Back to Journals » Journal of Pain Research » Volume 18
Associations Between Circulating Inflammatory Cytokines and Neuropathic Pain: A Two-Sample Mendelian Randomization Study
Authors Zheng Y , Wang H, Zhang H, Wu X, Zhou M , Denggui W
Received 12 September 2024
Accepted for publication 12 March 2025
Published 24 March 2025 Volume 2025:18 Pages 1525—1544
DOI https://doi.org/10.2147/JPR.S495896
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Alaa Abd-Elsayed
Yihan Zheng,1 Hongmei Wang,2 Huale Zhang,3 Xizhu Wu,1 Min Zhou,1 Wang Denggui1
1Department of Anesthesiology, Fujian Maternity and Child Health Hospital, College of Clinical Medicine for Obstetrics & Gynecology and Pediatrics, Fujian Medical University, Fuzhou, Fujian, 350001, People’s Republic of China; 2Department of Breast Surgery, Fujian Maternity and Child Health Hospital, College of Clinical Medicine for Obstetrics & Gynecology and Pediatrics, Fujian Medical University, Fuzhou, Fujian, 350001, People’s Republic of China; 3Department of Obstetrics, Fujian Maternity and Child Health Hospital, College of Clinical Medicine for Obstetrics & Gynecology and Pediatrics, Fujian Medical University, Fuzhou, Fujian, 350001, People’s Republic of China
Correspondence: Wang Denggui, Department of Anesthesiology, Fujian Maternity and Child Health Hospital, No. 18 Daoshan Road, Fuzhou City, Fujian Province, 350001, People’s Republic of China, Tel +86-0591-15980289738, Email [email protected]
Purpose: Several recent observational studies have reported that the circulating inflammatory cytokine composition is associated with neuropathic pain. However, the causal effect of 41 circulating inflammatory cytokines on neuropathic pain is unknown.
Patients and Methods: A two-sample Mendelian randomization study was performed using summary statistics for a genome-wide association study (GWAS) of circulating inflammatory cytokines conducted within three Finnish cohorts (YFS and FINRISK 1997 and 2002, n=8,293). The summary statistics of neuropathic pain were obtained from the GWAS dataset (800 patients and 195,047 controls). Inverse variance weighting, weighted median weighting, MR‒Egger regression, simple weighting, and weighted weighting were used to examine the causal associations between inflammatory cytokines and neuropathic pain. Sensitivity analyses, including the Cochran Q test, Egger intercept test, and leave-one-out analysis, were performed to verify the robustness of the MR results.
Results: Inverse variance weighted estimates suggested that G-CSF (OR=0.57, 95% CI=0.39– 0.83, P=3.4e− 03), IL-16 (OR=0.73, 95% CI=0.55– 0.96, P=2.7e− 02), and IL-1β (OR=0.57, 95% CI=0.33– 0.99, P=4.4e− 02) had protective effects on neuropathic pain. In addition, IP-10 (OR=1.36, 95% CI=1.06– 1.74, P=1.5e− 02) was suggested to be associated with neuropathic pain. No significant heterogeneity of instrumental variables or horizontal pleiotropy was found.
Conclusion: This two-sample Mendelian randomization study revealed that G-CSF, IL-16, IL-1β, and IP-10 were causally associated with neuropathic pain. This knowledge could guide future research in developing more effective treatments for neuropathic pain, potentially leading to better pain management options for patients.
Keywords: neuropathic pain, inflammatory cytokines, Mendelian randomization, genome-wide association study, pain management
Introduction
Neuropathic pain (NeP) is a complex and often chronic condition that results from nerve damage and significantly impacts quality of life.1,2 The impact of NeP on patients’ quality of life is substantial, imposing a significant economic burden on both society and individuals.3 Despite its prevalence, the biological mechanisms underlying neuropathic pain are poorly understood, hindering effective treatment development. A growing body of research suggests the potential role of inflammatory cytokines in the pathogenesis of neuropathic pain.4–6 Taken together, the intricate nature of NeP, its widespread prevalence, and its significant impact on both individual lives and societal economics underscore the importance and urgency of disease prevention strategies.
The intricate nature of the etiology of neuropathic pain continues to challenge the medical community, although recent advancements have emphasized the significant role of inflammatory processes, particularly the involvement of inflammatory cytokines.7 After nerve injury, inflammatory responses can lead to the onset and persistence of neuropathic pain. Inflammatory cytokines such as TNF- α, IL-1 β, and IL-6 play important roles in the pathophysiological process of neuropathic pain.7,8 These cytokines, which are critical for mediating immune responses, have emerged as focal points in understanding the pathophysiological mechanisms of NeP. Current research suggests that these signaling proteins potentially contribute to the sensitization that characterizes this pain state.9 Observational studies have further emphasized this, indicating a correlation between cytokine levels and the severity of neuropathic symptoms, pointing toward an intricate interplay of inflammatory factors and neural pathways.10 However, establishing a causal relationship has been challenging due to limitations in traditional observational studies, such as confounding factors and reverse causation.11
This study aimed to address these challenges using Mendelian randomization, a method that leverages genetic variants as instrumental variables to infer causal relationships between risk factors and clinical outcomes.12 Mendelian randomization offers a more robust approach than conventional observational studies by minimizing confounding factors. This is achieved through the random allocation of alleles at conception, mirroring the principles of a randomized controlled trial. Additionally, this method reduces the likelihood of reverse causation, as genetic variants are established at birth and therefore precede the development of neuropathic pain.13
In this work, we employed a two-sample Mendelian randomization strategy, an advanced form of MR, to determine the causal relationship between 41 inflammatory cytokines and NeP. This approach leverages data from extensive genome-wide association studies (GWASs), providing a more expansive genomic landscape to inform our analysis.11 Specifically, we aimed to discern whether the genetic factors that influence cytokine levels also play a role in susceptibility to or severity of NeP.
Material and Methods
This MR analysis included GWAS summary statistics that have already been published. The ethics committee at each institutional review board authorized all participants’ written informed consent in separate studies. No additional ethical approval or informed consent was needed. The STROBE-MR checklist has been checked and uploaded as supplementary data.14
MR Assumptions
There are three core assumptions of MR analysis, namely, relevance, independence, and exclusion restriction.15 It is assumed that the selected genetic variants are related to the risk factor (relevance) but not to any confounders in the risk factor–outcome association (independence) and that they are not connected with the outcome via any pathways other than the risk factor for interest (exclusion restriction). Here, in this bidirectional study, two GWASs were utilized to select genetically significant SNPs for 41 inflammatory cytokines and NeP (Figure 1).
Study Design and Data Sources
Our research utilized a two-sample Mendelian randomization (MR) approach, a powerful tool that leverages genetic variants as instrumental variables. This design is particularly advantageous because it minimizes potential confounders, offering more robust evidence of causality than traditional observational studies can provide. The primary objective was to ascertain the causal relationship between circulating inflammatory cytokines and the onset or severity of neuropathic pain.
With respect to our data, we performed a genome-wide association study (GWAS). The summary statistics for circulating inflammatory cytokines were extracted from studies conducted within three distinct Finnish cohorts: YFS, FINRISK 1997, and FINRISK 2002. Together, these cohorts encompassed a total of 8,293 individuals, providing a rich and diverse dataset for our analyses. On the other hand, the data concerning neuropathic pain were sourced from a separate GWAS dataset (https://gwas.mrcieu.ac.uk/datasets/finn-b-G6_TRINEU/). This dataset was notably extensive, comprising 800 patients with neuropathic pain and a substantial control group of 195,047 individuals. The sheer size of this control group was instrumental in enhancing the statistical power of our study, thereby increasing the reliability and validity of our findings. There was no overlap in population selection between the exposure group and the outcome group.
Instrumental Variable Selection
To ensure the reliability of these instruments, we implemented a stringent criterion, considering only single nucleotide polymorphisms (SNPs) that reached a genome-wide significance level (P<5×10−8) as valid instrumental variables. Given the scarcity of SNPs for certain cytokines when used as exposures, a higher cutoff (P<5×10−6) was applied. Subsequently, to mitigate linkage disequilibrium, we clumped these SNPs (kb=10,000, r2=0.001). Palindromic SNPs were excluded because their alignment direction for exposure and outcome in the GWASs of systemic inflammatory regulators could not be reliably determined. The proportion of variance in exposure was subsequently calculated using the R2 value of each SNP, and the instrument strength was estimated using the F-statistic to avoid weak instrument bias.16,17 Finally, we substituted the SNPs that were unavailable in the outcome summary with proxy SNPs (R2>0.9) from LDlink (https://ldlink.nci.nih.gov/).18
Statistical Analysis
Our analysis employed a multifaceted approach utilizing various MR methods to assess the causal association between inflammatory cytokines and neuropathic pain. The inverse variance weighted (IVW) method combines causal estimates from each SNP, weighting them by their precision; however, it assumes that all genetic variants are valid instrumental variables, an assumption that may not hold in practice.19 Thus, other robust methods that do not require all genetic variants to be valid IVs were also employed to give consistent estimates of a causal parameter. The weighted median approach was more robust than the other methods, providing a consistent estimate even if up to half of the weight came from invalid SNPs.20 The MR‒Egger method was particularly useful in cases of potential pleiotropy, offering a causal estimate that was corrected for such instances.21 Additionally, the simple mode and weighted mode methods prioritized the most consistent SNP-specific causal estimates. To further bolster the reliability of our findings, we conducted a series of sensitivity analyses. Cochrans’ Q test was employed to assess any heterogeneity among the different instrumental variables. The Egger intercept test was crucial in detecting directional horizontal pleiotropy, a scenario where genetic variants might affect the outcome through pathways other than the exposure pathway. Leave-one-out analysis was instrumental in evaluating the influence of individual SNPs on the overall results. Finally, we performed reverse Mendelian randomization and Steiger tests to verify the causal relationship between inflammatory factors and NeP.
The major assessment for each regulator among all the approaches listed above was chosen in accordance with the recommended strategy, which would consider three fundamental assumptions, NOME and InSIDE.22 Should MR-PRESSO identify any outlier SNPs, these outliers will be initially excluded. Subsequently, the remaining instrumental variables (IVs) will undergo further evaluation to determine the appropriate statistical strategy. Once the recommended approach has been established, sensitivity analyses for causal relationships will be conducted concurrently, employing additional analytical techniques. We applied a Bonferroni correction to account for the number of systemic inflammatory regulators assessed (P<0.0012; Bonferroni correction with 41 tests).
The culmination of our research was the visual representation of our findings. We employed two distinct visualization tools for this purpose. The circular heatmap was invaluable in offering a comprehensive view of the relationships between multiple inflammatory cytokines and neuropathic pain. The tool highlights patterns and intensities of associations in a visually intuitive manner. On the other hand, the MR forest plot provided a more detailed perspective, revealing the causal effect estimates for each inflammatory cytokine, complete with their respective confidence intervals. This approach allowed for easy comparison and interpretation of the data, increasing the accessibility of the results to both experts and laypersons. All the statistical analyses were performed using R version 4.2.1 (R Foundation for Statistical Computing, Vienna, Austria). MR analyses were performed using TwoSampleMR and MR-PRESSO (version 0.5.6).23 The study was not preregistered on any platform.
Ethics Approval and Consent to Participate
This research has been conducted using published studies and consortia providing publicly available summary statistics. All original studies have been approved by the corresponding ethical review board, and the participants have provided informed consent (FINRISK 1997: Ethical Committee of National Public Health Institute, Statement 38/96.30.10.1996; FINRISK 2002: Helsinki University Hospital, Ethical Committee of Epidemiology and Public Health, Statement 87/2001; YFS: The study protocol was reviewed and approved by Ethics Committees of each of the participating universities (medical schools of Helsinki, Turku, Tampere, Kuopio, and Oulu); finn-b-G6_TRINEU: North West Centre for Research Ethics Committee, 11/NW/0382). In addition, no individual-level data was used in this study. Therefore, no new ethical review board approval was required. According to the 2017 International Ethical Guidelines for Health-related Research Involving Humans (Council for International Organizations of Medical Sciences, CIOMS), studies using publicly available data that ensure participant anonymity may be exempt from Institutional Review Board (IRB) approval.24 Additionally, per Chinese national legislation guidelines (“Measures for Ethical Review of Life Science and Medical Research Involving Human Subjects, Article 32, Items 1 and 2”), this research is not subject to further ethics committee review.25
Results
Of the forty-one systemic inflammatory regulators examined, nine had three or more valid genetic variants when the genome-wide significance cutoff was set at P<5×10−8. For the remaining cytokines, a higher threshold (P<5×10−6) was applied to ensure that enough SNPs were present for subsequent MR analysis. All the F-statistic values of the SNPs surpassed 10, suggesting a low likelihood of significant weak instrument bias (Supplementary Tables S1–S3).
According to the selection criteria of IVs, a total of 745 SNPs were used as IVs for 41 circulating inflammatory cytokines. As shown in Table 1, five inflammatory cytokines, namely, G-CSF, IL-16, IL-1β, IL-2, and IP-10, were shown to be associated with neuropathic pain in at least one MR analysis. In our quest to understand the intricate relationship between circulating inflammatory cytokines and neuropathic pain, our Mendelian randomization analysis revealed several significant findings. By leveraging the inverse variance weighted (IVW) method, we were able to delve into the associations and unearth the roles of various inflammatory cytokines in relation to neuropathic pain.
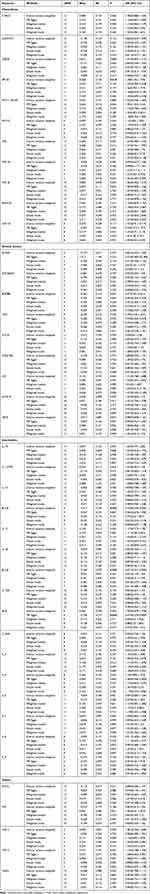 |
Table 1 MR Result of Causal Correlations of 41 Inflammatory Cytokines on Neuropathic Pain (NP) |
One of the most striking findings was the protective effect of G-CSF on neuropathic pain (OR=0.57, 95% CI=0.39–0.83; P=3.4e−03). In simpler terms, these numbers suggest that individuals with elevated levels of G-CSF might experience a decreased risk of developing neuropathic pain (Figure 2A and 3). This protective effect not only is statistically significant but also hints at potential therapeutic avenues.
 |
Figure 3 The results of Mendelian randomization (MR) analyses. |
IL-16, another inflammatory cytokine, was shown to be associated with the protective effect of G-CSF (OR=0.73, 95% CI=0.55–0.96; P=2.7e−02). These findings further reinforce the hypothesis that certain inflammatory cytokines, when present at higher concentrations, might play pivotal roles in mitigating the onset or severity of neuropathic pain (Figure 2B and 3).
IL-1β, yet another cytokine in our study, paralleled the findings of G-CSF and IL-16. This treatment had a protective effect (OR =0.57, 95% CI=0.33–0.99, P=4.4e−02). These trifecta of cytokines, which all indicate a protective effect, underscore the potential complexities and interplay involved in the inflammatory response related to neuropathic pain (Figure 2C and 3).
However, not all cytokines followed this protective trend. IP-10, for instance, deviated from this pattern. Our analysis indicated that IP-10 might be associated with an increased risk of neuropathic pain (OR=1.36, 95% CI=1.06–1.74; P= 1.5e−02). This finding suggests a potential cautionary role for IP-10, indicating that elevated levels of this cytokine might be linked to increased susceptibility to neuropathic pain (Figure 2D and 3). The results showing suggestive associations were considered significant (P < 0.05) before correction but did not maintain significance after multiple-comparison adjustment (P < 0.0012, Bonferroni correction with 41 tests).26 Since this was an exploratory study, we did not correct for multiple testing.
Given the profound implications of our primary findings, we deemed it crucial to validate these results through a series of sensitivity analyses. These analyses aimed to test the robustness and reliability of our primary results. Funnel plots of the Mendelian randomization analyses for G-CSF, IL-16, IL-1β, and IP-10 in patients with neuropathic pain are shown in Figure 4. There were not potential outliers of the IVs of G-CSF, IL-16, IL-1β, IP-10 that were present on visual inspection in leave-one-out plots (Figure 5). The Cochran Q test, a measure used to assess heterogeneity among different instrumental variables, did not indicate any significant discrepancies (Supplementary Table S4), and no outlier SNPs were detected with the MR-PRESSO method (Supplementary Table S5). Similarly, the Egger intercept test, which was designed to detect potential horizontal pleiotropy (Supplementary Table S6), and the leave-one-out analysis (Figure 5), which evaluates the influence of individual SNPs on the overall results, both corroborated our primary findings. The Steiger test showed that IL-16 was upstream of the outcome (P= 0.012; Supplementary Table S7). However, the influence of NeP on 41 inflammatory cytokines, according to the result of IVW (Table 2), was proven that there was no reverse causal association between Nep and G-CSF (P=0.541), IL-16 (P=0.794), IL-1β (P=0.940), IP-10 (P=0.593).
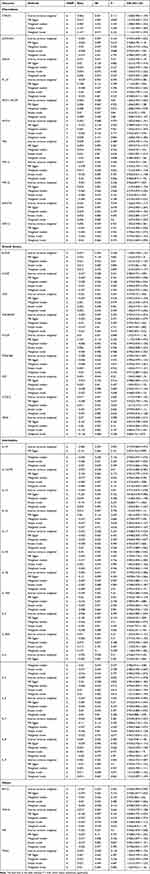 |
Table 2 MR Result of Causal Correlations of Neuropathic Pain (NP) on 41 Inflammatory Cytokines |
 |
Figure 5 Leave-one-out causal estimate of Mendelian randomization (MR) analyses. |
To further elucidate and visually represent our findings, we employed tools such as the circular heatmap (Figure 6) and the MR forest plot (Figure 7). With its vibrant color gradients, the heatmap provides a panoramic view of the relationships between multiple inflammatory cytokines and neuropathic pain. On the other hand, the MR forest plot provided a more granular perspective, detailing the causal effect estimates for each cytokine, complete with their respective confidence intervals.
 |
Figure 6 The circular heatmap. With its vibrant color gradients, the heatmap provides a panoramic view of the relationships between multiple inflammatory cytokines and neuropathic pain. |
 |
Figure 7 The MR Forest plot. MR forest plot provided a more granular perspective, detailing the causal effect estimates for each cytokine, complete with their respective confidence intervals. |
In conclusion, our results shed light on the multifaceted relationships between inflammatory cytokines and neuropathic pain, suggesting potential avenues for future research and therapeutic interventions.
Discussion
In this two-sample MR analysis, we first investigated the causative relationships of 41 biomarkers, including growth factor, interleukin, and chemokine levels, and evaluated NeP as the outcome. The relationship between circulating inflammatory cytokines and NeP has been a focal point of numerous studies, with the overarching goal of understanding the underlying mechanisms and identifying potential therapeutic targets. Our Mendelian randomization study shed light on this intricate relationship, suggesting a causal association between specific inflammatory cytokines and NeP. These findings not only corroborate the literature but also provide novel insights that could pave the way for future research and therapeutic interventions.
The protective effects observed for G-CSF, IL-16, and IL-1β in our study align with the broader understanding of the role of inflammatory cytokines in various diseases. Granulocyte colony stimulating factor (G-CSF) is known for its role in promoting the growth of white blood cells and may have implications in modulating pain pathways, potentially offering protective mechanisms against neuropathic pain.27 Ming-Feng Liao et al demonstrated that G-CSF can relieve neuropathic pain through animal experiments.28 Additionally, in a Phase I and IIa clinical trial, G-CSF was shown to relieve neuropathic pain in patients with compression myelopathy.29 Although there have been few studies on G-CSF in NeP, its underlying function in the formation of NeP should be investigated, and exploratory research utilizing more comprehensive data should be conducted to elucidate the link between G-CSF levels and NeP.
IL-1β (interleukin-1 beta), a cytokine known for its role in inflammatory processes, can influence the neuropathic pain pathway, either by exacerbating or alleviating pain symptoms. Mingzhu Li et al showed that IL-1β participates in preventing and treating oxaliplatin-induced neuropathic pain.30 Conversely, in an observational study, increased IL-1β release seemed to be a particular phenomenon in patients with NeP.31 In our study, we found that IL-1β has a protective effect against neuropathic pain. More research should be conducted to verify this relationship and elucidate the underlying mechanisms involved.
IL-16 (interleukin-16) is an immunomodulatory chemokine that signals through CD4+ T cells, monocytes, macrophages, and dendritic cells.32 However, the role of IL-16 in NeP is uncertain. In our research, we discovered that IL-16 plays a defensive role in mitigating neuropathic pain. Further investigations are warranted to confirm this link and to clarify the underlying processes involved. For instance, a Mendelian randomization analysis by Bouras et al revealed associations between specific inflammatory biomarkers and the risk of several cancers.33 Similarly, Li et al explored the causal effects of inflammatory cytokines on the risk of ischemic stroke.34 These observations contribute to the broader understanding of how inflammatory cytokines, often associated with various diseases, can have specific implications in the context of neuropathic pain. These studies underscore the multifaceted roles of inflammatory cytokines in health and disease.
Interestingly, our findings regarding the protective effects of certain cytokines against neuropathic pain are in line with recent studies that have investigated the role of inflammatory cytokines in other diseases. For instance, Guan et al conducted a Mendelian randomization study exploring the causal correlations between inflammatory cytokines and hypertensive disorders during pregnancy.35 Their study suggested that certain cytokines, such as interleukin-9 (IL-9) and macrophage migration inhibitory factor (MIF), might reduce HDP risk, while others could be involved in HDP development.
Furthermore, the role of inflammatory cytokines in the context of infectious diseases, such as COVID-19, has been a topic of recent interest. Wang et al conducted a Mendelian randomization analysis to identify the causal effects of COVID-19 on 41 cytokines.36 Their findings indicated that certain cytokines are promoted by COVID-19, while others are inhibited, emphasizing the complex interplay between viral infections and the host inflammatory response.
Interferon-γ (IFN-γ)-induced protein 10 (IP-10 or CXCL-10) is a chemokine involved in trafficking immune cells to inflammatory sites.37 The increased risk associated with IP-10, as observed in our study, is particularly intriguing. These findings underscore the need for a deeper understanding of the role of IP-10 in the pathogenesis of neuropathic pain. Dong and Ubogu highlighted the association between proinflammatory cytokines and chronic neuropathic pain in traumatic and inflammatory neuropathies.10 Their observations suggest that early expression of specific proinflammatory cytokines might predict the development of chronic nociception.
This study involved inaugural Mendelian randomization analysis to explore the causal link between NeP and 41 inflammatory cytokines. Nevertheless, it is important to acknowledge its limitations. First, constraints in the MR analysis meant that the second and third assumptions were not thoroughly tested, which could introduce bias. Second, our data were sourced from two extensive GWASs, but a lack of detailed demographic and clinical data precluded subgroup analyses. Third, the study may have an ethnic bias, as participants were predominantly of European descent; this cautions against generalizing the findings to other ethnic groups. Moreover, given the heterogeneity of neuropathic pain, with cytokine profiles varying across subpopulations due to factors like pain etiology and comorbidities, the findings may not fully represent the diversity observed in specific patient groups,38 Other molecules that are not cytokines, so far little investigated in neuropathic pain, may have a more causal role in neuropathic pain.39 However, further research is needed to validate our findings and explore their potential applications in clinical diagnosis and treatment strategies.
Conclusion
In conclusion, our study has added to the growing body of evidence highlighting the pivotal role of inflammatory cytokines in NeP. As the field continues to evolve, it is crucial to integrate findings from various studies to develop a comprehensive understanding of the underlying mechanisms and identify potential therapeutic targets.
Acknowledgments
The authors express their gratitude to the participants and investigators of the FinnGen study. The authors also sincerely thank related investigators for sharing the GWAS summary statistics included in this study.
Funding
(1) Fujian Provincial Health Commission Young and Middle-Aged Talents Training Project (Grant Number: 2020GGB043). (2) Joint Funds for the Innovation of Science and Technology, Fujian Province (Grant Number: 2023Y9390).
Disclosure
The authors declare that they have no competing interests.
References
1. Ji RR, Kohno T, Moore KA, Woolf CJ. Central sensitization and LTP: do pain and memory share similar mechanisms? Trends Neurosci. 2003;26(12):696–705. doi:10.1016/j.tins.2003.09.017
2. Gao Y, Sun N, Wang L, et al. Bioinformatics Analysis Identifies p53 as a Candidate Prognostic Biomarker for Neuropathic Pain. Front Genetics. 2018;9:320. doi:10.3389/fgene.2018.00320
3. Moisset X, Pagé MG. Interest of registries in neuropathic pain research. Revue Neurol. 2021;177(7):843–848. doi:10.1016/j.neurol.2021.07.011
4. Finnerup NB, Kuner R, Jensen TS. Neuropathic Pain: from Mechanisms to Treatment. Physiol Rev. 2021;101(1):259–301. doi:10.1152/physrev.00045.2019
5. Golubovic M, Kostic T, Djordjevic M, et al. In silico development of potential therapeutic for the pain treatment by inhibiting voltage-gated sodium channel 1.7. Comput Biol Med. 2021;132:104346. doi:10.1016/j.compbiomed.2021.104346
6. Seo H, Jun SC. Computational exploration of epidural cortical stimulation using a realistic head model. Comput Biol Med. 2021;135:104290. doi:10.1016/j.compbiomed.2021.104290
7. Sommer C, Leinders M, Üçeyler N. Inflammation in the pathophysiology of neuropathic pain. Pain. 2018;159(3):595–602. doi:10.1097/j.pain.0000000000001122
8. Hung A, Lim M, Doshi T. Targeting cytokines for treatment of neuropathic pain. Scand J Pain. 2017;17(1):287–293. doi:10.1016/j.sjpain.2017.08.002
9. Lees JG, Fivelman B, Duffy SS, Makker PG, Perera CJ, Moalem-Taylor G. Cytokines in Neuropathic Pain and Associated Depression. Modern Tends Pharmacopsychiatry. 2015;30:51–66.
10. Dong C, Ubogu EE. Pro-inflammatory cytokines and leukocyte integrins associated with chronic neuropathic pain in traumatic and inflammatory neuropathies: initial observations and hypotheses. Front Immunol. 2022;13:935306. doi:10.3389/fimmu.2022.935306
11. Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genetic Epidemiol. 2013;37(7):658–665. doi:10.1002/gepi.21758
12. Smith GD, Ebrahim S. ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol. 2003;32(1):1–22. doi:10.1093/ije/dyg070
13. Davey Smith G, Hemani G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Human Molecular Genetics. 2014;23(R1):R89–98. doi:10.1093/hmg/ddu328
14. Skrivankova VW, Richmond RC, Woolf BAR, et al. Strengthening the Reporting of Observational Studies in Epidemiology Using Mendelian Randomization: the STROBE-MR Statement. JAMA. 2021;326(16):1614–1621. doi:10.1001/jama.2021.18236
15. Emdin CA, Khera AV, Kathiresan S. Mendelian Randomization. JAMA. 2017;318(19):1925–1926. doi:10.1001/jama.2017.17219
16. Pierce BL, Ahsan H, Vanderweele TJ. Power and instrument strength requirements for Mendelian randomization studies using multiple genetic variants. Int J Epidemiol. 2011;40(3):740–752. doi:10.1093/ije/dyq151
17. Palmer TM, Lawlor DA, Harbord RM, et al. Using multiple genetic variants as instrumental variables for modifiable risk factors. Statistical Methods Med Res. 2012;21(3):223–242. doi:10.1177/0962280210394459
18. Machiela MJ, Chanock SJ. LDlink: a web-based application for exploring population-specific haplotype structure and linking correlated alleles of possible functional variants. Bioinformatics. 2015;31(21):3555–3557. doi:10.1093/bioinformatics/btv402
19. Wootton RE, Richmond RC, Stuijfzand BG, et al. Evidence for causal effects of lifetime smoking on risk for depression and schizophrenia: a Mendelian randomisation study. Psychological Med. 2020;50(14):2435–2443. doi:10.1017/S0033291719002678
20. Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent Estimation in Mendelian Randomization with Some Invalid Instruments Using a Weighted Median Estimator. Genetic Epidemiol. 2016;40(4):304–314. doi:10.1002/gepi.21965
21. Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44(2):512–525. doi:10.1093/ije/dyv080
22. Jin H, Lee S, Won S. Causal Evaluation of Laboratory Markers in Type 2 Diabetes on Cancer and Vascular Diseases Using Various Mendelian Randomization Tools. Front Genetics. 2020;11:597420. doi:10.3389/fgene.2020.597420
23. Hemani G, Tilling K, Davey Smith G. Orienting the causal relationship between imprecisely measured traits using GWAS summary data. PLoS Genetics. 2017;13(11):e1007081. doi:10.1371/journal.pgen.1007081
24. van Delden JJ, van der Graaf R. Revised CIOMS International Ethical Guidelines for Health-Related Research Involving Humans. JAMA. 2017;317(2):135–136. doi:10.1001/jama.2016.18977
25. National Health Commission of the People’s Republic of China MoE, Ministry of Science and Technology, National Administration of Traditional Chinese Medicine. Ethical Review Measures for Research Involving Human Life Sciences and Medicine. National Health Commission of the People’s Republic of China Website.
26. Georgakis MK, Gill D, Rannikmäe K, et al. Genetically Determined Levels of Circulating Cytokines and Risk of Stroke. Circulation. 2019;139(2):256–268. doi:10.1161/CIRCULATIONAHA.118.035905
27. Ro LS, Chen SR, Chao PK, Lee YL, Lu KT. The potential application of granulocyte colony stimulating factor therapy on neuropathic pain. Chang Gung Med J. 2009;32(3):235–246.
28. Liao MF, Hsu JL, Lu KT, et al. Granulocyte Colony Stimulating Factor (GCSF) Can Attenuate Neuropathic Pain by Suppressing Monocyte Chemoattractant Protein-1 (MCP-1) Expression, through Upregulating the Early MicroRNA-122 Expression in the Dorsal Root Ganglia. Cells. 2020;9(7):1669. doi:10.3390/cells9071669
29. Kato K, Yamazaki M, Okawa A, et al. Intravenous administration of granulocyte colony-stimulating factor for treating neuropathic pain associated with compression myelopathy: a phase I and IIa clinical trial. Eur Spine J. 2013;22(1):197–204. doi:10.1007/s00586-012-2556-9
30. Li M, Li Z, Ma X, et al. Huangqi Guizhi Wuwu Decoction can prevent and treat oxaliplatin-induced neuropathic pain by TNFα/IL-1β/IL-6/MAPK/NF-kB pathway. Aging. 2022;14(12):5013–5022. doi:10.18632/aging.203794
31. Luchting B, Heyn J, Woehrle T, et al. Differential expression of P2X7 receptor and IL-1β in nociceptive and neuropathic pain. J Neuroinflamm. 2016;13(1):100. doi:10.1186/s12974-016-0565-z
32. Huang Y, Du KL, Guo PY, et al. IL-16 regulates macrophage polarization as a target gene of mir-145-3p. Mol Immunol. 2019;107:1–9. doi:10.1016/j.molimm.2018.12.027
33. Bouras E, Karhunen V, Gill D, et al. Circulating inflammatory cytokines and risk of five cancers: a Mendelian randomization analysis. BMC Med. 2022;20(1):3. doi:10.1186/s12916-021-02193-0
34. Li Y, Lu J, Wang J, Deng P, Meng C, Tang H. Inflammatory Cytokines and Risk of Ischemic Stroke: a Mendelian Randomization Study. Front Pharmacol. 2021;12:779899. doi:10.3389/fphar.2021.779899
35. Guan S, Bai X, Ding J, Zhuang R. Circulating inflammatory cytokines and hypertensive disorders of pregnancy: a two-sample Mendelian randomization study. Front Immunol. 2023;14:1297929. doi:10.3389/fimmu.2023.1297929
36. Wang C, Yu R, Zhang S, et al. Genome-wide Mendelian randomization and single-cell RNA sequencing analyses identify the causal effects of COVID-19 on 41 cytokines. Brief Funct Genomics. 2022;21(6):423–432. doi:10.1093/bfgp/elac033
37. Lei J, Yin X, Shang H, Jiang Y. IP-10 is highly involved in HIV infection. Cytokine. 2019;115:97–103. doi:10.1016/j.cyto.2018.11.018
38. Pellesi L, Bellei E, Guerzoni S, et al. Exploration of candidate serum biomarkers potentially related to the chronic pain condition in Medication-overuse headache. BMC Neurol. 2019;19(1):239. doi:10.1186/s12883-019-1469-1
39. Pellesi L, Guerzoni S, Baraldi C, Cainazzo MM, Pini LA, Bellei E. Identification of candidate proteomic markers in the serum of medication overuse headache patients: an exploratory study. Cephalalgia. 2020;40(10):1070–1078. doi:10.1177/0333102420921847
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Genetically Predicted Serum Albumin and Risk of Colorectal Cancer: A Bidirectional Mendelian Randomization Study
Lv L, Sun X, Liu B, Song J, Wu DJH, Gao Y, Li A, Hu X, Mao Y, Ye D
Clinical Epidemiology 2022, 14:771-778
Published Date: 21 June 2022
A Randomized, Double-Blind, Placebo-Controlled Trial to Evaluate the Therapeutic Effect of Magnesium-L-Threonate Supplementation for Persistent Pain After Breast Cancer Surgery
Ni Y, Deng F, Yu S, Zhang J, Zhang X, Huang D, Zhou H
Breast Cancer: Targets and Therapy 2023, 15:495-504
Published Date: 25 July 2023
Causal Relationship Between Endometriosis and Pelvic Inflammatory Diseases: Mendelian Randomization Study
Liu K, Liu X, Cao T, Cui X, Sun P, Zhang L, Wu X
International Journal of Women's Health 2024, 16:727-735
Published Date: 24 April 2024
Assessing Causality Between Androgenetic Alopecia with Depression: A Bidirectional Mendelian Randomization Study
Li H, Cai H, Li P, Zeng Y, Zhang Y
Clinical, Cosmetic and Investigational Dermatology 2025, 18:445-451
Published Date: 22 February 2025
Exploring the Association Between Immune Cell Phenotypes and Osteoporosis Mediated by Inflammatory Cytokines: Insights from GWAS and Single-Cell Transcriptomics
Kuang S, Ma X, Sun L, Wang C, Li Y, Wang G, Sun J, Zhou F, Zhang C
ImmunoTargets and Therapy 2025, 14:227-246
Published Date: 17 March 2025




