Back to Journals » Infection and Drug Resistance » Volume 18
Case Report: Nanopore Sequencing-Based Detection of Pulmonary Nocardiosis Caused by Nocardia Otitidiscaviarum in an Immunocompetent Patient
Authors Li D, Liu Q, Xi X, Huang Z, Zhu C, Ding R , Zhang Q
Received 19 November 2024
Accepted for publication 28 March 2025
Published 8 April 2025 Volume 2025:18 Pages 1753—1759
DOI https://doi.org/10.2147/IDR.S507194
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Dan Li,1,* Qing Liu,2,* Xiaotong Xi,2 Zhen Huang,1 Chi Zhu,2 Ran Ding,2 Qi Zhang1
1Department of Respiratory, Xuzhou Central Hospital, Xuzhou, Jiangsu, People’s Republic of China; 2Jiangsu Simcere Diagnostics Co., Ltd., Nanjing Simcere Medical Laboratory Science Co., Ltd., The State Key Laboratory of Neurology and Oncology Drug Development, Nanjing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qi Zhang, Department of Respiratory, Xuzhou Central Hospital, Xuzhou, Jiangsu, People’s Republic of China, Email [email protected]
Purpose: Despite the increasing recognition of nocardiosis, there are still few reported cases of infections caused by Nocardia otitidiscaviarum (N. otitidiscaviarum). This particular strain is categorized as an opportunistic pathogen that predominantly affects individuals with compromised immune systems while seldom infecting immunocompetent individuals. The conventional diagnostic techniques for nocardiosis present difficulties due to their restricted effectiveness.
Case Description: We report on a case study of a 67-year-old male patient who was admitted to the hospital with a respiratory infection caused by N. otitidiscaviarum. Imaging and laboratory tests indicated lung infection, while conventional pathogenetic tests yielded negative results. Furthermore, bronchoalveolar lavage fluid (BALF) was subjected to nanopore sequencing (NS), which identified N. otitidiscaviarum infection after 4h of sequencing. Based on the combined findings from NS results and clinical symptoms, a diagnosis of pulmonary nocardiosis was established. The patient’s symptoms and signs showed improvement following treatment with imipenem cilastatin, linezolid and SMZ/TMP.
Conclusion: This case presents a pulmonary infection caused by N. otitidiscaviarum in an immunocompetent patient, where the pathogen was identified within 4 hours through NS. This rapid and accurate diagnostic approach offers significant advantages for the timely diagnosis of pulmonary nocardiosis.
Keywords: nanopore sequencing, Nocardia otitidiscaviarum, pulmonary nocardiosis, immunocompetent patients, case report
Introduction
The genus Nocardia is a Gram-positive aerobic and slow-growing actinomycete universally detected in soil, decaying vegetation, and water.1,2 Hao Wang et al conducted one of the most extensive studies to date on species diversity and drug resistance of Nocardia species in China in 2020. The study showed that Nocardia farcinica was the most commonly isolated species (39.9%, 176 of 441), followed by Nocardia cyriacigeorgica (28.6%, 126), Nocardia abscessus (6.6%, 29), and Nocardia otitidiscaviarum (5.9%, 26).3 Nocardia otitidiscaviarum (N. otitidiscaviarum), a species within the genus Nocardia, exhibits a lower isolation frequency compared to other Nocardia species. Despite this, it remains capable of causing a range of infections, such as pulmonary,4 cerebral,5 cutaneous,6 and disseminated infections.7 Notably, pulmonary infection is the most frequently observed clinical manifestation. Mazin Barry et al researched the literature on infections caused by N. otitidiscaviarum between 1997 and 2018 and found that more than half of those cases were reported in immunocompromised patients, and eight cases were reported in immunocompetent patients. Individuals with compromised immune system, such as patients suffering from diabetes mellitus, chronic obstructive pulmonary disease, mixed connective tissue disorder, ulcerative colitis, cirrhosis, human immunodeficiency virus (HIV) infection, malignancies, those receiving long-term or high doses of corticosteroid therapy, and recipients of stem cell or solid organ transplants are at an increased risk for infections caused by N. otitidiscaviarum.8 Due to the slow growth rate of Nocardia, visible colonies typically appear within 2–7 days, in certain cases, it may take up to 4–6 weeks for detection, potentially leading to instances of missed identification.9 Therefore, the rapid diagnosis of nocardiosis plays a crucial role in its management. In this study, we present a case of pulmonary infection caused by N. otitidiscaviarum in an immunocompetent individual that was promptly identified using nanopore sequencing (NS) within 4 hours. To our knowledge, this is the first reported instance worldwide where lung infection caused by N. otitidiscaviarum was rapidly detected utilizing nanopore sequencing technology.
Case Presentation
A 67-year-old male who was after suffering from cold 4 days ago presented with cough and expectoration, fever with chest pain, parochial cough, yellow and white sputum, the highest body temperature was 40°C, accompanied by chills, complaining of pain in the left season rib, chest pain was obvious when coughing and deep breathing. Subsequently, he was transferred to the local hospital for antibiotic treatment. Unfortunately, the patient’s condition did not show any signs of improvement. Moreover, a computed tomography (CT) scan of the chest revealed a solid lesion with scattered inflammation in the left lung. The patient has no history of diabetes, tumor, tuberculosis or immunodeficiency. In order to seek further diagnosis and treatment, the patient was admitted to the outpatient clinic of the Xuzhou Central Hospital with a diagnosis of community-acquired pneumonia on April 7.
On admission, the patient was presented with compromised mental health, moderate nutrition status, and exhibited mild periorbital edema upon arrival to the ward. The results of the routine blood tests are presented in detail in Table 1. The nucleic acid test of influenza A and influenza B viruses were negative. Both mycoplasma pneumoniae and chlamydia pneumoniae tests yielded negative results. All five lung cancer tests were normal, no pathogenic bacteria were cultured in multiple sputum smears, sputum cultures, and fungal cultures were in the blood samples tested negative for (1,3)-β-D-glucan assay (G test) and Aspergillus galactomannan (GM test), while the T-cell test for tuberculosis infection (T-spot) yielded a negative result.
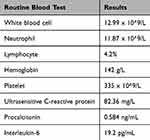 |
Table 1 The Results of the Routine Blood Tests |
After admission, the relevant examinations were enhanced, and a combination therapy of piperacillin tazobactam and moxifloxacin was initiated on April 7th to effectively manage the infection. On April 10th, the patient’s treatment regimen was modified to include a combination of disapenem and moxifloxacin due to elevated body temperature and persistent symptoms. On April 13th, the patient’s treatment regimen was adjusted to a combination of biapenem and vancomycin. The chest enhancement CT revealed the multiple nodules and mass shadow, with uneven enhancement examination observed in both lungs. The trachea and bronchial tubes exhibited the presence of cavities, while the mediastinal septum showed no signs of displacement. Enlarged lymph nodes were observed within the mediastinal septum, accompanied by a small quantity of pleural effusion in the right side of the pleural cavity. The pathology report on April 14th revealed the presence of acute and chronic inflammation accompanied by fibrinous exudation, mechanization, and fibrous hyperplasia. On April 13th, the bronchoalveolar lavage fluid (BALF) was concurrently subjected to cultivation and GM test, both of which yielded negative outcomes.
To identify the causative pathogen, the BALF was subjected to NS on April 14th, and the sample was tested by NS on April 15th. The nucleic acids were extracted using Quick-DNA/RNA Viral Kit-zymo kit. The libraries were prepared using VAHTS Universal End preparation Module for Illumina and VAHTS Universal Adapter Ligation Module for illumina. Library pools were then loaded onto a Gridion×5 (Oxford Nanopore Technologies) sequencer for 4 hours. Clean reads were obtained by removing short reads (length less than 500 bp) and low-quality reads (mean q-score less than 8). Subsequently, reads for the host DNA were removed by aligning to the human reference genome (GRCh38) using minimap2 (Version 2.14-r883). The remaining reads were mapped using the Centrifuge software (version 1.0.4) for taxonomic classification. The remaining sequences were aligned to the microbial genome database (NCBI; https://www.ncbi.nlm.nih.gov/genome) to identify potential pathogens.10 Human alphaherpesvirus 1 and human gammaherpesvirus 4 were detected in the targeted-sequencing results, and N. otitidiscaviarum (14,582 reads), Neisseria subflava (378 reads), Streptococcus mitis (54 reads) and Human gammaherpesvirus 4 (2 reads) were identified as the potential pathogen (Table 2). Neisseria subflava and Streptococcus mitis were considered a part of the normal flora in the respiratory tract, while Human gammaherpesvirus 4 virus is a prevalent human carrier virus, neither of them takes into account the role of pathogenic bacteria. The accuracy of N. otitidiscaviarum was further validated by performing a specific polymerase chain reaction (PCR) analysis on the remaining samples. The PCR products were assessed for their specificity in targeting the region of interest in N. otitidiscaviarum Primers (CTGACCGTACCCAGTCGTG and CGCAGTGACGGAACATATATTTCG) were designed specifically for this target region. The validation process yielded a positive outcome (Figure 1). In conjunction with the results obtained from NS analysis, PCR result and other clinical tests, the presence of N. otitidiscaviarum infection was confirmed.
 |
Table 2 The Pathogens and Reads Detected by NS in BALF Sample |
 |
Figure 1 QPCR verification results of N.otitidiscaviarum. blue line: negative control; green line: positive control; red line: the pus sample of the patient. |
The antimicrobial regimen was modified to include imipenem cilastatin in combination with SMZ/TMP on April 16th. On April 20th, the patient remained febrile, and linezolid was administered in addition to the original antimicrobial drugs. Subsequent CT scans revealed partial absorption improvement. The patient’s body temperature showed improvement, and there was an enhancement in the CT lung absorption on April 30th. The patient was discharged from the hospital on May 19th and continued to receive linezolid and SMZ/TMP treatment. There was no presence of fever or abnormal blood glucose levels. The administration of hypoglycemic drugs was discontinued, and CT absorption showed improvement (Figure 2). Intermittent administration of linezolid was implemented on June 14th. The entire treatment process is summarized in Figure 3.
 |
Figure 2 Computed tomography (CT) scan of the lung on May 19th. |
 |
Figure 3 The treatment timeline of the patient. |
Discussion
N. otitidiscaviarum is found in soil, decomposing vegetation, and other organic matter, as well as in fresh and saltwater.11 In 1924, N. otitidiscaviarum was first recognized by Snijders from a Sumatran cavy or guinea pig with ear disease.12 Infections caused by N. otitidiscaviarum are rare compared to other Nocardia genera, and human infections were reported until the middle 1960s.13 Chen et al reported a case of pulmonary infection caused by N. otitidiscaviarum that the patient was a cotton farmer who had close contact with the soil.14 Moreover, Steven et al suggested that N. otitidiscaviarum can cause skin infections which were traced back to a possible Iatrogenic infection caused by a PICC catheter.6 The patient’s previous engagement in farming prior to the onset of the disease prompted us to investigate the potential source of infection, leading us to consider the possibility of respiratory infection with N. otitidiscaviarum originating from soil.
The diagnosis of pulmonary nocardiosis caused by N. otitidiscaviarum poses challenges due to the non-specificity of clinical indications, imaging findings, and laboratory tests. Additionally, Venkataramana Kandi et al reported the clinical diagnosis of pulmonary nocardiosis poses challenges due to its presentation resembling other respiratory pathogens, including members of Actinomycetes and Mycobacterium tuberculosis.9 The cytomorphologic manifestations of pulmonary nocardiosis have been described by Ridhi Sood et al as acute and chronic inflammatory infiltrates accompanied by necrosis, but without definite granulomas.15 Despite the considerable diversity in CT manifestations of pulmonary Nocardiosis, nodules, patchy solid lesions and cavities are consistently observed, particularly when accompanied by extrapulmonary infections such as those affecting the brain and subcutaneous tissue.16 Meanwhile, laboratory tests for pulmonary nocardiosis lack specificity. Specifically, the patient exhibited elevated levels of white blood cells (WBC), neutrophils, procalcitonin (PCT), and C-reactive protein (CRP). Additionally, the CT imaging revealed the presence of cavities and nodules indicative of lung infection.
Due to the nonspecific signs and symptoms of Nocardia infection, diagnosing Nocardiosis remains a challenge. While Gram staining is a relatively rapid method in traditional methods, bacterial culture serves as the gold standard. However, it is important to note that Nocardia exhibits a relatively slow growth rate. At 37°C, aerobic cultures typically require 2 to 7 days to produce visible colonies.1 Consequently, relying solely on phenotypic tests, such as morphological observations, for the accurate classification and identification of Nocardia is inadequate. Therefore, it is imperative to employ a combination of phenotypic tests and molecular biology technologies for the identification of Nocardia.17 Laurent et al described a PCR method by using Nocardia-specific primers to differentiate Nocardia isolates in 1999.18 Additionally, Shaozeng Li et al employed 16s RNA sequencing to diagnose three cases of bone infections caused by Nocardia.19 Masahiro Toyokawa et al demonstrated that MALDI-TOF MS is a quick, easy and reliable method for the species/complex identification of Nocardia species.20 In this case, multiple sputum cultures yielded negative results, and other etiological tests also showed no evidence of infection. N. otitidiscaviarum was detected in BALF within 4 hours using nanopore sequencing, and the diagnosis was subsequently confirmed through PCR validation. Consequently, nanopore sequencing has demonstrated the capability to discern individual nucleotides through the measurement of alterations in electrical conductivity as DNA molecules traverse the pore. In contrast to prevailing major technologies, nanopore sequencing operates independently of sequencing by synthesis.21 The device boasts a low capital cost, unparalleled portability, and real-time data production capabilities.22 With long read lengths (10,000–50,000 bases), direct sequence reading without amplification or modification ease to operation in various environments, and its potential as a clinical platform, NS is an attractive option.23 However, it is rather difficult to confirm the actual pathogens responsible for infection based on NS results which are the only adjunctive methods for the screening of causative organisms. Clinical diagnosis needs more clinical experience and other laboratory tests such as culture and PCR validation for comprehensive judgment.
Regarding the treatment of nocardiosis, Hao Wang et al demonstrated that linezolid exhibited susceptibility against all Nocardia strains, followed by amikacin (99.3%; 3 of 7 Nocardia wallacei were amikacin-resistant) and TMP-SMX (99.1%; all 4 resistant strains belong to Nocardia farcinica). The antibiotic resistance profiles of other Nocardia species exhibited significant variations, highlighting the necessity for accurate species identification and/or antibiotic susceptibility testing prior to the administration of these antibiotics.3 In the absence of a drug susceptibility profile, clinicians should adopt a strategic approach to antibiotic selection, with treatment options being refined based on species identification and subsequent determination of susceptibilities.24 In this case, the patient had empirically administered antibiotics to manage the infection prior to receiving a definitive diagnosis. Treatment was adjusted to imipenem cilastatin combined with SMZ/TMP, and linezolid was added due to persistent fever, and partial improvement in lung absorption compared to the previous results. The temperature was stabilized on April 30th, and he was discharged from the hospital on May 19th. Subsequently, hypoglycemic medication was discontinued, and intermittent administration of linezolid commenced on June 14th. Follow-up assessments revealed normal results.
In summary, the lack of specificity in clinical features, laboratory tests, and imaging tests challenges for early diagnosis of pulmonary nocardiosis infection. Moreover, definitive diagnosis of pulmonary nocardiosis relies on pathogenetic tests; therefore, the utilization of molecular diagnostic methods is recommended to facilitate diagnosis when traditional pathogenetic tests provide insufficient clues. The first detection of N. otitidiscaviarum was achieved through three-generation nanopore sequencing in this study. This breakthrough technology holds immense potential for various domains including disease diagnosis, drug target discovery, pathological research, species protection and SARS-CoV-2 detection. Nanopore technology possesses the advantages of compact size and convenient portability, obviating the need for biochemical reagents, and direct reading through physical means. Although NS technology offers the advantages of rapidity and precision, its clinical application value requires validation in larger cohorts to be fully established. This study demonstrates that the implementation of NS technology has the potential to offer clinicians more expeditious and timely outcomes compared to conventional microbial detection methods, thereby reducing diagnostic time and significantly enhancing patient treatment.
Data Sharing Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://ngdc.cncb.ac.cn/omix: accession No. OMIX005011.
The patient data used to support the findings of this study are included in the article.
Ethical Approval
No specific ethics committee approval was required for this study.
Consent for Publication
Written informed consent was obtained from the individual, for the publication of any potentially identifiable images or data included in this article.
Acknowledgments
The authors would like to thank their hospital colleagues and the patient.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Brown-Elliott BA, Brown JM, Conville PS, Wallace RJ. Clinical and laboratory features of the Nocardia spp. based on current molecular taxonomy. Clin Microbiol Rev. 2006;19(2):259–282. doi:10.1128/CMR.19.2.259-282.2006
2. Huang L, Chen X, Xu H, et al. Clinical features, identification, antimicrobial resistance patterns of Nocardia species in China: 2009–2017. Diagn Microbiol Infect Dis. 2019;94(2):165–172. doi:10.1016/j.diagmicrobio.2018.12.007
3. Wang H, Zhu Y, Cui Q, et al. Epidemiology and antimicrobial resistance profiles of the Nocardia Species in China, 2009 to 2021. Microbiol Spectrum. 2022;10(2):e0156021. doi:10.1128/spectrum.01560-21
4. Mahgoub A, Gumaa SA, Joseph MR, et al. Pulmonary nocardiosis caused by Nocardia otitidiscaviarum in an adult asthmatic female patient: the presence of acid-fast branching filaments is always significant. South African Med J. 2016;107(1):43–45. doi:10.7196/SAMJ.2016.v107.i1.12006
5. Tajima K, Terada T, Okuyama S, et al. Nocardia otitidiscaviarum meningitis in a diffuse large B-cell lymphoma patient with CD4-positive lymphocytopenia and persistent oligoclonal CD8-positive lymphocytes in the peripheral blood. Int J Clin Exp Pathol. 2018;11(1):455–461.
6. Douedi S, Fadhel M, Patel S. Iatrogenic Nocardia otitidiscaviarum after PICC line placement. IDCases. 2020;22:e00986. doi:10.1016/j.idcr.2020.e00986
7. Sharma M, Gilbert BC, Benz RL, Santoro J. Disseminated Nocardia otitidiscaviarum infection in a woman with sickle cell anemia and end-stage renal disease. Am J Med Sci. 2007;333(6):372–375. doi:10.1097/MAJ.0b013e318065ab26
8. Barry M, AlShehri S, Alguhani A, et al. A fatal case of disseminated nocardiosis due to Nocardia otitidiscaviarum resistant to trimethoprim-sulfamethoxazole: case report and literature review. Ann Clin Microbiol Antimicrobials. 2022;21(1):17. doi:10.1186/s12941-022-00511-9
9. Kandi V. Human Nocardia infections: a review of pulmonary nocardiosis. Cureus. 2015;7(8):e304. doi:10.7759/cureus.304
10. Ma L. Illumina and Nanopore sequencing in culture-negative samples from suspected lower respiratory tract infection patients. Front Cell Infect Microbiol. 2024;14:1230650. doi:10.3389/fcimb.2024.1230650
11. Lerner PI. Nocardiosis. Clin Infect Dis. 1996;22(6):891–905. doi:10.1093/clinids/22.6.891
12. Snijders EP. Cavia-scheefkopperij, een nocardiose. Geneeskundig Tijdschrift Nederlandsch-Indie. 1924;64:85–87.
13. Clark NM, Braun DK, Pasternak A, Chenoweth CE. Primary cutaneous Nocardia otitidiscaviarum infection: case report and review. Clin Infect Dis. 1995;20(5):1266–1270. doi:10.1093/clinids/20.5.1266
14. Liu C, Feng M, Zhu J, Tao Y, Kang M, Chen L. Severe pneumonia due to Nocardia otitidiscaviarum identified by mass spectroscopy in a cotton farmer: a case report and literature review. Medicine. 2017;96(13):e6526. doi:10.1097/MD.0000000000006526
15. Sood R, Tyagi R, Selhi PK, Kaur G, Kaur H, Singh A. Role of FNA and special stains in rapid cytopathological diagnosis of pulmonary nocardiosis. Acta Cytologica. 2018;62(3):178–182. doi:10.1159/000488134
16. Su R, Wen Y, Liufu Y, Pan X, Guan Y. The computed tomography findings and follow-up course of pulmonary nocardiosis. J Comput Assist Tomography. 2023;47(3):418–423. doi:10.1097/RCT.0000000000001439
17. Liu A, Liu X, Lu Y, et al. Two chronically misdiagnosed patients infected with Nocardia cyriacigeorgica accurately diagnosed by whole genome resequencing. Front Cell Infect Microbiol. 2022;12:1032669. doi:10.3389/fcimb.2022.1032669
18. Laurent FJ, Provost F, Boiron P. Rapid identification of clinically relevant Nocardia species to genus level by 16S rRNA gene PCR. J Clin Microbiol. 1999;37(1):99–102. doi:10.1128/JCM.37.1.99-102.1999
19. Li S, Shi Y, Xiong Y, Liu Y. Diagnosis of rare bone infection caused by Nocardia by 16S rRNA gene sequencing. Infect Drug Resist. 2023;16:347–353. doi:10.2147/IDR.S392342
20. Toyokawa M, Ohana N, Ueda A, et al. Identification and antimicrobial susceptibility profiles of Nocardia species clinically isolated in Japan. Sci Rep. 2021;11(1):16742. doi:10.1038/s41598-021-95870-2
21. Olasagasti F, Lieberman KR, Benner S, et al. Replication of individual DNA molecules under electronic control using a protein nanopore. Nat Nanotechnol. 2010;5(11):798–806. doi:10.1038/nnano.2010.177
22. Laver T, Harrison J, O’Neill PA, et al. Assessing the performance of the Oxford nanopore technologies MinION. Biomol Detect Quantification. 2015;3:1–8. doi:10.1016/j.bdq.2015.02.001
23. Petersen LM, Martin IW, Moschetti WE, Kershaw CM, Tsongalis GJ. Third-generation sequencing in the clinical laboratory: exploring the advantages and challenges of nanopore sequencing. J Clin Microbiol. 2019;58(1):e01315–19. doi:10.1128/JCM.01315-19
24. Fu K, White K, Ramaniuk A, Kollu V, Urbine D. Manifestations and management of trimethoprim/sulfamethoxazole-resistant Nocardia otitidiscaviarum infection. Emerg Infect Dis. 2023;29(6):1266–1267. doi:10.3201/eid2906.221854
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

