Back to Journals » Psychology Research and Behavior Management » Volume 18
Associations Between Psychosocial Influence, Positive Thinking, and Vaccine Attitudes in Patients with Schizophrenia During the COVID-19 Pandemic
Authors Li DJ, Wang WC , Chou FHC , Hsu ST, Hsieh KY, Lin GG, Wu PJ , Liu CL, Wu HC, Huang JJ
Received 10 January 2025
Accepted for publication 22 May 2025
Published 10 June 2025 Volume 2025:18 Pages 1307—1318
DOI https://doi.org/10.2147/PRBM.S516814
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Bao-Liang Zhong
Dian-Jeng Li,1,2,* Wen-Chun Wang,3,* Frank Huang-Chih Chou,4 Su-Ting Hsu,5 Kuan-Ying Hsieh,6,7 Guei-Ging Lin,8 Pei-Jhen Wu,8 Chin-Lien Liu,8 Hui-Ching Wu,9 Joh-Jong Huang10,11
1Department of Addiction Science, Kaohsiung Municipal Kai-Syuan Psychiatric Hospital, Kaohsiung, Taiwan; 2Department of Nursing, Meiho University, Pingtung, Taiwan; 3Department of Forensic Psychiatry, Kaohsiung Municipal Kai-Syuan Psychiatric Hospital, Kaohsiung, Taiwan; 4Superintendent Office, Kaohsiung Municipal Kai-Syuan Psychiatric Hospital, Kaohsiung, Taiwan; 5Department of Community Psychiatry, Kaohsiung Municipal Kai-Syuan Psychiatric Hospital, Kaohsiung, Taiwan; 6Department of Child and Adolescent Psychiatry, Kaohsiung Municipal Kai-Syuan Psychiatric Hospital, Kaohsiung, Taiwan; 7Department of Physical Therapy, I-Shou University, Kaohsiung, Taiwan; 8Department of Nurse, Kaohsiung Municipal Kai-Syuan Psychiatric Hospital, Kaohsiung, Taiwan; 9Department of Social Work, National Taiwan University, Taipei, Taiwan; 10Department of Gerontological and Long-Term Care Business, Fooyin University, Kaohsiung, Taiwan; 11Department of Family Medicine, Kaohsiung Medical University Hospital, Kaohsiung, Taiwan
*These authors contributed equally to this work
Correspondence: Joh-Jong Huang, Department of Gerontological and Long-Term Care Business, Fooyin University, 151 Jinxue Road, Daliao District, Kaohsiung City, 83102, Taiwan, Tel +886 7243327, Fax +886 7152300, Email [email protected]
Background: The rate of vaccination is lower in patients with schizophrenia than in the general population, and therefore, further investigation into the psychosocial impact of COVID-19 on these patients and their vaccine attitudes is warranted. In this study, we investigated factors influencing vaccine attitudes in patients with schizophrenia and explored the interactions among these factors.
Methods: Cross-sectional, self-report surveys were conducted among Taiwanese patients with schizophrenia to collect data on vaccine attitudes and associated variables. Our sample was drawn from the largest psychiatric specialty hospital in Taiwan. As of December 1, 2022, 88% of the Taiwanese population had received at least two doses of the COVID-19 vaccine. Factors influencing vaccine attitudes and potential moderators were investigated through correlation analyses, hierarchical regression, and Hayes’ Process Macro.
Results: This study included 457 patients. Our results revealed that social anxiety and social desirability were respectively positively and negatively correlated with vaccine attitudes. Positive thinking moderated the overall effect of social influence on vaccine attitudes. Low levels of positive thinking intensified the effect of social influence on vaccine hesitancy.
Conclusion: This study clarified the association of social influence with vaccine attitudes and the moderating effect of positive thinking on this association. Reputable medical centers can enhance patients’ confidence in vaccination policies and foster positive thinking to increase vaccine acceptance among patients with schizophrenia.
Keywords: schizophrenia, COVID-19, Societal Influences Survey Questionnaire, vaccine attitudes, positive thinking, psychosocial impact
Graphical Abstract:

Introduction
After its emergence in late 2019, COVID-19 considerably affected individuals’ mental health by imposing a substantial psychological burden on the general population,1 health-care workers,2,3 and patients with mental disorders.4–7 For example, patients with schizophrenia faced multidimensional effects of COVID-19.
The coronavirus pandemic has had a significant impact on both health and social systems8 and it could potentially alter the health conditions of patients with schizophrenia.8 Because of their susceptibility to respiratory infections,9 these patients exhibited a high risk of COVID-19-related mortality.10 Schizophrenia was characterized by a range of symptoms commonly classified into positive (eg, hallucinations, delusions, disorganized speech, catatonic behavior), negative (eg, blunted affect, alogia, anhedonia, avolition, social withdrawal), and cognitive symptoms (eg, impaired attention, working memory, and executive functioning).11 In addition, core disturbances in self-experiences—such as disrupted self-boundaries, thought insertion, derealization, and loss of agency—were identified as central features of the disorder.12 These combined impairments could compromise an individual’s ability to understand, evaluate, and act on health-related information. As shown in prior research, individuals with psychotic disorders were among the least likely to receive vaccines, likely due to substantial impairments in decisional capacity that affected risk perception, trust, and motivation to engage in preventive health behaviors.13
Patients with schizophrenia experienced extensive psychological stress during the pandemic attributable to factors such as increased distress, sleep disturbances, depression, and anxiety due to quarantine measures.14 Prolonged social isolation and widespread COVID-19-related misinformation likely contributed to the onset of psychotic symptoms in these patients.15 Psychotic relapses may result from environmental factors, poor treatment adherence, and inflammatory response due to COVID-19.16 A study demonstrated that COVID-19 led to severe psychotic episodes and poor prognoses of psychotic disorder.17 In summary, COVID-19 imposed an appreciable psychological burden on individuals that was attributable to both infection and social isolation.
In addition to the aforementioned burden, COVID-19’s psychosocial impact and patients’ vaccine attitudes are key concerns in individuals with schizophrenia. Social distancing and other preventive measures implemented during the pandemic negatively affected patients with schizophrenia. For example, they exhibited poorer social interactions than did the general population.18 Social distancing and isolation further imposed a psychological burden on these patients.14,19 Obtaining COVID-19-related information from the Internet, television, or radio exerted both positive and negative effects on individuals with schizophrenia. A study involving health-care workers revealed a significant association between receiving COVID-19-related information from multiple sources and having high confidence levels.20 Another study suggested that acquiring COVID-19-related information enhanced individuals’ intention to self-isolate.21 However, excessive exposure to pandemic-related news exacerbated anxiety and stress in the general population.22 Among patients with schizophrenia, gathering COVID-19-related information was significantly associated with psychological distress and sleep disturbance.5
Negative vaccination attitudes are a crucial problem in patients with schizophrenia. However, both preventive measures and vaccination were required to reduce the risk of long COVID during the pandemic.23 A meta-analysis indicated that patients with schizophrenia had an elevated risk of COVID-19-related mortality.24 Notably, antipsychotics and other psychotropic medications can interact with Paxlovid, a common antiviral medicine for COVID-19.25 Regarding vaccination, the rates of receiving initial and booster doses were lower in patients with schizophrenia than in the general population.26,27 Such differences are especially pronounced among individuals with schizophrenia who are older or male.28 Patients with schizophrenia experienced lower rates of COVID-19 infection but higher mortality, largely due to low vaccination uptake.29 This may be attributed to the fact that individuals with psychiatric disorders—especially those with schizophrenia or related conditions—were more likely to refuse the COVID-19 vaccine.30 Thus, researchers should investigate these patients’ willingness to be vaccinated and the psychosocial impact COVID-19 had on this population.
The multidimensional effects of COVID-19 on patients with schizophrenia are dependent on COVID-19’s psychosocial impact5 and patients’ motivation to receive a vaccination.31 The swift development of COVID-19 vaccines has evolved into a politicized issue, drawing significant attention from both mainstream and social media.32 Factors such as the accelerated timeline, concerns over potential side effects,33 and individuals’ political beliefs may all influence their willingness to receive the vaccine.34 This indicated that attitudes toward vaccination were shaped by a complex process. However, few studies have comprehensively explored the determinants of vaccine attitudes in these patients. The interactions between psychological burden, psychosocial impact, and vaccine attitudes remain unclear. The rate of COVID-19-related mortality was higher in patients with schizophrenia than in the general population,10 and therefore, the factors influencing vaccine attitudes in these patients should be identified. Thus, we conducted this cross-sectional study to identify key factors influencing vaccine attitudes in patients with schizophrenia. Our objectives were to investigate the association between COVID-19’s psychosocial impact and patients’ vaccine attitudes and identify factors moderating this association.
Methods
Study Cohort and Ethical Considerations
This study was conducted using data from an ongoing cross-sectional survey for measuring the multidimensional effects of COVID-19 on patients with mental disorders, health-care workers, and the general population.1–7,35–38 Patients with schizophrenia were recruited through printed advertisements posted in public areas of Kaohsiung Municipal Kai-Syuan Psychiatric Hospital (KSPH), the largest psychiatric specialty hospital in Taiwan, and its affiliated institutes as well as through online advertisements shared on social media platforms. Cross-sectional surveys were conducted using paper-and-pencil questionnaires. For this study, we used data corresponding to the period from October 2022 to March 2023, which coincided with the third wave of COVID-19 in Taiwan. As of December 1, 2022, 88% of people in Taiwan had received at least two doses of the COVID-19 vaccine.39 We included patients who received a psychiatrist-made diagnosis of schizophrenia, were hospitalized in either the acute or the chronic ward of KSPH, could understand the study objectives and follow instructions from research assistants, were aged ≥20 years, and provided informed consent before the survey. Patients were excluded if they exhibited substantial cognitive impairments that could interfere with their ability to complete the questionnaires. The study protocol was approved by the Institutional Review Board of KSPH (KSPH-2020-03, KSPH-2021-08, and KSPH-2023-04). We conducted these studies in accordance with the latest revision of national legal requirements (Human Subjects Research Act, Taiwan) and complied with the Declaration of Helsinki. Each participant provided informed consent before participating.
Study Variables
Vaccination Attitudes
The Vaccination Attitude Examination (VAX) scale was used to assess patients’ vaccine attitudes. This scale was reported to exhibit strong validity and reliability.40 The Chinese version of the VAX was reported to exhibit acceptable reliability.35 The VAX comprises 12 items, including “Although most vaccines appeared to be safe, problems might have remained undiscovered” and “Authorities promoted vaccination for financial gain, not for people’s health.” Each response was scored on a 6-point Likert-type scale, with end points ranging from 1 (“strongly agree”) to 6 (“strongly disagree”). A higher overall score on VAX indicated stronger vaccine hesitancy (Supplementary Table S1).
Social Anxiety, Social Desirability, and Social Information
Three subscales of the Societal Influences Survey Questionnaire (SISQ)—social anxiety, social desirability, and social information—were used to measure the psychosocial impact of COVID-19. The SISQ has been reported to exhibit strong validity and reliability.1,37 It comprises 15 items, which constitute 5 categories: social distance, social anxiety, social desirability, social information, and social adaptation. Each response is scored on a 4-point Likert scale, with end points ranging from 1 (“never”) to 4 (“often”). The social anxiety subscale comprises 4 items, including “I worried about the pandemic affecting my work” and “I felt anxious or fearful because of the pandemic.” A higher total score on this subscale indicates a higher level of anxiety due to external factors during the COVID-19 pandemic. The social desirability subscale comprises 3 items, including “I believe that self-management of health can help control the spread of COVID-19.” A higher score indicates a higher level of confidence in and a higher level of adherence to government policies regarding COVID-19. The social information subscale comprises 2 items, including “I constantly sought the latest pandemic news through television, the computer, or the phone.” A higher score indicates a higher level of inclination to seek COVID-19-related information (Supplementary Table S1).
Positive Thinking
Lo’s Healthy and Happy Lifestyle Scale (LHHLS) was used to measure positive thinking. LHHLS evaluates well-being in relation to mental health and lifestyle. It was reported to exhibit acceptable reliability and good validity.36 LHHLS comprises 2 subscales: self-efficacy and positive thinking. Positive thinking is assessed using 6 items, including “I am optimistic about my future” and “I feel that life is carefree.” Each response is scored on a 5-point Likert scale, with end points ranging from 1 (“never”) to 5 (“always”). Respondents are asked to evaluate their feelings over the previous 2 weeks. A higher score on LHHLS indicates a higher level of positive thinking (Supplementary Table S1).
Demographic Characteristics
The following demographic data were collected from the patients: age (yr), sex (male or female), education level (high school or below, college, and graduate school or above), holding religious beliefs (yes or no), and history of comorbidities (yes or no). Vaccine acceptance tends to be lower in younger individuals, women, and individuals with lower education levels than in others.41 Religious beliefs influence vaccine acceptance and vaccine hesitancy.42 Furthermore, the preexistence of comorbidities influences individuals’ willingness to be vaccinated.43
Statistical Analysis
Data were analyzed using SPSS (version 27.0; IBM Corporation, Armonk, NY, USA). Descriptive statistics were used for demographic characteristics and quantitative variables. We employed several analytical methods to examine how the psychosocial impact of COVID-19—specifically social anxiety, social desirability, and social information—affects patients’ vaccine attitudes, and to assess the moderating role of positive thinking in these relationships. Correlation analyses, such as Pearson correlation analysis and point-biserial correlation analysis and hierarchical regression were performed to identify factors associated with vaccine attitudes. To assess the moderating effect of positive thinking, we first conducted regression analyses with social anxiety, social desirability, and social information as independent variables predicting vaccine attitudes. We then introduced positive thinking into the model as a moderating variable. Finally, we analyzed the moderating effect of the interaction between psychosocial impact and positive thinking on vaccine attitudes. Adjusted R2, ΔR2, and ΔF values were calculated to assess model fit. Once the interaction terms between psychosocial impact variables and positive thinking showed a significant effect on vaccine attitudes, the moderating effect of positive thinking was further analyzed using Hayes’ PROCESS Macro. This analysis aimed to examine the associations between psychosocial impact and vaccine attitudes among patients with varying levels of positive thinking.44
Results
This study included 457 patients with schizophrenia (mean age: 57.16 ± 11.26; men: 61.1%). Among the patients, 91.2% had a high school education or below, 51.4% held religious beliefs, and 36.1% had comorbidities. Table 1 presents the demographic characteristics of the study cohort. The results of Pearson correlation analysis (Table 2) indicated that vaccine attitudes were positively correlated with social anxiety (r(455) =0.12; p <0.05) but negatively correlated with social desirability (r(455) = −0.16; p <0.01).
 |
Table 1 Demographic Characteristics of the Study Cohort (N = 457) |
 |
Table 2 Correlation Matrix for the Study Variables |
Hierarchical regression was performed to analyze the direct and moderating effects of the study variables on vaccine attitudes. In the first step, the statistical model was adjusted for demographic characteristics (eg, age, sex, education level, religious beliefs, and comorbidities; adjusted R² =0.01). In the second step, the model was fitted with social anxiety, social desirability, and social information (ΔR² =0.11; ΔF = 19.68; p <0.001). Social anxiety was found to be positively associated with vaccine attitudes (β = 1.36; p <0.001), whereas social desirability was negatively associated with them (β = −1.25; p <0.001). In the third step, positive thinking was introduced into the model (ΔR² =0.15; ΔF = 19.83; p <0.001). This variable was positively associated with vaccine attitudes (β = 0.35; p <0.001). In the final step, interaction terms were incorporated into the model (ΔR² =0.24; ΔF = 17.78; p <0.001). The results (Table 3) indicated the presence of moderating effects on the direct associations of social anxiety (β = 0.14; p <0.001), social desirability (β = −0.12; p <0.001), and social information (β = −0.18; p <0.01) with vaccine attitudes.
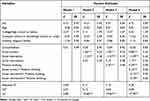 |
Table 3 Predictors of and Moderating Effects on Vaccine Attitudes Analyzed Through Hierarchical Regression |
As presented in Figure 1, social anxiety induced vaccine hesitancy more strongly in patients with a low level of positive thinking (β = 2.01; t = 6.80; p <0.001) than in those with a high level of positive thinking (β = 1.32; t = 5.53; p <0.001). As indicated in Figure 2, social desirability reduced vaccine hesitancy more strongly in patients with a high level of positive thinking (β = −2.07; t = −1.18; p <0.01) than in those with a low level of positive thinking (β = −0.76; t = −3.26; p <0.001). Among patients with a low level of positive thinking, those with a higher tendency to seek COVID-19-related information developed stronger vaccine hesitancy (β = 2.26; t = 4.22; p <0.001; Figure 3).
 |
Figure 1 Moderating effect of positive thinking on the direct association between social anxiety and vaccine attitudes. |
 |
Figure 2 Moderating effect of positive thinking on the direct association between social desirability and vaccine attitudes. |
 |
Figure 3 Moderating effect of positive thinking on the direct association between social information and vaccine attitudes. |
Discussion
We analyzed the effect of social influence on the vaccine attitudes of patients with schizophrenia during the COVID-19 pandemic. Our findings revealed a positive correlation between social anxiety and vaccine attitudes but a negative correlation between social desirability and vaccine attitudes. The psychological effects of pandemic-related changes in patients’ external environment—for example, occupational changes, economic changes, and social distancing—were measured using the social anxiety subscale of SISQ.1 The fear of negative changes in social status and financial situation likely reduced vaccine acceptance.45
Social desirability reflected patients’ levels of trust in and compliance with pandemic policies. Studies have reported negative vaccine attitudes to be associated with conspiracy beliefs and vaccine skepticism.46,47 Consequently, trust in government policies might mitigate vaccine hesitancy. Our findings align with those of other studies. External factors such as social anxiety and social desirability partially represented the levels of trust the patients had in government policies. Higher levels of confidence in these policies were correlated with higher levels of vaccine acceptance.48–50 A study demonstrated that trust in health-care providers improved vaccine acceptance.51 Therefore, during pandemics, fostering trust in health-care providers and communicating accurate preventive measures may improve patients’ adherence to public health guidelines.
We identified no significant association between patients’ tendency to seek COVID-19-related information and vaccine attitudes. In line with our findings, a study revealed that seeking information did not necessarily influence individuals’ vaccine attitudes.52 Rather, the information source and personal factors shaped individuals’ willingness to be vaccinated. The levels of vaccine acceptance significantly differed between individuals receiving vaccine-related information from medical institutions or official media and those receiving information from unregulated platforms or social media.53–56 Because our sample comprised patients with schizophrenia, they likely had more opportunities to interact with health-care professionals than did the general population. Consequently, they were more likely than the general population to receive accurate information on vaccines. However, whether exposure to accurate information improved their vaccine attitudes remains to be clarified. Receiving information from various sources might have clouded patients’ vaccine attitudes and increased cognitive complexity.57
Effect of the Interaction Between Positive Thinking and Social Influence on Vaccine Attitudes
We identified no association between positive thinking and vaccine attitudes. However, further analysis performed using positive thinking as a moderator of the association between social influence and vaccine attitudes revealed that positive thinking moderated the associations of social anxiety, social desirability, and social information with vaccine attitudes. Specifically, among patients with a high level of positive thinking, social anxiety weakly induced vaccine hesitancy. Furthermore, in these patients, social desirability strongly reduced vaccine hesitancy. These findings suggest that the development of vaccine hesitancy is a complex process influenced by multiple factors. Although positive thinking did not directly affect vaccine hesitancy, it played a moderating role in shaping vaccine attitudes.
Negative thoughts often trigger a chain reaction, leading to further negativity. Positive thinking, which involves developing uplifting emotions and constructive habits, is essential for breaking the cycle of negativity. Evidence suggests that positive thinking can help with managing stress, anxiety, and other mental health problems.58 It was reported to mitigate the role of stress in developing mental health disorders during the COVID-19 pandemic.59 Positive thinking can improve mental health during public health crises.60 Although concerns regarding the social and economic consequences of crises can markedly increase stress, positive thinking can mitigate the effects of concerns and stress.61 Our study provides empirical evidence of the moderating effect of positive thinking on stress due to external factors and thus vaccine hesitancy. To improve patients’ compliance with preventive measures implemented during pandemics, positive thinking should be fostered through appropriate health education and training.
Although this study indicated that a strong desire to receive COVID-19-related information had no direct association with vaccine attitudes, actively seeking such information increased vaccine hesitancy in patients with a low level of positive thinking. The level of enthusiasm in acquiring pandemic-related information significantly influenced vaccine attitudes. A complete lack of interest in or avoidance of pandemic-related news was associated with vaccine hesitancy. Among patients who actively sought pandemic-related information, vaccine attitudes were influenced by the information source (eg, official media and social media) or personal factors (conspiracy beliefs).45,52 We discovered that positive thinking exerted moderating effects on relevant information seeking and its association with vaccine attitudes. Individuals not practicing positive thinking can be trapped in a vicious cycle of negativity under stress.58 Further studies are required to clarify the causal relationship between negative emotions and active pursuit of pandemic-related information.
On the basis of our findings, we recommend enhancing patients’ trust in government policies and encouraging patients to seek relevant information from credible sources (health-care providers) to improve their compliance with preventive measures. We further recommend promoting positive thinking through targeted training or health education adherence to preventive measures during pandemics. These efforts would increase the overall effectiveness of public health interventions during crises.
Positive thinking in individuals with schizophrenia is often impaired by negative symptoms, low motivation, and cognitive distortions. However, growing evidence supports the use of interventions such as positive psychology exercises,62 recovery-oriented approaches,63,64 mindfulness-based programs,65,66 peer support and recovery narratives,67,68 and exercise interventions69 to enhance optimism, emotional resilience, and engagement in treatment. These strategies are particularly effective during periods of symptom stability and may contribute to improved quality of life and long-term recovery.
Limitations
This study has some limitations. First, it was conducted at a single center, which may limit the applicability of our conclusions to different regions or environments. Second, the exclusion of patients with major mental illnesses, despite research indicating a strong comorbid association between schizophrenia and other psychiatric disorders, may reduce the relevance of our findings in real-world contexts. This exclusion narrowed the scope of this study, reducing its applicability to populations in which mental health comorbidities are prevalent and thus limiting our understanding of the broader patient population affected by schizophrenia. In the future, multicenter studies involving a diverse range of patients should be conducted to validate our findings and enhance their real-world relevance. Third, we lacked information on the specific platforms the patients used to obtain pandemic-related information, which limited our ability to precisely analyze the association between information seeking and vaccine attitudes. Finally, the absence of a formal assessment of symptom severity (eg, PANSS, BPRS, or CGI) should be acknowledged as a study limitation. Considering ethical requirements and the inherent limitations of survey research research, we were unable to include clinical evaluations of participants’ psychiatric symptoms. All participants were able to independently complete the questionnaires, which suggests that they did not exhibit severe cognitive or symptomatic impairments. However, the lack of standardized severity data limits our ability to control for potential confounding effects arising from symptom heterogeneity. Future studies may benefit from incorporating validated clinical scales to better account for these variables.
Conclusion
We investigated the association between COVID-19’s psychosocial impact and vaccine attitudes in hospitalized patients with schizophrenia as well as the moderating effect of positive thinking on this association. Our findings indicated that social anxiety, trust in government policies, and adherence to preventive measures significantly influenced patients’ vaccine acceptance during the pandemic. Positive thinking moderated the association between patients’ exposure to pandemic-related information and their vaccine attitudes. To improve patients’ compliance with preventive measures, their trust in government policies should be enhanced, and they should be encouraged to seek information from reliable sources, such as health-care providers. Furthermore, positive thinking should be fostered through targeted training and health education to improve patients’ adherence to pandemic guidelines.
Highlights
- Social anxiety increases vaccine hesitancy in patients with schizophrenia.
- Social desirability reduces vaccine hesitancy in patients with schizophrenia.
- Positive thinking moderates how social influence affects patients’ vaccine attitudes.
- Enhancing trust in policies and promoting credible information-seeking may increase vaccine acceptance in schizophrenia patients.
- Encouraging positive thinking may boost preventive adherence and public health impact during pandemics.
Data Sharing Statement
The data presented in the manuscript are available from the corresponding author (Dr. Joh-Jong Huang, email: [email protected]) upon reasonable request.
Ethics Approval and Consent to Participate
Data were derived through a series of investigations. The study protocol was approved by the Institutional Review Board of Kaohsiung Municipal Kai-Syuan Psychiatric Hospital (permit numbers: KSPH-2020-03, KSPH-2021-08, and KSPH-2023-04). All procedures adhered to the current revision of the national legal requirements for human research (Human Subjects Research Act, Taiwan). Informed consent was obtained from all patients before their participation.
Acknowledgments
Dian-Jeng Li and Wen-Chun Wang are co-first authors for this study. We thank all the participants in this study and support from the Department of Health, Kaohsiung City and Kaohsiung Municipal Kai-Syuan Psychiatric Hospital.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study received no financial support from any funding agency in the public, private, or not-for-profit sector.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Li D-J, Kao W-T, Shieh V, Chou FH-C, Lo H-WA. Development and implementation of societal influences survey questionnaire (SISQ) for peoples during COVID-19 pandemic: a validity and reliability analysis. Int J Environ Res Public Health. 2020;17(17):6246. doi:10.3390/ijerph17176246
2. Li DJ, Huang JJ, Hsu ST, et al. Characteristics of sleep disturbance and comparison across three waves of the COVID-19 pandemic among healthcare workers. Psychiatry Invest. 2024;21(8):838–849. doi:10.30773/pi.2024.0006
3. Li D-J, Wu H-C, Chou FH-C, et al. The social and mental impact on healthcare workers: a comparative and cross-sectional study during two waves of the COVID-19 pandemic in Taiwan. Medicine. 2022;101(42). doi:10.1097/MD.0000000000031316
4. Hsieh K-Y, Kao W-T, Chou FH-C, et al. Predictors for probable posttraumatic stress disorder among outpatients with psychiatric disorders and their caregivers during the COVID-19 pandemic: a cross-sectional study in Taiwan. Taiwan J Psychiatry. 2021;35(1):32–39. doi:10.4103/TPSY.TPSY_7_21
5. Li D-J, Chou L-S, Chou FH-C, et al. COVID-related psychological distress fully mediates the association from social impact to sleep disturbance among patients with chronic schizophrenia. Sci Rep. 2021;11(1):16524. doi:10.1038/s41598-021-96022-2
6. Li D-J, Hsu S-T, Chou FH-C, et al. Predictors for depression, sleep disturbance, and subjective pain among inpatients with depressive disorders during the COVID-19 pandemic: a cross-sectional study. Int J Environ Res Public Health. 2021;18(12):6523. doi:10.3390/ijerph18126523
7. Li D-J, Huang -J-J, Hsu S-T, et al. The impact of psychological burdens and vaccine worries on confidence and adherence to governmental policies against COVID-19 among patients with substance use disorder: a cross-sectional study in Taiwan. Neuropsychiatr Dis Treat. 2024;Volume 20:597–606. doi:10.2147/NDT.S453238
8. Ms KU. Coronary blindness: desensitization after excessive exposure to coronavirus-related information. Health Policy Technol. 2022;11(3):100625. doi:10.1016/j.hlpt.2022.100625
9. Vadamalai K, Sanchez‐Tejera D, Bress J, Mustafa SS. Screening for humoral immunodeficiency in patients with community-acquired pneumonia. J Hospital Med. 2019;14(1):33–37. doi:10.12788/jhm.3106
10. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi:10.1016/S0140-6736(20)30566-3
11. Millan MJ, Fone K, Steckler T, Horan WP. Negative symptoms of schizophrenia: clinical characteristics, pathophysiological substrates, experimental models and prospects for improved treatment. Eur Neuropsychopharmacol. 2014;24(5):645–692. doi:10.1016/j.euroneuro.2014.03.008
12. Parnas J. A disappearing heritage: the clinical core of schizophrenia. Schizophr Bull. 2011;37(6):1121–1130. doi:10.1093/schbul/sbr081
13. Jeste DV, Depp CA, Palmer BW. Magnitude of impairment in decisional capacity in people with schizophrenia compared to normal subjects: an overview. 2006.
14. Liu X, Lin H, Jiang H, et al. Clinical characteristics of hospitalised patients with schizophrenia who were suspected to have coronavirus disease (COVID-19) in Hubei Province, China. General Psychiatry. 2020;33(2):e100222. doi:10.1136/gpsych-2020-100222
15. Barlati S, Nibbio G, Vita A. Schizophrenia during the COVID-19 pandemic. Curr Opin Psychiatry. 2021;34(3):203–210. doi:10.1097/YCO.0000000000000702
16. Kowalski K, Misiak B. Schizophrenia and the COVID-19 pandemic: a narrative review from the biomedical perspective. Revista de Psiquiatría y Salud Mental. 2023. doi:10.1016/j.rpsm.2023.04.002
17. Toubasi AA, AbuAnzeh RB, Tawileh HBA, Aldebei RH, Alryalat SAS. A meta-analysis: the mortality and severity of COVID-19 among patients with mental disorders. Psychiatry Res. 2021;299:113856. doi:10.1016/j.psychres.2021.113856
18. Degnan A, Berry K, Sweet D, Abel K, Crossley N, Edge D. Social networks and symptomatic and functional outcomes in schizophrenia: a systematic review and meta-analysis. Social Psychiatry Psychiatric Epidemiol. 2018;53:873–888. doi:10.1007/s00127-018-1552-8
19. Ma J, Hua T, Zeng K, Zhong B, Wang G, Liu X. Influence of social isolation caused by coronavirus disease 2019 (COVID-19) on the psychological characteristics of hospitalized schizophrenia patients: a case-control study. Transl Psychiatry. 2020;10(1):411. doi:10.1038/s41398-020-01098-5
20. Wang P-W, Lu W-H, Ko N-Y, et al. COVID-19-related information sources and the relationship with confidence in people coping with COVID-19: Facebook survey study in Taiwan. J Med Internet Res. 2020;22(6):e20021. doi:10.2196/20021
21. Farooq A, Laato S, Islam AN. Impact of online information on self-isolation intention during the COVID-19 pandemic: cross-sectional study. J Med Internet Res. 2020;22(5):e19128. doi:10.2196/19128
22. Garfin DR, Silver RC, Holman EA. The novel coronavirus (COVID-2019) outbreak: amplification of public health consequences by media exposure. Health Psychol. 2020;39(5):355. doi:10.1037/hea0000875
23. Ceban F, Kulzhabayeva D, Rodrigues NB, et al. COVID-19 vaccination for the prevention and treatment of long COVID: a systematic review and meta-analysis. Brain Behav Immun. 2023;111:211–229. doi:10.1016/j.bbi.2023.03.022
24. Pardamean E, Roan W, Iskandar KTA, Prayangga R, Hariyanto TI. Mortality from coronavirus disease 2019 (Covid-19) in patients with schizophrenia: a systematic review, meta-analysis and meta-regression. General Hospital Psychiatry. 2022;75:61–67. doi:10.1016/j.genhosppsych.2022.01.010
25. Boppana U, Leonard TS, Jolayemi A, Ansari MI, Salib A. Drug-drug interactions between COVID-19 treatments and psychotropic medications: an updated study. Cureus. 2023;15(12). doi:10.7759/cureus.50469
26. Bitan DT, Kridin K, Givon-Lavi N, et al. COVID-19 booster vaccination among individuals with schizophrenia in Israel. JAMA psychiatry. 2022;79(5):508–512. doi:10.1001/jamapsychiatry.2022.0382
27. Tzur Bitan D, Kridin K, Cohen AD, Weinstein O. COVID-19 hospitalisation, mortality, vaccination, and postvaccination trends among people with schizophrenia in Israel: a longitudinal cohort study. Lancet Psychiatry. 2021;8(10):901–908. doi:10.1016/S2215-0366(21)00256-X
28. Tzur Bitan D. Patients with schizophrenia are under-vaccinated for COVID-19: a report from Israel. World Psychiatry. 2021;20(2):300–301. doi:10.1002/wps.20874
29. Lee D-W, Bae YS, Lee J-R, Sohn JH, Lee H, Lee JY. COVID-19 vaccination, incidence, and mortality rates among individuals with mental disorders in South Korea: a nationwide retrospective study. Asian J Psychiatry. 2023;85:103600. doi:10.1016/j.ajp.2023.103600
30. Hassan L, Sawyer C, Peek N, et al. COVID-19 vaccination uptake in people with severe mental illness: a UK-based cohort study. World Psychiatry. 2022;21(1):153–154. doi:10.1002/wps.20945
31. Lin C-W, Chang Y-P, Yen C-F. Predictors of motivation to receive a COVID-19 vaccination and the number of COVID-19 vaccine doses received in patients with schizophrenia. Vaccines. 2023;11(12):1781. doi:10.3390/vaccines11121781
32. Mazereel V, Van Assche K, Detraux J, De Hert M. COVID-19 vaccination for people with severe mental illness: why, what, and how? Lancet Psychiatry. 2021;8(5):444–450. doi:10.1016/S2215-0366(20)30564-2
33. Dror AA, Eisenbach N, Taiber S, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–779. doi:10.1007/s10654-020-00671-y
34. Peretti-Watel P, Seror V, Cortaredona S, et al. A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. Lancet Infect Dis. 2020;20(7):769–770. doi:10.1016/S1473-3099(20)30426-6
35. Hsieh K-Y, Li D-J, Chou FH-C, et al. Relationship of societal adaptation with vaccine worries among healthcare workers during the COVID-19 pandemic: the mediating effects of posttraumatic stress disorder. Int J Environ Res Public Health. 2022;19(15):9498. doi:10.3390/ijerph19159498
36. Lo A, Hsieh K-Y, Lu W-C, Shieh I, Chou FH-C, Shieh V. Development and validation of the Lo’s Healthy and Happy Lifestyle Scale (LHHLS): the resilience in general population facing COVID-19 in Taiwan. Int J Social Psychiatry. 2021;67(5):532–539. doi:10.1177/0020764020960771
37. Lo A, Jun B-O, Shieh V, Starlin CM, Sugahara S, Li D-J. A comparative study of social impacts of the COVID-19 pandemic on Republic of Korea, Japan, and Taiwan. Psychiatry Invest. 2021;18(10):1006. doi:10.30773/pi.2021.0220
38. Kao W-T, Hsu S-T, Chou FH-C, et al. The societal influences and quality of life among healthcare team members during the COVID-19 pandemic. Frontiers in Psychiatry. 2021;12:706443. doi:10.3389/fpsyt.2021.706443
39. Sheng W-H, Hsieh S-M, Chang S-C. Achievements of COVID-19 vaccination programs: Taiwanese perspective. JFormos Med Assoc. 2024;123:S70–S76. doi:10.1016/j.jfma.2023.04.017
40. Martin LR, Petrie KJ. Understanding the dimensions of anti-vaccination attitudes: the vaccination attitudes examination (VAX) scale. Ann Behav Med. 2017;51(5):652–660. doi:10.1007/s12160-017-9888-y
41. Dhanani LY, Franz B. A meta-analysis of COVID-19 vaccine attitudes and demographic characteristics in the United States. Public Health. 2022;207:31–38. doi:10.1016/j.puhe.2022.03.012
42. Tiwana MH, Smith J. Faith and vaccination: a scoping review of the relationships between religious beliefs and vaccine hesitancy. BMC Public Health. 2024;24(1):1806. doi:10.1186/s12889-024-18873-4
43. García LY, Cerda AA. Contingent assessment of the COVID-19 vaccine. Vaccine. 2020;38(34):5424–5429. doi:10.1016/j.vaccine.2020.06.068
44. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford publications; 2017.
45. Bendau A, Plag J, Petzold MB, Ströhle A. COVID-19 vaccine hesitancy and related fears and anxiety. Int Immunopharmacol. 2021;97:107724. doi:10.1016/j.intimp.2021.107724
46. Seddig D, Maskileyson D, Davidov E, Ajzen I, Schmidt P. Correlates of COVID-19 vaccination intentions: attitudes, institutional trust, fear, conspiracy beliefs, and vaccine skepticism. Soc Sci Med. 2022;302:114981. doi:10.1016/j.socscimed.2022.114981
47. Earnshaw VA, Eaton LA, Kalichman SC, Brousseau NM, Hill EC, Fox AB. COVID-19 conspiracy beliefs, health behaviors, and policy support. Transl Behav Med. 2020;10(4):850–856. doi:10.1093/tbm/ibaa090
48. Schernhammer E, Weitzer J, Laubichler MD, et al. Correlates of COVID-19 vaccine hesitancy in Austria: trust and the government. J Public Health. 2022;44(1):e106–e116. doi:10.1093/pubmed/fdab122
49. Soares P, Rocha JV, Moniz M, et al. Factors associated with COVID-19 vaccine hesitancy. Vaccines. 2021;9(3):300. doi:10.3390/vaccines9030300
50. Trent M, Seale H, Chughtai AA, Salmon D, MacIntyre CR. Trust in government, intention to vaccinate and COVID-19 vaccine hesitancy: a comparative survey of five large cities in the United States, United Kingdom, and Australia. Vaccine. 2022;40(17):2498–2505. doi:10.1016/j.vaccine.2021.06.048
51. Silver D, Kim Y, McNeill E, Piltch-Loeb R, Wang V, Abramson D. Association between COVID-19 vaccine hesitancy and trust in the medical profession and public health officials. Preventive Med. 2022;164:107311. doi:10.1016/j.ypmed.2022.107311
52. Chadwick A, Kaiser J, Vaccari C, et al. Online social endorsement and Covid-19 vaccine hesitancy in the United Kingdom. Social Media+ Society. 2021;7(2):20563051211008817. doi:10.1177/20563051211008817
53. Murphy J, Vallières F, Bentall RP, et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021;12(1):29. doi:10.1038/s41467-020-20226-9
54. Allington D, McAndrew S, Moxham-Hall V, Duffy B. Coronavirus conspiracy suspicions, general vaccine attitudes, trust and coronavirus information source as predictors of vaccine hesitancy among UK residents during the COVID-19 pandemic. Psychol Med. 2023;53(1):236–247. doi:10.1017/S0033291721001434
55. Wilson SL, Wiysonge C. Social media and vaccine hesitancy. BMJ Global Health. 2020;5(10):e004206. doi:10.1136/bmjgh-2020-004206
56. Jennings W, Stoker G, Bunting H, et al. Lack of trust, conspiracy beliefs, and social media use predict COVID-19 vaccine hesitancy. Vaccines. 2021;9(6):593. doi:10.3390/vaccines9060593
57. Lee C-J, Nagler RH, Wang N. Source-specific exposure to contradictory nutrition information: documenting prevalence and effects on adverse cognitive and behavioral outcomes. Health Commun. 2018;33(4):453–461. doi:10.1080/10410236.2016.1278495
58. Naseem Z, Khalid R. Positive thinking in coping with stress and health outcomes: literature review. J Res Reflect Educ. 2010;4(1).
59. Fournier A, Laurent A, Lheureux F, et al. Impact of the COVID-19 pandemic on the mental health of professionals in 77 hospitals in France. PLoS One. 2022;17(2):e0263666. doi:10.1371/journal.pone.0263666
60. Yang D, Tu -C-C, Dai X. The effect of the 2019 novel coronavirus pandemic on college students in Wuhan. Psychol Trauma Theory Res Prac Policy. 2020;12(S1):S6. doi:10.1037/tra0000930
61. Wissmath B, Mast FW, Kraus F, Weibel D. Understanding the psychological impact of the COVID-19 pandemic and containment measures: an empirical model of stress. PLoS One. 2021;16(7):e0254883. doi:10.1371/journal.pone.0254883
62. Meyer PS, Johnson DP, Parks A, Iwanski C, Penn DL. Positive living: a pilot study of group positive psychotherapy for people with schizophrenia. J Positive Psychol. 2012;7(3):239–248. doi:10.1080/17439760.2012.677467
63. Leamy M, Bird V, Le Boutillier C, Williams J, Slade M. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry. 2011;199(6):445–452. doi:10.1192/bjp.bp.110.083733
64. Slade M, Amering M, Oades L. Recovery: an international perspective. Epidemiol Psychiatric Sci. 2008;17(2):128–137. doi:10.1017/S1121189X00002827
65. Chadwick P, Taylor KN, Abba N. Mindfulness groups for people with psychosis. Behav Cognitive Psychother. 2005;33(3):351–359. doi:10.1017/S1352465805002158
66. Khoury B, Lecomte T, Gaudiano BA, Paquin K. Mindfulness interventions for psychosis: a meta-analysis. Schizophr Res. 2013;150(1):176–184. doi:10.1016/j.schres.2013.07.055
67. Repper J, Carter T. A review of the literature on peer support in mental health services. J Ment Health. 2011;20(4):392–411. doi:10.3109/09638237.2011.583947
68. Yanos PT, Roe D, Lysaker PH. Narrative enhancement and cognitive therapy: a new group-based treatment for internalized stigma among persons with severe mental illness. Int J Group Psychother. 2011;61(4):576–595. doi:10.1521/ijgp.2011.61.4.576
69. Firth J, Cotter J, Elliott R, French P, Yung AR. A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychol Med. 2015;45(7):1343–1361. doi:10.1017/S0033291714003110
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Understanding the Health System Conditions Affecting the Use of Long-Acting Injectable Antipsychotics in the Treatment of Schizophrenia in Clinical Practice: A US Healthcare Provider Survey
Zhdanava M, Starr HL, Lefebvre P, Totev TI, Shah A, Sheng K, Pilon D
Neuropsychiatric Disease and Treatment 2022, 18:1479-1493
Published Date: 22 July 2022
Impact of COVID-19 Pandemic on Prescribing of Long-Acting Injectable Antipsychotics for Schizophrenia: Results from a United States Prescriber Survey
Zhdanava M, Starr HL, Totev TI, Lefebvre P, Shah A, Sheng K, Pilon D
Neuropsychiatric Disease and Treatment 2022, 18:2003-2019
Published Date: 7 September 2022

