Back to Journals » Journal of Inflammation Research » Volume 18
Association Between Uric Acid to High-Density Lipoprotein Cholesterol Ratio and Abdominal Aortic Aneurysm: A Single-Center Retrospective Study
Received 24 November 2024
Accepted for publication 22 February 2025
Published 5 March 2025 Volume 2025:18 Pages 3217—3226
DOI https://doi.org/10.2147/JIR.S508355
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Da Lu,1,* Ke Si,2,* Guijun Huo3
1Department of Thoracic-Cardiac Surgery, Hubei Provincial Hospital of Traditional Chinese Medicine, Affiliated Hospital of Hubei University of Chinese Medicine, Wuhan, People’s Republic of China; 2Department of Cardiovascular Surgery, The First Affiliated Hospital of Soochow University, Suzhou, People’s Republic of China; 3The Affiliated Suzhou Hospital of Nanjing Medical University, Suzhou Municipal Hospital, Suzhou, Jiangsu, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Guijun Huo, The Affiliated Suzhou Hospital of Nanjing Medical University, Suzhou Municipal Hospital, No. 26 Daoqian Street, Suzhou, Jiangsu, People’s Republic of China, Email [email protected]
Objective: Uric acid (UA) to high-density lipoprotein cholesterol (HDL-C) ratio (UHR) has been recognized as a novel biomarker for evaluating inflammatory and anti-inflammatory interaction. However, it is not known whether UHR is related to abdominal aortic aneurysm (AAA). The current research aims to explore the potential role of UHR in predicting AAA.
Methods: In this study, 303 AAA patients and 408 normal subjects were retrospectively analyzed. The relationship between UHR and AAA was evaluated using Logistic regression models. Receiver operating characteristic (ROC) curves and restricted cubic spline (RCS) analysis were employed to elucidate the detailed association between UHR and AAA.
Results: UHR value in the AAA group was significantly higher than that in the normal group, and UHA was an independent risk factor for AAA. After adjusting for covariates, each 1-unit increase in UHR was associated with a 12% rise in AAA risk (OR: 1.12, 95% CI: 1.03, 1.21). ROC value of UHR was 0.847 (95% CI, 0.811~0.887, P < 0.05), and the optimal critical value of UHR was 17.2%. The incidence of AAA in the UHR≥ 17.2% group was significantly higher than that in the UHR < 17.2% group. RCS curves revealed a significant nonlinear relationship between UHR and AAA events (p-value < 0.001, p-nonlinear = 0.002).
Conclusion: This study demonstrates that UHR levels are significantly linked to increased AAA risk, which can be widely used as an indicator for dynamic screening of AAA.
Keywords: abdominal aortic aneurysms, UA, HDL-C, lipids, UHR
Introduction
Abdominal aortic aneurysm (AAA) is defined as localized dilatation of the abdominal aorta ≥50% of normal artery diameter, AAA rupture is an important cause of death in adults.1,2 The treatment of AAA includes surgical treatment and medical treatment, and surgical treatment requires a comprehensive evaluation of the patient’s condition.3 In 2019, the global prevalence of AAA among individuals aged 30 to 79 years was 0.92%, which represents approximately 35.12 million cases.4 Reports from population-based screening studies indicate a significantly higher prevalence of AAA in men compared to women, with rates ranging from 1.9% to 18.5% in men and from 0.1% to 4.2% in women.5 AAA are often challenging for patients and medical personnel to detect. A comprehensive meta-analysis of 24 retrospective cohort studies has reported that the fatality rate following a rupture of an AAA is as high as 81%, with approximately one-third of those individuals dying before reaching the hospital.6 Therefore, early identification of high-risk groups for AAA is crucial.
Studies have shown that chronic inflammation of the vascular wall, abnormal proliferation and apoptosis of smooth muscle cells, increased expression of matrix metalloproteinases, and degradation of extracellular matrix all promote the course of AAA.7–9 These pathological processes interact to accelerate the development of AAA.10 The results of epidemiological and genetic studies show that the increase in serum uric acid level is closely related to atherosclerotic cardiovascular disease.11,12 Hyperuricemia is associated with inflammatory response and oxidative stress and leads to endothelial dysfunction. High uric acid can lead to the occurrence and development of AAA by promoting an inflammatory response. High-density lipoprotein-cholesterol can reduce atherosclerosis through anti-inflammatory and antioxidant effects and reverse cholesterol transport, and HDL-C level is negatively correlated with the occurrence and development of AAA.13 Recently, uric acid to high-density lipoprotein cholesterol ratio (UHR) has been recognized as a novel biomarker for evaluating inflammatory and anti-inflammatory interactions.14 Recent studies have demonstrated a nonlinear relationship between UHR and brachial-ankle PWV.15 Furthermore, research indicates that an increase in UHR is linked to a heightened risk of major adverse vascular events in patients with chronic total coronary occlusion.16 Additionally, UHR has been shown to be a valuable predictor of the recurrence of atrial fibrillation.17 However, as a novel biomarker reflecting the interaction between inflammation and anti-inflammatory, there are few studies on whether UHR is related to AAA.
To address this knowledge gaps, in this study, we intend to examine whether there is an association between AAA patients and the UHR, and our results may provide ideas for improving AAA risk stratification and clinical decision-making.
Materials and Methods
Study Design
This retrospective study complied with the Helsinki Declaration and was approved by The Affiliated Suzhou Hospital of Nanjing Medical University Ethical Committee (KL901463). Human participants’ names have been removed from all sections of the manuscript. The Affiliated Suzhou Hospital of Nanjing Medical University Ethical Committee waived the need for informed consent. This study was conducted in accordance with the guidelines of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE).18 We confirm that all methods were performed according to the relevant guidelines and regulations. The clinical data of patients hospitalized in the Vascular Surgery Center of Suzhou Hospital of Nanjing Medical University from January 2010 to January 2024 were analyzed retrospectively. The following clinical data were obtained: gender, age, diabetes mellitus (DM), body mass index (BMI), smoke, hypertension, statins, antiplatelet, metformin, uric acid (UA), low-density lipoprotein cholesterol (LDL-C), high density lipoprotein cholesterol (HDL-C), total cholesterol (TC), triglycerides (TG), fasting blood glucose (FBG), uric acid to high-density lipoprotein cholesterol ratio (UHR). The criteria for diagnosing an abdominal aortic aneurysm are as follows: (1) The diameter of the aorta is greater than 30 mm. (2) The aneurysm is located within the abdominal aorta.19 The inclusion criteria for this study included the following: (1) The patient was hospitalized in the vascular surgery center. (2) All patients underwent complete aortic CTA examination with high-quality images. The exclusion criteria for this study included the following: (1) Patients with active inflammation and hematologic diseases. (2) Traumatic aortic aneurysm, syphilitic aortic aneurysm, pseudo aortic aneurysm, aortic dissection. (3) Patients with autoimmune diseases, connective tissue diseases, rheumatic immune diseases, or malignant tumors. (4) Patients with incomplete baseline or laboratory data. (5) Long-term use of corticosteroid drugs was excluded. After strict inclusion and exclusion criteria, the data of 303 patients diagnosed as AAA and 408 normal adults were analyzed retrospectively.
Statistical Analysis
Descriptive statistics are presented as median (interquartile range) or mean ± standard deviation for continuous variables and as frequency (percentage) for categorical variables. For quantitative variables that follow a normal distribution, we used analysis of variance (ANOVA) to assess group differences. When the quantitative variables do not adhere to a normal distribution, the Kruskal–Wallis test is employed to evaluate differences among groups. Categorical variables were analyzed using the Chi-square test.
Logistic proportional hazards regression models were utilized, which calculated odds ratio (ORs) along with 95% confidence intervals (95% CIs). Three models with varying levels of covariate adjustment were developed. Model 1 had no adjustments, Model 2 adjusted for gender and age, and Model 3 further adjusted for BMI, hypertension, statins, smoke, diabetes, antiplatelet, TC, TG, FBG, and LDL-C. Furthermore, a fully adjusted restricted cubic splines (RCS) analysis was performed to investigate the dose-response relationship between UHR and the risk of AAA.
The “pROC” package is used to draw the receiver operating characteristic (ROC) curve to evaluate the predictive value of UHR for the incidence of AAA. The optimal cut-off point on the ROC curve is selected by the Youden index. The dose-response relationship between UHR and AAA risk was evaluated using restricted cubic splines (RCS) with four knots (“rms” package). Subgroup analyses were carried out to determine whether the relationship between UHR and AAA risk was consistent across various demographic and clinical categories, such as gender, age, BMI, hypertension, diabetes, statins, smoke, and antiplatelet. Interaction analyses were also conducted to examine potential modifications of AAA risk across these subgroups. To ensure the stability of the study findings, we implemented a sensitivity analyses. E-values were calculated based on Model 3 to assess the minimum strength of the link between unmeasured confounders and UHR, which could explain the observed relationship with AAA risk. All statistical analyses were executed employing Stata 17.0 and R version 4.2.2, with P-values < 0.05 deemed statistically significant.
Results
Population Characteristics
All patients’ demographic characteristics are summarized in Table 1. Compared with the normal group, the AAA group was more male, relatively older, and had more smoking and hypertension patients.
 |
Table 1 Comparison of Baseline Characteristics Between AAA Group and Normal Group |
UHR Is an Independent Predictor of AAA
To investigate whether UHR was useful as a predictor of AAA, Logistic regression analyses for the factors related to AAA were conducted in 711 subjects. The Logistic proportional hazard models confirmed a significant relationship between UHR and the risk of AAA. In Model 1, each 1-unit increase in UHR was linked to a 20% rise in AAA risk (OR: 1.20, 95% CI: 1.15, 1.24). Model 2 indicated that for each additional unit of UHR, there was a 19% increase in AAA risk (OR: 1.19, 95% CI: 1.14, 1.23). Model 3 illustrated a 12% increase in AAA risk for every 1-unit rise in UHR (OR: 1.12, 95% CI: 1.03, 1.21) (Table 2).
 |
Table 2 Multivariable Logistic Regression Analysis of the Relationship Between UHR and AAA |
ROC Curve and RCS Regression Analysis
Establishing the ROC curve is integral for evaluating the sensitivity and specificity of AAA as a diagnostic tool. The Youden index selects the optimal cut-off point on the ROC curve. The ROC analysis determined that the predictive cut-off value of the UHR was 17.2%, and the area under the curve was 0.847 (95% CI, 0.811~0.887, P < 0.05) (Figure 1). The sensitivity and specificity of AAA were 0.776 and 0. 934 respectively. All 711 patients were divided into UHR<17.2% group and UHR≥17.2% group with the optimal cut-off value of UHR as the dividing line (Table 3), and the incidence of AAA was significantly different between the two groups (Figure 2). Adjusted RCS curves revealed a significant nonlinear relationship between UHR and AAA events (p-value < 0.001, p-nonlinear = 0.002) (Figure 3).
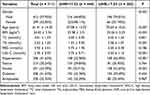 |
Table 3 Baseline Characteristics Based on UHR Group |
 |
Figure 1 The receiving operating characteristic curve for UHR in predicting AAA. Abbreviations: AAA, abdominal aortic aneurysm; UHR, uric acid to high-density lipoprotein cholesterol ratio. |
Subgroup Analysis and Interaction Analysis
We also conducted various subgroup analyses to assess whether UHR is consistent in different demographic characteristics. The results revealed that elevated UHR levels were consistent across different subgroups, including age < 65 years, BMI < 24, non-hypertension, and diabetes. To elucidate the potential interactions between these subgroups and the risk of AAA, we also conducted interaction analyses concurrently. Interaction analysis showed that UHR did not interact with these factors, which collectively affected AAA (Figure 4).
Sensitivity Analysis
To assess the stability of the outcomes, we conducted a sensitivity analyses. The E-value for UHR was calculated based on Model 3, revealing a value of 1.483, indicating that only a relatively large unmeasured confounding factor could explain the observed association.
Discussion
This is the largest sample size study so far on the correlation between UHR and AAA. In our study, we found that the increase in UHR was significantly correlated with the incidence of AAA. After adjusting other covariables, the relationship still existed, suggesting that UHR is an independent risk factor for the occurrence of AAA. The ROC analysis determined that the predictive cut-off value of the UHR AAA was 17.2%, and the area under the curve was 0.847; the AAA calculation rate of the UHR ≥ 17.2% group was significantly higher than that of the UHR < 17.2% group. These findings underscore the usefulness of this simple and easily calculated measure for early identification of patients with AAA. The dose-response analysis found that this association between UHR and AAA was nonlinear.
Uric acid is the final product of purine catabolism, which is excreted by the kidney with urine and intestine. Hyperuricemia is related to DNA damage, oxidation, inflammatory cytokine production, and even apoptosis.20,21 The Second Manifestations of Arterial Disease (SMART) study was a case-cohort study of 431 patients. During the follow-up period, 220 patients developed new vascular events, including AAA. The study showed that increased plasma uric acid levels increased the incidence of AAA.22 Previous studies have shown that the uric acid level in the aortic aneurysm wall is significantly higher than in the normal aortic wall.23 The relationship between serum uric acid levels and atherosclerosis has been studied for decades, and studies have shown that high uric acid levels promote the occurrence and development of atherosclerosis and, thus, the formation of aneurysms.24,25 Uric acid can aggravate the occurrence and development of atherosclerosis through ERK/p38 mitogen-activated protein kinase (MAPK) cascade, AMP-activated protein kinase (AMPK), Phosphatidylinositol-3 kinase (PI3K)-Akt Pathway, Inflammasome, and other signal pathways.26 Inflammation plays a vital role in the occurrence and development of AAA. It has been found that a large number of inflammatory cells infiltrate before the formation of AAA, and uric acid promotes the occurrence and development of aortic disease.27 Oxidative stress is considered the beginning of vascular injury, and people in the patients with the AAA group detected a large number of reactive oxygen species (ROS).28 It was reported that KLF11 expression was decreased in endothelial cells from human aneurysms, and it was time-dependently decreased in the aneurysmal endothelium from both elastase- and Pcsk9/AngII-induced AAA mouse models. The deficiency of KLF11 in endothelial cells significantly increased AAA formation, while selective overexpression of KLF11 in endothelial cells significantly inhibited AAA formation.29 In summary, it is currently believed that uric acid can cause vascular injury through inflammatory response, oxidative stress, reduced availability of nitric oxide, endothelial dysfunction, vasoconstriction and proliferation of vascular smooth muscle cells, insulin resistance, and metabolic disorders, and then cause vascular dilation, leading to the formation of AAA.30–32
High-density lipoprotein cholesterol (HDL-C) is synthesized primarily in the liver and is an anti-atherosclerotic lipoprotein that transports cholesterol from extrahepatic tissues to the liver for metabolism and excretion by bile. In a nationwide Danish registry, it was found that AAA patients (n=6560) had lower average HDL-C concentrations than those with aortic and iliac artery occlusive disease (n=23,496).33 An AAA is usually characterized by cholesterol accumulation and macrophage infiltration in the aortic wall. The ability of HDL-C to promote cholesterol excretion from macrophages is considered the primary vascular protection function of HDL-C, while the removal of cholesterol from macrophages by AAA patients under the promotion of HDL-C is damaged, which may be related to the AAA mechanism.34 Through the analysis of plasma and tissues of AAA patients, it was found that the anti-HDL level of IgG in AAA patients increased, which indicated that there was a potential immune response against HDL-C in AAA and supported the new role of anti-HDL antibody in AAA.35 The decrease of HDL-C, its anti-inflammatory, anti-oxidation, and anti-atherosclerosis effects are weakened, which can also lead to AAA.36,37 It has been reported that the level of HDL-C is negatively correlated with the diameter of AAA, and targeted therapy for HDL-C can prevent the formation of AAA.38
In this study, we found that with each 1-unit increase in UHR, the risk of AAA incidence rises by 12%; this significant correlation remained even after adjusting for all potential covariates. More importantly, our study further revealed a significant nonlinear relationship between UHR and AAA events. This clearly demonstrates the critical need to monitor UHR levels to assess AAA risk accurately. The ROC analysis determined that the predictive cut-off value of the UHR AAA was 17.2%, and the area under the curve was 0.847. These findings underscore the usefulness of this simple and easily calculated measure for early identification of patients with AAA. It is worth noting that significant positive associations exist among individuals with age < 65 years, BMI < 24, non-hypertension, and diabetes. These findings emphasize the need for clinicians to focus on these specific subgroups and individuals. Interaction analysis showed that UHR did not interact with these factors in collectively affecting AAA. This suggests the generalizability of our study findings to a broad population.
UHR is considered an index of metabolic imbalance and evaluates the interaction between inflammation and anti-inflammation. Although the exact mechanism of the interaction between UHR and AAA is not fully understood, it can be explained as follows. First, the UHR index is reliable for evaluating the interaction between inflammation and anti-inflammation. Previous evidence shows that inflammation plays a vital role in the occurrence and development of AAA.27,39 Secondly, UHR is usually related to metabolism, and the abnormality of the UHR index well reflects the metabolic disorder in the body. Many studies have shown that metabolic disorders will promote the occurrence and development of AAA.40–42 In addition, a higher UHR index is independently related to atherosclerosis, microvascular injury, and the occurrence and development of various cardiovascular diseases, which are high-risk factors for AAA patients.15,43–45 Therefore, it seems reasonable to suggest that patients with higher UHR levels are more likely to be experiencing vascular injury, so the incidence of AAA increases. In clinical practice, our findings can guide clinicians to control UHR within a target range, which is beneficial to prevent AAA.
This study clarifies the role of the UHR in predicting AAA, offering a comprehensive approach to clinical decision-making that aligns with existing evidence. The global incidence of AAA patients is on the rise, making it crucial to identify high-risk individuals promptly. In clinical practice, evaluating a patient’s UHR index can enhance disease assessment and facilitate the development of more effective, personalized treatment and management strategies. Furthermore, understanding the relationship between UHR and AAA can assist healthcare professionals in better assessing patient risks and in timely identification and management of potential complications.
However, this study also has many limitations. Firstly, this study is a retrospective study, which requires more prospective studies. Secondly, despite the use of multivariate adjustment, confounding factors may still bias the results, but the calculated E value indicates the robustness of the results, and the absence of confounding factors is improbable to alter the conclusions of this investigation. Thirdly, the population in this study may have a higher prevalence of abdominal aortic aneurysms (AAA) compared to the general population. As a result, the findings may not be entirely applicable to the broader population. Further research involving larger and more diverse samples is needed to verify these results. Lastly, the correlation between UHR and AAA diameter has yet to be explored. In the future, prospective studies will be designed to reduce selection bias and study the correlation between UHR and AAA diameter, and further animal experiments will be carried out to reveal the correlation mechanism between UHR and AAA.
Conclusion
In summary, UHR shows potential as an independent predictor of the incidence of AAA, and our study identified possible cut-off values for UHR in predicting AAA. Although further validation in a larger population is essential, the detection of UHR proves to be valuable for the early identification and risk stratification of individuals at high risk for AAA.
Patient Data Confidentiality Statement
This study follows strict data confidentiality and privacy protection protocols, with the following measures:
- All study data has been anonymized and does not contain any personal information that could identify patients (eg, names, identification numbers, contact details, etc.).
- The data is stored on secure servers, with access restricted to the research team members, all of whom have signed confidentiality agreements.
- The use of the data is limited to the purposes of this study and will not be shared with third parties or used for other purposes.
- During the publication of study results, all reported data will be in aggregated statistical form, ensuring that patient privacy is fully protected.
This study has been approved by the Ethics Committee of Suzhou Hospital Affiliated to Nanjing Medical University (Ethics Approval Number: KL901463), which has granted a waiver of patient informed consent. The reasons for the waiver are as follows:
- This is a retrospective study that primarily utilizes historical data from the hospital’s electronic health records (EHR) system. No additional interventions or treatments were administered to the patients, and the research poses minimal risk to them.
- The data used in the study has been de-identified to ensure that no personally identifiable information of the patients will be disclosed or compromised.
- The data collection and analysis strictly adhere to the Declaration of Helsinki and other relevant ethical guidelines to protect patient privacy and data security.
Data Sharing Statement
All data related to this study can be obtained upon reasonable request from the correspondent.
Ethics Approval and Consent to Participate
This paper did not involve the direct use of any human tissue. This study was conducted by the Declaration of Helsinki and was approved by the Ethics Committee of The Affiliated Suzhou Hospital of Nanjing Medical University. Written consent was obtained from all participants in the study.
Funding
This work was supported by the Suzhou “Science and Education Revitalize Health” Youth Science and Technology Project (KJXW2021031).
Disclosure
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
References
1. Chaikof EL, Dalman RL, Eskandari MK, et al. The society for vascular surgery practice guidelines on the care of patients with an abdominal aortic aneurysm[J]. J Vasc Surg. 2018;67(1):2–77.e72. doi:10.1016/j.jvs.2017.10.044
2. Golledge J. Golledge JAbdominal aortic aneurysm: update on pathogenesis and medical treatments[J]. Nat Rev Cardiol. 2019;16(4):225–242. doi:10.1038/s41569-018-0114-9
3. Quaye KB, Pack N, Wilson-Byrne T, et al. Contemporary management of abdominal aortic aneurysms[J]. Curr Cardiol Rep. 2022;24(4):431–438. doi:10.1007/s11886-022-01662-z
4. Song P, He Y, Adeloye D, et al. The global and regional prevalence of abdominal aortic aneurysms: a systematic review and modeling analysis[J. Ann Surg. 2023;277(6):912–919. doi:10.1097/SLA.0000000000005716
5. Al-Balah A, Goodall R, Salciccioli JD, et al. Mortality from abdominal aortic aneurysm: trends in European Union 15+ countries from 1990 to 2017[J]. Br J Surg. 2020;107(11):1459–1467. doi:10.1002/bjs.11635
6. Reimerink JJ, van der Laan MJ, Koelemay MJ, et al. Systematic review and meta-analysis of population-based mortality from ruptured abdominal aortic aneurysm[J]. Br J Surg. 2013;100(11):1405–1413. doi:10.1002/bjs.9235
7. Toczek J, Meadows JL, Sadeghi MM. Novel molecular imaging approaches to abdominal aortic aneurysm risk stratification. Circ Cardiovasc Imaging. 2016;9(1):e003023. doi:10.1161/CIRCIMAGING.115.003023
8. Hellenthal FA, Buurman WA, Wodzig WK, et al. Biomarkers of abdominal aortic aneurysm progression. Part 2: inflammation[J]. Nat Rev Cardiol. 2009;6(8):543–552. doi:10.1038/nrcardio.2009.102
9. Weng H, Li H, Zhang Z, et al. Association between uric acid and risk of venous thromboembolism in East Asian populations: a cohort and Mendelian randomization study[J]. Lancet Reg Health West Pac. 2023;39(100848):1.
10. Qin Y, Wang Y, Liu O, et al. Tauroursodeoxycholic acid attenuates angiotensin ii induced abdominal aortic aneurysm formation in apolipoprotein E-deficient mice by inhibiting endoplasmic reticulum stress[J]. Eur J Vasc Endovasc Surg. 2017;53(3):337–345. doi:10.1016/j.ejvs.2016.10.026
11. Gill D, Cameron AC, Burgess S, et al. Urate, blood pressure, and cardiovascular disease: evidence from Mendelian randomization and meta-analysis of clinical trials[J]. Hypertension. 2021;77(2):383–392. doi:10.1161/HYPERTENSIONAHA.120.16547
12. Cho C, Kim B, Kim DS, et al. Large-scale cross-ancestry genome-wide meta-analysis of serum urate[J]. Nat Commun. 2024;15(1):3441. doi:10.1038/s41467-024-47805-4
13. Takagi H, Manabe H, Umemoto TA. meta-analysis of association between serum lipoproteins and abdominal aortic aneurysm[J]. Am J Cardiol. 2010;106(5):753–754. doi:10.1016/j.amjcard.2010.06.021
14. Liu P, Li J, Yang L, et al. Association between cumulative uric acid to high-density lipoprotein cholesterol ratio and the incidence and progression of chronic kidney disease[J]. Front Endocrinol. 2023;14. doi:10.3389/fendo.2023.1269580
15. Wang H, Ba Y, Gao X, et al. Association between serum uric acid to high density lipoprotein-cholesterol ratio and arterial stiffness in a Japanese population[J]. Medicine. 2023;102(31):e34182. doi:10.1097/MD.0000000000034182
16. Yang Y, Zhang J, Jia L, et al. Uric acid to high-density lipoprotein cholesterol ratio predicts adverse cardiovascular events in patients with coronary chronic total occlusion[J]. Nutr Metab Cardiovasc Dis. 2023;33(12):2471–2478. doi:10.1016/j.numecd.2023.07.037
17. Dervis E, Ozkan E, Yakut I, et al. The uric acid-to-high-density lipoprotein cholesterol ratio: a new biomarker for predicting arrhythmia recurrence after atrial fibrillation ablation. J Clin Med. 2024;13(24):7854. doi:10.3390/jcm13247854
18. von Elm E, Altman DG, Egger M, et al. The Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies[J]. Lancet. 2007;370(9596):1453–1457. doi:10.1016/S0140-6736(07)61602-X
19. Wanhainen A, Van Herzeele I, Bastos Goncalves F, et al. European society for vascular surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms[J]. Eur J Vasc Endovasc Surg. 2024;67(2):192–331. doi:10.1016/j.ejvs.2023.11.002
20. Gherghina ME, Peride I, Tiglis M, et al. Uric acid and oxidative stress-relationship with cardiovascular, metabolic, and renal impairment[J]. Int J Mol Sci. 2022;23(6):3188. doi:10.3390/ijms23063188
21. Sun HL, Wu YW, Bian HG, et al. Function of uric acid transporters and their inhibitors in hyperuricaemia[J]. Front Pharmacol. 2021;12. doi:10.3389/fphar.2021.667753
22. Hjortnaes J, Algra A, Olijhoek J, et al. Serum uric acid levels and risk for vascular diseases in patients with metabolic syndrome[J]. J Rheumatol. 2007;34(9):1882–1887.
23. Patetsios P, Rodino W, Wisselink W, et al. Identification of uric acid in aortic aneurysms and atherosclerotic artery[J]. Ann N Y Acad Sci. 1996;800:243–245. doi:10.1111/j.1749-6632.1996.tb33318.x
24. Kimura Y, Yanagida T, Onda A, et al. Soluble uric acid promotes atherosclerosis via AMPK (AMP-activated protein kinase)-mediated inflammation[J]. Arterioscler Thromb Vasc Biol. 2020;40(3):570–582. doi:10.1161/ATVBAHA.119.313224
25. Kubota Y, McAdams-DeMarco M, Folsom AR. Serum uric acid, gout, and venous thromboembolism: the atherosclerosis risk in communities study[J]. Thromb Res. 2016;144:144–148. doi:10.1016/j.thromres.2016.06.020
26. Kimura Y, Tsukui D, Kono H. Uric acid in inflammation and the pathogenesis of atherosclerosis[J]. Int J Mol Sci. 2021;22(22):12394. doi:10.3390/ijms222212394
27. Yuan Z, Lu Y, Wei J, et al. Abdominal aortic aneurysm: roles of inflammatory cells. Front Immunol. 2020;11:609161. doi:10.3389/fimmu.2020.609161
28. Quintana RA, Taylor WR. Cellular mechanisms of aortic aneurysm formation[J]. Circ Res. 2019;124(4):607–618. doi:10.1161/CIRCRESAHA.118.313187
29. Zhao G, Chang Z, Zhao Y, et al. KLF11 protects against abdominal aortic aneurysm through inhibition of endothelial cell dysfunction[J]. JCI Insight. 2021;6(5). doi:10.1172/jci.insight.141673.
30. Sharaf El Din UAA, Salem MM, Abdulazim DO. Uric acid in the pathogenesis of metabolic, renal, and cardiovascular diseases: a review. J Adv Res. 2017;8(5):537–548.
31. Ndrepepa G. Uric acid and cardiovascular disease[J]. Clin Chim Acta. 2018;484:150–163.
32. Kawai T, Ohishi M, Takeya Y, et al. Serum uric acid is an independent risk factor for cardiovascular disease and mortality in hypertensive patients[J]. Hypertens Res. 2012;35(11):1087–1092. doi:10.1038/hr.2012.99
33. Burillo E, Lindholt JS, Molina-Sánchez P, et al. ApoA-I/HDL-C levels are inversely associated with abdominal aortic aneurysm progression[J]. Thromb Haemost. 2015;113(6):1335–1346. doi:10.1160/TH14-10-0874
34. Martínez-López D, Cedó L, Metso J, et al. Impaired HDL (high-density lipoprotein)-mediated macrophage cholesterol efflux in patients with abdominal aortic aneurysm-brief report[J]. Arterioscler Thromb Vasc Biol. 2018;38(11):2750–2754. doi:10.1161/ATVBAHA.118.311704
35. Rodríguez-Carrio J, Lindholt JS, Canyelles M, et al. IgG Anti-high density lipoprotein antibodies are elevated in abdominal aortic aneurysm and associated with lipid profile and clinical features[J]. J Clin Med. 2019;9:1.
36. Berger S, Raman G, Vishwanathan R, et al. Dietary cholesterol and cardiovascular disease: a systematic review and meta-analysis[J]. Am J Clin Nutr. 2015;102(2):276–294. doi:10.3945/ajcn.114.100305
37. Wang HH, Garruti G, Liu M, et al. Cholesterol and lipoprotein metabolism and atherosclerosis: recent advances in reverse cholesterol transport[J]. Ann Hepatol. 2017;16(Suppl. 1: s3–105):s27–s42.
38. Hellenthal FA, Pulinx B, Welten RJ, et al. Circulating biomarkers and abdominal aortic aneurysm size[J]. J Surg Res. 2012;176(2):672–678. doi:10.1016/j.jss.2011.09.040
39. Pi S, Xiong S, Yuan Y, et al. The role of inflammasome in abdominal aortic aneurysm and its potential drugs[J]. Int J mol Sci. 2024;25(9):5001. doi:10.3390/ijms25095001
40. Lee JS, Park SC, Kim SD. The relation between metabolic syndrome and aspects of abdominal aortic aneurysm[J]. Asian J Surg. 2022;45(1):307–314.
41. Cho IY, Koo HY, Han K, et al. Metabolic syndrome and the risk of abdominal aortic aneurysm: a nationwide cohort study[J]. Atherosclerosis. 2023;386:117329. doi:10.1016/j.atherosclerosis.2023.117329
42. Kolahi Ahari R, Mansoori A, Sahranavard T, et al. Serum uric acid to high-density lipoprotein ratio as a novel indicator of inflammation is correlated with the presence and severity of metabolic syndrome: a large-scale study[J]. Endocrinol Diabetes Metab. 2023;6(6):e446. doi:10.1002/edm2.446
43. Liu R, Peng Y, Wu H, et al. Uric acid to high-density lipoprotein cholesterol ratio predicts cardiovascular mortality in patients on peritoneal dialysis[J]. Nutr Metab Cardiovasc Dis. 2021;31(2):561–569. doi:10.1016/j.numecd.2020.10.005
44. Li Y, Liu X, Luo Y. Monocyte to high-density lipoprotein cholesterol ratio and serum uric acid in Chinese adults: a cross-sectional study[J]. BMC Endocr Disord. 2022;22(1):48. doi:10.1186/s12902-022-00966-z
45. Han X, Tan X, Liu M, et al. Association between serum uric acid/high-density lipoprotein cholesterol ratio and hypertension among reproductive-aged women[J]. J Health Popul Nutr. 2023;42(1):123. doi:10.1186/s41043-023-00458-3
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




