Back to Journals » Journal of Pain Research » Volume 18
Causal Relationship Between Psychosocial Factors and Neck Pain: A Two-Sample Mendelian Randomization Study
Authors Liang H, Wu Q, Yang S, Zhang S, Miao J, Jin H , Wang X
Received 10 December 2024
Accepted for publication 14 April 2025
Published 25 April 2025 Volume 2025:18 Pages 2191—2201
DOI https://doi.org/10.2147/JPR.S508287
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Jonathan Greenberg
Haibo Liang,1,2,* Qihang Wu,1,2,* Shu Yang,1,2,* Shuhao Zhang,1,2 Jiansen Miao,1,2 Haiming Jin,1,2 Xiangyang Wang1,2
1Division of Spine Surgery, Department of Orthopaedics, The Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University, Wenzhou, People’s Republic of China; 2School of The Second Clinical Medical Sciences, Wenzhou Medical University, Wenzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiangyang Wang, Email [email protected]; Haiming Jin, Email [email protected]
Purpose: Neck pain (NP) is a multifactorial disorder that leads to severe disability. This study aimed to investigate whether potential risk factors have a causal effect on NP at the genetic level using a two-sample Mendelian randomization (MR) analysis.
Methods: Summary-level data for potential risk factors, including distress, anxiety disorder, depression, mood, sleep disorder, loneliness, education, alcohol consumption, smoking, time spent using the computer, and physical activity, as well as NP, were obtained from multiple large-scale Genome-Wide Association Studies (GWAS). Instrumental variables (IVs) were extracted from these datasets. We employed inverse variance weighting (IVW), weighted median, and MR-Egger regression methods to assess causal effects. Heterogeneity was evaluated using MR-Egger regression and IVW, while horizontal pleiotropy was assessed using MR-PRESSO analysis and MR-Egger regression.
Results: The IVW results showed that major depressive disorder (OR = 1.51, 95% CI: 1.15, 1.98, p = 3.40× 10− 3) and experiencing mood swings (OR = 2.73, 95% CI: 1.57, 4.75, p = 3.86× 10− 4) were positively associated with NP and years of schooling (OR = 0.504, 95% CI: 0.410, 0.619, p = 6.55× 10− 11) was negatively associated with NP. Additionally, loneliness (OR = 16.0, 95% CI: 1.29– 198, p = 0.0307) showed a suggestive association with NP. As for the other factors we did not find a clear causal relationship (All p-values > 0.05).
Conclusion: This two-sample MR study provides genetic evidence supporting a causal relationship between major depressive disorder, mood swings, and years of schooling with NP, while loneliness showed a potential association. These findings highlight the critical role of psychosocial factors, such as depression, mood swings, and education level, in the prevention and management of NP. Our results may offer new insights for clinicians to develop targeted intervention strategies aimed at reducing the incidence of NP.
Keywords: genome-wide association study, Mendelian randomization analysis, neck pain, psychosocial factor
Introduction
Neck pain (NP) is the fourth leading cause of disability worldwide, imposing substantial life and financial burdens on patients.1 Globally, the age-standardized point prevalence and incidence of NP in 2019 were estimated to be 2696.5 per 100,000 and 579.1 per 100,000, respectively.2 At the national level, NP also poses considerable economic and health burdens. According to healthcare spending data from the United States (1996–2016), the healthcare costs associated with low back pain and NP reached $13.4 billion in 2016, ranking as the highest expenditure among 154 health conditions.3 Similarly, a cross-sectional study conducted in Singapore revealed that NP significantly reduces quality of life and increases disability, further highlighting the substantial burden of NP.4
NP is a multifactorial condition, with risk factors predominantly related to psychosocial factors.5 The primary psychological factors associated with NP include stress, pain, anxiety, mood and emotions, cognitive factors, and pain-related behaviors. Additionally, other contributing factors, such as sleep disturbances, social support, work-related factors, and biological factors, have also been identified as potential contributors to NP.6,7 Current clinical guidelines emphasize a biopsychosocial approach, incorporating interventions such as back school programs or therapeutic exercise regimens to address these factors.8,9 Although these strategies have demonstrated effectiveness in managing NP, and numerous risk factors for NP have been identified in observational studies, further evidence is needed to determine the relative contribution of genetic predisposition versus environmental factors (eg, education, exercise) to the development and persistence of NP. This is particularly important because pain conditions and pain perception are often influenced by genetic susceptibility.10 Understanding this distinction is crucial for developing targeted interventions that integrate genetic predisposition with modifiable lifestyle factors in NP management.
Observational studies are commonly used to explore the relationship between psychosocial factors and NP. However, these studies are prone to confounding bias and reverse causality, which limit their ability to establish causal relationships. While randomized controlled trials (RCTs) are considered the gold standard for assessing causality, conducting large-scale RCTs is often impractical for multifactorial conditions such as NP. Mendelian randomization (MR) is a genetic instrumental variable (IV) approach that investigates the causal relationship between an exposure and an outcome by leveraging genetic variation as an IV for the exposure.11 The random allocation of alleles at conception mitigates confounding effects within the population, and since genotype determination precedes disease onset, reverse causality is effectively minimized.12,13 Madrid-Valero and Andreucci’s study identified a significant association between chronic NP and sleep quality, highlighting the influence of both genetic and environmental factors.14,15 Similarly, Tang et al demonstrated a bidirectional causal relationship between depression and NP through MR analysis.16 However, the causal roles of other psychosocial and individual-related factors in NP remain incompletely established.
The aim of this study is to use MR to investigate whether psychosocial factors, such as major depressive disorder, mood swings, loneliness, and years of schooling, have a potential causal effect on the occurrence of NP at the genetic level. Based on this background, we hypothesize that these psychosocial factors exert a potential causal impact on NP, possibly mediated through genetic mechanisms.
Methods
Study Design and Data Sources
To investigate the genetic causality between risk factors and NP, a two-sample MR analysis was conducted in this study. The selected risk factors included psychological factors (distress, anxiety disorder, depression, mood swings), sleep disorders, social support (loneliness), education, alcohol consumption, smoking, time spent using the computer, and physical activity, which were used as exposure variables. Genetic variants associated with these exposure factors were selected as IVs. MR was then used to analyze the potential causal relationships between these risk factors and NP. Summary statistics for both risk factors and NP were obtained from the IEU Open Genome-Wide Association Studies (GWAS) database, the FinnGen database, and the UK Biobank database.17–19 The corresponding details and data sources are listed in Table 1.
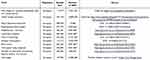 |
Table 1 Summary of Data From European Genome-Wide Association Studies of Associated Risk Factors and NP |
In this study, we focused on psychosocial and lifestyle-related risk factors, which have been widely examined in observational research as potential contributors to NP.6 However, work-related stress and occupational physical activity, both of which have been previously associated with NP, were not included. This decision was primarily influenced by data availability from large-scale GWAS studies, which may not have included these variables. Additionally, the aim of this study was to assess the causal role of genetic factors, and the selected risk factors have been well-established in the literature as being closely linked to genetic predisposition and pain perception.
Genetic Instrumental Variables (IVs)
The single-nucleotide polymorphism (SNP) selection process followed six sequential steps: 1. Initial Extraction: SNPs associated with exposures at genome-wide significance (P < 5 × 10−8) were extracted from GWAS summary statistics. 2. Linkage Disequilibrium (LD) Clumping: To ensure independence, SNPs within 5000 kb were clumped using a stringent R2>0.01 threshold. 3. Minor Allele Frequency (MAF) Filtering: SNPs with MAF < 0.01 were excluded, and data for the above-selected SNPs were subsequently extracted from the GWAS summaries of the outcome traits. 4. Proxy SNP Replacement: proxy SNPs with high LD (R2>0.8) were selected to replace them based on the 1000 genomes project. 5. Palindromic SNP Removal: Ambiguous SNPs (A/T or C/G alleles) with intermediate allele frequencies (MAF>0.42) were excluded to avoid strand-mismatch errors. 6. Weak Instrument Removal: SNPs with weak instrument strength were excluded by calculating F-statistics20 (F = β²exposure / SE²exposure) and removing those with F < 10. A detailed flowchart of SNP exclusion (Figure 1) and the final list of SNPs (Table S1).
 |
Figure 1 Flow chart of MR analysis steps in this study. |
Three assumptions had to be satisfied before IVs could be analyzed for MR. 1. Relevance Assumption: IVs were selected based on their strong association with the exposure variables (eg, psychosocial factors like major depressive disorder and mood swings). For example, SNPs associated with major depressive disorder were identified from the GWAS summary data and included as IVs in this analysis; 2. Independence Assumption: To avoid confounding, we ensured that the selected IVs were not associated with any potential confounders that could influence both the exposure and the outcome (NP). We removed SNPs with known pleiotropic effects or any that were associated with other risk factors outside the exposure of interest; 3. Exclusion-Restriction Assumption: The IVs selected can only affect the outcome (NP) through their association with the exposure factors. This was ensured by carefully filtering the SNPs and excluding those with potential direct effects on NP outside of the exposure pathway.11 The rigorously selected SNPs were then used as IVs for two-sample MR analysis.
Mendelian Randomization (MR) Analyses
For the MR analysis, after screening instrumental variables, this study evaluated the causal relationships between 11 risk factors and neck pain (NP) using three methods: inverse-variance weighted (IVW),21 MR-Egger regression,22 and the weighted median approach.23 IVW, one of the most widely used MR methods, combines the Wald ratios of SNPs through a meta-analysis approach to estimate the effect of exposure on the outcome.21 We employed fixed-effect IVW as the primary method to estimate the causal effects of exposures on outcomes.
Sensitivity analyses were conducted to address pleiotropy and heterogeneity: 1. Horizontal pleiotropy: This was assessed using the MR-Egger intercept and MR-PRESSO global test, with a p-value < 0.05 indicating significant pleiotropy. 2. Heterogeneity: This was quantified using Cochran’s Q statistic. A p-value < 0.05 was considered indicative of significant heterogeneity, and IVs exhibiting significant heterogeneity were analyzed using a random-effects IVW model.24 3. Influential SNP detection: We performed a leave-one-out analysis to identify influential SNPs. This method involves sequentially removing each SNP, calculating the meta-effect of the remaining SNPs, and evaluating whether the results change significantly after excluding a particular SNP. If the exclusion of a specific SNP results in a substantial change in the results, it suggests that this SNP has a strong influence on the outcome. The MR analysis procedure is illustrated in Figure 1.
In this study, we compared the relationships between 11 exposure factors and NP. To account for multiple comparisons and reduce the risk of Type I error, we applied the Bonferroni correction. This method is particularly effective for ensuring a stringent threshold for statistical significance when testing multiple hypotheses simultaneously. Given that we investigated causal relationships between multiple psychosocial factors and NP, the Bonferroni correction was the most appropriate choice to maintain the integrity of our findings. The adjusted p-value threshold was set at 0.00455 (0.05/11) to account for the 11 hypotheses tested in this study.25 After Bonferroni correction, a p-value < 0.00455 was considered statistically significant, while a p-value between 0.00455 and 0.05 was considered to indicate suggestive significance. For the analysis, we used the TwoSampleMR package (version 0.5.6) and the MRPRESSO package (version 1.0) in R (version 4.2.2).
Results
Selection of Instrumental Variables
The independent SNPs obtained from the GWAS data of all exposure factors after the clumping process are listed in Table S1. The selected SNPs were further filtered according to the procedure described in the Methods section. Specifically, the following SNPs were excluded: 1. SNPs without corresponding matches in the NP GWAS summary data; 2. Palindromic SNPs; 3. SNPs for which proxy SNPs could not be identified. As a result, the number of SNPs included in the final MR analysis may be smaller than the initial number extracted, as detailed in Figure 2. Additionally, all exposure-related IVs had F-statistics greater than 10, indicating a low likelihood of weak instrument bias.
 |
Figure 2 Mendelian randomization estimate results of exposures on neck pain. |
Causal Relationship Between Exposure Factors and NP
Table 2 contains the MR results of multiple methods to assess exposure factors on NP. As shown in Table 2, Major Depressive Disorder was positively associated with NP at the genetic level (IVW: OR (95% CI) 1.51 (1.15, 1.98), p = 3.40×10−3; Weighted median: OR (95% CI) 1.67 (1.12, 2.51), p = 0.0128); Experiencing mood swings was positively associated with NP at the genetic level (IVW: OR (95% CI) 2.73 (1.57, 4.75), p = 3.86×10−4; Weighted median: OR (95% CI) 2.62 (1.15, 5.96), p = 0.0214); Loneliness was positively associated with NP at the genetic level (IVW: OR (95% CI) 16.0 (1.29, 198), p = 0.0307); Years of schooling was negatively associated with NP at the genetic level (IVW: OR (95% CI) 0.504 (0.410, 0.619), p=6.55×10−11; Weighted median: OR (95% CI) 0.525 (0.388, 0.709), p = 2.66×10−5). When tested using Bonferroni-corrected p-values (p<0.00417), Major Depressive Disorder, Experiencing mood swings, and Years of schooling still had a causal effect on NP.
 |
Table 2 MR Estimates from Different Methods of Assessing the Causal Effect of Exposure Factors on NP |
While loneliness exhibited a suggestive association with NP, the wide confidence interval indicates limited precision in this estimate. This uncertainty likely stems from the relatively small sample size of the loneliness GWAS (N= 82,436) and the limited number of instrumental variables meeting genome-wide significance. Consequently, these results should be interpreted cautiously and validated in larger cohorts.
We did not find significant results in heterogeneity tests and horizontal pleiotropy analyses; however, the results of MR-Egger regression indicated the presence of pleiotropy in the IVs of sleep disorders (p=0.036982097), suggesting that the IVs may be associated with some confounding factors. Detailed results are provided in Tables S2 and S3. Forest plots of MR results analysis are shown in Figure 2. Effect sizes of SNPs on exposure and outcome are illustrated in scatter plots (Figure S1). The leave-one-out analysis results are presented in Figure S2. A potentially influential SNP (rs113851554) was identified in the analysis of sleeplessness on NP. After removing this SNP, the MR results were as follows: IVW: 2.54 (1.15, 5.61), p= 0.0207; MR Egger: 2.92 (0.0496, 172), p= 0.609; Weighted median: 2.78 (0.907, 8.51), p= 0.0735). These results are inconsistent with the original causal estimates, indicating that this SNP has a significant influence on the association between sleeplessness and NP. Therefore, we cannot draw robust or definitive conclusions regarding this relationship.
Discussion
The aim of this study was to evaluate the causal relationships between psychosocial factors and individual-related risk factors for NP. We obtained summary statistics from publicly available GWAS databases and performed two-sample MR analyses to assess the causal effects of exposures on outcomes. The results demonstrated that major depressive disorder and mood swings were positively associated with NP, while years of schooling showed a negative association. Additionally, the relationship between loneliness and NP reached suggestive significance.
Psychological factors, including distress, anxiety, depression, and emotional problems, are important risk factors for NP.6 Numerous studies have reported significant associations between psychological distress and NP or other spinal pain conditions.26,27 For example, Lee et al demonstrated that psychological distress significantly mediates the relationship between pain and disability in patients with low back pain or NP.28 However, our findings did not support a causal effect of distress on NP. A meta-analysis revealed that anxiety and depressive symptoms are associated with a higher prevalence of NP.29 Additionally, depression has been shown to have a bidirectional causal relationship with neck/shoulder pain,16 which is consistent with our study’s demonstration of a causal link between depression and NP. Although anxiety and NP are often associated, Myburgh et al suggested that NP is not consistently linked to anxiety.30 Our results, which showed no causal effect of anxiety on NP, partially contradict the findings of observational studies. One possible reason for this discrepancy is the presence of reverse causality, where NP might lead to increased anxiety rather than anxiety causing NP. However, due to the lack of sufficient IVs from the GWAS data, we could not perform a bidirectional MR analysis to further explore this relationship. Moreover, previous research showed that certain specific types of anxiety disorders are more strongly correlated with spinal pain compared to other anxiety disorders.6 In particular, generalized anxiety disorder (GAD) and post-traumatic stress disorder (PTSD) have shown higher comorbidity rates with spinal pain, including NP, compared to social anxiety disorder or panic disorder/agoraphobia. However, the specific mechanisms underlying the association between anxiety disorders and NP remain incompletely understood. Therefore, we speculate that the non-significant result may be due to the heterogeneity of anxiety disorders included in the GWAS dataset, suggesting that future MR studies focusing on specific anxiety subtypes could provide clearer insights into this association. From a clinical perspective, these findings suggest that targeted psychological interventions for patients with GAD or PTSD may be beneficial in managing NP. Further studies are warranted to explore the underlying mechanisms and to determine if intervention strategies for anxiety disorders can improve NP outcomes. A prospective study demonstrated that the combination of multiple risk factors, including loneliness, increases the likelihood of NP in young adulthood.31 Our results suggest a potential link between social loneliness and NP. This finding has implications for the prevention of NP in adolescents.
We identified a causal effect of mood swings on neck pain (NP), a factor not previously reported in the literature. This finding may have important implications for the prevention and treatment of NP. The observed causal relationship between mood swings and NP is a novel finding that warrants further investigation. One potential mechanism involves the dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, where frequent mood fluctuations may lead to chronic stress responses, increased cortisol levels, and heightened pain sensitivity.32 Additionally, mood swings may influence pain perception through alterations in neurotransmitter systems (eg, serotonin and dopamine), which play critical roles in both mood regulation and nociceptive processing.33 Behaviorally, individuals experiencing mood swings may engage in maladaptive coping strategies, such as poor posture, physical inactivity, or increased muscle tension, all of which can contribute to NP. These potential pathways underscore the importance of addressing emotional instability in NP prevention and management strategies. Future research should explore these mechanisms in depth to guide targeted interventions.
A significant association has been found between sleep disorders and NP. Results from a twin study indicated that the association between sleep quality and chronic NP is partially influenced by genetic factors,15 while another study suggested that environmental factors play a more substantial role.14 Our findings suggested no causal effect of sleep disorders on NP; however, this result may have been influenced by confounding factors and requires further investigation. Additionally, we identified a potentially influential SNP (rs113851554) that may play a significant role in the association between sleep disorders and NP.
Inadequate education level, low social support, and physical activity are associated with NP.34–36 Two randomized controlled trials (RCTs) demonstrated the potential benefits of pain neuroscience education combined with neck/shoulder exercises, as well as exercise alone, in adolescents with chronic idiopathic neck pain (CINP).37,38 However, our study identified only a causal effect of years of schooling on NP. The relationship between education and NP in our study differs from the results of RCTs. This difference may be attributed to the fact that RCTs primarily evaluate the effects of educational interventions, such as pain neuroscience education, while our study examines the broader effect of education level (ie, years of schooling) on NP risk through genetic factors. While RCTs focus on the direct impact of interventions on pain management, our study explores how education level, as a proxy for socioeconomic and psychosocial factors, may influence the genetic risk of NP. Thus, while both approaches are valuable, they address different aspects of the relationship between education and NP.
The effects of physical activity on NP show considerable variability across systematic reviews in recent years. Luc et al reported low-quality evidence suggesting that leisure-time physical activity among workers reduces the occurrence and persistence of nonspecific neck pain (NSNP),39 whereas Øverås et al found that physical activity in blue-collar workers increased the risk of NP and low back pain (LBP).40 In contrast, Jahre et al concluded that physical activity in adolescents is not associated with NP.41 A recent systematic review indicated that moderate-intensity aerobic exercise three times per week may benefit patients with NSNP.42 Although previous studies have confirmed that exercise can reduce pain and disability in patients with NP, further research is needed to determine the optimal type, intensity, frequency, and target populations for exercise interventions.43
Regarding time spent using computers, a systematic review found limited evidence for a causal relationship between computer work and shoulder/neck disorders,44 and our results also indicate no causal effect of computer use on NP. Existing MR studies suggest a bidirectional causal relationship between smoking/alcohol consumption and chronic back pain,45 as well as an association between smoking and an increased risk of LBP.46 However, we did not observe similar causal associations for NP.
Given the causal relationships between psychosocial factors (such as depression, mood swings, loneliness, and years of education) and NP identified in our study, it is essential to strengthen mental health screening and incorporate psychological interventions as potential treatment strategies for NP prevention and management. Specifically, individuals with genetic predispositions to depression or mood disorders may benefit from early mental health screening and timely interventions, which could help alleviate psychological distress and reduce the risk of chronic pain. Considering the effectiveness of education and therapeutic exercise in pain management, targeted interventions—such as cognitive-behavioral therapy (CBT) and patient education programs (eg, back schools)—should be integrated into NP prevention and treatment strategies.8,47 Moreover, our findings align with international guidelines advocating for a biopsychosocial approach to NP. For example, the WHO emphasizes addressing psychosocial factors (eg, emotional distress, anxiety, depression, and poor academic performance) in multidisciplinary care, and our genetic evidence further supports prioritizing mental health screening and education in NP management.48 Similarly, the Practice Guideline of the Orthopaedic Section of the American Physical Therapy Association (APTA) recommends enhanced monitoring of psychosocial functioning in patients with NP.49 Future research should investigate the effectiveness of personalized interventions addressing these psychosocial determinants.
While our MR analysis supports a causal relationship between psychosocial factors and NP, it is important to recognize that genetic predisposition interacts with environmental factors, such as occupational stress, socioeconomic status, and lifestyle habits. This interplay suggests that while genetic findings provide valuable insights, they should be interpreted within the broader biopsychosocial model of pain. Further observational and interventional studies are necessary to validate these relationships and translate them into targeted clinical strategies.
This study has several strengths. First, we used a MR approach, which minimized biases from confounding and reverse causation, providing stronger evidence for causal relationships compared to traditional observational studies. Second, we utilized large-scale GWAS data, ensuring high statistical power and reliable genetic instruments for exposure variables. Third, multiple sensitivity analyses were performed to validate the robustness of our findings and to check for potential pleiotropic effects. Finally, our study contributes novel insights into the genetic influences on psychosocial factors and their role in NP, offering a foundation for future research and clinical applications.
There are some limitations to this study. First, the GWAS data used in this study were derived exclusively from European populations, and caution is required when generalizing these findings to other populations. Future studies should validate these results in more diverse populations. Second, while a bidirectional causal relationship between exposure and outcome may exist, we were unable to perform bidirectional MR due to insufficient GWAS data for NP, which limited the extraction of adequate IVs. Third, the application of a strict Bonferroni correction for positive MR results may increase the likelihood of false-negative findings. Fourth, data availability from large-scale GWAS studies influenced our choice, as some risk factors (such as work-related stress and occupational physical activity) lack sufficiently powered GWAS datasets. Fifth, the wide confidence intervals observed in some results (eg, loneliness) may limit the precision of these analyses. Therefore, these findings should be interpreted with caution, and future studies with larger sample sizes are needed to further investigate these relationships.
Conclusion
Our findings suggest that psychosocial factors such as depression, mood changes, loneliness, and educational attainment have a causal relationship with NP. These insights underscore the importance of early psychological screening and timely interventions in NP prevention and management. Individuals with a genetic predisposition to depression or mood disorders may benefit from proactive mental health assessments and psychological interventions such as cognitive-behavioral therapy to alleviate psychological distress and reduce chronic pain risks. Given the established role of education and therapeutic exercise programs in pain management, our findings highlight the need to integrate targeted interventions such as patient education programs into prevention and treatment strategies. These programs align with international guidelines advocating for a biopsychosocial approach to NP, including WHO recommendations to address psychosocial factors through multidisciplinary care. Furthermore, our study emphasizes the role of genetic predisposition in NP, suggesting that future research should explore how genetic insights can inform personalized prevention and treatment strategies. Tailored interventions based on genetic susceptibility, combined with modifiable lifestyle factors, may optimize outcomes in NP management.
Ethics Approval Statement
This study is based on publicly available, de-identified summary-level genetic data obtained from previous genome-wide association studies (GWAS), in which ethical approval and informed consent were obtained by the original authors. According to item 1 and 2 of Article 32 of the Measures for Ethical Review of Life Science and Medical Research Involving Human Subjects (dated February 18, 2023, China), our study does not involve direct interaction with human participants, biological samples, or identifiable personal data; thus, it is exempt from ethical review by our Institutional Review Board (IRB).
Acknowledgments
We want to acknowledge the participants and investigators of the FinnGen study, UK Biobank, Neale lab, and Open GWAS database.
Funding
This work supported by the National Natural Science Foundation of China (82372461,82172494), “Pioneer” and “Leading Goose” R & D Program of Zhejiang (2022C013144), Wenzhou Science and Technology Bureau Foundation (ZY2023015).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hoy D, March L, Woolf A, et al. The global burden of neck pain: estimates from the global burden of disease 2010 study. Ann Rheumatic Dis. 2014;73(7):1309–1315. doi:10.1136/annrheumdis-2013-204431
2. Shin DW, Shin JI, Koyanagi A, et al. Global, regional, and national neck pain burden in the general population, 1990-2019: an analysis of the global burden of disease study 2019. Front Neurol. 2022;13:955367. doi:10.3389/fneur.2022.955367
3. Dieleman JL, Cao J, Chapin A, et al. US health care spending by payer and health condition, 1996–2016. JAMA. 2020;323(9):863–884. doi:10.1001/jama.2020.0734
4. Hey HWD, Lim JXY, Ong JZ, Luo N. Epidemiology of neck pain and its impact on quality-of-life-a population-based, cross sectional study in Singapore. Spine. 2021;46(22):1572–1580. doi:10.1097/brs.0000000000004071
5. Kim R, Wiest C, Clark K, Cook C, Horn M. Identifying risk factors for first-episode neck pain: a systematic review. Musculoskeletal Sci Pract. 2018;33:77–83. doi:10.1016/j.msksp.2017.11.007
6. Kazeminasab S, Nejadghaderi SA, Amiri P, et al. Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet Disord. 2022;23(1):26. doi:10.1186/s12891-021-04957-4
7. Cohen SP, Hooten WM. Advances in the diagnosis and management of neck pain. BMJ. 2017;358:j3221. doi:10.1136/bmj.j3221
8. Hernandez-Lucas P, Leirós-Rodríguez R, Lopez-Barreiro J, García-Soidán JL. Prevention of neck pain in adults with a back school-based intervention: a randomized controlled trial. Physiother Theory Pract. 2025;41(1):54–64. doi:10.1080/09593985.2024.2316313
9. Bernal-Utrera C, Gonzalez-Gerez JJ, Anarte-Lazo E, Rodriguez-Blanco C. Manual therapy versus therapeutic exercise in non-specific chronic neck pain: a randomized controlled trial. Trials. 2020;21(1):682. doi:10.1186/s13063-020-04610-w
10. Mogil JS. Pain genetics: past, present and future. Trends Genet. 2012;28(6):258–266. doi:10.1016/j.tig.2012.02.004
11. Hartley AE, Power GM, Sanderson E, Smith GD. A guide for understanding and designing Mendelian randomization studies in the musculoskeletal field. JBMR Plus. 2022;6(10):e10675. doi:10.1002/jbm4.10675
12. Zheng J, Baird D, Borges MC, et al. Recent developments in Mendelian randomization studies. Curr Epidemiol Rep. 2017;4(4):330–345. doi:10.1007/s40471-017-0128-6
13. Burgess S, Butterworth A, Malarstig A, Thompson SG. Use of Mendelian randomisation to assess potential benefit of clinical intervention. BMJ. 2012;345(nov06 1):e7325. doi:10.1136/bmj.e7325
14. Madrid-Valero JJ, Andreucci A, Carrillo E, Ferreira PH, Martínez-Selva JM, Ordoñana JR. Nature and nurture. genetic and environmental factors on the relationship between back pain and sleep quality. Eur J Pain. 2022;26(7):1460–1468. doi:10.1002/ejp.1973
15. Andreucci A, Madrid-Valero JJ, Ferreira PH, Ordoñana JR. Sleep quality and chronic neck pain: a cotwin study. J Clin Sleep Med. 2020;16(5):679–687. doi:10.5664/jcsm.8316
16. Tang B, Meng W, Hägg S, Burgess S, Jiang X. Reciprocal interaction between depression and pain: results from a comprehensive bidirectional Mendelian randomization study and functional annotation analysis. Pain. 2022;163(1):e40–e48. doi:10.1097/j.pain.0000000000002305
17. Elsworth B, Lyon M, Alexander T, et al. The MRC IEU openGWAS data infrastructure. BioRxiv. 2020:244293. doi:10.1101/2020.08.10.244293
18. Hemani G, Zheng J, Elsworth B, et al. The MR-base platform supports systematic causal inference across the human phenome. eLife. 2018;7. doi:10.7554/eLife.34408
19. Kurki MI, Karjalainen J, Palta P, et al. FinnGen: unique genetic insights from combining isolated population and national health register data. MedRxiv. 2022:22271360. doi:10.1101/2022.03.03.22271360
20. Mensah-Kane J, Schmidt AF, Hingorani AD, et al. No clinically relevant effect of heart rate increase and heart rate recovery during exercise on cardiovascular disease: a Mendelian randomization analysis. Front Genetics. 2021;12:569323. doi:10.3389/fgene.2021.569323
21. Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol. 2013;37(7):658–665. doi:10.1002/gepi.21758
22. Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through egger regression. Int J Epidemiol. 2015;44(2):512–525. doi:10.1093/ije/dyv080
23. Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol. 2016;40(4):304–314. doi:10.1002/gepi.21965
24. Bowden J, Del Greco MF, Minelli C, Davey Smith G, Sheehan N, Thompson J. A framework for the investigation of pleiotropy in two-sample summary data Mendelian randomization. Stat Med. 2017;36(11):1783–1802. doi:10.1002/sim.7221
25. Sedgwick P. Multiple hypothesis testing and bonferroni’s correction. BMJ. 2014;349:g6284. doi:10.1136/bmj.g6284
26. Al-Ghamdi S, Shubair MM, Angawi K, et al. Combined’ neck/back pain and psychological distress/morbidity among the Saudi population: a cross-sectional study. Front Psychol. 2022;13:870600. doi:10.3389/fpsyg.2022.870600
27. Dario AB, Kamper SJ, Williams C, et al. Psychological distress in early childhood and the risk of adolescent spinal pain with impact. Eur J Pain. 2022;26(2):522–530. doi:10.1002/ejp.1878
28. Lee H, Hübscher M, Moseley GL, et al. How does pain lead to disability? A systematic review and meta-analysis of mediation studies in people with back and neck pain. Pain. 2015;156(6):988–997. doi:10.1097/j.pain.0000000000000146
29. Liu F, Fang T, Zhou F, et al. Association of depression/anxiety symptoms with neck pain: a systematic review and meta-analysis of literature in China. Pain Res Manag. 2018;2018:3259431. doi:10.1155/2018/3259431
30. Myburgh C, Roessler KK, Larsen AH, Hartvigsen J. Neck pain and anxiety do not always go together. Chiropractic Osteopathy. 2010;18(1):6. doi:10.1186/1746-1340-18-6
31. Jahre H, Grotle M, Småstuen M, et al. Risk factors and risk profiles for neck pain in young adults: prospective analyses from adolescence to young adulthood-the North-Trøndelag health study. PLoS One. 2021;16(8):e0256006. doi:10.1371/journal.pone.0256006
32. Sic A, Bogicevic M, Brezic N, Nemr C, Knezevic NN. Chronic stress and headaches: the role of the HPA axis and autonomic nervous system. Biomedicines. 2025;13(2):463. doi:10.3390/biomedicines13020463
33. Li M, She K, Zhu P, et al. Chronic pain and comorbid emotional disorders: neural circuitry and neuroimmunity pathways. Int J Mol Sci. 2025;26(2):436. doi:10.3390/ijms26020436
34. Markotić V, Zubac D, Miljko M, et al. Level of education as a risk factor for extensive prevalence of cervical intervertebral disc degenerative changes and chronic neck pain. Cent Eur J Public Health. 2017;25(3):245–250. doi:10.21101/cejph.a4897
35. Rasmussen-Barr E, Halvorsen M, Bohman T, et al. Summarizing the effects of different exercise types in chronic neck pain - a systematic review and meta-analysis of systematic reviews. BMC Musculoskelet Disord. 2023;24(1):806. doi:10.1186/s12891-023-06930-9
36. Samulowitz A, Hensing G, Haukenes I, Bergman S, Grimby-Ekman A. General self-efficacy and social support in men and women with pain - irregular sex patterns of cross-sectional and longitudinal associations in a general population sample. BMC Musculoskelet Disord. 2022;23(1):1026. doi:10.1186/s12891-022-05992-5
37. Andias R, Neto M, Silva AG. The effects of pain neuroscience education and exercise on pain, muscle endurance, catastrophizing and anxiety in adolescents with chronic idiopathic neck pain: a school-based pilot, randomized and controlled study. Physiother Theory Pract. 2018;34(9):682–691. doi:10.1080/09593985.2018.1423590
38. Andias R, Sa-Couto P, Silva AG. Blended-learning pain neuroscience education and exercise in high school students with chronic neck pain: a randomized controlled trial. Physl Ther. 2022;102(6). doi:10.1093/ptj/pzac048
39. Luc A, Antoine F, Bekkering G, Detrembleur C, Pitance L. Relationship between leisure time physical activity, weight, and the onset and persistence of nonspecific neck pain: a systematic review. J Orthop Sports Phys Ther. 2022;52(12):777–791. doi:10.2519/jospt.2022.11137
40. Øverås CK, Villumsen M, Axén I, et al. Association between objectively measured physical behaviour and neck- and/or low back pain: a systematic review. Eur J Pain. 2020;24(6):1007–1022. doi:10.1002/ejp.1551
41. Jahre H, Grotle M, Smedbråten K, Dunn KM, Øiestad BE. Risk factors for non-specific neck pain in young adults. A systematic review. BMC Musculoskelet Disord. 2020;21(1):366. doi:10.1186/s12891-020-03379-y
42. Paraskevopoulos E, Koumantakis GA, Papandreou M. A systematic review of the aerobic exercise program variables for patients with non-specific neck pain: effectiveness and clinical applications. Healthcare. 2023;11(3). doi:10.3390/healthcare11030339
43. Wilhelm MP, Donaldson M, Griswold D, et al. The effects of exercise dosage on neck-related pain and disability: a systematic review with meta-analysis. J Orthop Sports Phys Ther. 2020;50(11):607–621. doi:10.2519/jospt.2020.9155
44. Waersted M, Hanvold TN, Veiersted KB. Computer work and musculoskeletal disorders of the neck and upper extremity: a systematic review. BMC Musculoskelet Disord. 2010;29(11):79. doi:10.1186/1471-2474-11-79
45. Williams FMK, Elgaeva EE, Freidin MB, et al. Causal effects of psychosocial factors on chronic back pain: a bidirectional Mendelian randomisation study. Eur Spine J. 2022;31(7):1906–1915. doi:10.1007/s00586-022-07263-2
46. Lv Z, Cui J, Zhang J. Smoking, alcohol and coffee consumption and risk of low back pain: a Mendelian randomization study. Eur Spine J. 2022;31(11):2913–2919. doi:10.1007/s00586-022-07389-3
47. Ploutarchou G, Savva C, Karagiannis C, Pavlou K, O’Sullivan K, Korakakis V. The effectiveness of cognitive behavioural therapy in chronic neck pain: a systematic review with meta-analysis. Cogn Behav Ther. 2023;52(5):523–563. doi:10.1080/16506073.2023.2236296
48. WHO Guidelines Approved by the Guidelines Review Committee. Guidelines on the management of chronic pain in children. World Health Organization; 2020.
49. Blanpied PR, Gross AR, Elliott JM, et al. Neck pain: revision 2017. J Orthop Sports Phys Ther. 2017;47(7):A1–A83. doi:10.2519/jospt.2017.0302
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

