Back to Journals » Journal of Multidisciplinary Healthcare » Volume 18
Clinical and Radiographic Evaluation of Bone Profile Around Dental Implants Placed in the Esthetic Zone
Authors Alssum L, Al-Kattan R, Al-Shibani N, Al Ali H , Aldossari F , Allam E
Received 28 October 2024
Accepted for publication 23 January 2025
Published 5 February 2025 Volume 2025:18 Pages 591—601
DOI https://doi.org/10.2147/JMDH.S503269
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Charles V Pollack
Lamees Alssum,1 Reem Al-Kattan,1 Nouf Al-Shibani,1 Hafsah Al Ali,2 Farah Aldossari,2 Eman Allam3
1Department of Periodontics and Community Dentistry, College of Dentistry, King Saud University, Riyadh, Saudi Arabia; 2College of Dentistry, King Saud University, Riyadh, Saudi Arabia; 3Research and Graduate Studies Department, Mohammed Bin Rashid University of Medicine and Health Sciences, Dubai, United Arab Emirates
Correspondence: Lamees Alssum, Department of Periodontics and Community Dentistry College of Dentistry King Saud University, Riyadh, Saudi Arabia, Email [email protected]
Objective: To evaluate the bone profile around dental implants placed in the esthetic zone through periodontal assessment and radiographic analysis using cone-beam computed tomography (CBCT).
Methods: We conducted a clinical observational study of 35 subjects who received dental implants placed in the esthetic zone to replace lost anterior teeth. Clinical evaluation included a comprehensive periodontal examination. The esthetic outcomes of the soft tissue around the implants were assessed using the pink esthetic score (PES). Patient satisfaction was assessed by using a specially designed questionnaire. The Oral Health Impact Profile (OHIP)-14 was used to assess the quality of life. The bone profile around the implant was assessed using CBCT. All the values were compared and statistically analyzed.
Results: A soft tissue graft (STG) was associated with the presence of > 2 mm of bone thickness 1 mm from the implant shoulder (p < 0.01). The STG was also significantly associated with bone thickness at 3 and 5 mm (p = 0.04). PES was not significantly associated with the bone thickness, OHIP score, or satisfaction score. Patients with fenestrations had significantly higher scores for functional limitations and pain than those without fenestrations (p = 0.01 and 0.04 respectively).
Conclusion: The bone profile around the anterior implant is not ideal. Although the buccal bone was thin around the implant placed in the esthetic zone, it did not affect the esthetic outcomes or overall satisfaction of the patient. However, fenestration defects may affect patients’ quality of life.
Keywords: dental implants, esthetic zone, periodontal assessment, cone beam computed tomography
Introduction
Anterior maxillary rehabilitation using dental implants represents a clinical challenge because of the complex anatomy of the region and the difficulty in satisfying patients’ rigorous esthetic requirements.1 The anterior maxilla, often known as the “esthetic zone”, has unique anatomical and osseous features. The quality and thickness of the bone surrounding the implant are crucial for successful restoration. Evidence indicates a minimum bone thickness requirement of at least 2 mm around the implant for optimal results.2,3
One of the main challenges that complicate restorative treatment using implants is the dimensional variations that occur in the alveolar process following tooth extraction.4,5 Because the buccal bone wall is frequently thinner, bone loss at the buccal surface of the marginal 1/3rd of the socket is usually more pronounced than that at the palatal surface after healing is completed. The presence of buccal undercuts, a common finding, is a recognized technical complication. Some reports have indicated that buccal bone thickness was less than ideal in more than 50% of the sites treated in the esthetic zone.6,7 Zang et al reported buccal concavity in 41% of central incisors, 77% of lateral incisors, and 33% of canines in the anterior maxilla, located approximately 4–6 mm from the bone crest.8 Todorovic et al concluded that immediate implants in the anterior maxillae have anatomical risks and that the alveolar bone on the buccal aspect is very thin, with fenestrations in certain positions. Alveolar bone on the palatal side, in their sample, was thicker than buccal and increased from <1 mm at crestal level up to 3.77 mm, 4.56 mm, and 5.43 mm for centrals, laterals, and canines at the 9 mm level, respectively.9
In addition to reduced vertical and horizontal bone dimensions after tooth extraction, factors that could limit the amount of bone available for implant placement include the presence of the nasopalatine canal and nasal fossa. Altered bone remodeling after tooth extraction and healing after implant placement could lead to the development of anomalies in the bone surrounding the dental implants, such as dehiscence and fenestration.10,11
Cone-beam computed tomography (CBCT) is commonly used for implant treatment planning. It overcomes some of the main limitations of standard radiographs and provides a 3-dimensional view of the area of interest. The American Academy of Oral and Maxillofacial Radiology (AAOMR) recommends that CBCT be considered the imaging modality of choice for the preoperative assessment of potential implant sites and for postoperative bone assessment to evaluate treatment outcomes.12,13 The aim of this study was to evaluate the bone profile surrounding dental implants in the esthetic zone through clinical periodontal assessment and radiographic analysis using CBCT scans.
Materials and Methods
All patients who presented to the outpatient clinic of the College of Dentistry, King Saud University, between January 2015 and January 2019, had implants placed at the anterior esthetic zone, and met the inclusion criteria were included in the study. The study complies with the Declaration of Helsinki. Written informed consent was obtained from all participants, and ethical approval was obtained from the Research Ethics Committee of King Saud University, KSA (approval no. E-20-5579).
The subjects were selected based on the following criteria: at least 18 years of age, a single implant (titanium, Straumann LLC, Andover, MA, USA) placed in the anterior maxillary region with existing neighboring teeth, implant restoration, and function for at least 6 months. All participants were contacted for a follow-up visit, including comprehensive clinical and radiographic examination of the implant sites. Clinical evaluation included periodontal examination, recording plaque index, and bleeding index around the Ramfjord teeth (number of teeth: 16, 21, 24, 36, 41, 44). Pocket depth, soft tissue recession, amount of keratinized tissue, pain, mobility, and suppuration around the dental implant were also recorded. The esthetic outcome of the soft tissue around the implants was assessed using the pink esthetic score (PES).14 The PES is based on seven variables: mesial papilla, distal papilla, soft-tissue level, soft tissue contour, alveolar process deficiency, soft-tissue color and texture. Each variable was assessed with a 2-1-0 score, with 2 being the best and 0 being the poorest score. The highest possible score reflecting a perfect match of the peri-implant soft tissue with that of the reference tooth was 14.14 Data collected from patients’ which included implant size and length, surgical procedures performed at the implant site, type of implant placement, and duration of implant function.
Patients’ satisfaction was assessed using a specifically designed questionnaire evaluating the level of general satisfaction with the outcome of their implant-supported restorations, comfort, speech, esthetics, function, and cleanability.15 Responses were recorded using five-point agreement Likert scale with the five answers options of strongly agree (5), agree (4), I do not know (3), disagree (2), and strongly disagree (1). The Oral Health Impact Profile (OHIP)-14 was used to assess quality of life by measuring dysfunction, discomfort, and disability.16 The OHIP-14 captures seven domains of OHRQoL with two items per domain: functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability, and handicap. The OHIP-14 scores can range from 0 to 56 and are calculated by summing the ordinal values for the 14 items.16
A limited field of view CBCT was performed for the area of interest and assessed by a single trained investigator (L.A). All scans were taken at 90 kV and 11.0 mA for 12s (voxel size: 200 µm; grey scale: 15 bit; focal spot: 0.5 mm; field of view: 100×55 mm) using a Planmeca ProMax 3D Plus (Planmeca Co., Helsinki, Finland) machine. Image reconstruction for visual analysis was performed using the Romixes software (Planmeca Oy, Helsinki, Finland). Measurements recorded from the CBCT scans included buccal bone thickness (Figure 1) measured at the implant shoulder as well as three levels through the implant body, (1,3,5 mm) using the implant shoulder as a reference point, buccal bone level defined as the distance from the implant shoulder to the first bone implant contact on the buccal surface, and the presence of undercuts (identified by drawing a line on the buccal surface of the implant site and location of the deepest area). An undercut was reported whenever there was at least a 1 mm difference from the outline of the ridge. Implant angle was recorded as the angle of the implant relative to the ridge. Shoulder position of the implant was recorded relative to the midline of the ridge. Dehiscence and fenestration were recorded as present or absent.
Data were organized into an Excel spreadsheet and analyzed using R Studio (Version: 2024.04.2+764). Categorical data were described as frequencies and percentages. For continuous variables, the normality distribution of the data was tested using the Shapiro–Wilk test and visual assessment (eg, histograms). Parametric variables are shown as means and standard deviations (SD), whereas non-parametric variables are shown as medians and interquartile ranges (IQR). A cutoff value of 7 was used with the PES, where a value below 7 was deemed unacceptable The chi-square test was used to detect associations between categorical variables, whereas the Mann–Whitney U and Kruskal–Wallis H-tests were used for continuous non-parametric variables between two or more groups. Spearman correlation coefficients were calculated for two continuous non-parametric variables. Statistical significance was deemed significant if p ≤ 0.05.
Results
A total of 35 patients met the inclusion criteria and were included in the final analysis, with a mean age of 44.8 ±14.2 years. The clinical and surgical details of the included sample, as well as the radiographic findings, are presented in Tables 1 and 2 and Figure 2. The median (IQR) PES was 10.00 (7.75 to 11.00) with 31 patients (86.11%) having an acceptable score. The median (IQR) satisfaction score was 37.50 (32.75 42.00). The overall OHIP score yielded a median (IQR) of 0.00 (0.00 4.25) with comparable results in the subdomains. Only four patients (11.11%) had fenestration, while 16 (44.44%) had dehiscence. Most patients (29 [80.56%]) had a buccal bone thickness of less than 1 mm at the implant shoulder. The median (IQR) buccal bone level was 1.00 (0.00 to 9.50).
 |
Table 1 Clinical and Surgical Details of the Included Sample |
 |
Table 2 Descriptive Analysis of the Radiographic Findings |
 |
Table 3 Association of Surgical Procedures with Outcomes |
Chi-square analysis indicated no significant association between the surgical procedures performed at the site of the implant and the outcomes, except for socket preservation (SP) and bone thickness at 1 mm (p = 0.02). Furthermore, soft tissue grafting (STG) was associated with bone thickness > 2 mm at 1 mm (100%; p < 0.01). Similarly, the STG was significantly associated with bone thickness at 3 and 5 mm (p = 0.04). A buccal undercut was detected in 50% of the cases that experienced SP compared to only one case (3.57%) that did not (p = 0.01) (Table 3).
PES was not significantly associated with bone thickness at 1, 3, or 5 mm (p = 0.53, 0.63, and 0.76, respectively), while it was negatively and weakly correlated with buccal bone level (ρ = − 0.33) (Table 4).
 |
Table 4 Association of Pink Esthetic Score with Measures and Outcomes |
Most fenestration cases (n = 3; 75%) had buccal undercuts (p < 0.01). Furthermore, patients with fenestration had a significantly higher median (IQR) of OHIP of 4.00 (1.75 to 6.50) compared to 0.00 (0.00 to 3.00) in patients without fenestration (p = 0.05). Similarly, patients with fenestrations had significantly higher scores in the domains of functional limitations and pain than patients without fenestrations (p = 0.01 and 0.04 respectively). Dehiscence was not significantly associated with any of the tested variables (Table 5).
 |
Table 5 Association of Dehiscence and Fenestration with Variables and Outcomes |
The PES was not significantly correlated with either OHIP or satisfaction (p = 0.41 and 0.98 respectively). The overall and subdomains of OHIP and satisfaction scores showed significant correlations. The physical pain domain was the domain most negatively correlated with satisfaction (ρ= − 0.63, p < 0.01), while social disability was the least negatively correlated (ρ= − 0.33, p = 0.05) (Table 6).
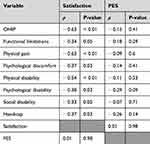 |
Table 6 Spearman Correlation Analysis |
Discussion
Today’s dental community faces several clinical challenges, including the growing number of patients selecting dental implants to replace lost teeth with expectations of ultimate functional effectiveness and stability, together with the aesthetic goal of restoration with natural teeth resemblance. Careful analysis of the anatomical circumstances and a thoughtfully designed treatment plan for each case are essential. Incorrectly positioned implants are candidates for poor esthetic and functional prognosis. Consequently, there have been constant attempts to improve surgical procedures, biocompatible materials, and grafts used to ensure successful regeneration of the implant’s surrounding bone and enhance the maintenance of dental implants. CBCT is an appropriate practice for assessing treatment results following implant placement, especially in the esthetic zone, where anticipated problems are better identified and diagnosed at an early stage for better overall patient management.12,13 The aim of this study was to evaluate the bone characteristics surrounding dental implants in the esthetic zone through clinical periodontal assessment and radiographic analysis using CBCT scans.
Bone fenestration and dehiscence were assessed on the sagittal sections of the CBCT scans rather than using the reconstructed volume since the reconstructed volume may over- or under-estimate the amount of bone covering the implant surface while the sagittal sections are expected to represent the anatomical truth. Caution must be taken in consideration when interpreting the findings because of the limited spatial resolution of the CBCT images.17–21
One of the requirements for successful dental implant surgery is appropriate width and thickness of the gingival connective tissue. Clinicians believe that good quality soft tissue guarantees proper wound closure and more efficient implant treatment.22 The results of the current study indicate that patients receiving STG were associated with the presence of more than 2 mm bone thickness at 1 mm from the implant shoulder. In agreement with these findings, Linkevicius23 reported that the initial gingival tissue thickness at the crest significantly influenced the marginal bone loss around implants and that when the soft tissue was less than 2.0 mm thick, more crestal bone loss occurred. It is possible to conclude that greater soft-tissue thickness resists the progression of inflammation and subsequent alveolar bone loss.23
The PES was used to assess the esthetic outcomes of the implants. It is essential to recognize the relationship between PES scores and bone thickness around the implant as both are key determinants of effective management. PES is considered a reliable and reproducible tool for evaluating soft tissue around single-tooth implant crowns, and it assesses esthetic outcomes using seven variables: mesial papilla, distal papilla, soft-tissue level, soft-tissue contour, alveolar process deficiency, soft-tissue color, and texture. Each variable was assessed with a score of 2–1–0, with 2 being the best and 0 being the poorest. All variables were assessed by comparison with a reference tooth.14,24 In the current study, the PES scores were not significantly associated with bone thickness around the implants placed in the esthetic zone. Although the buccal bone around the implants was generally thin, most patients had acceptable PES scores. Similarly, previous studies have reported no significant correlation between marginal bone loss and PES.25–27
Fenestration and buccal undercuts are common challenges associated with dental implant placement, particularly esthetic. In the current sample, 75% of patients with fenestration had buccal undercuts. Fenestration was associated with higher functional limitation and pain scores. Both conditions are considered factors that can complicate the surgical procedure and affect the long-term success and esthetic outcomes of the implant.28 Their incidence is influenced by certain technical and anatomical factors such as discrepancies between the ridge angle and implant angle, and deeper alveolar ridge concavities.29 Several bone augmentation and guided bone regeneration techniques are commonly recommended to effectively manage fenestration around dental implants, potentially improving outcomes, such as laser-assisted periosteal fenestration (LA-PF) using Erbium YAG laser and guided bone regeneration techniques using Gore-Tex membranes.30,31
In this study, patient satisfaction following implant treatment and its possible correlations were assessed. The results indicated that PES scores were not significantly correlated with either the OHIP or satisfaction domains. Overall and subdomains of the OHIP were significantly correlated with pain. Satisfaction with dental implants has been reported to be influenced by various factors, including esthetic outcomes, pain, surgical complications, and duration of the treatment process. In previous reports, factors such as operator experience, female sex, and surgical difficulty have been significantly associated with pain levels.32,33
This study has several limitations. The small sample size and observational design limit the generalizability of the findings. In addition, subjective assessments, including patient satisfaction and quality of life, may introduce reporting bias. In addition, the reliance on the PES alone may not fully describe esthetic outcomes.
Conclusion
In conclusion, the bone profile around the anterior implant was not ideal. Although the buccal bone was thin around the implant placed in the esthetic zone, it did not affect the esthetic outcomes or overall satisfaction of the patient. However, fenestration defects may affect patients’ quality of life.
Data Sharing Statement
Data used in this study are available from the corresponding author upon request.
Ethical Approval
This study was approved by the Research Ethics Committee of the King Saud University, KSA (approval no. E-20-5579). Written informed consent was obtained from all participants.
Funding
There is no funding to report.
Disclosure
The authors declare no competing interests in this work.
References
1. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19(7):43–61.
2. Merheb J, Quirynen M, Teughels W. Critical buccal bone dimensions along implants. Periodontol 2000. 2014;66(1):97–105. doi:10.1111/prd.12042
3. Linares A, Dopico J, Magrin G, Blanco J. Critical review on bone grafting during immediate implant placement. Periodontol 2000. 2023;93:309–326. doi:10.1111/prd.12516
4. Masaki C, Nakamoto T, Mukaibo T, Kondo Y, Hosokawa R. Strategies for alveolar ridge reconstruction and preservation for implant therapy. J Prosthodont Res. 2015;59(4):220–228. doi:10.1016/j.jpor.2015.04.005
5. Jung RE, Ioannidis A, Hämmerle CHF, Thoma DS. Alveolar ridge preservation in the esthetic zone. Periodontol 2000. 2018;77(1):165–175. doi:10.1111/prd.12209
6. Januario AL, Duarte WR, Barriviera M, Mesti JC, Araujo MG, Lindhe J. Dimension of the facial bone wall in the anterior maxilla: a cone-beam computed tomography study. Clin Oral Implants Res. 2011;22(10):1168–1171. doi:10.1111/j.1600-0501.2010.02086.x
7. Lopez-Jarana P, Diaz-Castro CM, Falcao A, Falcao C, Rios-Santos JV, Herrero-Climent M. Thickness of the buccal bone wall and root angulation in the maxilla and mandible: an approach to cone beam computed tomography. BMC Oral Health. 2018;18(1):194. doi:10.1186/s12903-018-0652-x
8. Zhang W, Skrypczak A, Weltman R. Anterior maxilla alveolar ridge dimension and morphology measurement by cone beam computerized tomography (CBCT) for immediate implant treatment planning. BMC Oral Health. 2015;15:65. doi:10.1186/s12903-015-0055-1
9. Todorovic VS, Postma TC, Hoffman J, van Zyl AW. Buccal and palatal alveolar bone dimensions in the anterior maxilla: a micro-CT study. Clin Implant Dent Relat Res. 2023;25(2):261–270. doi:10.1111/cid.13175
10. Ferrus J, Cecchinato D, Pjetursson EB, Lang NP, Sanz M, Lindhe J. Factors influencing ridge alterations following immediate implant placement into extraction sockets. Clin Oral Implants Res. 2010;21(1):22–29. doi:10.1111/j.1600-0501.2009.01825.x
11. Vera C, De Kok IJ, Chen W, Reside G, Tyndall D, Cooper LF. Evaluation of post-implant buccal bone resorption using cone beam computed tomography: a clinical pilot study. Int J Oral Maxillofac Implants. 2012;27(5):1249–1257.
12. Tyndall DA, Price JB, Tetradis S, et al. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(6):817–826. doi:10.1016/j.oooo.2012.03.005
13. Valizadeh S, Baharestani M, Amid R, Ahsaie MG. Evaluation of maxillary alveolar ridge morphology and residual bone for implant placement by cone beam computed tomography (CBCT). J Long Term Eff Med Implants. 2022;32(2):61–71. doi:10.1615/JLongTermEffMedImplants.2022039223
14. Furhauser R, Florescu D, Benesch T, Haas R, Mailath G, Watzek G. Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score. Clin Oral Implants Res. 2005;16(6):639–644. doi:10.1111/j.1600-0501.2005.01193.x
15. Heo YY, Seong-Joo H, Myung-Woo C, Ji-Man P. The patients’ satisfaction following implant treatment. J Korean Acad Prosthod. 2008;46:569–576. doi:10.4047/jkap.2008.46.6.569
16. Slade GD. Assessing change in quality of life using the oral health impact profile. Oral Epidemiol. 1998;26(1):52–61. doi:10.1111/j.1600-0528.1998.tb02084.x
17. Brüllmann D, Schulze RK. Spatial resolution in CBCT machines for dental/maxillofacial applications-what do we know today? Dentomaxillofac Radiol. 2015;44(1):20140204. doi:10.1259/dmfr.20140204
18. Schulze R, Couso-Queiruga E, Katsaros C. Accuracy of cone-beam computed tomography in imaging the components of the periodontal phenotype. Periodontol 2000. 2024. doi:10.1111/prd.12556
19. Schulze R. CBCT artefact-burden of zirconia-based as compared to titanium implants for different beam energies: an analytical approach. Sci Rep. 2022;12(1):15276. doi:10.1038/s41598-022-19379-y
20. Schulze R, Heil U, Gross D, et al. Artefacts in CBCT: a review. Dentomaxillofac Radiol. 2011;40(5):265–273. doi:10.1259/dmfr/30642039
21. Patcas R, Müller L, Ullrich O, Peltomäki T. Accuracy of cone-beam computed tomography at different resolutions assessed on the bony covering of the mandibular anterior teeth. Am J Orthod Dentofacial Orthop. 2012;141(1):41–50. doi:10.1016/j.ajodo.2011.06.034
22. Hadzik J, Błaszczyszyn A, Gedrange T, Dominiak M. Soft-tissue augmentation around dental implants with a connective tissue graft (CTG) and xenogeneic collagen matrix (CMX)-5-year follow-up. J Clin Med. 2023;12(3):924. doi:10.3390/jcm12030924
23. Linkevicius T, Apse P, Grybauskas S, Puisys A. The influence of soft tissue thickness on crestal bone changes around implants: a 1-year prospective controlled clinical trial. Int J Oral Maxillofac Implant. 2009;24:712–719.
24. Cho HL, Lee JK, Um HS, Chang BS. Esthetic evaluation of maxillary single-tooth implants in the esthetic zone. J Periodontal Implant Sci. 2010;40(4):188–193. doi:10.5051/jpis.2010.40.4.188
25. Naiem S, Hosny M, El-Nahass H. Esthetics and bone changes of immediate implants with or without vascularized interpositional periosteal connective tissue grafting: a 2-year randomized controlled trial. Clin Oral Implants Res. 2023;34(5):498–511. doi:10.1111/clr.14056
26. Gouveia M, Sousa S, Fonseca P, Branco P, Quintanilla J. Marginal bone loss and pink esthetic evaluation of narrow-diameter dental implants for single crowns: 1-year prospective clinical study. Int J Oral Maxillofac Implants. 2022;37(3):515–524. doi:10.11607/jomi.9051
27. Dini C, Borges GA, Costa RC, Magno MB, Maia LC, Barão VAR. Peri-implant and esthetic outcomes of cemented and screw-retained crowns using zirconia abutments in single implant-supported restorations-A systematic review and meta-analysis. Clin Oral Implants Res. 2021;32(10):1143–1158. doi:10.1111/clr.13824
28. Steier L, Steier G. Successful dental implant placement surgeries with buccal bone fenestrations. J Oral Implant. 2015;41(1):112–118. doi:10.1563/AAID-JOI-D-12-00233
29. Chan H, Garaicoa‐Pazmiño C, Suárez F, et al. Incidence of implant buccal plate fenestration in the esthetic zone: a cone beam computed tomography study. Int J Oral Maxillofac Implants. 2014;29:(1):171–177. doi:10.11607/jomi.3397
30. Lim K, Lee W. Technical note on vestibuloplasty around dental implants using Erbium YAG laser-assisted periosteal fenestration (LA-PF). Medicina. 2023;59(10):1884. doi:10.3390/medicina59101884
31. Dahlin C, Andersson L, Linde A. Bone augmentation at fenestrated implants by an osteopromotive membrane technique. A controlled clinical study. Clin Oral Implant Res. 1991;2(4):159–165. doi:10.1034/j.1600-0501.1991.020401.x
32. Al-Khabbaz A, Griffin T, Al-Shammari K. Assessment of pain associated with the surgical placement of dental implants. J Periodontol. 2007;78(2):239–246. doi:10.1902/jop.2007.060032
33. Kim Y, Kim H, Yi Y, Yun P. Evaluation of subjective satisfaction of dental implant patients. J Korean Assoc Oral Maxillofac Surg. 2014;40(3):130–134. doi:10.5125/jkaoms.2014.40.3.130
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



