Back to Journals » Cancer Management and Research » Volume 17
Associations Between Postoperative Symptom Clusters and Functional Status in Lung Cancer Patients: A Cross-Sectional Study
Authors Liu Y, Lin S, Bai M, Yi H
Received 19 November 2024
Accepted for publication 2 June 2025
Published 12 June 2025 Volume 2025:17 Pages 1099—1111
DOI https://doi.org/10.2147/CMAR.S507420
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Sanjeev K. Srivastava
Yali Liu,1,* Siya Lin,2,* Meirong Bai,1 Huochun Yi3
1Department of Thoracic Surgery, Zhongshan Hospital Xiamen University, School of Medicine, Xiamen University, Xiamen, Fujian, 361004, People’s Republic of China; 2School of Nursing, Fujian Medical University, Fuzhou, Fujian, 350122, People’s Republic of China; 3Center of Clinical Laboratory, Zhongshan Hospital Xiamen University, School of Medicine, Xiamen University, Xiamen, Fujian, 361004, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Meirong Bai, Department of Thoracic Surgery, Zhongshan Hospital Xiamen University, School of Medicine, Xiamen University, 201 hubin South Road, Siming District, Xiamen, Fujian, 361004, People’s Republic of China, Email [email protected] Huochun Yi, Center of Clinical Laboratory, Zhongshan Hospital Xiamen University, School of Medicine, Xiamen University, 201 hubin South Road, Siming District, Xiamen, Fujian, 361004, People’s Republic of China, Email [email protected]
Background: Symptom clusters in cancer symptom management research, providing a scientific basis for developing effective strategies for symptom assessment and intervention aimed at improving patient quality of life and survival.
Objective: To analyze symptom clusters in postoperative lung cancer patients, examine its influenced factor, and explore the relationship between postoperative symptom clusters and functional status in lung cancer patients.
Methods: Between August 2023 and February 2024, 441 lung cancer patients who underwent surgical treatment in the Department of Thoracic Surgery at a tertiary hospital in Xiamen were selected. Data collection included a general information questionnaire, the Postoperative Patient-Reported Outcomes Scale for Early-Stage Lung Cancer Patients, the Tampa Scale for Kinesiophobia (TSK), and the Karnofsky Performance Status Scale (KPSS). Latent class analysis was employed to categorize the self-reported outcomes. Statistical analyses were performed on the relevant factors.
Results: The self-reported postoperative symptoms in lung cancer patients were divided into two groups: high-symptom burden and low-symptom burden. Significant differences were observed between these groups concerning surgery duration, kinesiophobia score, personality traits, KPSS, and the use of analgesic pumps (P < 0.005). After adjusting for sex, age, lifestyle, and health status, a multi-model approach confirmed a significant inverse relationship between higher KPSS levels and higher symptom burden (P < 0.001). High-symptom levels are negatively associated with functional status (P < 0.005).
Conclusion: Postoperative symptom clusters in lung cancer patients can be specifically categorized into high and low-symptom burdens. Surgery duration, kinesiophobia scores, personality traits, KPSS, and the use of analgesic pumps are significant risk factors affecting symptom burden. Postoperative symptom cluster assessment provides a scientific basis for developing effective management strategies, which may improve functional recovery and long-term outcomes in lung cancer patients.
Keywords: symptom clusters, functional status, lung cancer
Corrigendum for this paper has been published.
Introduction
Lung cancer is one of the most common malignancies globally, with rising incidence and mortality rates worldwide. In China, it is the most prevalent malignancy and the leading cause of cancer-related deaths.1,2 Surgery remains the primary treatment for patients with early-stage lung cancer. Improved public health awareness and advances in imaging technology have significantly improved the detection of early-stage lung cancer, leading to a considerable number of patients undergoing surgery. However, the invasive nature of the procedure presents a high risk of postoperative complications.
Research indicates that up to 79.5% of lung cancer patients experience postoperative symptoms.3 Common symptoms include pain, cough, sputum production, and sleep disturbances. These symptoms often occur together in interrelated groups, forming “symptom clusters” that influence each other, potentially exacerbating patient discomfort and negatively impacting their quality of life and functional status.4,5 Early detection and surgical treatment have improved the survival rate, assessing postoperative symptom clusters and effectively managing them may further improve survival and quality of life.6–9
Existing research on lung cancer symptoms usually centers on the general population or isolated symptoms, often overlooking the variability in symptom manifestation and distress among individuals. Latent Class Analysis (LCA), a probabilistic model-based classification method, identifies homogeneous subgroups of individuals with similar observable characteristics, grouping them into distinct classes based on their inherent traits. This method increases the distinction between classes while reducing differences within each class, aiding in identifying unique groups based on underlying connections and enabling more specific interventions for different patient groups.10
This study aims to analyze symptom clusters in postoperative lung cancer patients using a latent class analysis model and explore their internal characteristics. It examines risk indicators for patients with varying symptom characteristics. A multi-model approach is employed to investigate further the trend of the impact of high-symptom burden on postoperative functional status as measured by the Karnofsky Performance Status Scale (KPSS) score.
Methods
Design and Subjects
A convenience sampling method was used to select patients who underwent lung cancer resection surgery in the Department of Thoracic Surgery at a tertiary hospital in Xiamen, Fujian Province, from August 2023 to February 2024. The inclusion criteria were: (1) a confirmed diagnosis of lung cancer through cytological or histopathological examination; (2) age ≥ 18 years; (3) clear consciousness and adequate reading and comprehension abilities. Exclusion criteria were: (1) critical postoperative condition requiring transfer to the intensive care unit or voluntary discharge; (2) prior radiotherapy and/or chemotherapy before surgery; (3) co-morbid psychiatric disorders or other severe physical illnesses. Using Kendall’s sample size estimation method, with a total of 31 variables and accounting for a 10% dropout rate, the final sample size was 441 patients11 (Figure 1).
 |
Figure 1 Flowchart of patients inclusion and exclusion. |
Data Collection Methods
Before the survey began, all investigators received standardized training. They completed the general information questionnaire using the electronic medical record system. Before patient discharge, with consent obtained, investigators explained the survey’s purpose, instructed on questionnaire completion, and provided necessary instructions using standardized language. Any unclear items were clarified in simple terms. For illiterate patients or those who had difficulty with the questionnaire, investigators read the items aloud and recorded responses based on the patients’ answers. The questionnaires were distributed and collected on-site to ensure completeness and accuracy. If any items were unanswered, investigators prompted patients to complete them immediately. Incomplete questionnaires or those with obviously inconsistent answers were considered invalid.
This study used structured questionnaires for data collection, divided into the following parts:
General Information Questionnaire
A self-designed general information questionnaire was developed based on a thorough review of relevant literature and the objectives of this study. It includes variables such as gender, age, marital status, education level, employment status, economic level, lifestyle, personality type, BMI, actual FEV1 value, ejection fraction (EF), duration of surgery, lymph node dissection, use of patient controlled analgesia (PCA), intraoperative anesthesia, intraoperative bleeding, and the extent of surgical resection (Table 1).
 |
Table 1 Early Postoperative Patient-Reported Outcomes Scale for Lung Surgery |
Postoperative Patient-Reported Outcomes Scale for Lung Cancer Patients
The Postoperative Patient-Reported Outcomes Scale for Lung Cancer Patients, created by Ohguri et al12 includes 54 items across four domains: physiological (chest symptoms, gastrointestinal symptoms, systemic symptoms, independence), psychological (anxiety, depression, pessimism), social (social support, social adaptation), and treatment (effectiveness, satisfaction, compliance, adverse treatment reactions). Each item is rated on a 5-point Likert scale, with items 1–17, 20–32, 38–42, and 53 scored positively from 1 to 5 points, and items 18–19, 33–37, 43–52, and 54 reverse-scored. The scale’s item-level content validity index (I-CVI) ranges from 0.800 to 1.000, with a scale-level content validity index/average (S-CVI/Ave) of 0.940. The Cronbach’s alpha coefficient is 0.927, and the split-half reliability is 0.735.
Tampa Scale for Kinesiophobia-11 (TSK-11)
The Tampa Scale for Kinesiophobia-11 (TSK-11) was originally developed by Das et al13 and later revised into a shorter version by Woby et al.14 The Chinese version was translated and validated by Cai Libai et al.15 This scale assesses the level of kinesiophobia in patients, comprising 11 items across three dimensions: cognitive aspects of activity, behavioral aspects of activity, and attitudes towards activity. The total score ranges from 11 to 44, with scores over 26 indicating kinesiophobia. Higher scores suggest increased levels of kinesiophobia. The scale’s Cronbach’s alpha coefficient is 0.88, and its test-retest reliability is 0.80.
Karnofsky Performance Status Scale (KPSS)
The Karnofsky Performance Status Scale (KPSS), developed by Karnofsky et al16 is employed to assess patients’ functional status based on their activity level, disease condition, and ability to perform self-care. The scale includes 11 levels, with a total score ranging from 0 to 100, where each level represents a 10-point increment. Higher scores indicate better health status. The scale’s Cronbach’s alpha coefficient ranges from 0.97 to 1.00, and its inter-rater reliability is 0.89.
Data Analysis
Two individuals independently entered and verified all data before analysis using SPSS version 27.0. The Kolmogorov–Smirnov test assessed data normality. Normally distributed continuous variables were shown as mean ± standard deviation, while non-normally distributed continuous variables were reported as median and interquartile range. Categorical variables were presented as frequencies and percentages. Latent class analysis using R version 4.3.3 classified six dimensions of self-reported outcomes: chest symptoms, gastrointestinal symptoms, systemic symptoms, anxiety, depression, and pessimism. Univariate analysis and logistic regression identified risk factors associated with these categories. Using R version 4.3.3, covariates were excluded, and a multi-model strategy examined the impact trend of high-symptom burden on postoperative functional status as measured by the Karnofsky Performance Status Scale (KPSS) score. Statistical significance was defined as P < 0.05.
Results
General Information of Study Subjects
Out of 450 distributed questionnaires, and 441 valid responses were included in the final analysis after excluding incomplete (n=6) and logically inconsistent responses (n=3), yielding a valid response rate of 98%. Patient ages ranged from 19 to 83 years, with a mean of (55.92 ± 12.76) years. The mean duration of indwelling catheters was (4.44 ± 3.82) days, and the mean surgery time was 167.0 [100.0, 216.0] minutes. The kinesiophobia score averaged 23.0 [19.0, 28.0].
Latent Class Analysis of Postoperative Symptom Clusters in Lung Cancer Patients
A latent class model (LCM) was developed using six dimensions of self-reported distress symptoms: chest symptoms, gastrointestinal symptoms, systemic symptoms, anxiety, stress, and pessimism. The analysis began with a single-class model and incrementally increased the number of classes to five. Model fit was evaluated using AIC, BIC, G², and χ² values, with lower values indicating a better fit. In cases of conflicting indicators, BIC was prioritized.17 The results indicated that the minimum values for AIC and BIC were achieved with two classes. Increasing the number of classes resulted in higher indices. Although G² increased when transitioning from one to two classes, this increase was not significant. After evaluating all fit indices, the two-class model was identified as the most appropriate (Table 2).
 |
Table 2 Goodness-of-Fit Test Results |
Patients were categorized based on the severity of six symptoms. Those with high levels of all six symptoms were placed in the “high-symptoms Group”, while those with low levels were placed in the “low-symptoms Group”. The analysis identified 147 patients (33.33%) in the high-symptoms Group and 294 patients (66.67%) in the low-symptoms Group (Figure 2).
 |
Figure 2 The characteristic distribution of 2 potential categories of postoperative symptoms in lung cancer patients. |
Univariate Analysis of Postoperative Symptoms in Lung Cancer Patients
Univariate analysis was conducted with symptom levels (high vs low) as the dependent variable. It was found that the duration of surgery, Kinesiophobia scores, KPSS scores, personality traits, and discontinuation of PCA significantly influenced symptom levels in lung cancer patients (Table 3).
 |
Table 3 Univariate Analysis Results for High and Low-Symptoms in Postoperative Lung Cancer Patients |
Multivariate Logistic Regression Analysis of Factors Influencing High and Low-Symptoms in Postoperative Lung Cancer Patients
A multivariate logistic regression analysis was performed using variables that showed statistical significance (P <0.05) in the univariate analysis as independent variables, with high and low-symptom levels as the dependent variable. The analysis revealed that the duration of surgery, Kinesiophobia scores, KPSS scores, personality type, and use of an analgesic pump were independent risk factors for high or low-symptom levels in postoperative lung cancer patients (P <0.05) (Table 4).
 |
Table 4 Multivariate Analysis Results for High and Low-Symptoms |
Multi-Model Relationship Between Postoperative Functional Status Scores and High-Symptom Levels in Lung Cancer Patients
Postoperative functional status was categorized based on scores, and covariates were adjusted. Results from Model 1, Model 2, and Model 3 indicated that the P for trend was less than 0.05 in all models. This shows a negative correlation between high-symptom levels and functional status scores, with higher functional status scores associated with fewer incidences of high-symptoms (Table 5).
 |
Table 5 Multimodel Strategy for Functional Status Scale (KPSS) Scores and High-Symptom |
The restricted cubic spline (RCS) plot reveals a significant negative correlation between functional status (KPSS) scores and the incidence of high-symptom levels in both male and female patients. As functional status (KPSS) scores increase, the risk of high-symptom occurrence decreases. The 95% confidence interval narrows in the higher score range, indicating less uncertainty in risk estimates at these levels. The overall P-value of the model is extremely low (<0.001), indicating statistical significance. The P-value for nonlinearity is 0.116, suggesting there is insufficient statistical evidence for a significant nonlinear relationship between functional status (KPSS) scores and symptom severity. Refer to Figure 3 for a detailed presentation of the results.
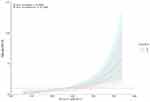 |
Figure 3 Restricted Cubic Spline Plot of Postoperative Functional Status (KPSS) Scores and high-symptom Levels in Lung Cancer Patients. |
Discussion
Specificity of Potential Categories of Symptom Clusters in Postoperative Lung Cancer Patients
Latent class analysis of symptom clusters in postoperative lung cancer patients revealed significant differences among the clusters. Notably, 33.3% of patients fell into the high-symptom group, characterized by elevated levels of distressing symptoms, particularly anxiety, chest symptoms, and systemic symptoms. Anxiety, which is prevalent among postoperative lung cancer patients, can reduce quality of life and hinder recovery. Healthcare professionals are advised to closely monitor patients’ psychological states, providing timely interventions and calming measures to manage anxiety.
Chest symptoms are pronounced in postoperative lung cancer patients. Contributing factors include healing of chest wounds, pain, chest drainage tubes, and increased airway secretions, all of which can cause discomfort.18 Healthcare professionals should monitor these symptoms closely, adjust treatment plans promptly, and alleviate discomfort.
Systemic symptoms, common in postoperative patients, may stem from surgical stress, reduced immune function, discomfort in the hospital setting, and perioperative physical depletion. It is crucial for healthcare professionals to assess these symptoms comprehensively and develop appropriate rehabilitation plans to improve patients’ quality of life.
The Impact of Surgery Duration on Symptom Clusters in Postoperative Lung Cancer Patients
Research has shown that surgery duration can independently predict the extent of postoperative symptoms. This occurs for several reasons. First, patients requiring longer surgeries, such as those involving extensive lymph node dissection, often have more severe conditions. For instance, the average surgery time for a lobectomy is 144.9 minutes, compared to 111.2 minutes for a sub-lobar resection.19 This indicates that the severity of the condition correlates with surgery duration, thus exacerbating postoperative symptoms. Additionally, prolonged surgeries can induce stress responses in patients, affecting their blood pressure, blood sugar levels, and immune systems. Notably, surgeries exceeding 240 minutes have been linked to intraoperative hyperglycemia,20 and extended surgery durations are associated with higher rates of postoperative infections.21 Consequently, surgical duration not only reflects the severity of a patient’s condition but may also worsen postoperative symptoms through various physiological stress responses. Therefore, it is crucial to focus on multidisciplinary collaboration to reduce surgical duration,22 involving improved coordination among surgeons, nurses, anesthesiologists, and pathologists to improve the efficiency of surgical teams, shorten surgery times, and reduce postoperative complications, thereby improving patient recovery rates.
Impact of Kinesiophobia on Postoperative Symptom Clusters in Lung Cancer Patients
In this study, kinesiophobia was present in 174 patients, representing an incidence rate of 39.50%, consistent with findings by Liu Yanjin et al.23 According to the “fear-avoidance” model by Lethem et al, kinesiophobia occurs when patients perceive pain as a threat, leading to fear associated with pain sensations. This fear significantly affects their physical sensations, increasing sensitivity to normal bodily responses like touch or movement.
During postoperative rehabilitation, this fear results in avoidance or resistance to physical activity, negatively impacting quality of life and worsening pain issues. Patients who focus excessively on pain and its associated threats experience increased fear, which increases their attention to these stimuli, creating a vicious cycle that can lead to organ disuse. According to a 2014 systematic review by Wertli et al24 higher levels of kinesiophobia correlate with stronger perceptions of pain and significantly affect the recovery of physical activity levels.
Impact of Personality on Postoperative Symptom Clusters in Lung Cancer Patients
This study discovered that extroverted patients experienced fewer severe symptom burdens compared to introverted patients. This difference may be due to the six dimensions of symptoms—chest, gastrointestinal, systemic, anxiety, stress, and pessimism—which include both physiological and psychological elements. Introverted patients, who are less likely to express their psychological concerns, showed more intense psychological symptoms. Research indicates that individuals with a sanguine, extroverted, and cheerful personality recover more quickly from total joint replacement surgery than those with different personality traits.25 Conversely, melancholic, introverted, and pessimistic individuals take longer to recover.26 These findings align with our own. During the questionnaire survey, it was noted that patients with cheerful personalities had milder symptoms, suggesting that personality traits significantly impact postoperative recovery.
At a conference on breast cancer postoperative recovery, research highlighted that personality traits influence patients’ expectations of postoperative outcomes, psychological status, and need for social support, thus affecting recovery. This supports the findings of our study. The results also emphasize the importance of increased psychological counselling and communication for introverted patients to decrease severe symptom burdens after surgery.
Impact of PCA Used on Postoperative Symptom Clusters in Lung Cancer Patients
Our study examined the effect of PCA used on postoperative symptom clusters in lung cancer patients. Among the 163 patients who used PCA after surgery, 58.3% reported a lower incidence of symptoms, while 41.7% experienced a higher incidence. In comparison, of the 278 patients who did not use PCA, 71.7% reported a lower incidence of symptoms, and 28.3% experienced a higher incidence. This indicates a greater occurrence of nausea and vomiting among patients using PCA, leading some to discontinue their use.
Further analysis revealed that side effects such as nausea and vomiting are common with the anesthetics used in these pumps. Additionally, female patients had a higher incidence of these side effects compared to male patients,27 consistent with previous studies noting gender differences in postoperative nausea and vomiting rates. As a result, we recommend that anesthesiologists consider reducing the use of analgesic pumps in female patients who are prone to high rates of nausea and vomiting. Alternative pain management strategies, such as oral or intravenous analgesics, should be considered to reduce these side effects, thereby improving postoperative functional status.
Correlation Between Postoperative Functional Status (KPSS) and Symptom Clusters in Lung Cancer Patients
Our study’s analysis shows that postoperative functional status, as measured by the Karnofsky Performance Status Scale (KPSS) score, is inversely related to high-symptom levels in lung cancer patients. Postoperative fear of movement (kinesiophobia) is positively associated with high-symptom levels; all high-symptom levels are negatively associated with functional status (all P < 0.05).
Following lung cancer surgery, patients may experience symptoms such as pain, dyspnea, and fatigue, which can restrict their daily activities and reduce their functional status. Additionally, anxiety and depression often affect postoperative patients, further hindering their recovery process and functional status. This study suggests a significant link between postoperative physical activity levels and functional status, kinesiophobia, self-efficacy, and quality of life (P < 0.05).3,28 Notably, patients with lower physical activity levels reported higher kinesiophobia and poorer quality of life.
Therefore, our findings suggest that postoperative symptom clusters, including pain levels, significantly impact functional recovery. Effective pain management strategies, such as multimodal analgesia, could further optimize postoperative outcomes. The negative impact of high-symptom levels can lead to a decline in patients’ functional status. This highlights the importance of addressing and managing high-symptoms in postoperative care for lung cancer patients to improve their quality of life and encourage early recovery.
Limitation
There are limitations of our study. First, this study did not specifically analyze differences in pathological types between male and female patients, which could be explored in future research. Second, the study uses convenience sampling, which may introduce selection bias, and it is a recommendation for future probability-based sampling studies. Third, this study was conducted in only one hospital, larger cohorts with detailed clinicopathological data is need in future.
Conclusions
This study highlighted the interconnection of postoperative symptom clusters in lung cancer patients. According to the LCM model, patients were categorized into high and low-symptom groups. Those in the high-symptom group experienced greater physiological and psychological distress than those in the low-symptom group. Postoperative symptom cluster assessment provides a scientific basis for developing effective management strategies, which may improve functional recovery and long-term outcomes in lung cancer patients. Thus, healthcare providers are advised to manage these symptom clusters to improve patients’ functional status and quality of life.
Ethics Statement
This study was approved by the Ethics Committee of Zhongshan Hospital, Xiamen University (Ethics No.: XMZSYYKY 2023-050). All participants provided informed consent. This study is in line with the Helsinki Declaration of the World Medical Association.
Funding
This work was supported by ResearchProject of Xiamen Nursing Society (No. XMSHLXH2302) and Health and Medical Guidance Project of Xiamen Municipal Science and Technology Bureau (No. 3502Z20244ZD1079).
Disclosure
The authors declare no competing interests in this work.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Yuan MW, Wang HH, Duan RF, et al. Analysis on cancer incidence and mortality attributed to human papillomavirus infection in China, 2016. Zhonghua Liu Xing Bing Xue Za Zhi. 2022;43(5):702–708. doi:10.3760/cma.j.cn112338-20211010-00777
3. Liang Y, Jing P, Gu Z, et al. Application of the patient-reported outcome-based postoperative symptom management model in lung cancer: a multicenter randomized controlled trial protocol. Trials. 2024;25(1):130. doi:10.1186/s13063-024-07963-8
4. Thavarajah N, Chen E, Zeng L, et al. Symptom clusters in patients with metastatic cancer: a literature review. Expert Rev Pharmacoecon Outcomes Res. 2012;12(5):597–604. doi:10.1586/erp.12.41
5. Liao J, Wang Y, Dai W, et al. Profiling symptom burden and its influencing factors at discharge for patients undergoing lung cancer surgery: a cross-sectional analysis. J Cardiothorac Surg. 2022;17(1):229. doi:10.1186/s13019-022-01974-9
6. Miaskowski C, Dodd M, Lee K. Symptom clusters: the new frontier in symptom management research. J Natl Cancer Inst Monogr. 2004;32(32):17–21. doi:10.1093/jncimonographs/lgh023
7. Ju X, Bai J, She Y, et al. Symptom cluster trajectories and sentinel symptoms during the first cycle of chemotherapy in patients with lung cancer. Eur J Oncol Nurs. 2023;63:102282. doi:10.1016/j.ejon.2023.102282
8. Tran TO, Lam LHT, Le NQK. Hyper-methylation of ABCG1 as an epigenetics biomarker in non-small cell lung cancer. Funct Integr Genomics. 2023;23(3):256. doi:10.1007/s10142-023-01185-y
9. Tran TO, Vo TH, Le NQK. Omics-based deep learning approaches for lung cancer decision-making and therapeutics development. Brief Funct Genomics. 2024;23(3):181–192. doi:10.1093/bfgp/elad031
10. Kamata A, Kara Y, Patarapichayatham C, Lan P. Evaluation of analysis approaches for latent class analysis with auxiliary linear growth model. Front Psychol. 2018;9:130. doi:10.3389/fpsyg.2018.00130
11. Preacher KJ, Kelley K. Effect size measures for mediation models: quantitative strategies for communicating indirect effects. Psychol Methods. 2011;16(2):93–115. doi:10.1037/a0022658
12. Ohguri T, Yahara K, Moon SD, et al. Postoperative radiotherapy for incompletely resected non-small cell lung cancer: clinical outcomes and prognostic value of the histological subtype. J Radiat Res. 2012;53(2):319–325. doi:10.1269/jrr.11082
13. De Das S, Vranceanu AM, Ring DC. Contribution of kinesophobia and catastrophic thinking to upper-extremity-specific disability. J Bone Joint Surg Am. 2013;95(1):76–81. doi:10.2106/JBJS.L.00064
14. Woby SR, Roach NK, Urmston M, Watson PJ. Psychometric properties of the TSK-11: a shortened version of the Tampa scale for kinesiophobia. Pain. 2005;117(1–2):137–144. doi:10.1016/j.pain.2005.05.029
15. Rozmiarek M, Grajek M, Malchrowicz-Mosko E, et al. Polish adaptation of the modified Tampa scale of kinesiophobia for fatigue (TSK-F) and the revision of the Tampa scale in terms of pain for cancer patients. Int J Environ Res Public Health. 2022;19(19):12730. doi:10.3390/ijerph191912730
16. Friendlander AH, Ettinger RL. Karnofsky performance status scale. Spec Care Dentist. 2009;29(4):147–148. doi:10.1111/j.1754-4505.2009.00088.x
17. Edwards D, de Abreu GC, Labouriau R. Selecting high-dimensional mixed graphical models using minimal AIC or BIC forests. BMC Bioinf. 2010;11(1):18. doi:10.1186/1471-2105-11-18
18. Burel J, El Ayoubi M, Baste JM, et al. Surgery for lung cancer: postoperative changes and complications-what the radiologist needs to know. Insights Imaging. 2021;12(1):116. doi:10.1186/s13244-021-01047-w
19. Zhang R, Yang Z, Shen X, Xia L, Cheng Y. Preoperative physical dysfunction characteristics and influence factors among elderly patients with early lung cancer: a latent class analysis. J Multidiscip Healthc. 2024;17:1743–1754. doi:10.2147/JMDH.S455669
20. Ma J, Li X, Zhao S, Wang J, Zhang W, Sun G. Robot-assisted thoracic surgery versus video-assisted thoracic surgery for lung lobectomy or segmentectomy in patients with non-small cell lung cancer: a meta-analysis. BMC Cancer. 2021;21(1):498. doi:10.1186/s12885-021-08241-5
21. Shah NJ, Leis A, Kheterpal S, Englesbe MJ, Kumar SS. Association of intraoperative hyperglycemia and postoperative outcomes in patients undergoing non-cardiac surgery: a multicenter retrospective study. BMC Anesthesiol. 2020;20(1):106. doi:10.1186/s12871-020-01022-w
22. Riveros Perez E, Kerko R, Lever N, White A, Kahf S, Avella-Molano B. Operating room relay strategy for turnover time improvement: a quality improvement project. BMJ Open Qual. 2022;11(3):e001957. doi:10.1136/bmjoq-2022-001957
23. Pasquer A, Ducarroz S, Lifante JC, Skinner S, Poncet G, Duclos A. Operating room organization and surgical performance: a systematic review. Patient Saf Surg. 2024;18(1):5. doi:10.1186/s13037-023-00388-3
24. Wertli MM, Rasmussen-Barr E, Held U, Weiser S, Bachmann LM, Brunner F. Fear-avoidance beliefs-a moderator of treatment efficacy in patients with low back pain: a systematic review. Spine J. 2014;14(11):2658–2678. doi:10.1016/j.spinee.2014.02.033
25. Zeng C, Koonce RC, Tavel HM, et al. Pre-operative predictors for discharge to post-acute care facilities after total knee arthroplasty. J Arthroplasty. 2022;37(1):31–38e32. doi:10.1016/j.arth.2021.09.019
26. Taurisano P, Abbatantuono C, Verri V, et al. Pre-surgery supportive and goal-oriented strategies are associated with lower post-surgery perceived distress in women diagnosed with breast cancer. BMC Psychol. 2022;10(1):2. doi:10.1186/s40359-021-00714-3
27. Yang Y, Wu J, Li H, et al. Prospective investigation of intravenous patient-controlled analgesia with hydromorphone or sufentanil: impact on mood, opioid adverse effects, and recovery. BMC Anesthesiol. 2018;18(1):37. doi:10.1186/s12871-018-0500-1
28. Goff AJ, Jones LE, Lim CJ, Tan BY. A cross sectional study exploring the relationship of self-reported physical activity with function, kinesiophobia, self-efficacy and quality of life in an Asian population seeking care for knee osteoarthritis. BMC Musculoskelet Disord. 2024;25(1):74. doi:10.1186/s12891-024-07181-y
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

