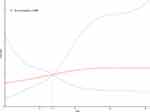
We used the receiver operating characteristic curve to evaluate the predictive ability of UHR for pneumonia after EVT of VBAO. We used the restricted cubic spline curve with 4 knots (5th, 35th, 65th, and 95th percentiles) to explore the dose–response relationship between UHR and pneumonia after EVT adjusted for variables included in model 3. In a sensitivity analysis, we validated the predictive value of UHR in hospital-acquired pneumonia after EVT. We performed subgroup analyses to verify the robustness of the association between UHR and pneumonia after EVT according to age, gender, hypertension, diabetes mellitus, and intravenous thrombolysis treatment subgroups.
All statistical analyses were performed using R software version 4.2.1. (R Foundation, Vienna, Austria). A two-sided P value <0.05 was considered to be statistically significant.
Results
In our study, a total of 378 patients (mean age, 63.3 ± 12.8 years; 73.3% male) were enrolled in the PERSIST study after excluding 182 patients with missing information and 17 with chronic inflammation diseases. The baseline characteristics of patients with or without pneumonia were shown in Table 1: 236 (62.4%) patients were diagnosed with pneumonia, 296 (78.3%) were diagnosed with basilar artery occlusion alone, 77 (20.4%) received intravenous thrombolysis treatment, and 333 (88.1%) had successful recanalization. The mean NIHSS score was 22.5 points, and the median UHR value was 11.8. Our results found that elevated inflammatory markers (white blood cell count, neutrophil-to-lymphocyte ratio, UHR, and reduced high-density lipoprotein cholesterol) were significantly associated with pneumonia. Additionally, factors reflecting stroke severity (NIHSS and GCS scores), larger infarcts (indicated by ASPECTS scores), intravenous thrombolysis, poor collateral circulation, and extended reperfusion times were also identified as significant predictors of pneumonia (all P < 0.05). Meanwhile, higher UHR values were significantly associated with increased inflammatory markers, larger infarcts, poorer consciousness, and a higher risk of pneumonia (all P < 0.05; Table S1), as well as hospital-acquired pneumonia (57.9% vs 44.4%; Figure 1).
 |
Table 1 Baseline Characteristics of Participants with or without Pneumonia After EVT for VBAO |
The results of the univariable logistic regression models aligned closely with the findings from the baseline characteristics analysis (Tables 1 and S2). The area under the curve (AUC) for UHR demonstrated a modest predictive ability for pneumonia risk, with a value of 0.59 (95% confidence interval [CI], 0.53–0.64; Figure S1). Multivariable logistical regression analyses found that increased UHR was associated with a higher pneumonia risk in model 1 (odds ratio [OR], 1.05; 95% CI, 1.01–1.10; P = 0.009; tertile 3 versus tertile 1: OR, 2.04; 95% CI, 1.20–3.51; P = 0.009), model 2 (OR, 1.06; 95% CI, 1.02–1.11; P = 0.004; tertile 3 versus tertile 1: OR, 2.38; 95% CI, 1.37–4.20; P = 0.002), and model 3 (OR, 1.05; 95% CI, 1.01–1.10; P = 0.020; tertile 3 versus tertile 1: OR, 2.09; 95% CI, 1.15–3.82; P = 0.016; Table 2). The dose–response relationship indicated that UHR was linearly associated with the risk of pneumonia (P = 0.888; Figure 2).
 |
Table 2 Association Between UHR and the Risk of Pneumonia After EVT for VBAO |
In sensitivity analyses, UHR was significantly associated with hospital-acquired pneumonia in model 1 (OR, 1.06; 95% CI, 1.02–1.10; P = 0.003; tertile 3 versus tertile 1: OR, 1.75; 95% CI, 1.05–2.93; P = 0.031), model 2 (OR, 1.07; 95% CI, 1.03–1.11; P = 0.001; tertile 3 versus tertile 1: OR, 1.99; 95% CI, 1.18–3.41; P = 0.011), and model 3 (OR, 1.06; 95% CI, 1.02–1.10; P = 0.008; tertile 3 versus tertile 1: OR, 1.74; 95% CI, 1.00–3.05; P = 0.051; Table S3). In addition, there was no significant interaction between UHR and pneumonia risk across different subgroups stratified by gender, hypertension, diabetes mellitus, and intravenous thrombolysis treatment (P > 0.05), except for the older age (P = 0.041; Figure 3).
Discussion
In this study, we found that about 62% of patients with VBAO developed pneumonia after EVT. The dose- response relationship curve suggested that a higher UHR was associated with an increased risk of pneumonia after EVT. The association of UHR and pneumonia risk remained significant in different subgroups and pneumonia types.
Pneumonia is a preventable complication associated with poor outcomes in patients with posterior circulation stroke. In our study, 62% of VBAO patients had pneumonia after EVT. In the Endovascular Treatment for Acute Basilar Artery Occlusion Study Registry, pneumonia occurred in approximately 70.7% of patients and was an independent predictor for early mortality.11 The Berlin Stroke Register found that pneumonia was associated with mortality beyond 7 days and suggested that prophylactic antibiotics in high-risk patients might reduce early mortality.9
Early dysphagia screening can improve the detection rate of pneumonia.27 VBAO patients were more likely to suffer from dysphagia compared to anterior circulation stroke.28 Instrumental assessments, like fiberoptic endoscopic evaluation of swallowing and videofluoroscopy, were considered the gold standard for diagnosing dysphagia.29 However, these tests required specialized staff and equipments. Previous studies suggested that the water swallow test may be a simpler method for identifying dysphagia in the hyperacute stroke.30
UHR is a novel biomarker for inflammation and metabolic diseases, easily calculated from routine clinical measures of UA and HDL. Previous studies suggested that UHR had been widely used in different diseases, such as poorly controlled hypertension, diabetes mellitus, and atrial fibrillation. In subgroup analyses, we found that UHR was significantly associated with pneumonia in patients with hypertension and atrial fibrillation. In a cross-sectional study, serum UHR was positively correlated with hypertension after adjusting for covariates, suggesting a link with hypertension through the pathophysiology of hypertension, including inflammation, oxidative damage, and endothelial dysfunction.12,31 UHR levels were reported to be higher in patients with atrial fibrillation and non-alcoholic fatty liver disease compared to the control group, and when combined with age, it could improve the predictive ability for atrial fibrillation.21 Another study found that UHR was positively associated with visceral fat in patients with type 2 diabetes and may reflect insulin resistance and metabolic disorders.22
Inflammatory markers have proven helpful in identifying high-risk patients, with previous studies confirming their predictive value for pneumonia after ischemic stroke. Hotter et al conducted a pooled analysis of 2 acute stroke studies and found that ultrasensitive copeptin and ultrasensitive procalcitonin were associated with functional outcomes at 3 months.32 In a retrospective analysis, the neutrophil-to-lymphocyte ratio was found to be associated with an increased risk of severe pneumonia, as assessed by the Pneumonia Severity Index.33 We found that a higher UHR was associated with an increased risk of pneumonia. Furthermore, when combined with recanalization status, neurological deterioration, and hemorrhagic transformation after EVT, UHR may provide a more robust prediction of outcomes and help identify VBAO patients who are more likely to benefit from more aggressive antibiotic therapy after EVT.34
The underlying mechanism regarding the association between UHR and pneumonia might be explained by the combined effects of elevated UA and decreased HDL levels. UA could decrease insulin-induced nitric oxide synthesis and activate the renin-angiotensin system of endothelial cells,35 resulting in enhancing the proliferation of smooth muscle cells by mediating inflammation,36 promoting the production of free radical species,37 and suppressing oxidative stress reactions.38 Meanwhile, UA at scale concentrations can help protect the endothelium against oxidative stress by acting as a selective free radical scavenger and functioning as an antioxidant.39 HDL can reverse cholesterol transport, which exhibits anti-oxidation and anti-inflammation properties and protects endothelial cells from atherosclerotic burdens.40,41 Hence, a high serum UA level and low HDL level may synergistically have detrimental effects on pneumonia after ischemic stroke.
To the best of our knowledge, this was the first study to investigate the association between UHR and pneumonia after EVT in VBAO patients. However, there were several limitations of this study. Firstly, this was a multi-center study conducted in China, introducing potential biases due to variations in the experiences and treatment strategies among the different centers. Secondly, due to the retrospective nature of this study, we were unable to collect preoperative information on systemic infections nor dynamically monitor changes in inflammatory indicators. This limitation may introduce confounding effects on pneumonia risk, as it hindered the ability to account for pre-existing infections as potential contributors and restricted the predictive ability of serial measurement of UHR. Third, we could not investigate other potentially confounding factors, such as calcium, and volume status, as they were not routinely assessed in patients treated with EVT. Fourth, although we used multiple imputation to handle missing data, the potential influence of missing values remained a significant source of bias. The sample size for subgroup analyses might have been insufficient to yield reliable results, and these findings should be interpreted with caution. Finally, the AUC for UHR in our study was relatively low, which might indicate a limited predictive capability.
Conclusion
In conclusion, our study revealed that approximately 62% of VBAO patients developed pneumonia following EVT. Elevated UHR levels were significantly associated with an increased risk of pneumonia after the procedure. Factors such as heightened inflammatory markers, larger infarcts, and reduced consciousness appeared to strongly correlate with UHR in influencing pneumonia risk. These findings highlight the potential utility of UHR as a biomarker for identifying high-risk VBAO patients, aiding in early screening and informing therapeutic interventions for pneumonia post-EVT. Further research is necessary to validate the prognostic role of UHR in outcomes of pneumonia after EVT in VBAO patients.
Acknowledgment
The authors would like to thank Dr Juan Du for the support in data collection and statistical analysis.
Funding
The study was supported by the National Natural Science Foundation of China (No. 82371312).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Tao C, Nogueira RG, Zhu Y, et al. Trial of endovascular treatment of acute basilar-artery occlusion. N Engl J Med. 2022;387(15):1361–1372. doi:10.1056/NEJMoa2206317
2. Jovin TG, Li C, Wu L, et al. Trial of thrombectomy 6 to 24 hours after stroke due to basilar-artery occlusion. N Engl J Med. 2022;387(15):1373–1384. doi:10.1056/NEJMoa2207576
3. Writing Group for the BG, Zi W, Qiu Z, Wu D, et al. Assessment of endovascular treatment for acute basilar artery occlusion via a nationwide prospective registry. JAMA Neurol. 2020;77(5):561–573. doi:10.1001/jamaneurol.2020.0156.
4. Alemseged F, Nguyen TN, Coutts SB, Cordonnier C, Schonewille WJ, Campbell BCV. Endovascular thrombectomy for basilar artery occlusion: translating research findings into clinical practice. Lancet Neurol. 2023;S1474-4422(22):00483–5.
5. Abdalkader M, Finitsis S, Li C, et al. Endovascular versus medical management of acute basilar artery occlusion: a systematic review and meta-analysis of the randomized controlled trials. J Stroke. 2023;25(1):81–91. doi:10.5853/jos.2022.03755
6. Sun Y, Jou E, Nguyen TN, et al. Predictors of futile recanalization after endovascular treatment in acute ischemic stroke: a multi-center study. Front Neurosci. 2023;17:1279366. doi:10.3389/fnins.2023.1279366
7. Katzan IL, Cebul RD, Husak SH, Dawson NV, Baker DW. The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology. 2003;60(4):620–625. doi:10.1212/01.WNL.0000046586.38284.60
8. Finlayson O, Kapral M, Hall R, Asllani E, Selchen D, Saposnik G, Canadian Stroke Network, Stroke Outcome Research Canada (SORCan) Working Group. Risk factors, inpatient care, and outcomes of pneumonia after ischemic stroke. Neurology. 2011;77(14):1338–1345. doi:10.1212/WNL.0b013e31823152b1
9. Koennecke H-C, Belz W, Berfelde D, et al. Factors influencing in-hospital mortality and morbidity in patients treated on a stroke unit. Neurology. 2011;77(10):965–972. doi:10.1212/WNL.0b013e31822dc795
10. Yuan M, Li Q, Zhang R, et al. Risk factors for and impact of poststroke pneumonia in patients with acute ischemic stroke. Medicine. 2021;100(12):e25213. doi:10.1097/MD.0000000000025213
11. Huang J, Wang M, Li F, et al. Clinical predictors for early mortality of patients with acute basilar artery occlusion. Cerebrovasc Dis Basel Switz. 2023;52(2):202–209. doi:10.1159/000526124
12. Aktas G, Khalid A, Kurtkulagi O, et al. Poorly controlled hypertension is associated with elevated serum uric acid to HDL-cholesterol ratio: a cross-sectional cohort study. Postgrad Med. 2022;134(3):297–302. doi:10.1080/00325481.2022.2039007
13. Yazdi F, Baghaei MH, Baniasad A, Naghibzadeh-Tahami A, Najafipour H, Gozashti MH. Investigating the relationship between serum uric acid to high-density lipoprotein ratio and metabolic syndrome. Endocrinol Diabetes Metab. 2022;5(1):e00311. doi:10.1002/edm2.311
14. Zhao J, Wei K, Jiang P, et al. Inflammatory response to regulated cell death in gout and its functional implications. Front Immunol. 2022;13:888306. doi:10.3389/fimmu.2022.888306
15. Zhu L, Lin X, Chen M. LncRNA NEAT1 correlates with Th17 cells and proinflammatory cytokines, also reflects stenosis degree and cholesterol level in coronary heart disease patients. J Clin Lab Anal. 2022;36(6):e23975. doi:10.1002/jcla.23975
16. Gasse P, Riteau N, Charron S, et al. Uric acid is a danger signal activating NALP3 inflammasome in lung injury inflammation and fibrosis. Am J Respir Crit Care Med. 2009;179(10):903–913. doi:10.1164/rccm.200808-1274OC
17. Murphy AJ, Chin-Dusting JPF, Sviridov D, Woollard KJ. The anti inflammatory effects of high density lipoproteins. Curr Med Chem. 2009;16(6):667–675. doi:10.2174/092986709787458425
18. Norata GD, Pirillo A, Ammirati E, Catapano AL. Emerging role of high density lipoproteins as a player in the immune system. Atherosclerosis. 2012;220(1):11–21. doi:10.1016/j.atherosclerosis.2011.06.045
19. Mostaza JM, Salinero-Fort MA, Cardenas-Valladolid J, et al. Pre-infection HDL-cholesterol levels and mortality among elderly patients infected with SARS-CoV-2. Atherosclerosis. 2022;341:13–19. doi:10.1016/j.atherosclerosis.2021.12.009
20. Liu Z, Tang Y, Sun Y, et al. Uric acid-to-high-density lipoprotein cholesterol ratio and osteoporosis: evidence from the national health and nutrition examination survey. J Orthop Surg Hong Kong. 2024;32(3):10225536241293489. doi:10.1177/10225536241293489
21. Liu G, Zhang Q, Zhou M, et al. Correlation between serum uric acid to high-density lipoprotein cholesterol ratio and atrial fibrillation in patients with NAFLD. PLoS One. 2024;19(6):e0305952. doi:10.1371/journal.pone.0305952
22. Sun H, Su H, Zheng R, Liu C, Wang Y, Fang C. Serum uric acid to high‑density lipoprotein cholesterol ratio is associated with visceral fat in patients with type 2 diabetes. Diabetes, Metab Syndr Obes Targets Ther. 2023;16:959–967. doi:10.2147/DMSO.S403895
23. Xiao L, Gu M, Lu Y, et al. Influence of renal impairment on clinical outcomes after endovascular recanalization in vertebrobasilar artery occlusions. J Neurointerv Surg. 2022;14(11):1077–1083. doi:10.1136/neurintsurg-2021-018003
24. Wang J, Zhu S, Xu P, et al. Initial symptoms of vertebrobasilar artery occlusions and the outcomes after endovascular treatment. J Neurol. 2022;269(10):5561–5570. doi:10.1007/s00415-022-11218-4
25. Sun W, Duan Z, Xu P, et al. The safety and effectiveness of endovascular treatment for patients with vertebrobasilar artery occlusions: according to the BEST and BASICS criteria. Ther Adv Neurol Disord. 2022;15:17562864221114627. doi:10.1177/17562864221114627
26. Smith CJ, Kishore AK, Vail A, et al. Diagnosis of stroke-associated pneumonia: recommendations from the pneumonia in stroke consensus group. Stroke. 2015;46(8):2335–2340. doi:10.1161/STROKEAHA.115.009617
27. Liang J, Yin Z, Li Z, et al. Predictors of dysphagia screening and pneumonia among patients with acute ischaemic stroke in China: findings from the Chinese stroke center alliance (CSCA). Stroke Vasc Neurol. 2022;7(4):294–301. doi:10.1136/svn-2020-000746
28. Westendorp WF, Dames C, Nederkoorn PJ, Immunodepression MA. Infections, and functional outcome in ischemic stroke. Stroke. 2022;53(5):1438–1448. doi:10.1161/STROKEAHA.122.038867
29. Cohen DL, Roffe C, Beavan J, et al. Post-stroke dysphagia: a review and design considerations for future trials. Int J Stroke off J Int Stroke Soc. 2016;11(4):399–411. doi:10.1177/1747493016639057
30. Daniels SK, Anderson JA, Willson PC. Valid items for screening dysphagia risk in patients with stroke: a systematic review. Stroke. 2012;43(3):892–897. doi:10.1161/STROKEAHA.111.640946
31. Han X, Tan X, Liu M, et al. Association between serum uric acid/high-density lipoprotein cholesterol ratio and hypertension among reproductive-aged women. J Health Popul Nutr. 2023;42(1):123. doi:10.1186/s41043-023-00458-3
32. Hotter B, Hoffmann S, Ulm L, et al. Inflammatory and stress markers predicting pneumonia, outcome, and etiology in patients with stroke: biomarkers for predicting pneumonia, functional outcome, and death after stroke. Neurol Neuroimmunol Neuroinflammation. 2020;7(3):e692. doi:10.1212/NXI.0000000000000692
33. Nam K-W, Kim TJ, Lee JS, et al. High neutrophil-to-lymphocyte ratio predicts stroke-associated pneumonia. Stroke. 2018;49(8):1886–1892. doi:10.1161/STROKEAHA.118.021228
34. Chen Y, Zhou S, Yang S, et al. Developing and predicting of early mortality after endovascular thrombectomy in patients with acute ischemic stroke. Front Neurosci. 2022;16:1034472. doi:10.3389/fnins.2022.1034472
35. Yu M-A, Sánchez-Lozada LG, Johnson RJ, Kang D-H. Oxidative stress with an activation of the renin-angiotensin system in human vascular endothelial cells as a novel mechanism of uric acid-induced endothelial dysfunction. J Hypertens. 2010;28(6):1234–1242. doi:10.1097/HJH.0b013e328337da1d
36. Kang D-H, Park S-K, Lee I-K, Johnson RJ. Uric acid-induced C-reactive protein expression: implication on cell proliferation and nitric oxide production of human vascular cells. J Am Soc Nephrol JASN. 2005;16(12):3553–3562. doi:10.1681/ASN.2005050572
37. Sautin YY, Nakagawa T, Zharikov S, Johnson RJ. Adverse effects of the classic antioxidant uric acid in adipocytes: NADPH oxidase-mediated oxidative/nitrosative stress. Am J Physiol Cell Physiol. 2007;293(2):C584–596. doi:10.1152/ajpcell.00600.2006
38. Zhi L, Yuzhang Z, Tianliang H, Hisatome I, Yamamoto T, Jidong C. High uric acid induces insulin resistance in cardiomyocytes in vitro and in vivo. PLoS One. 2016;11(2):e0147737. doi:10.1371/journal.pone.0147737
39. Stinefelt B, Leonard SS, Blemings KP, Shi X, Klandorf H. Free radical scavenging, DNA protection, and inhibition of lipid peroxidation mediated by uric acid. Ann Clin Lab Sci. 2005;35(1):37–45.
40. Navab M, Yu R, Gharavi N, et al. High-density lipoprotein: antioxidant and anti-inflammatory properties. Curr Atheroscler Rep. 2007;9(3):244–248. doi:10.1007/s11883-007-0026-3
41. Tran-Dinh A, Diallo D, Delbosc S, et al. HDL and endothelial protection. Br J Pharmacol. 2013;169(3):493–511. doi:10.1111/bph.12174
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
The Influence of Influenza Virus Infections in Patients with Chronic Obstructive Pulmonary Disease
Liao KM, Chen YJ, Shen CW, Ou SK, Chen CY
International Journal of Chronic Obstructive Pulmonary Disease 2022, 17:2253-2261
Published Date: 14 September 2022
Association Between Inflammatory Burden Index and Unfavorable Prognosis After Endovascular Thrombectomy in Acute Ischemic Stroke
Du M, Xu L, Zhang X, Huang X, Cao H, Qiu F, Lan W, Jiang H
Journal of Inflammation Research 2023, 16:3009-3017
Published Date: 19 July 2023