Back to Journals » Therapeutics and Clinical Risk Management » Volume 20
Clinical and Radiological Factors Associated with Nonoperative Management Failure for Small Bowel Obstruction: A Retrospective Study from a Resource-Limited Setting
Authors Al-wageeh S , Alyhari Q, Ahmed F , Mohammed H, Dahan N, Almohtadi AM, AL-Nuzili Jnr STS, Badheeb M , Naji A
Received 2 October 2024
Accepted for publication 20 December 2024
Published 25 December 2024 Volume 2024:20 Pages 893—906
DOI https://doi.org/10.2147/TCRM.S496629
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor De Yun Wang
Saleh Al-wageeh,1 Qasem Alyhari,1 Faisal Ahmed,2 Hanan Mohammed,1 Noha Dahan,1 Abdullatif Mothanna Almohtadi,3 Sameer Taha said AL-Nuzili Jnr,4 Mohamed Badheeb,5 Abdulsattar Naji1
1Department of General Surgery, School of Medicine, Ibb University, Ibb, Yemen; 2Department of Urology, School of Medicine, Ibb University, Ibb, Yemen; 3Department of Radiology, School of Medicine, Ibb University, Ibb, Yemen; 4Department of Vascular Surgery, School of Medicine, Ibb University, Ibb, Yemen; 5Department of Internal Medicine, Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT, USA
Correspondence: Faisal Ahmed, Department of Urology, School of Medicine, Ibb University, Ibb, Yemen, Email [email protected] Qasem Alyhari, Department of General Surgery, School of Medicine, Ibb University, Ibb, Yemen, Email [email protected]
Background: Recognizing factors that predict non-operative management (NOM) failure for patients with small bowel obstruction (SBO) aids in limiting surgical intervention when needed. This study investigated the predictive factors for NOM failure in SBO patients in a resource-limited setting.
Material and Method: A retrospective study included 165 patients who were diagnosed with SBO and were admitted and managed at Althora General Hospital, IBB, Yemen, from April 2022 to March 2024. Patients’ baseline characteristics and profiles along with factors associated with failure of NOM were investigated and analyzed with univariate and multivariate analysis.
Results: 51 (30.4%) of included cohorts were managed non-operatively. The mean age was 47.7± 16.9 years, and males were disproportionally presented (62.7%). The majority of patients presented with abdominal pain (96.1%). Failure of NOM was seen in 18 (35.3%) patients and intra-operative findings were adhesive bands, volvulus, intussusception, and mesenteric ischemia in 7 (38.9%), 5 (27.8%), 4 (22.2%), and 2 (11.1%) patients, respectively. Bowel resection was performed in 11 (61.1%), and 4 of them needed a colostomy diversion. Postoperative complications occurred in 13 (25.5%) patients, including fever, paralytic ileus, surgical site infection, and reoperation in 13 (25.5%), 5 (9.8%), 4 (7.8%), and 2 (3.9%) patients, respectively. Sixteen patients were discharged, and two patients died due to mesenteric ischemia. Among NOM successful patients, recurrence has occurred in 8 patients. In multivariate analysis, poor bowel wall enhancement (OR: 8.59; 95% CI: 1.14– 64.59, p=0.037) and high level of obstruction (OR: 11.64; 95% CI: 1.34– 100.85, p=0.026) in computed tomography (CT) scan were independently associated with NOM failure.
Conclusion: Poor bowel wall enhancement and significant obstruction on CT images are critical indicators for selecting SBO patients requiring urgent surgery. However, evaluating the advantages of surgical intervention versus NOM demands a comprehensive analysis of surgical risks, comorbidities, and the presence of bowel strangulation or ischemia.
Keywords: computed tomography scan, failure, nonoperative management, predictive factors, small bowel obstruction
Introduction
Small bowel obstruction (SBO) represents one of the most common causes of surgical emergencies, accounting for up to 15% of surgical admissions for acute nontraumatic abdominal pain.1 Notably, the overall incidence and prevalence of SBO have increased significantly over the years.2 This trend was reflected in enormous healthcare expenditure and significant mortality and morbidity.3 The complexity of SBO diagnosis stems from its variable presentation that is influenced by the obstruction’s level, duration, underlying pathology, and presence or absence of intestinal ischemia.4 The earliest manifestations of SBO include abdominal pain, distension, constipation, and bloating. Later, patients can exhibit a progression of abdominal pain into more localized constant pain reflecting peritonism secondary to bowel ischemia or necrosis.4 In more advanced cases, patients may develop hypovolemic shock, septicemia, and multi-organ dysfunction.5
The identification of the underlying SBO etiology represents another challenge for clinicians. Notwithstanding this, approximately 75% of SBO cases arise from intra-abdominal adhesions, typically resulting from prior surgical procedures.6 Other causes of mechanical obstruction may include hernias, inflammation (eg, Crohn’s disease), infectious (eg, tuberculosis, ascariasis), or malignancies.7 Radiologic imaging, including abdominal radiographs, ultrasonography, and computerized tomography (CT) scans, can provide significant value in the diagnosis and possible surgical planning for SBO cases.8 However, there is a notable difference in CT imaging sensitivity, with higher rates reported among adhesive SBO (96%), compared to other causes (78%).9 Similarly, a higher accuracy for predicting the need for surgical intervention was noted for adhesions, hernias, and tumor detection.9
The advancement and incorporation of medical imaging resulted in a transition into less aggressive treatment measures, moving from the traditional teaching “Never let the sun rise or set on an obstructed abdomen”, into more conservative “non-operative management”, that includes gastric decompression, fluid, and electrolyte replacement, and pain management.6 Such an approach has been preferred in the management of adhesive SBO, with 70% to 80% of patients achieving symptom resolution.4 This approach, however, has been limited with the concerns of retaining the existing adhesions, potentially leading to recurrent SBO.10 Recurrence is prevalent, occurring in roughly 20% of patients.10 In addition to the inconsistency of non-operative management (NOM) success rates in the literature, the ambiguity of the underlying cause of SBO renders many surgeons preferring to advocate early surgery for most patients.11 Nonetheless, a trial of NOM remains appropriate for the majority of patients as earlier surgical intervention was shown to be associated with higher mortality and morbidity.12,13
Determining the need for surgical intervention can be challenging even among the most experienced surgeons.14 Several scoring systems have been proposed integrating clinical and radiological findings, however, these scores predominantly include patients with adhesive SBO and exclude patients with the virgin abdomen.11 Here in, we investigated the clinical and radiological factors that might contribute in non-operative management failure among SBO patients in resource-limited settings.
Materials and Methods
Study Design and Population
A retrospective analysis was conducted from April 2022 to March 2024, including 165 consecutive adult patients with SBO who were managed in the General Surgery Department of Althora General Hospital, Ibb, Yemen. The study protocol adhered to the principles of the Declaration of Helsinki and was approved by the Ethics Committee of Ibb University. Adult patients aged 18 years or older, clinically diagnosed with SBO based on presenting symptoms, physical examination, and radiologic findings, were included. Patients with a previously established cause of SBO (eg, tumor or abdominal hernia), pregnant females, or those with incomplete medical records were excluded. Follow-up for each patient lasted a minimum of 90 days. The diagnosis of SBO was confirmed through clinical evaluation by a general surgeon, supplemented by laboratory tests and radiological imaging. For greater diagnostic accuracy, only patients with SBO confirmed by abdominal CT were included. Non-operative management (NOM) was defined as supportive medical care provided without surgical, endoscopic, or radiologic intervention. Early management included nil per os status, nasogastric or long intestinal tube decompression, fluid resuscitation, correction of electrolyte imbalances, nutritional support, and measures to prevent aspiration.
Diagnosis and Treatment
Patients with suspected bowel strangulation or perforation underwent emergent laparotomy, while NOM was reserved for patients with uncomplicated SBO. Clinical improvement during NOM was indicated by reduced abdominal discomfort, tenderness, or distension, decreased nasogastric tube output, or the passage of stool in patients with prior constipation. Radiologic improvement, such as reduced bowel loop dilation or a decrease in small intestinal diameter, was also used to guide continued NOM. Resolution of SBO was confirmed when symptoms and clinical indicators of obstruction disappeared, and abdominal imaging revealed no dilated small bowel. A gradual reintroduction of diet was initiated, beginning with liquids, progressing to a soft diet the following day, and advancing to solid meals as tolerated. Patients were discharged once they could tolerate solid meals. Patients who showed no clinical or radiologic improvement were considered for surgical exploration. The algorithm for SBO management is detailed in Figure 1 as was described in a previous report by Bauer et al15
 |
Figure 1 Algorithm for management of small bowel obstruction. |
Data Gathering
The demographic characteristics of patients, including age, gender, residency, smoking status, Khate chewing and comorbidities (eg, hypertension, ischemic heart disease, diabetes mellitus, obesity, and chronic renal failure), previous abdominal surgery, clinical symptoms (eg, abdominal pain, pain duration, vomiting, anorexia, nausea, fever, constipation, and peritonism) and physical examination findings (eg, tachycardia, bowel sound, guarding), laboratory data (eg, white blood cell, hemoglobin, and C-reactive protein), and CT scan imaging, NOM outcome (failure vs success), intensive care unit (ICU) admission, details of hospital course and surgical procedure, and postoperative outcome (eg, death), length of follow-up time, and complications and recurrence were collected from the patient’s medical profiles. The collected CT scan findings of SBO included air-fluid level (presence vs; absent) reduction of CT small bowel wall contrast enhancement (presence vs; absent), dilated small bowel (presence vs; absent), pneumoperitoneum, a lack of colorectal gas (presence vs; absent), gasless abdomen (presence vs; absent), and level of obstruction (low vs; high).8 The collected data were thoroughly assessed for accuracy, completeness, and consistency. In cases where contradictory or missing information was identified, the charts were reviewed and reevaluated to ensure data quality.
Study Outcome
The primary outcome was predictive factors for NOM failure in small bowel obstruction.
Statistical Analysis
Quantitative variables were provided as means ± standard deviations (SD), while qualitative variables were reported as frequencies and percentages. The data’s normality was validated using the Kolmogorov–Smirnov test. All continuous variables were changed to categorical variables to improve the nomogram’s presentation. We used the chi-square test to identify significant connections between qualitative factors. Fisher’s exact test was considered appropriate in patients when the predicted frequency was constrained. Univariate analysis determined the statistically significant aspects related to NOM failure. Variables having a p-value < 0.05 in univariate analysis were included in the multivariate model. The relationships between each risk factor and NOM failure were represented by an odds ratio (OR) and 95% confidence interval (CI). A p-value of <0.05 was considered statistically significant. Statistical analyses were performed using IBM SPSS version 22 software (Armonk, New York).
Result
Patient Demographic Characteristics
Of 168 patients diagnosed with SBO, 51 patients were treated with NOM while the others underwent urgent surgical exploration. Of 51 patients, NOM failed in 18 (35.3%) and was successful in 33 (64.7%) (Figure 2). The mean age was 47.7±16.9 years (20–85 years), and 8 (15.7%) were more than 65 years. There were 32 (62.7%) males and 19 (37.3%) females. Most patients were from urban areas 33 (64.7%) and Khat chewer 38 (74.5%), while 11 (21.6%) of patients were overweight. Comorbidities included diabetes mellitus, hypertension, ischemic heart disease, and chronic renal failure in 9 (17.6%), 5 (9.8%), 5 (9.8%), and 2 (3.9%), respectively (Table 1).
 |
Table 1 Patient Demographic Characteristics |
 |
Figure 2 Clinical pathways of small bowel obstruction patients. |
Patient Symptoms, Physical Exam, and Laboratory Data Findings
Most reported symptoms were abdominal pain in 49 (96.1%) patients, and the mean duration was 84.4 ± 54.2 hours (range: 3–240 hours) with pain duration of more than three days in 21 (41.2%) patients. Constipation and vomiting were presented in 43 (84.3%) and 38 (74.5%) patients, respectively. Other symptoms were nausea, anorexia, and fever >37.5°C in 28 (54.9%), 27 (52.9%), and 19 (37.3%) patients, respectively. Abdominal scar due to previous abdominal operation was reported in 27 (52.9%) patients. The main physical examination findings were peritonism, absent bowel sound, abdominal tenderness (guarding), and tachycardia in 35 (68.6%), 18 (35.3%), 37 (72.5%), and 42 (82.4%) patients, respectively. In laboratory data, the mean Hemoglobin was 13.0 ±1.9 mg/dl, and leukocytosis (White cell count > 12× 109/L) was presented in 24 (47.1%) patients. High C- reactive protein (> 24 mg/dl) was presented in 15 (29.4%) patients (Table 2).
 |
Table 2 Patient Symptoms, Physical Exam Findings, and Laboratory Data |
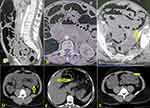
Radiologic Image Findings
A lack of colorectal gas was the most commonly reported finding in radiologic CT images in 36 (70.6%) patients. Other findings were air-fluid level, reduction of small bowel wall enhancement, dilated small bowel, and high-level obstruction in 23 (45.1%), 18 (35.3%), 5 (9.8%), and 21 (41.2%) patients, respectively (Figure 3) (Table 3).
 |
Table 3 Radiologic Computed Tomography Findings |
Univariate Analysis for Factors Associated with NOM Failure
In univariate analysis, a history of diabetes (p= 0.011), previous abdominal surgery (p= 0.004), guarding (p= 0.024), and leukocytosis (White cell count > 12× 109/L) (p=0.018), the presence of air-fluid level (p=0.022), reduction of small bowel wall enhancement (p< 0.001), and high level of obstruction (p< 0.001) were associated with NOM failure and were statistically significant (Tables 1–3).
Multivariate Analysis for Factors Associated with NOM Failure
In multivariate analysis, only reduction of small bowel wall enhancement (OR: 8.59; 95% CI:1.14–64.59, p=0.037) and high level of obstruction (OR: 11.64; 95% CI:1.34–100.85, p=0.026) were associated with NOM failure and were statistically significant. The chance of NOM failure for those with previous abdominal surgery (OR: 2.01; 95% CI:0.23–17.67), those with guarding (OR: 7.84; 95% CI:0.60–103.01), presence of air-fluid level (OR: 0.46; 95% CI:0.05–4.36), leukocytosis (OR: 2.16; 95% CI:0.29–15.95), history of diabetes (OR: 4.19; 95% CI:0.41–42.53), but these factors were not statistically significant (p > 0.05) (Table 4).
 |
Table 4 Multivariate Analysis of Predictive Factors for SBO Nonoperative Treatment Failure |
Operative and Follow-Up Findings of Filed NOM Patients
NOM failure was observed in 18 (35.3%) patients. The mean time for surgical intervention decision was 69.1 ± 53.8 hours with a median of 72 hours with a range of 24 to 240 hours. The operative findings were adhesive band, volvulus, intussusception, and mesenteric ischemia in 7 (38.9%), 5 (27.8%), 4 (22.2%), and 2 (11.1%) patients, respectively (Figure 4). Bowel resection was performed in 11 (61.1%), and 4 of them needed a colostomy diversion. Postoperative complications occurred in 13 (25.5%) patients, which included fever, paralytic ileus, surgical site infection, and reoperation (due to bleeding) in 13 (25.5%), 5 (9.8%), 4 (7.8%), and 2 (3.9%) patients, respectively. ICU admission was needed in 11 (61.1%) patients with a duration of 5.8±5.2 days (Range 1–28 days). The mean duration of hospital admission was 5.3±2.9 (Range 2–12 days). Sixteen patients were discharged with good health, and two patients expired due to mesenteric ischemia. Among NOM successful patients, recurrence has occurred in 8 (15.7%) patients (Table 5).
 |
Table 5 Operative Findings and Postoperative Findings for Patients with Nonoperative Management Failure (N= 18) |
Discussion
The management of SBO remains challenging despite cumulative years of experience and advancements in surgical literature.16 While surgical intervention is often essential, studies have demonstrated higher rates of mortality and morbidity associated with surgery compared to NOM.17,18 NOM, on the other hand, carries an elevated risk of treatment failure, exceeding 50% in some cases, underscoring the importance of proper patient selection.19 This study investigated predictive factors for NOM failure in SBO patients within a resource-limited setting. In univariate analysis, factors such as a history of diabetes mellitus, previous abdominal surgery, guarding, leukocytosis, the presence of air-fluid levels, reduction of small bowel wall enhancement, and high-level obstruction were associated with NOM failure. However, in multivariate analysis, only the reduction of small bowel wall enhancement and high-level obstruction were statistically significant predictors of NOM failure.
In this study, the failure rate of NOM was 35.3%. These findings align with prior studies reporting failure rates ranging from 20% to 57%, reflecting the heterogeneity of patient populations and the influence of possible uncontrolled variables.20,21 The term SBO encompasses a broad spectrum of clinical presentations with diverse underlying etiologies. NOM is most effective in adhesive SBO, and its application to patients with alternative etiologies may yield suboptimal outcomes.5 Notably, this study, like many retrospective analyses, did not stratify outcomes based on the underlying etiology of SBO, which may limit the interpretability and generalizability of the findings.
An analysis of the demographic and clinical profiles of our cohort showed that the majority of patients were male, with an age range of 20 to 85 years and a mean age of 47.7 years. Only 15.7% of the patients were older than 65 years. This study did not identify a significant association between advanced age and NOM failure. Similarly, prior investigations have not demonstrated a correlation between older age and failure of non-operative management for SBO.17,22 However, given the relatively small proportion of elderly patients in this cohort, these findings should be interpreted cautiously. Longer-term and larger-scale studies are warranted to elucidate the role and risks of NOM in older patients.
Consistent with findings from Cho et al, this study found no significant association between baseline characteristics such as gender, smoking history, and hypertension with therapeutic outcomes in SBO.23 Nevertheless, the presence of diabetes mellitus increased the likelihood of NOM failure by over four times in this study, though this association was not statistically significant in multivariate analysis, likely due to inherent biases and small sample size.
In this study, patients’ symptoms and physical examination findings did not demonstrate a significant relationship with the therapeutic outcome of SBO. However, univariate analysis revealed that patients with guarding were over seven times more likely to experience NOM failure, though this factor was not statistically significant in multivariate analysis. A recent systematic review identified abdominal distension and peritonism as predictors of the need for surgical intervention in SBO.12 Similarly, Schwenter et al reported six independent risk indicators, including guarding and pain duration exceeding four days.24 Zielinski et al found vomiting to be predictive of NOM failure, positing that vomiting reflects the severity and persistence of SBO. While its predictive value was limited when analyzed independently, its utility increases when considered alongside other variables.22 The authors stated that vomiting is a frequent symptom of SBO, indicating severity and persistence. Its clinical utility is lower when analyzed alone but has a high predictive potential when paired with other variables.22 This study also found that more than half of the patients had a history of previous abdominal surgery, but no significant association with NOM failure was noted. These findings align with prior literature indicating that clinical presentation and physical examination are neither sufficiently sensitive nor specific for determining the etiology, level, or severity of SBO.25,26
In this cohort, neither Khat chewing nor smoking was associated with NOM failure. These results differ from prior studies suggesting that smoking increases complications in conditions such as acute diverticulitis and bowel obstruction, including NOM failure.27 Although Khat contains cathinone and amphetamine-like compounds known to reduce gastrointestinal motility, but no significant impact on NOM outcomes was observed.28 Further research is warranted to clarify the influence of these factors on SBO management.
Leukocytosis, present in 47.1% of patients at initial presentation, doubled the likelihood of NOM failure, though this was not statistically significant in multivariate analysis. Similar findings were reported by Schwenter et al and Cho et al, who identified leukocytosis as a predictor of NOM failure.23,24 These findings suggest that elevated leukocyte counts may reflect the inflammatory severity and a heightened likelihood of requiring surgical intervention. However, additional studies are needed to substantiate this observation.
Abdominal imaging plays a pivotal role in diagnosing SBO and provides valuable information on the level and severity of obstruction.9,29,30 Advanced imaging, particularly CT, has been shown to effectively identify ischemia complicating adhesive SBO, with features such as reduced bowel wall enhancement, wall thickening, mesenteric fluid, haziness, edema, peritoneal fluid, engorged veins, whirl sign, closed-loop mechanism, pneumatosis, mesenteric or portal venous gas, and increased wall attenuation.31,32 However, the reliability of these findings depends significantly on the radiologist’s expertise.29 This study demonstrated that a reduction in small bowel wall enhancement and high-level obstruction were significantly associated with NOM failure. Consistent with our findings, Wang et al reported that intestinal wall edema and high obstruction levels increased the risk of NOM failure, though the latter was not statistically significant.33 A systematic review further highlighted the high specificity of mesenteric edema and lack of bowel wall enhancement for predicting surgical intervention.34 Zielinski et al noted that intraperitoneal free fluid was not predictive of the need for surgery, whereas mesenteric edema and the absence of small bowel feces signs were associated with NOM failure.35 We propose integrating clinical and radiological findings to optimize the assessment of surgical necessity in patients with adhesive SBO. This approach is supported by comparative studies demonstrating superior diagnostic performance.36
In this study, during the follow-up of the NOM successes of SBO patients, recurrence occurred in 8/33 (25%) of patients requiring surgical intervention. Our findings are consistent with prior reports of NOM success rates. Nevertheless, this approach allows for the persistence of the problematic adhesions, thereby increasing the likelihood of recurrence. Conversely, surgical intervention represents a more conclusive treatment modality; however, it is accompanied by the potential for the development of new adhesions and the incidence of postoperative surgical site infections, with the latter being the most prevalent postoperative complication encountered following colorectal surgery, inflicting pain and distress upon patients. Furthermore, this complication is linked to adverse economic consequences, heightened morbidity, prolonged postoperative hospitalization, readmissions, sepsis, and mortality.37,38 Despite the clinical significance of these findings, the literature remains limited to randomized clinical trials that offer a comprehensive comparative evaluation of NOM and surgical approaches, including the optimal timing for each.18 Such research is essential to guide clinical decision-making and improve outcomes for patients with SBO.
Clinical Implication
Computed tomography represents a viable alternative in countries with limited resources, particularly in instances where there exists minimal suspicion based on clinical and laboratory findings for urgent surgical intervention in SBO patients. It is recognized as the imaging modality of choice for the majority of patients presenting with SBO, due to its precision in diagnostic assessment, and ability to provide critical information that aids in understanding the underlying causes of obstruction and identifying potential complications. The implementation of CT scans for patients with SBO, in conjunction with established practices in resource-constrained environments, has the potential to enhance diagnostic accuracy and therapeutic outcomes. Consequently, we advocate for the utilization of CT scans for all patients with suspected SBO, even in settings with limited resources. To facilitate the effective integration of CT scans in resource-limited nations, it is imperative to adopt a comprehensive strategy that encompasses the education of clinical radiologists and the establishment of necessary infrastructure. This approach can augment the capabilities of local radiologists and surgeons, thereby enhancing the overall quality of healthcare delivery for patients experiencing SBO.
Study Limitations
This study has been limited by its retrospective methodology and small sample size, which assessed the medical records of SBO patients who attended the Althora General Hospital in Ibb, Yemen. Moreover, because this is a single-center study, it cannot exclude possible selection biases. A retrospective document review for patients’ ultimate diagnosis may be unrelated to their principal complaint, which needed to be more comprehensive and sensitive to obstruction-related tools. However, instead of a low sample in this report, our investigation constitutes the inaugural analysis of the predictive variables influencing NOM failure in patients experiencing SBO in Yemen. Further prospective randomized studies are required to help guide the pragmatic and surgical vs conservative decisions of SBO patients utilizing a prospective registry of consecutive patients.
Conclusion
In this study, CT scan findings of reduced small bowel wall enhancement and elevated obstruction levels are predictive factors for NOM failure in SBO patients. Nonetheless, the heterogeneity in the initial suspicion of SBO among patients constitutes a considerable confounding variable in the current analysis. The merits of surgical intervention in comparison to NOM necessitate a thorough assessment of the potential risks associated with surgical procedures, the comorbid conditions of the patient, as well as the presence or absence of bowel strangulation or ischemia. Computed tomography is typically regarded as the most suitable and precise diagnostic imaging technique for the majority of suspected SBOs. Irrespective of the imaging technique employed, the interpretation of imaging findings should adhere to a systematic and methodical protocol to ensure diagnostic precision, even in settings where resources may be limited.
Data Sharing Statement
All the data was included in this study.
Ethics Approval
The study protocol was designed following the principles of the Declaration of Helsinki and approved by the Ethics Committee of Ibb University (Code number: IBBUNI.AC.YEM.2024.10.102). After thoroughly explaining the research purpose, all the patients consented to and signed an informed consent form for the gathering of data from their medical records, as well as the publishing of their medical information and photographs, at the time of registration.
Patient Consent for Publication
Written informed consent was obtained for anonymized patient information to be published in this article.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The author declares no potential conflict of interest.
References
1. Catena F, De Simone B, Coccolini F, Di Saverio S, Sartelli M, Ansaloni L. Bowel obstruction: a narrative review for all physicians. World J Emerg Surg. 2019;14:20. doi:10.1186/s13017-019-0240-7
2. Long D, Mao C, Liu Y, Zhou T, Xu Y, Zhu Y. Global, regional, and national burden of intestinal obstruction from 1990 to 2019: an analysis from the global burden of disease study 2019. Int J Colorectal Dis. 2023;38:245. doi:10.1007/s00384-023-04522-6
3. Gao XH, Chouhan H, Gorgun E, Stocchi L, Ozuner G. Comparisons of the surgical outcomes and medical costs between transferred and directly admitted patients diagnosed with intestinal obstruction in an American Tertiary Referral Center. Int J Colorectal Dis. 2018;33:1617–1625. doi:10.1007/s00384-018-3052-4
4. Smith DA, Kashyap S, Nehring SM. Bowel Obstruction. StatPearls. Treasure Island (FL) ineligible companies. Disclosure: Sarang Kashyap declares no relevant financial relationships with ineligible companies. Disclosure: Sara Nehring declares no relevant financial relationships with ineligible companies.: StatPearls PublishingCopyright©2024, StatPearls Publishing LLC; 2024.
5. Detz DJ, Podrat JL, Muniz Castro JC, et al. Small bowel obstruction. Curr Problems Surg. 2021;58:100893.
6. Victory Srinivasan N, Khan AI, Mashat GD, et al. Recurrence of small bowel obstruction in adults after operative management of adhesive small bowel obstruction: a systematic review. Cureus. 2022;14:e29141. doi:10.7759/cureus.29141
7. Miller G, Boman J, Shrier I, Gordon PH. Etiology of small bowel obstruction. Am J Surg. 2000;180:33–36. doi:10.1016/S0002-9610(00)00407-4
8. Nelms DW, Kann BR. Imaging modalities for evaluation of intestinal obstruction. Clin Colon Rectal Surg. 2021;34:205–218. doi:10.1055/s-0041-1729737
9. Li Z, Zhang L, Liu X, Yuan F, Song B. Diagnostic utility of CT for small bowel obstruction: systematic review and meta-analysis. PLoS One. 2019;14:e0226740. doi:10.1371/journal.pone.0226740
10. Foster NM, McGory ML, Zingmond DS, Ko CY. Small bowel obstruction: a population-based appraisal. J Am Coll Surg. 2006;203:170–176. doi:10.1016/j.jamcollsurg.2006.04.020
11. Ghabisha S, Ahmed F, Altam A, Hassan F, Badheeb M. Small bowel obstruction in virgin abdomen: predictors of surgical intervention need in resource-limited setting. J Multidiscip Healthc. 2023;16:4003–4014. doi:10.2147/JMDH.S441958
12. Eze VN, Parry T, Boone D, Mallett S, Halligan S. Prognostic factors to identify resolution of small bowel obstruction without need for operative management: systematic review. Eur Radiol. 2024;34:3861–3871. doi:10.1007/s00330-023-10421-9
13. Smolarek S, Shalaby M, Paolo Angelucci G, et al. Small-bowel obstruction secondary to adhesions after open or laparoscopic colorectal surgery. Jsls. 2016;20.
14. Behman R, Nathens AB, Mason S, et al. Association of surgical intervention for adhesive small-bowel obstruction with the risk of recurrence. JAMA Surg. 2019;154:413–420. doi:10.1001/jamasurg.2018.5248
15. Bauer J, Keeley B, Krieger B, et al. Adhesive small bowel obstruction: early operative versus observational management. Am Surg. 2015;81:614–620. doi:10.1177/000313481508100627
16. Ten Broek RPG, Krielen P, Di Saverio S, et al. Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2017 update of the evidence-based guidelines from the world society of emergency surgery ASBO working group. World J Emerg Surg. 2018;13:24. doi:10.1186/s13017-018-0185-2
17. Ng ZQ, Hsu V, Tee WWH, Tan JH, Wijesuriya R. Predictors for success of non-operative management of adhesive small bowel obstruction. World J Gastrointest Surg. 2023;15:1116–1124. doi:10.4240/wjgs.v15.i6.1116
18. Hajibandeh S, Hajibandeh S, Panda N, et al. Operative versus non-operative management of adhesive small bowel obstruction: a systematic review and meta-analysis. Int J Surg. 2017;45:58–66. doi:10.1016/j.ijsu.2017.07.073
19. Williams SB, Greenspon J, Young HA, Orkin BA. Small bowel obstruction: conservative vs. surgical management. Dis Colon Rectum. 2005;48:1140–1146. doi:10.1007/s10350-004-0882-7
20. van Veen T, Ramanathan P, Ramsey L, Dort J, Tabello D. Predictive factors for operative intervention and ideal length of non-operative trial in adhesive small bowel obstruction. Surg Endosc. 2023;37:8628–8635. doi:10.1007/s00464-023-10282-9
21. Bayat Z, Guttman MP, Shiroky J, Karanicolas PJ. Non-operative management of small bowel obstruction in patients with no previous abdominal surgery: a systematic review and meta-analysis. World J Surg. 2021;45:2092–2099. doi:10.1007/s00268-021-06061-z
22. Zielinski MD, Eiken PW, Bannon MP, et al. Small bowel obstruction-who needs an operation? A multivariate prediction model. World J Surg. 2010;34:910–919. doi:10.1007/s00268-010-0479-3
23. Cho YJ, Park IS, Kim J, et al. Factors predicting the need for early surgical intervention for small bowel obstruction. Ann Coloproctol. 2020;36:223–228. doi:10.3393/ac.2019.09.30
24. Schwenter F, Poletti PA, Platon A, Perneger T, Morel P, Gervaz P. Clinicoradiological score for predicting the risk of strangulated small bowel obstruction. Br J Surg. 2010;97:1119–1125. doi:10.1002/bjs.7037
25. Chang KJ, Marin D, Kim DH, et al. ACR appropriateness Criteria® suspected small-bowel obstruction. J Am Coll Radiol. 2020;17:S305–s314. doi:10.1016/j.jacr.2020.01.025
26. Rami Reddy SR, Cappell MS. A systematic review of the clinical presentation, diagnosis, and treatment of small bowel obstruction. Curr Gastroenterol Rep. 2017;19:28. doi:10.1007/s11894-017-0566-9
27. Murzi V, Locci E, Carta A, et al. Tobacco smoking is a strong predictor of failure of conservative treatment in Hinchey IIa and IIb acute diverticulitis-a retrospective single-center cohort study. Medicina. 2023;59:1236. doi:10.3390/medicina59071236
28. Ahmed F, Alnadhari I, Ghabisha S, et al. The effects of khat (Catha edulis) use on the genitourinary system: a systematic review and meta-analysis. J Ethn Subst Abuse;2024. 1–13. doi:10.1080/15332640.2024.2382691
29. Li B, Wu Z, Wang J. The target sign: a significant CT sign for predicting small-bowel ischemia and necrosis. Radiol Med. 2024;129:368–379. doi:10.1007/s11547-024-01793-z
30. Liu M, Cheng F, Liu X, et al. Diagnosis and surgical management strategy for pediatric small bowel obstruction: experience from a single medical center. Front Surg. 2023;10:1043470. doi:10.3389/fsurg.2023.1043470
31. Sheedy SP, Earnest F, Fletcher JG, Fidler JL, Hoskin TL. CT of small-bowel ischemia associated with obstruction in emergency department patients: diagnostic performance evaluation. Radiology. 2006;241:729–736. doi:10.1148/radiol.2413050965
32. Chuong AM, Corno L, Beaussier H, et al. Assessment of bowel wall enhancement for the diagnosis of intestinal ischemia in patients with small bowel obstruction: value of adding unenhanced CT to contrast-enhanced CT. Radiology. 2016;280:98–107. doi:10.1148/radiol.2016151029
33. Wang H, Zhang JR, Tu PS, et al. Comparison of the effect between traditional conservation and nasointestinal tube placement in adhesive small bowel obstruction: a matched case-control study. Asian J Surg. 2024;47:2168–2177. doi:10.1016/j.asjsur.2024.02.042
34. Jha AK, Tang WH, Bai ZB, Xiao JQ. Sensitivity and specificity of CT and its signs for diagnosis of strangulation in patients with acute small bowel obstruction. JNMA J Nepal Med Assoc. 2014;52:735–744. doi:10.31729/jnma.2148
35. Zielinski MD, Eiken PW, Heller SF, et al. Prospective, observational validation of a multivariate small-bowel obstruction model to predict the need for operative intervention. J Am Coll Surg. 2011;212:1068–1076. doi:10.1016/j.jamcollsurg.2011.02.023
36. Schulwolf S, Brower C, Karam A, et al. Clinical features vs CT findings to estimate need for surgery in small bowel obstruction. JAMA Netw Open. 2023;6:e2341376. doi:10.1001/jamanetworkopen.2023.41376
37. Mulita F, Liolis E, Akinosoglou K, et al. Postoperative sepsis after colorectal surgery: a prospective single-center observational study and review of the literature. Prz Gastroenterol. 2022;17:47–51. doi:10.5114/pg.2021.106083
38. Verras GI, Mulita F. Butyrylcholinesterase levels correlate with surgical site infection risk and severity after colorectal surgery: a prospective single-center study. Front Surg. 2024;11:1379410. doi:10.3389/fsurg.2024.1379410
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.