Back to Journals » Infection and Drug Resistance » Volume 18
Bacterial Epidemiology and Antimicrobial Resistance in Children in Shandong Province, China, 2017–2022: A Multicentre Retrospective Study
Authors Yang S, Wang M , Wang S
Received 24 December 2024
Accepted for publication 8 May 2025
Published 1 June 2025 Volume 2025:18 Pages 2823—2836
DOI https://doi.org/10.2147/IDR.S511161
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Oliver Planz
Shangmin Yang,1,2 Mengyuan Wang,1,2 Shifu Wang1,2 On behalf of Shandong Provincial Microbiome Research Center Children Bacterial and fungal Resistance Monitoring Research Network
1Department of Clinical Microbiology, Children’s Hospital affiliated to Shandong University, Jinan, Shandong, People’s Republic of China; 2Shandong Provincial Clinical Research Center for Children’s Health and Disease, Jinan, Shandong, People’s Republic of China
Correspondence: Shifu Wang, Children’s Hospital affiliated to Shandong University, Jinan, Shandong, 250022, People’s Republic of China, Email [email protected]
Introduction: Bacterial antimicrobial resistance is becoming increasingly serious, but there are very limited studies in children. Shandong Province Pediatric bacterial & fungal Antimicrobial Resistance Surveillance System (SPARSS) program was established in 2017 to monitor and analyze the trends of bacterial epidemiology and antimicrobial resistance in children. Clinical bacterial isolates were collected from 59 tertiary hospital in Shandong Province China during 2017 to 2022.
Methods: We conducted a retrospective analysis of bacterial distribution and resistance patterns, utilizing data from the SPARSS network and analyzed with WHONET 5.6 software.
Results: A total of 185,274 isolates were collected, and the top 5 bacteria were Staphylococcus aureus (19.0%), Escherichia coli (12.8%), Streptococcus pneumoniae (12.3%), Haemophilus influenzae (11.0%) and Klebsiella pneumoniae (7.1%). In the composition of strain specimens, most of the strains came from the respiratory tract (59.8%), followed by pus (11.4%). The resistance rate of Staphylococcus spp. to penicillins remains high at 90%, while the resistance rate to linezolid is low but shows an upward trend. Vancomycin-resistant strains have emerged in Enterococcus spp. which due to its complex genetic structure, possesses inherent resistance to most drugs. The resistance rate of Enterobacter spp. to meropenem remains low, although it exhibits a high resistance rate to β-lactams. Notably, carbapenem-resistant Salmonella spp. has been identified since from 2022. Acinetobacter baumannii and Pseudomonas aeruginosa demonstrate high drug resistance to most antibiotics. H. influenzae and Moraxella catarrhalis, primarily isolated from respiratory tract samples, show an increasing trend in β-lactamase-producing strains annually. The detection rates of multi-drug-resistant bacteria, including MRSA, CREO, CRKP, CRPA, and CRAB, have been decreasing annually, with their distribution varying among children of different ages. The resistance rate of Candida tropicalis to fluconazole was 43.6%, which was much higher than the detection rate of adults in China and Europe.
Discussion: Despite restrictions on antibiotic use in China, the situation of bacterial drug resistance remains critical, particularly in children. Therefore, long-term monitoring of bacterial drug resistance in this population is essential to develop effective strategies for the early and accurate treatment of childhood infections.
Keywords: bacteria, antimicrobial resistance, children, China, Multi-Drug-Resistant Organisms, MDROs
Introduction
Bacterial antimicrobial resistance (AMR) is becoming increasingly serious with the unreasonable use of antibiotics, which is a serious threat to human public health security.1 It has been estimated to cause 10 million deaths worldwide by year 2050 if the current trend of inappropriate and excessive use of antibiotics continues.2 In addition to being associated with a high mortality rate, bacteria AMR imposes a significant financial burden on health-care systems. For instance, in the United States, more than 2.8 million multidrug-resistant (MDR) bacterial infections occur annually, causing at least 35,000 deaths and $20 billion in health-care expenditures.3 So, both preventing bacterial AMR and increasing microbiological laboratory and data collection capacity to improve scientific understanding of this health threat should be a very high priority for global health policy makers. Although there has been a lot of testing in the world to detect the prevalence of AMR and MDR bacteria in humans, such as Global Antimicrobial Resistance and Use Surveillance System (GLASS), European Antimicrobial Resistance Surveillance Network (EARS-Net), CARSS (China Antimicrobial Resistance Surveillance System) and CHINET (China Antimicrobial Surveillance Network),4–6 there are very limited studies in children,7 and the quality of published studies assessing the distribution of Multi-Drug-Resistant Organisms (MDROs) in children is mixed. At the same time, there is no monitoring data report on the rate of fungal resistance in children for consecutive years from China. Therefore, AMR surveillance network unique to children is essential for pediatric antimicrobial stewardship. To focus on the AMR surveillance in pediatric patients, we established the Shandong Province Pediatric bacterial and fungal Antimicrobial Resistance Surveillance System (SPARSS) program in 2017, which currently comprises 59 hospitals. We presented a large amount of bacteria data in the past six years from SPARSS and made a comprehensive analysis on the evolution of bacteria epidemiology and the AMR profiles.
On the basis of our data, we analyzed the bacterial epidemiology and resistance profiles of primary pathogens in Shandong Province’s children from 2017 to 2022 for the first time, analyzed the MDROs distributions with time and/or with age, and described MDROs’ potential threaten to children, especially to the low-immunity neonates. Our study will be very useful to guide the anti-infection therapy in Shandong Province’s children as well as the worldwide pediatric patients.
Materials and Methods
Enrollment of Bacteria and Patients
During 2017 to 2022, all unduplicated aerobic bacteria were collected from 59 tertiary hospitals in Shandong Province, China. For the repeated strains: only the first isolate from the same species and the same patient was enrolled in this study.
Neonatal patients were defined as the discharge with age in days between 0 and 28 days (inclusive), while non-neonatal patients were defined as the children with 29 days to 18 years (exclusive).
Isolate Inclusion and Exclusion Criteria
Unified standard was conducted stringently in each hospital. Inclusion and exclusion criteria from different samples were conducted as follows. Respiratory tract includes: upper respiratory tract specimens (throat swabs) and lower respiratory tract specimens (sputum and BALF). All α-hemolytic Streptococcus spp. were excluded, except Streptococcus pneumoniae. Blood: all unduplicated aerobic bacteria collected from blood culture were involved. Stool: only enteropathogenic bacteria were involved. Urine: only involved the bacteria >104 colony forming units (CFU)/mL and the bacterial species were ≤2.
Strain Identification
We used Matrix assisted laser desorption ionization (MALDI) TOF MS to identify the strains.
Antimicrobial Susceptibility
Antimicrobial susceptibility test was carried out using Kirby-Bauer method or automated systems interpreted according to the criteria of Clinical and Laboratory Standards Institute (CLSI) 2024 breakpoints.8 Penicillin susceptibility of S. pneumonia was detected by E-test, its breakpoint in meningitis and nonmeningitis samples were different.
CRE were defined as the Enterobacteriaceae spp. strains, which presented resistance to one of ertapenem, imipenem or meropenem. CRAB and CRPA were identified as imipenem or meropenem resistant Acinetobacter baumannii and Pseudomonas aeruginosa. Penicillin-nonsusceptible S. pneumoniae (PNSP) was defined as penicillin-intermediate or resistant. PNSP was tested using penicillin E-test and interpreted according to 2024 CLSI standard.
β-Lactams Test
Oxoid™ touch stick β-lactams product was used to detect the β-lactams activity according to the instructions. This product exhibits a rapid distinctive color change from yellow to red. Positive result was defined as yellow to pink-red color change of the disk. Negative result was considered as no color change. Positive control: Staphylococcus aureus ATCC 29213 or the β-lactams product positive strain has been confirmed in the lab; negative control: Haemophilus influenzae ATCC 10211 or the β-lactams product negative strain has been confirmed in the lab.
Reference Strains
S. aureus ATCC 29213, Escherichia coli ATCC 25922 and P. aeruginosa ATCC 27853 were included to ensure reproducibility of the antibiotic susceptibility testing procedure.
Statistical Analysis
Statistics analyses were performed using GraphPad Prism 7.0 (GraphPad Software, Inc., San Diego, California, USA). Differences among the groups were analyzed with independent samples t test. Two side P values of less than 0.05 were considered as statistically significance.
Results
Distribution of Clinical Isolates
From 2017 to 2022, a total of 185,274 bacterial strains isolated from children were enrolled in the SPARSS program, of which 3.2% (5,886) were collected from outpatients and 96.8% (179,388) were collected from inpatients. There were 77,804 Gram-positive bacteria (42.0%) and 105,110 Gram-negative bacteria (56.7%). The top 10 bacteria were S. aureus (19.0%), E. coli (12.8%), S. pneumoniae (12.3%), H. influenzae (11.0%), Klebsiella pneumoniae (7.1%), Moraxella catarrhalis (6.4%), P. aeruginosa (4.6%), A. baumannii (3.2%), Enterobacter cloacae (2.6%), and Staphylococcus epidermidis (2.3%). In the composition of strain specimens, most of the strains came from the respiratory tract (59.8%), followed by pus (11.4%), blood specimen (7.1%) and urine specimen (4.7%) (Table S1). Notably, the constituent proportion in the respiratory tract dropped from 64.18% in 2017 to 53.28% in 2022. Compared to other specimen types, there have been significant changes in the composition of respiratory tract specimen strains over the past six years. The proportion of H. influenzae and S. pneumoniae in respiratory specimens decreased significantly in 2020, while the proportion of S. aureus increased markedly (Figure 1A). The proportion of M. catarrhalis reached its peak in 2020, and overall, there was a decreasing trend in the proportions of E. coli and K. pneumoniae in respiratory specimens. The E. coli in pus samples and urine samples are the most frequently detected bacteria. In blood samples, the main bacteria detected are S. epidermidis and Staphylococcus hominis, the main bacteria detected are E. coli and Enterococcus faecium in urine specimen and in the pus specimen it is mainly E. coli and S. aureus (Figure 1B–D).
AMR Trends in Main Bacteria
Staphylococcus spp
S. aureus exhibits the highest resistance rate to penicillin G at 95.8%, with no declining trend observed in recent years. The resistance rate to oxacillin is 28.3% and remains stable, showing a relatively stable trend. In contrast, there has been a declining trend in resistance rates to aminoglycosides and fluoroquinolones. Coagulase-negative staphylococci (CoNS) has the highest resistance rate to penicillin G (93.2%), but there has been a gradual decrease in recent years (P=0.0129). Additionally, there is a downward trend in resistance rates to erythromycin (P=0.0034), trimethoprim-sulfamethoxazole (SXT) (P<0.0001). The resistance rates of S. aureus and CoNS to linezolid are generally low, and no vancomycin-resistant Staphylococcus. spp. was identified. Overall, CoNS exhibits a higher resistance compared to S. aureus (Table S2).
The prevalence of antibiotic resistance in Methicillin-resistant S. aureus (MRSA) is generally higher than that in Methicillin-sensitive S. aureus (MSSA), with a statistically significant difference (P< 0.05). However, the resistance rates to gentamicin and SXT in MRSA are lower than those in MSSA, with no significant differences in resistance rates to levofloxacin and moxifloxacin between MRSA and MSSA. There is no significant decreasing trend in resistance rates of MRSA to SXT (P=0.926), ciprofloxacin (P=0.0764), and rifampin (P=0.183). In MSSA, there is no significant decreasing trend in resistance rates to penicillin, but there is a decreasing trend in resistance rates to erythromycin, clindamycin, tetracycline and fluoroquinolones (P<0.05) (Table 1).
 |
Table 1 AMR Profiles of MRSA and MSSA Reported by SPASS Program in Shandong Province, China, 2017 to 2022 |
Streptococcus spp
S. pneumoniae and Streptococcus pyogenic are highly sensitive to penicillin, while Streptococcus mitis exhibits lower sensitivity to penicillin compared to the first two. All three species demonstrate relatively high resistance to clindamycin and erythromycin, with S. pneumoniae and S. pyogenic being more pronounced. S. mitis has a significantly higher resistance rate to levofloxacin than the others. The resistance rate of S. pneumoniae to SXT and ceftriaxone remains relatively stable, while the resistance rate of S. pyogenic to levofloxacin has shown a downward trend over the years (P<0.0019) (Table S3).
Enterococcus spp
The resistance of E. faecium is generally higher than that of E. faecalis (except for tetracycline). Both species show low rates of vancomycin resistance, no E. faecalis strains resistant to linezolid were found, but resistant strains of E. faecium do exist. The resistance rates of E. faecalis to high concentrations of gentamicin, ciprofloxacin, and levofloxacin have been decreasing annually (P<0.05). In contrast, E. faecium shows a decreasing trend in resistance rates to tetracycline, erythromycin, ampicillin, and penicillin (P<0.05) (Table S4).
Enterobacteriaceae spp
E. coli and K. pneumoniae have shown a declining trend in resistance to most antibiotics (P<0.05). The resistance of E. coli to tigecycline, amikacin, meropenem, and cefoxitin remains relatively stable, while K. pneumoniae exhibits consistent resistance to levofloxacin, ciprofloxacin, amikacin, and meropenem. The proportion of carbapenem-resistant E. coli (CREO) is 1% (302/23,790), whereas the proportion of carbapenem-resistant K. pneumoniae (CRKP) is 6.2% (813/13,129) (Table S5).
Non-Fermentative Gram-Negative Bacilli
The antibiotic resistance rates of A. baumannii against cefepime, ceftriaxone, levofloxacin, meropenem, and imipenem have shown a declining trend over the years (P<0.05). In contrast, P. aeruginosa exhibits stable resistance rates against levofloxacin, ciprofloxacin, and gentamicin. The proportion of carbapenem-resistant A. baumannii (CRAB) is 20.8% (1218/5845), while the proportion of carbapenem-resistant P. aeruginosa (CRPA) stands at 8.7% (750/8595) (Table S6).
Fastidious Bacteria
The antibiotic resistance rates of H. influenzae to levofloxacin remain relatively low and exhibit a consistent annual downward trend (P<0.05). However, the prevalence of β-lactamase-producing strains is on the rise (P<0.05). The resistance rates to amoxicillin-clavulanate, cefotaxime, chloramphenicol, and SXT are decreasing over the years (P<0.05). In contrast, there is an increasing trend in resistance rates to ampicillin-sulbactam and cefuroxime, while the rare strains β-lactamase negative ampicillin resistance (BLNAR) H. influenzae is also becoming more prevalent annually (P<0.05). For M. catarrhalis, the resistance rate to chloramphenicol remains low without a significant upward trend. Nevertheless, the emergence of β-lactamase-producing strains is increasing annually (P<0.05). Resistance rate to SXT is also on the rise, whereas resistance to amoxicillin-clavulanate, cefuroxime, cefotaxime, and levofloxacin, have shown a downward trend over the years (P<0.05) (Table S7).
Salmonella spp
The resistance rates of Salmonella spp. to ampicillin, ceftriaxone, and Aztreonam have been increasing over the years (P<0.05). The resistance rate to carbapenems remains at a relatively low level, but resistant strains have emerged. The resistance rates to combination formulations such as ampicillin/sulbactam, piperacillin/tazobactam, and cefoperazone/sulbactam have remained stable, with piperacillin/tazobactam showing a lower resistance rate (0.7~2%). The resistance rate to ampicillin/sulbactam remains at a high level (Table 2). Notably, the detection rate of carbapenem resistant Salmonella spp. in 2022 is as high as 0.5%, which deserves further attention and research.
 |
Table 2 AMR Profiles of Salmonella spp. Reported by SPARSS Program in Shandong Province, China, 2017 to 2022 |
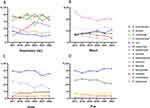
Change Trend in MDROs Resistance
We have conducted an analysis on the drug resistance changes of four types of MDR bacteria, namely CREO, CRKP, CRAB, and CRPA. CREO has a significantly lower resistance rate to amikacin compared to other antibiotics. In 2020, the resistance rates of CREO to most antibiotics decreased to their lowest levels (except for ciprofloxacin and SXT), but in 2021, they increased back to the original levels or even higher (Figure 2A). For CRKP, the resistance rates to ciprofloxacin, levofloxacin, gentamicin, amikacin, and tobramycin showed a decreasing trend from 2017 to 2018, but after 2018, they started to increase. Among them, the resistance rate to levofloxacin decreased in 2021, while the rates for ciprofloxacin and gentamicin decreased in 2020, but ciprofloxacin showed an increasing trend after 2021 (Figure 2B). CRAB had resistance rates to most antibiotics above 40%, with the highest resistance rate to ciprofloxacin. The resistance rates of CRAB to fluoroquinolones, ciprofloxacin and levofloxacin increased in 2017, remained relatively stable from 2018 to 2021, and showed a decreasing trend in 2022. The resistance rates of CRAB to amikacin and tobramycin with an overall decreasing trend, reaching their lowest points in 2019 (Figure 2C). The trends of CRPA resistance to fluoroquinolones (ciprofloxacin, levofloxacin), aminoglycosides, and piperacillin-tazobactam were similar, increasing from 2017 to 2018, decreasing from 2018 to 2019, increasing from 2019 to 2021, and decreasing in 2022 (Figure 2D).
 |
Figure 2 AMR rates of carbapenem-resistant strains reported by the SPARSS Program, 2017 to 2022. (A) AMR rates of CREO; (B) AMR rates of CRKP; (C) AMR rates of CRAB; (D) AMR rates of CRPA. |
We analyzed the annual proportions of MRDOS. Except for MRSA, which showed no significant trend, there was a noticeable year-on-year decline in CREO, CRKP, CRAB, and CRPA. The proportion of fluconazole resistant Candida tropicalis (FRCT) increased significantly in 2019, followed by a steady decline in the subsequent years (Figure 3A). CRPA was found to be more prevalent in newborns compared to other age groups, while MRSA showed a higher prevalence among school-aged children. CRAB was significantly more common in school-aged children than in other age groups. In contrast, CRKP exhibited a relatively even distribution across different age groups, with no significant differences observed. CREO maintained a consistently low proportion across all age stages (Figure 3B).
 |
Figure 3 Distribution trends of MDROs as reported by the SPARSS program, 2017 to 2022. (A) Distribution trends of MDROs year-by-year; (B) Distribution trends of MDROs in different age groups. |
Discussion
Children are major consumers of antimicrobial agents and have high rates of AMR, due to their underdeveloped immune systems make them more susceptible to infectious diseases. The limited use of antibacterial drugs in children has led to the widespread use of carbapenems in children, this antibiotic pressure caused the detection rate of CRE was also higher in children than in adults.9 Long-term global and national surveillance of AMR trends is thus required to guide the clinic anti-infection treatment. To our knowledge, we firstly described and analyzed the overall AMR profiles of common bacteria isolated from children in Shandong Province, China, indicating that MDROs (which include MRSA, CREO, CRKP, CRAB, and CRPA) were commonly detected from children and presented much higher antimicrobial resistance compared with the sensitive strains. During 2017 to 2022, a total of 185,274 bacteria were enrolled in SPARSS Program, the top ten predominant bacteria isolated from children were S. aureus, E. coli, S. pneumoniae, H. influenzae, K. pneumoniae, M. catarrhalis, P. aeruginosa, A. baumannii, E. cloacae and S. epidermidis.
According to statistics,10 respiratory tract infections are the most significant infectious disease factor affecting children’s health. Most bacteria we isolated were derived from respiratory specimens (>50%), with the highest proportion being S. pneumoniae (19.0%, 21,059/110,720), followed by H. influenzae (17.79%, 19,702/110,720). From 2017 to 2022, the proportions of S. pneumoniae and H. influenzae isolated from respiratory specimens showed a decline in both 2020 and 2022. This phenomenon is associated with the strict COVID-19 containment measures (for example, attending classes at home) implemented in Shandong Province, which not only reduced the transmission rate of COVID-19 but also decreased the spread of other microorganisms transmitted through respiratory secretions. However, the percentage of M. catarrhalis, a common cause of respiratory infections,11 showed an increasing trend from 2017 to 2019, followed by a gradual decline from 2020 to 2022. This trend does not align with that of H. influenzae and S. pneumoniae, and it also differs from data reported in Xiangtan City, Hunan Province.12 Aside from respiratory specimens, there were no significant changes in the percentage of bacteria detected in other specimen types, suggesting that the hospital from which our data was sourced was not significantly impacted by COVID-19, leading to a stable dataset.
S. pneumoniae is the most detected bacterium in respiratory specimens. Despite the availability of effective vaccines such as pneumococcal conjugate vaccines (PCV) and the 23-valent pneumococcal polysaccharide vaccine (PPV23), the vaccination rate remains low in China due to the high cost of these vaccines,13 posing a significant threat to children’s health. Our study identified a total of 22,772 strains of S. pneumoniae, which exhibited high resistance to macrolide antibiotics and SXT, while showing relatively low resistance to β-lactam antibiotics, with a declining trend observed over the years. This finding is consistent with previous literature.13 The misuse of macrolide drugs and the clonal spread of MDR strains may contribute to the high prevalence of macrolide resistance in China. Therefore, macrolide antibiotics should be used with caution as empirical treatment for S. pneumoniae infections in the current context in China. Most of the resistance patterns observed in Streptococci spp. are like those of S. pneumoniae; however, S. mitis strains of Streptococci spp. displayed higher resistance to penicillin, while showing lower resistance rates to macrolide antibiotics, that is also consistent with existing literature.14
H. influenzae can cause a range of infectious diseases in children, including pneumonia, invasive diseases, otitis media, upper respiratory tract infections, and vulvovaginitis in preadolescent children, posing a serious threat to their health.15 In this study, a total of 20,408 strains of H. influenzae were detected, with 19,702 strains (96.54%) originating from respiratory specimens. Due to limitations in experimental conditions, not all strains were serotyped. According to relevant literature,16 since the introduction of the conjugate vaccine against H. influenzae type b (Hib), invasive diseases caused by this bacterium are now predominantly attributed to non-typeable H. influenzae (NTHi), with most strains detected in China being NTHi. In recent years, there has been an increase in strains producing β-lactamase and BLNAR, as well as strains resistant to ampicillin-sulbactam, cefuroxime, and azithromycin, which aligns with existing literature.15 Therefore, third-generation cephalosporins may be the preferred treatment option for infections caused by ampicillin-resistant H. influenzae.
S. aureus is one of the most prevalent infectious pathogens and is responsible for a range of infectious diseases, including pneumonia, bloodstream infections, and skin infections.17 In this study, S. aureus was found to occupy a significant position across various specimens. Notably, despite ranking second in respiratory specimens, its prevalence trend has remained unaffected by COVID-19 control measures, potentially due to its unique infection mechanisms. The infection mechanisms of S. aureus differ depending on the body site. For instance, pulmonary infections often occur as secondary infections following viral pneumonia.18 Skin infections typically arise after skin injuries,17 while food poisoning caused by staphylococcal enterotoxin usually results from the consumption of contaminated food.19 In our study, we detected 8,746 strains of MRSA. Currently, vancomycin is the first-line treatment for MRSA; however, its use should be approached with caution due to its slow bactericidal activity, poor tissue permeability, and potential renal toxicity.20,21 CoNS, recognized as opportunistic pathogens, are among the leading causes of hospital-associated infections.22 In this study, CoNS was predominantly isolated from pus and blood, these CoNS found in the bloodstream are considered non-pathogenic. However, due to the lack of relevant clinical information, we cannot further confirm their pathogenicity. As a normal flora of the skin and mucous membranes, CoNS can easily lead to invasive infections following skin injuries.22 The resistance rate of Staphylococcus spp. to penicillin was notably high (>90%), and approximately 50% of strains exhibited resistance to macrolide antibiotics, which was similar to a foreign study.23 Since their initial report, resistance to linezolid has been steadily increasing.24 Our study also identified linezolid-resistant Staphylococcus spp., though we did not investigate the resistance mechanisms of these strains further. Previous research indicates that the most common mechanisms of resistance involve transmissible cfr ribosomal methyltransferase or mutations in 23S rRNA.25 Thus, it is essential to enhance the monitoring of drug resistance in Staphylococcus spp. to provide timely and effective information for clinical empirical treatments.
Enterococcus spp. is a significant pathogen associated with healthcare-related infections.26 Since the emergence of vancomycin-resistant strains of E. faecium and E. faecalis in clinical isolates, E. faecium has garnered considerable medical and public attention. The primary species detected are E. faecium and E. faecalis, with 5 strains of E. faecium and 2 strains of E. faecalis identified as resistant to vancomycin. Notably, the resistance rate of E. faecium to β-lactam antibiotics is higher than that of E. faecalis, aligning with findings from the literature.27 Enterococcus spp. possesses inherent resistance to various antimicrobial agents, including cephalosporins, aminoglycosides, clindamycin, and SXT. Additionally, due to the plasticity of its genome, Enterococcus spp. demonstrates a significant capacity to acquire new resistance determinants.28 To mitigate the spread of antibiotic resistance in Enterococcus spp., it is crucial to enhance resistance detection and explore new treatment strategies. Furthermore, stricter management of antibiotic usage practices should be implemented.27
Enterobacteriaceae spp. bacteria are among the most common human pathogens and are a significant source of both community-acquired and hospital-acquired infections, with E. coli being the most important for human health.29 In this study, E. coli was found at a high isolation rate in various samples. As a normal inhabitant of the intestinal flora, E. coli can cause a range of infections including cystitis, pyelonephritis, septicemia, pneumonia, peritonitis, meningitis, and device-related infections, presenting a serious threat to children’s health.29 In China, K. pneumoniae was responsible for 11.9% of pathogens isolated from ventilator-associated pneumonia (VAP) and intensive care unit (ICU) acquired pneumonia.30 This high infection and mortality rate has placed a substantial burden on the country’s healthcare system. Currently, β-lactam antibiotics are the most used antibiotics.31 However, their widespread use has led to a dramatic increase in bacteria producing β-lactamases over the past few decades.32 Our study found high resistance rates in E. coli and K. pneumoniae to penicillin, first-generation, and third-generation cephalosporins, but lower resistance rates to amoxicillin-clavulanate and fourth-generation cephalosporins. The resistance rate to the carbapenem antibiotic meropenem remained low. Compared with a European study, the resistance rate of the Enterobacteriaceae spp. detected in our study was relatively low to the above drugs.33 Extended-spectrum β-lactamases (ESBLs) are a group of rapidly evolving enzymes that hydrolyze broad-spectrum cephalosporins, penicillin, and aztreonam, but not carbapenems.34 These enzymes can be inhibited by “classical” β-lactamase inhibitors such as clavulanate, sulbactam, and tazobactam.35 Due to the limited use of carbapenems in children, they remain the preferred treatment option for treating severe pediatric ESBLs infections.36 However, increased carbapenem use could lead to the emergence and global spread of carbapenem-resistant Enterobacteriaceae (CRE). Our study showed a decreasing trend in CRE rates over the past six years, with CREO and CRKP being distributed relatively evenly across different age groups, a finding that differs somewhat from both domestic and international studies.37,38 Most of the CRE strains we detected were resistant to cephalosporins, piperacillin, cefoperazone-sulbactam, piperacillin-tazobactam, aztreonam, and carbapenems. Due to some hospitals’ limitations, we could not determine enzyme types, so we did not quantify the production of each enzyme type. Research indicates that39 common enzyme types of CRE isolated from children in China are NDM, KPC, and OXA, in that order, with K. pneumoniae producing the blaOXA-232 enzyme being isolated exclusively from children. According to IDSA treatment guidelines, the treatment of CRE infections should begin with identifying the enzyme type produced by the strain,40 which will guide the subsequent treatment plan based on the enzyme type and infection site.
Salmonella spp. can lead to diarrhea and even fatal outcomes in children. In addition to the well-known typhoid and paratyphoid types, non-typhoidal Salmonella spp. can also have serious consequences.41,42 This study identified a total of 2,821 strains of Salmonella spp., and a comprehensive analysis of their drug susceptibility was conducted. The resistance rates to first-line antibiotics, such as ampicillin and cotrimoxazole, were significantly elevated. Furthermore, the resistance rates to third-generation cephalosporins and fluoroquinolones were also notably high, aligning with findings from international studies.43–45 While the resistance rate to carbapenem antibiotics remains low (in 2022 is as high as 0.5%) at present, drug-resistant strains have begun to emerge, potentially jeopardizing our last line of treatment for Salmonella spp. infections.45
P. aeruginosa and A. baumannii were the most isolated pathogens among non-fermentative bacteria. A. baumannii was predominantly found in respiratory tract, while P. aeruginosa accounted for a higher proportion of isolates from pus samples. A. baumannii is known to cause hospital-acquired infections such as ventilator-associated pneumonia, bacteremia, urinary tract infections, meningitis, and surgical wound infections.46 Due to its strong drug resistance and ability for clonal transmission,47 infections caused by A. baumannii can be particularly challenging to treat. In this study, it was observed that the resistance rates of A. baumannii to most antibiotics had increased in 2020, possibly linked to the epidemic control measures implemented in Shandong Province during that year. According to the World Health Organization’s list of drug-resistant bacteria, carbapenem-resistant A. baumannii (CRAB) was identified as the top threat to human health in 2017 in terms of the urgent need for the development of new antibiotics.48 A total of 1218 CRAB strains were detected in this study, with a higher proportion isolated from school-age children compared to other age groups, which is consistent with findings from a similar study in Shanghai.49 Treatment of CRAB infections typically involves combination therapy, especially for moderate to severe cases.50 Infections caused by P. aeruginosa pose a significant challenge due to the pathogen’s ability to develop drug resistance, produce multiple virulence factors, and form biofilms.51,52 Over the years, the resistance of P. aeruginosa to commonly used antibiotics has increased significantly,53 with β-lactam antibiotics being the primary choice for treatment.52 In this study, the resistance of P. aeruginosa to β-lactams was higher compared to other antibiotics, with fluoroquinolones following closely behind. The resistance to meropenem remained relatively low, consistent with findings from other countries.54 Treatment guidelines from the IDSA recommend tailoring antibiotic therapy based on sensitivity results,40 with adjustments made as needed and real-time monitoring of sensitivity data. For infections caused by MDR P. aeruginosa, preferred antibiotics include ceftazidime-avibactam, cefepime-tazobactam, and imipenem-cilastatin-relebactam.
The detection rate of FRCT in this study was 43.6%, which is higher than that reported in other studies in China,55 this discrepancy may be attributed to the fact that all specimens were collected from children. Globally, resistance to azole drugs in C. tropicalis is primarily observed in the Asia-Pacific region, whereas resistance levels in European and US countries remain low (below 10%).56 Compared to Candida albicans, there is a paucity of research on the mechanisms of drug resistance in C. tropicalis, both domestically and internationally. Currently, the mechanisms of C. tropicalis resistance to azole antibiotics mainly involve two factors: mutations in the drug’s target site and increased expression of efflux pumps.57,58 Therefore, enhancing the detection of C. tropicalis resistance will aid in the development of more accurate diagnostic and treatment strategies.
Our research may have some limitations due to the lack of relevant clinical information, we cannot further confirm their pathogenicity.
Conclusion
The pathogen epidemiology and resistance in children are characteristic and quite different from those for the adult population. MDROs presented much higher AMR profiles and have become an urgent threat to children, with CRKP, CRAB, and CRPA strains showing decreasing but fluctuating trends between 2017 and 2022 due to factors such as COVID-19 and a lower birth rate in China. Keeping effective and continuous surveillance on the trends of bacterial epidemiology and AMR profiles among children is of great significance, because of the emergence of carbapenem-resistant salmonella and the proportion of fluconazole resistant Candida tropicalis continued to increase.
Availability of Supporting Data
The authors confirm that the other data supporting the results of this study are available within the article and its supplementary materials. All of the associated data are available from the corresponding author.
Ethic Statement
All experiments involving human participants were performed according to the guidelines and regulations of the Declaration of Helsinki (2013 version). The study guarantees that the identities of the participants and other related data have been kept anonymous and confidential. The requirement for informed consent was waived because of the retrospective nature of the study.
Ethical Approval
This study was reviewed and approved by the Ethical Review Committee of Children’s Hospital Affiliated to Shandong University (approval no. SDFE-IRB/P-2022017).
Funding
This work was supported by the Shandong Children’s Health and Disease Clinical Medical Research Center Project (grant number: RC006), the special fund for high-level talents in the medical and health industry of Jinan City (Shifu Wang), and the Science and Technology Development Program of Jinan Municipal Health Commission (2022-1-45 and 2022-2-149).
Disclosure
All authors disclose no competing interests in this work.
References
1. Xiao G, Li J, Sun Z. The combination of antibiotic and non-antibiotic compounds improves antibiotic efficacy against multidrug-resistant bacteria. Int J Mol Sci. 2023;24(20):15493. doi:10.3390/ijms242015493
2. Pulingam T, Parumasivam T, Gazzali AM, et al. Antimicrobial resistance: prevalence, economic burden, mechanisms of resistance and strategies to overcome. Eur J Pharm Sci. 2022;170:106103. doi:10.1016/j.ejps.2021.106103
3. Strathdee SA, Davies SC, Marcelin JR. Confronting antimicrobial resistance beyond the COVID-19 pandemic and the 2020 US election. Lancet. 2020;396(10257):1050–1053. doi:10.1016/S0140-6736(20)32063-8
4. Veeraraghavan B, Walia K. Erratum: antimicrobial susceptibility profile & resistance mechanisms of global antimicrobial resistance surveillance system (GLASS) priority pathogens from India. Indian J Med Res. 2019;149(3):432. doi:10.4103/0971-5916.261122
5. Mader R, Damborg P, Amat J-P, et al. Building the European antimicrobial resistance surveillance network in veterinary medicine (EARS-Vet). Euro Surveill. 2021;26(4). doi:10.2807/1560-7917.ES.2021.26.4.2001359
6. Hu F, Zhu D, Wang F, et al. Current Status and Trends of Antibacterial Resistance in China. Clin Infect Dis. 2018;67(suppl_2):S128–S134. doi:10.1093/cid/ciy657
7. Pana ZD, El-Shabrawi M, Sultan Ma, et al. Fighting the hidden pandemic of antimicrobial resistance in paediatrics: recommendations from the international pediatric association. BMJ Paediatr Open. 2023;7(1):e002084. doi:10.1136/bmjpo-2023-002084
8. CLSI.Performance standards for antimicrobial susceptibility testing.
9. Kariuki K, Diakhate MM, Musembi S, et al. Plasmid-mediated quinolone resistance genes detected in Ciprofloxacin non-susceptible Escherichia coli and Klebsiella isolated from children under five years at hospital discharge, Kenya. BMC Microbiol. 2023;23(1):129. doi:10.1186/s12866-023-02849-2
10. Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222.
11. Morris DE, Osman KL, Cleary DW, Clarke SC, et al. The characterization of Moraxella catarrhalis carried in the general population. Microb Genom. 2022;8(5). 000820
12. Feng Y, Zhang H, Zhang B, et al. Impact of normalized COVID-19 prevention and control measures on lower respiratory tract infection pathogenesis in hospitalized children. Front Public Health. 2024;12:1367614. doi:10.3389/fpubh.2024.1367614
13. Xu Y, Zhou X, Zheng W, et al. Serotype distribution, antibiotic resistance, multilocus sequence typing, and virulence factors of invasive and non-invasive Streptococcus pneumoniae in Northeast China from 2000 to 2021. Med Microbiol Immunol. 2024;213(1):12. doi:10.1007/s00430-024-00797-w
14. Davidovich NV, Galieva AS, Davydova NG, et al. Spectrum and resistance determinants of oral streptococci clinical isolates. Klin Lab Diagn. 2020;65(10):632–637. doi:10.18821/0869-2084-2020-65-10-632-637
15. Zhou M, Fu P, Fang C, et al. Antimicrobial resistance of Haemophilus influenzae isolates from pediatric hospitals in Mainland China: report from the ISPED program, 2017-2019. Indian J Med Microbiol. 2021;39(4):434–438. doi:10.1016/j.ijmmb.2021.09.001
16. Zhou Y, Wang Y, Cheng J, et al. Molecular epidemiology and antimicrobial resistance of Haemophilus influenzae in Guiyang, Guizhou, China. Front Public Health. 2022;10:947051. doi:10.3389/fpubh.2022.947051
17. Cheung GYC, Bae JS, Otto M. Pathogenicity and virulence of Staphylococcus aureus. Virulence. 2021;12(1):547–569. doi:10.1080/21505594.2021.1878688
18. McCullers JA. The co-pathogenesis of influenza viruses with bacteria in the lung. Nat Rev Microbiol. 2014;12(4):252–262. doi:10.1038/nrmicro3231
19. Fisher EL, Otto M, Cheung GYC. Basis of virulence in enterotoxin-mediated staphylococcal food poisoning. Front Microbiol. 2018;9:436. doi:10.3389/fmicb.2018.00436
20. Hassoun A, Linden PK, Friedman B. Incidence, prevalence, and management of MRSA bacteremia across patient populations-a review of recent developments in MRSA management and treatment. Crit Care. 2017;21(1):211. doi:10.1186/s13054-017-1801-3
21. Echeverria-Esnal D, Marín-Casino M, Retamero A, et al. Can we guarantee less nephrotoxicity when vancomycin is administered by continuous infusion? Int J Antimicrob Agents. 2016;48(1):116–117. doi:10.1016/j.ijantimicag.2016.04.003
22. Becker K, Heilmann C, Peters G. Coagulase-negative staphylococci. Clin Microbiol Rev. 2014;27(4):870–926. doi:10.1128/CMR.00109-13
23. Fallah F, Karimi A, Azimi L, et al. The impact of the COVID-19 pandemic on pediatric bloodstream infections and alteration in antimicrobial resistance phenotypes in Gram-positive bacteria, 2020-2022. BMC Pediatr. 2024;24(1):671. doi:10.1186/s12887-024-05146-7
24. Azhar A, Rasool S, Haque A, et al. Detection of high levels of resistance to linezolid and vancomycin in Staphylococcus aureus. J Med Microbiol. 2017;66(9):1328–1331. doi:10.1099/jmm.0.000566
25. Gu B, Kelesidis T, Tsiodras S, et al. The emerging problem of linezolid-resistant Staphylococcus. J Antimicrob Chemother. 2013;68(1):4–11. doi:10.1093/jac/dks354
26. Banla LI, Salzman NH, Kristich CJ. Colonization of the mammalian intestinal tract by enterococci. Curr Opin Microbiol. 2019;47:26–31. doi:10.1016/j.mib.2018.10.005
27. Lee T, Pang S, Abraham S, et al. Antimicrobial-resistant CC17 Enterococcus faecium: the past, the present and the future. J Glob Antimicrob Resist. 2019;16:36–47. doi:10.1016/j.jgar.2018.08.016
28. Sparo M, Delpech G, Garcia Allende N. Impact on public health of the spread of high-level resistance to gentamicin and vancomycin in enterococci. Front Microbiol. 2018;9:3073. doi:10.3389/fmicb.2018.03073
29. Nordmann P, Dortet L, Poirel L. Carbapenem resistance in Enterobacteriaceae: here is the storm! Trends Mol Med. 2012;18(5):263–272. doi:10.1016/j.molmed.2012.03.003
30. Zhang Y, Yao Z, Zhan S, et al. Disease burden of intensive care unit-acquired pneumonia in China: a systematic review and meta-analysis. Int J Infect Dis. 2014;29:84–90. doi:10.1016/j.ijid.2014.05.030
31. Klein EY, Van Boeckel TP, Martinez EM, et al. Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proc Natl Acad Sci U S A. 2018;115(15):E3463–E3470. doi:10.1073/pnas.1717295115
32. Bush K. Proliferation and significance of clinically relevant beta-lactamases. Ann N Y Acad Sci. 2013;1277:84–90. doi:10.1111/nyas.12023
33. Golli AL, Popa SG, Cara ML, et al. Antibiotic resistance pattern of pathogens isolated from pediatric patients during and after the COVID-19 pandemic. Antibiotics. 2024;13(10). doi:10.3390/antibiotics13100966.
34. Duru C, Olanipekun G, Odili V, et al. Molecular characterization of invasive Enterobacteriaceae from pediatric patients in Central and Northwestern Nigeria. PLoS One. 2020;15(10):e0230037. doi:10.1371/journal.pone.0230037
35. Peirano G, Pitout JDD. Extended-spectrum beta-lactamase-producing Enterobacteriaceae: update on molecular epidemiology and treatment options. Drugs. 2019;79(14):1529–1541. doi:10.1007/s40265-019-01180-3
36. Lukac PJ, Bonomo RA, Logan LK. Extended-spectrum beta-lactamase-producing Enterobacteriaceae in children: old foe, emerging threat. Clin Infect Dis. 2015;60(9):1389–1397. doi:10.1093/cid/civ020
37. Ye L, Zhang L-Y, Zhao Y, et al. Clinical features and molecular epidemiology of carbapenem-resistant Enterobacterales infection in children. Zhongguo Dang Dai Er Ke Za Zhi. 2022;24(8):881–886. doi:10.7499/j.issn.1008-8830.2203145
38. Grome HN, Grass JE, Duffy N, et al. Carbapenem-resistant and extended-spectrum beta-lactamase-producing enterobacterales in children, United States, 2016-2020. Emerg Infect Dis. 2024;30(6):1104–1114. doi:10.3201/eid3006.231734
39. Han R, Shi Q, Wu S, et al. Dissemination of Carbapenemases (KPC, NDM, OXA-48, IMP, and VIM) among carbapenem-resistant Enterobacteriaceae isolated from adult and children patients in China. Front Cell Infect Microbiol. 2020;10:314. doi:10.3389/fcimb.2020.00314
40. Tamma PD, Aitken SL, Bonomo RA, et al. Infectious diseases society of America 2022 guidance on the treatment of Extended-Spectrum beta-lactamase Producing Enterobacterales (ESBL-E), Carbapenem-Resistant Enterobacterales (CRE), and Pseudomonas aeruginosa with Difficult-to-Treat Resistance (DTR-P. aeruginosa). Clin Infect Dis. 2022;75(2):187–212. doi:10.1093/cid/ciac268
41. Wen SC, Best E, Nourse C. Non-typhoidal Salmonella infections in children: review of literature and recommendations for management. J Paediatr Child Health. 2017;53(10):936–941. doi:10.1111/jpc.13585
42. Dekker JP, Frank KM. Salmonella, Shigella, and yersinia. Clin Lab Med. 2015;35(2):225–246. doi:10.1016/j.cll.2015.02.002
43. Kariuki S, Gordon MA, Feasey N, et al. Antimicrobial resistance and management of invasive Salmonella disease. Vaccine. 2015;33(Suppl 3):C21–9. doi:10.1016/j.vaccine.2015.03.102
44. Jain P, Chowdhury G, Samajpati S, et al. Characterization of non-typhoidal Salmonella isolates from children with acute gastroenteritis, Kolkata, India, during 2000-2016. Braz J Microbiol. 2020;51(2):613–627. doi:10.1007/s42770-019-00213-z
45. Wain J, Hendriksen RS, Mikoleit ML, et al. Typhoid fever. Lancet. 2015;385(9973):1136–1145. doi:10.1016/S0140-6736(13)62708-7
46. Nie D, Hu Y, Chen Z, et al. Outer membrane protein A (OmpA) as a potential therapeutic target for Acinetobacter baumannii infection. J Biomed Sci. 2020;27(1):26. doi:10.1186/s12929-020-0617-7
47. Shi J, Cheng J, Liu S, et al. Acinetobacter baumannii: an evolving and cunning opponent. Front Microbiol. 2024;15:1332108. doi:10.3389/fmicb.2024.1332108
48. Willyard C. The drug-resistant bacteria that pose the greatest health threats. Nature. 2017;543(7643):15. doi:10.1038/nature.2017.21550
49. Fu P, Xu H, Jing C, et al. Bacterial epidemiology and antimicrobial resistance profiles in children reported by the ISPED Program in China, 2016 to 2020. Microbiol Spectr. 2021;9(3):e0028321. doi:10.1128/Spectrum.00283-21
50. Tamma PD, Aitken SL, Bonomo RA, et al. Infectious diseases society of America guidance on the treatment of AmpC beta-lactamase-producing enterobacterales, carbapenem-resistant Acinetobacter baumannii, and Stenotrophomonas maltophilia infections. Clin Infect Dis. 2022;74(12):2089–2114. doi:10.1093/cid/ciab1013
51. Jurado-Martin I, Sainz-Mejias M, McClean S. Pseudomonas aeruginosa: an audacious pathogen with an adaptable arsenal of virulence factors. Int J Mol Sci. 2021;22(6). doi:10.3390/ijms22063128
52. Kessler E. The Secreted Aminopeptidase of Pseudomonas aeruginosa (PaAP). Int J Mol Sci. 2024;25(15):8444. doi:10.3390/ijms25158444
53. Kunz Coyne AJ, El Ghali A, Holger D, et al. Therapeutic strategies for emerging multidrug-resistant pseudomonas aeruginosa. Infect Dis Ther. 2022;11(2):661–682. doi:10.1007/s40121-022-00591-2
54. Kherroubi L, Bacon J, Rahman KM. Navigating fluoroquinolone resistance in Gram-negative bacteria: a comprehensive evaluation. JAC Antimicrob Resist. 2024;6(4):127.
55. Bilal H, Shafiq M, Hou B, et al. Distribution and antifungal susceptibility pattern of Candida species from mainland China: a systematic analysis. Virulence. 2022;13(1):1573–1589. doi:10.1080/21505594.2022.2123325
56. Liu F, Zhong L, Zhou F, et al. Clinical features, strain distribution, antifungal resistance and prognosis of patients with non-albicans candidemia: a retrospective observational study. Infect Drug Resist. 2021;14:3233–3246. doi:10.2147/IDR.S323583
57. Fan X, Xiao M, Zhang D, et al. Molecular mechanisms of azole resistance in Candida tropicalis isolates causing invasive candidiasis in China. Clin Microbiol Infect. 2019;25(7):885–891. doi:10.1016/j.cmi.2018.11.007
58. Chen PY, et al. Correction: Chen et al. mechanisms of azole resistance and trailing in candida tropicalis bloodstream isolates. J Fungi. 2021;7(612).
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.