Back to Journals » Infection and Drug Resistance » Volume 18
Clinical Characteristics and Predicting Disease Severity in Chlamydia psittaci Infection Based on Metagenomic Next-Generation Sequencing
Authors Huang M, Wang Y, Lu Y, Qu W, Zou Q, Zhang D, Shen Y, Han D, Yu F, Zheng S
Received 12 December 2024
Accepted for publication 8 February 2025
Published 26 February 2025 Volume 2025:18 Pages 1171—1181
DOI https://doi.org/10.2147/IDR.S509879
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sandip Patil
Mingzhu Huang,1– 3 Yuefeng Wang,1,4 Yun Lu,1,5 Wenxin Qu,1 Qianda Zou,1 Dan Zhang,1– 3 Yifei Shen,1– 3 Dongsheng Han,1– 3 Fei Yu,1– 3 Shufa Zheng1– 3
1Department of Laboratory Medicine, the First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, People’s Republic of China; 2Key Laboratory of Clinical in Vitro Diagnostic Techniques of Zhejiang Province, Hangzhou, People’s Republic of China; 3Institute of Laboratory Medicine, Zhejiang University, Hangzhou, People’s Republic of China; 4Department of Blood Transfusion, Shaoxing Maternity and Child Health Care Hospital, Shaoxing, People’s Republic of China; 5Department of Laboratory Medicine, the Children’s Hospital, Zhejiang University School of Medicine, National Clinical Research Center for Child Health, National Children’s Regional Medical Center, Hangzhou, People’s Republic of China
Correspondence: Fei Yu; Shufa Zheng, Department of Laboratory Medicine, the First Affiliated Hospital, Zhejiang University School of Medicine, No. 79, Qingchun Road, Hangzhou, 310003, People’s Republic of China, Email [email protected]; [email protected]
Introduction: Psittacosis pneumonia, as a zoonotic infection, is induced by the pathogen Chlamydia psittaci. In the present study, we sought to characterize the clinical manifestations and prognosticate the severity of psittacosis pneumonia.
Methods: We retrospectively verified instances of psittacosis pneumonia in Zhejiang province, China, from January 2021 to April 2024. Relevant data pertaining to epidemiological, clinical, and laboratory aspects were compiled and evaluated.
Results: Among a total of 110 individuals enrolled who were diagnosed with psittacosis pneumonia, the median age being 62.0 years (IQR, 53– 69 years). The most common comorbidities were hypertension (36.4%) and diabetes mellitus (17.3%). Patients categorized as having severe disease (n=68) were significantly older than those with mild disease (n=42). Most patients had notable elevations in aspartate aminotransferase (AST), creatine kinase (CK), creatine kinase-MB (CK-MB), lactate dehydrogenase (LDH), D-dimer, C-reactive protein (CRP), procalcitonin, total bilirubin (TBil), and interleukin-6, as along with significant reductions in lymphocytes, monocytes, albumin, and interleukin-4. Chest CT scans showed bilateral lung involvement in 70 cases. In the cohort of patients having received empirical antibiotic therapy, 57.3% had their antibacterial medication adjusted in light of the mNGS findings. mNGS results indicated that 31.8% (35/110) had suspected coinfections. The random forest classifiers based upon the clinical and laboratory characteristics attained AUC values of 0.822.
Discussion: The study underscores the efficacy of mNGS as a robust diagnostic tool for detecting Chlamydia psittaci, which can simultaneously detect other pathogens and guide clinical treatment. Severe patients exhibit significant inflammatory imbalances and lymphocyte depletion. A predictive model based on clinical and laboratory data at admission can effectively guide early clinical intervention.
Keywords: Chlamydia psittaci, psittacosis pneumonia, mNGS, clinical characteristics, severity
Introduction
Psittacosis pneumonia, also referred to as parrot fever or ornithosis, is a zoonotic infectious disease precipitated by the gram-negative, aerobic bacterium Chlamydia psittaci (C. psittaci).1,2 Transmission of C. psittaci primarily occurs through infected birds, poultry, livestock animals, and the secretions of infected patients or asymptomatic carriers.3 The disease can present with a variety of symptoms, varying from being asymptomatic to causing severe systemic complications. Most patients experience mild symptoms, including fever, headache, myalgia, cough, and dyspnea and generally have favorable clinical outcomes.2,4 However, in severe instances, the disease can progress to fulminant sepsis, acute respiratory distress syndrome (ARDS), multiple organ dysfunction syndrome (MODS), and potentially lead to fatality.5,6 Accounting for approximately 1.03% of community-acquired pneumonia (CAP) cases and 7.3~7.5% of severe CAP cases,6–8 psittacosis pneumonia constitutes a significant public health concern. An epidemiological research has shown that the incidence of psittacosis is elevated in males compared to females.9 The incidence of psittacosis is higher during the winter and spring seasons and is more frequently reported in the southwestern and central regions of China.2 Furthermore, recent clinical observations have noted an increasing trend of severe cases of psittacosis pneumonia.2
A multicenter retrospective investigation reported that 6.8% of Chlamydia psittaci infection was detected among patients with severe CAP in China.10 However, the actual positivity rate might be higher due to limitations in detection methods. Diagnosing psittacosis pneumonia in its early stages is challenging due to its atypical presentation, and few diagnostic tests are available. The diagnostic techniques for C. psittaci currently in use comprise of culturing the pathogen, serological testing, and polymerase chain reaction (PCR).2 However, culture methods for C. psittaci are seldom performed routinely due to their low sensitivity and the complex procedures involved. Serological tests, often prone to cross-reactions, are considered auxiliary rather than definitive.2,11 PCR, being a targeted test, is only used when there is a suspicion for the specific pathogen.2,12 Metagenomic next-generation sequencing (mNGS) represents a more comprehensive method by sequencing and analyzing both microorganisms and host nucleic acids in clinical samples, thus facilitating the rapid identification of pathogens and enabling timely initiation of targeted treatments.13 The expedited detection of pathogens is crucial for the prompt initiation of specific antibiotic therapies. Early and accurate diagnosis through mNGS has been shown to improve clinical outcomes by enabling targeted antibiotic therapy, minimizing the risk of severe complications, including ARDS and sepsis. Consequently, mNGS has increasingly been implemented in clinical practice over recent years. To date, a multitude of research has underscored its superiority and benefits for detecting Chlamydia psittaci compared with conventional diagnostic techniques.11,12
In the present study, we attempt to examine the clinical features of psittacosis pneumonia diagnosed via mNGS, and to construct a prognosticative model for severe cases on the basis of initial patient demographic information and routine laboratory indicators, aiming to provide a basis for improving clinicians’ understanding and clinical diagnosis ability of psittacosis pneumonia.
Materials and Methods
Study Design
In this retrospective analysis, we compiled data on patients with laboratory-confirmed Chlamydia psittaci cases who were admitted to the First Affiliated Hospital, Zhejiang University School of Medicine, between January 2021 and April 2024. A laboratory-confirmed case of psittacosis is defined as the detection of Chlamydia psittaci in respiratory specimens (eg, sputum, bronchoalveolar lavage fluid), swabs of the nasopharynx and oropharynx or serum using mNGS or PCR (Polymerase Chain Reaction).14 This study aligned with the ethical guidelines of the 2013 Declaration of Helsinki and was conducted after authorization by the institutional review board of the First Affiliated Hospital of Zhejiang University (IIT20240722B). Institutional review board approval was obtained to waive patient informed consent, as the data utilized do not contain any patient-identifiable information in this study.
Data Collection
We extracted the initial clinical features, laboratory test results, and radiographic findings of each patient from the hospital electronic medical record system. A panel of senior respiratory physicians independently collated, assessed, and interpreted the clinical data. The baseline characteristics encompassed details on patient demographics (eg, age and sex), medical comorbidities, clinical presentation details, severity of illness, and clinical outcome. Therapeutic interventions involved varied means of respiratory support, life-sustaining measures, and pharmacological treatment. The laboratory investigations consisted of a spectrum of analyses, including full blood count, blood biochemistry, liver and kidney functions, myocardial injury markers, inflammatory markers, and procalcitonin levels. The radiographic assessment of pulmonary lesions, which entailed evaluations of their locations and characteristics, was conducted by two experienced radiologists.
Diagnostic Criteria for Severe Pneumonia
Patients were categorized into severe and non-severe groups according to their clinical manifestations. The criteria for diagnosing severe pneumonia were derived from the eighth edition of Internal Medicine, the Infectious Diseases Association of America/American Thoracic Society (IDSA/ATS), and the Guidelines for the Diagnosis and Treatment of Community-Acquired Pneumonia in Chinese Adults.15 For a diagnosis of severe pneumonia, patients had to fulfill a minimum of one major criterion or at least three minor criteria. The principal criteria included the necessity for mechanical ventilation with endotracheal intubation, and septic shock warranting vasoactive therapy administration following active fluid resuscitation. Secondary criteria encompassed (1) respiratory rate ≥ 30 breaths/min; (2) PaO2/FiO2 ratio ≤ 250; (3) multilobar infiltrates; (4) confusion/disorientation; (5) blood urea nitrogen ≥ 7.14 mmol/L; and (6) systolic blood pressure < 90 mm Hg, with hypotension necessitating aggressive fluid resuscitation.
Metagenomic Sequencing and Data Preprocessing
mNGS was performed on 200μL of bronchoalveolar lavage fluid (BALF) and plasma samples to identify DNA and RNA pathogens.16–18 For DNA extraction, BALF samples were treated with Tween 20 (Sigma) and Benzonase (Qiagen) to remove host cells and DNA, whereas plasma samples did not require this step. Microbial DNA was extracted using the QIAamp® UCP Pathogen DNA Kit (Qiagen). RNA extraction from the samples was carried out using the QIAamp® Viral RNA Kit (Qiagen). The extracted RNA was reverse transcribed to generate cDNA, which was then processed in the same manner as the DNA samples using the NextEra XT DNA Library Prep Kit (Illumina, San Diego, CA, USA). Sequencing was performed on the Illumina Nextseq CN500 with 50 cycles of single-end sequencing (SE-50). Approximately 20 million sequencing reads were generated per sample. Quality control included the use of negative and positive control samples, and the bioinformatics analysis and result interpretation followed the same procedures as in our published study.
Predicting Psittacosis Severity Based on Clinical and Laboratory Data
To distinguish between severe and non-severe cases, we developed stratification models based on clinical and laboratory data using random forest models, which were validated through 10-fold stratified cross-validation (ie, where the dataset was divided and resampled with 10 iterations).19 For each test, the model’s accuracy was appraised using the receiver operating characteristic (ROC) curve, and low-abundance features were filtered out by determining the mean relative abundance. Specifically, the random forest modeling involved two stages. First, the model was built using either the clinical or laboratory profiles. We utilized all prefiltered features to execute the random forest function with specified parameters (500 trees, balanced class weight) and calculate the “feature importance” based on the Mean Decrease Gini. The optimal quantity of features was identified by the recursive feature elimination method, employing a parameter step size of 0.1 and utilizing five distinct random seeds. In the second phase, the combined model was formulated incorporating features identified from the individual models. The feature selection process was conducted using the recursive feature elimination technique. All computations were carried out utilizing the R software (v. 4.0.0) package “randomForest”.
Statistical Analyses
Descriptive statistics were applied to the majority of variables, including mean standard deviation (SD; for normal distribution data), median with interquartile range (IQR; for skewed distribution data), and proportion (%). For continuous variables, we employed the t-test, analysis of variance, Mann–Whitney U-test, and Kruskal–Wallis test. Categorical variables were analyzed using the χ2 test and Fisher’s exact test. A P-value of less than 0.05 was set as the threshold for statistical significance. All statistical analyses were conducted using R software (v. 3.5.3, R Project for Statistical Computing).
Results
Patient Description
A total of 110 confirmed Chlamydia psittaci infected individuals identified by mNGS were included in the study between January 2021 and April 2024, including 66 males and 44 females. The median age was 62.0 years (IQR, 53–69 years). Sixty-seven patients (60.9%) had underlying comorbidities, with 28 cases (25.5%) presenting with two or more comorbid conditions. The most prevalent comorbidities included hypertension (36.4%), diabetes mellitus (17.3%), and heart disease (16.4%). The typical clinical manifestations were fever (100%), cough (63.6%), and fatigue (44.5%). Severe cases saw a markedly higher median age compared to mild cases (P=0.003), and a greater percentage of patients with cardiac involvement and expectoration (P=0.015, P=0.012, respectively). The demographic and clinical features of the enrolled C. psittaci patients are presented in Table 1.
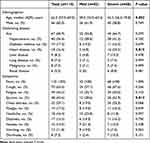 |
Table 1 Demographics and Clinical Characteristics of Patients With C. psittaci Pneumonia |
Laboratory Characteristics
Among routine laboratory indicators for all patients on admission, the lymphocyte count (P<0.001), monocytes count (P<0.001) as well as albumin (P<0.001) of those who suffered from severe disease were significantly lower than those of the patients with mild disease. Similarly, aspartate aminotransferase (AST) (P<0.001), creatine kinase (CK) (P=0.003), Creatine kinase-MB (CKMB) (P=0.004), lactate dehydrogenase (LDH) (P<0.001), D-dimer (P<0.001), C-reactive protein (CRP) (P<0.001), procalcitonin (P<0.001), and total bilirubin (TBil) (P=0.005) were significantly higher in those with severe than in those who with mild disease. Levels of inflammatory factors were measured in 16 mild cases and 32 severe cases. Among them, the pro-inflammatory factor interleukin-6 was higher in the severe cohort (P=0.030), while the anti-inflammatory interleukin-4 was higher in the mild disease group (P=0.011). The lymphocytes of 11 mild patients and 25 severe patients were classified. In severe patients, the number of CD45+ lymphocytes, CD3+ lymphocytes, CD4+ lymphocytes, CD8+ lymphocytes, CD19+ lymphocytes and CD56+ lymphocytes were markedly reduced compared to those in mild patients (P<0.001, P=0.003, P=0.003, P=0.003, P=0.005, and P=0.037, respectively). The results of all laboratory tests are detailed in Table 2.
 |
Table 2 Clinical Laboratory Characteristics of Patients With C. psittaci Pneumonia |
Radiological Manifestations
All patients in the study underwent computerized tomography (CT) scans of the lungs, revealing unilateral lesions in 40 cases (36.4%) and bilateral lesions in 70 cases (63.6%). The severe group exhibited a significantly higher proportion of bilateral lung lesions at 85.3%, compared to the mild group. Consolidation was the most frequently detected type of lesion (Figure 1A–C), followed by ground glass exudation and patch shadow (Figure 1D-F).
Treatment and Clinical Outcomes
Therapeutic interventions and clinical outcomes for patients with psittacosis pneumonia are presented in Table 3. Among the cohort, 19 (17.3%) patients received invasive mechanical ventilation, 4 (3.6%) underwent continuous renal replacement therapy, and one patient warranted extracorporeal membrane oxygenation. Corticosteroids were administered in 64.5% of cases, with significantly higher usage in patients with severe compared to those with mild disease (P=0.036). Among all patients, 45 (40.9%) were treated with tetracycline alone, 35 (31.8%) with quinolones alone and 30 (27.3%) with tetracycline and quinolones in combination. Based on mNGS results, 57.3% of patients had their antibiotic therapy adjusted. Of these, 11 received increased medications in different classes and 20 had decreased medication usage in different classes. Finally, 108 patients were discharged after recovery, while 2 patients died.
 |
Table 3 Treatments and Clinical Outcomes of Patients With C. psittaci Pneumonia |
Co-Infection With Other Pathogens Based on mNGS Findings
According to mNGS testing and clinical diagnosis, 31.8% (35/110) of the patients were identified as having secondary infections, including 11 patients in the mild group and 24 patients in the severe group (Figure 2A and C). In the severe group, viral infections (11.8%, 8/68) were the most common secondary infections, with fungal infections (7.4%, 5/68) being the next most frequent (Figure 2C). mNGS tests identified a total of 14 pathogens (11 species) and 42 pathogens (21 species) causing secondary infections in the mild and severe group, respectively (Figure 2B and D). The most prevalent pathogens in severe patients were Candida albicans (n=7) and human herpes simplex virus type 4 (HSV4) (n=6) (Figure 2D).
Predictors for Severe Pneumonia
The predictive capability of the 20 factors for classifying patients into the severe group was evaluated utilizing the ROC curve (Table 4 and Figure 3A). The area under the ROC curve (AUC) value of D-dimer, LDH, procalcitonin, lymphocyte, AST and albumin all surpassed 0.7 (0.769, 0.767, 0.756, 0.747, 0.734 and 0.719, respectively). To identify the clinical and laboratory characteristics associated with psittacosis pneumonia severity, a leave-one-out cross-validation method was implemented for the unsupervised random forest classification analysis. The random forest classifiers using the clinical and laboratory features achieved AUC values of 0.822 (Figure 3A). For the classifier, lesions in bilateral lungs, LDH, and D-dimer were the top three characteristics (Figure 3B).
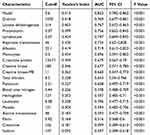 |
Table 4 ROC Curve Analysis Results |
Discussion
With the advancement of molecular diagnostic techniques, particularly mNGS, a greater number of psittacosis pneumonia cases have been identified.20,21 In the current study, we scrutinized the clinical and treatment data of 110 patients with psittacosis pneumonia diagnosed via mNGS, and established a prediction model for severe disease based clinical and laboratory indicators on admission, which provides valuable guidance for clinical treatment and timely prediction of severe disease of psittacosis pneumonia.
We observed that patients with psittacosis pneumonia tended to be older compared to those with other forms of community-acquired pneumonia,22 which may be associated with the source of C. psittaci infections, and the elderly also have an increased risk of poultry and bird exposures. Furthermore, akin to other respiratory infections, old age is also a crucial predisposing risk factor for severe or critical disease in patients with psittacosis pneumonia.23,24 This may be attributed to the deterioration of immune status and systemic function in the elderly. On the other hand, the elderly also have more underlying diseases, which also increases the risk of severe disease. Consistent with Liu’s reports, fever and cough were the most frequently observed symptoms of psittacosis pneumonia patients.25 Notably, expectoration was more common among severe cases, potentially indicating more pronounced lung inflammation in these patients.
Our findings also showed significantly reduced levels of peripheral blood lymphocytes in critically ill patients. A deeper analysis into lymphocyte subtypes revealed marked reductions across all categories in these patients, suggesting a decline in immune function. Other laboratory parameters such as Monocytes, Albumin, AST, CK, CKMB, LDH, D-dimer, CRP, Procalcitonin, and TBil also differed significantly between mild and severe cases, aligning with previous reports.20,26 It has been documented that respiratory tract pathogen infection can trigger a substantial release of cytokines and chemokines, particularly in lung activation, and mobilize neutrophils, macrophages and other inflammatory cells to the site of infection. Excessive inflammation resulted in serious injury to the alveolar epithelium, which is a significant contributor to severe infection.27,28 In severe psittacosis pneumonia patients, we noted a marked escalation in the levels of pro-inflammatory mediators, coupled with a concomitant reduction in anti-inflammatory mediators, indicating an imbalance in inflammatory responses.
It has been reported that imaging has been highlighted as highly valuable for early diagnosis of psittacosis pneumonia. Available evidence indicates that the lesions associated with psittacosis pneumonia typically manifest within the secondary pulmonary lobules, in proximity to the bronchovascular bundles, subpleurally or diffusely distributed, and the lung parenchyma and interstitium are typically implicated.29,30 These findings underscore the importance of early, targeted treatment based on imaging findings, exposure history, clinical manifestations, and laboratory tests. We advocate for more aggressive treatment in patients with bilateral pneumonia due to psittacosis.
Psittacosis pneumonia progresses rapidly, and early targeted treatment can significantly reduce the morbidity and mortality. Tetracyclines, quinolones and macrolides are the first-line and the most efficacious antibiotics for C. psittaci.15,31 A number of related studies and guidelines recommend tetracycline antibiotics as the therapy of choice for the treatment of psittacosis pneumonia, with a course of treatment typically lasting 7–10 days, where doxycycline is the most commonly used.21,30 Doxycycline was also used in nearly 70% of the patients in the present study. Our study also highlighted that empirical antimicrobial therapy often proved ineffective, with about 60% of patients requiring adjustments based on mNGS results. The presence of coinfections in patients with psittacosis pneumonia could result in more dire clinical consequences, which merits further investigation. Co-infections were detected by mNGS in 31.8% of patients in this study, which is marginally lower than 41.3% in other related works.21 Despite the detection rate of co-infection pathogens in the severe disease group was not significantly higher compared to the mild disease group, we still believe that co-infection will exacerbate the psittacosis disease severity.
The early prediction of severe psittacosis pneumonia can facilitate targeted clinical interventions, significantly reducing severe outcomes.20,32 Currently, there is a scarcity of indicators for early prediction of severe disease. In our study, further ROC curve analysis implies that D-dimer, LDH, procalcitonin, lymphocyte, AST and albumin are markers of disease severity and predictors for the development of severe pneumonia. At the same time, based on the clinical characteristics and routine laboratory indicators at admission, we used the large-scale model to establish an early prediction model for severe disease, which provided a means for early prediction of severe disease.
Our study had several limitations. First, as a single-center study, an assessment of geographical and national patient differences was not feasible. We nonetheless believe that our results are universally applicable. Second, despite enrolling 110 cases of psittacosis in our study, which is more than similar studies, the case quantity was still not sufficiently large, and selection bias may have occurred. Third, we did not select other C. psittaci detection techniques other than mNGS and therefore cannot evaluate the diagnostic efficacy of mNGS in the detection of C. psittaci. Finally, although we have a dedicated team of clinicians combined with the patient’s clinical characteristics and other relevant information to make a judgment, it remains uncertain whether other pathogens detected by mNGS contribute to the pathogenesis.
In conclusion, enhancing pathogen detection and screening for C. psittaci in patients with unexplained CAP, especially among the elderly patients with a history of bird exposure, is crucial. Patients with psittacosis pneumonia often present with atypical clinical symptoms, mainly fever and cough. Decreased peripheral blood lymphocytes and an imbalance of inflammatory factors are observed in severe cases. mNGS not only guides clinical interventions and treatment but also aids in identifying co-infectious pathogens. Furthermore, our predictive model, based on clinical and laboratory indicators at admission, offers effective early diagnostic and intervention strategies. These findings broaden our comprehension of the pathogenic mechanisms of psittacosis pneumonia, particularly in severe cases.
Acknowledgments
We acknowledge the contributions of other clinical and technical staff of the First Affiliated Hospital, Zhejiang University School of Medicine; Yu Chen (Department of Laboratory Medicine, the First Affiliated Hospital, Zhejiang University School of Medicine) for guidance in the study design; and Jili Ni (Department of Laboratory Medicine, the First Affiliated Hospital, Zhejiang University School of Medicine) for manuscript revised.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The Zhejiang Provincial Natural Science Foundation for Distinguished Young Scholar (grant number LR23H200002).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Balsamo G, Maxted AM, Midla JW, et al. Compendium of measures to control Chlamydia psittaci infection among humans (psittacosis) and pet birds (Avian Chlamydiosis), 2017. J Avian Med Surg. 2017;31(3):262–282. doi:10.1647/217-265
2. Huang W, Wang F, Cai Q, et al. Epidemiological and clinical characteristics of psittacosis among cases with complicated or atypical pulmonary infection using metagenomic next-generation sequencing: a multi-center observational study in China. Ann Clin Microbiol Antimicrob. 2023;22(1):80. doi:10.1186/s12941-023-00631-w
3. Hogerwerf L, Roof I, de Jong MJK, Dijkstra F, van der Hoek W. Animal sources for zoonotic transmission of psittacosis: a systematic review. BMC Infect Dis. 2020;20(1):192. doi:10.1186/s12879-020-4918-y
4. Branley JM, Weston KM, England J, Dwyer DE, Sorrell TC. Clinical features of endemic community-acquired psittacosis. New Microbes New Infect. 2014;2(1):7–12. doi:10.1002/2052-2975.29
5. Kovacova E, Majtan J, Botek R, et al. A fatal case of psittacosis in Slovakia, 2006. Euro Surveill. 2007;12(8):
6. Hogerwerf L, DE Gier B, Baan B, VAN DER Hoek W. Chlamydia psittaci (psittacosis) as a cause of community-acquired pneumonia: a systematic review and meta-analysis. Epidemiol Infect. 2017;145(15):3096–3105. doi:10.1017/S0950268817002060
7. Marrie TJ, Peeling RW, Reid T, De Carolis E. Canadian Chlamydia species as a cause of community-acquired pneumonia in Canada. Eur Respir J. 2003;21(5):779–784. doi:10.1183/09031936.03.00095403
8. Wu X, Li Y, Zhang M, et al. Etiology of severe community-acquired pneumonia in adults based on metagenomic next-generation sequencing: a prospective multicenter study. Infect Dis Ther. 2020;9(4):1003–1015. doi:10.1007/s40121-020-00353-y
9. Kozuki E, Arima Y, Matsui T, et al. Human psittacosis in Japan: notification trends and differences in infection source and age distribution by gender, 2007 to 2016. Ann Epidemiol. 2020;44:60–63. doi:10.1016/j.annepidem.2020.03.001
10. Qu J, Zhang J, Chen Y, et al. Aetiology of severe community acquired pneumonia in adults identified by combined detection methods: a multi-centre prospective study in China. Emerg Microbes Infect. 2022;11(1):556–566. doi:10.1080/22221751.2022.2035194
11. Chen X, Cao K, Wei Y, et al. Metagenomic next-generation sequencing in the diagnosis of severe pneumonias caused by Chlamydia psittaci. Infection. 2020;48(4):535–542. doi:10.1007/s15010-020-01429-0
12. Duan Z, Gao Y, Liu B, et al. The application value of metagenomic and whole-genome capture next-generation sequencing in the diagnosis and epidemiological analysis of psittacosis. Front Cell Infect Microbiol. 2022;12:872899. doi:10.3389/fcimb.2022.872899
13. Diao Z, Han D, Zhang R, Li J. Metagenomics next-generation sequencing tests take the stage in the diagnosis of lower respiratory tract infections. J Adv Res. 2021;38:201–212. doi:10.1016/j.jare.2021.09.012
14. Vande Weygaerde Y, Versteele C, Thijs E, et al. An unusual presentation of a case of human psittacosis. Respir MedCase Rep. 2018;23:138–142 doi:10.1016/j.rmcr.2018.01.010.
15. Mandell LA, Wunderink RG, Anzueto A, et al. Infectious diseases society of America; American thoracic society. Infectious diseases society of America/American thoracic society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44 Suppl 2(Suppl 2):S27–72. doi:10.1086/511159
16. Han D, Yu F, Zhang D, et al. The real-world clinical impact of plasma mNGS testing: an observational study. Microbiol Spectr. 2023;11(2):e0398322. doi:10.1128/spectrum.03983-22
17. Han D, Yu F, Zhang D, et al. Applicability of bronchoalveolar lavage fluid and plasma metagenomic next-generation sequencing assays in the diagnosis of pneumonia. Open Forum Infect Dis. 2023;11(1):ofad631. doi:10.1093/ofid/ofad631
18. Zhang X, Chen H, Han D, Wu W. Clinical usefulness of metagenomic next-generation sequencing for Rickettsia and Coxiella burnetii diagnosis. Eur J Clin Microbiol Infect Dis. 2023;42(6):681–689. doi:10.1007/s10096-023-04586-w
19. Shen Y, Yu F, Zhang D, et al. Dynamic alterations in the respiratory tract microbiota of patients with COVID-19 and its association with microbiota in the gut. Adv Sci. 2022;9(27):e2200956. doi:10.1002/advs.202200956
20. Gao Y, Wu Y, Xu D, et al. Chlamydia psittaci pneumonia in Wuxi, China: retrospective analysis of 55 cases and predictors of severe disease. Front Med. 2023;10:1150746. doi:10.3389/fmed.2023.1150746
21. Yuan L, Chen Q, Zhu XY, Lai LM, Zhao R, Liu Y. Evaluation of clinical characteristics and risk factors associated with Chlamydia psittaci infection based on metagenomic next-generation sequencing. BMC Microbiol. 2024;24(1):86. doi:10.1186/s12866-024-03236-1
22. Torres A, Cilloniz C, Niederman MS, et al. Pneumonia. Nat Rev Dis Primers. 2021;7(1):25. doi:10.1038/s41572-021-00259-0
23. Zheng S, Fan J, Yu F, et al. Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January-March 2020: retrospective cohort study. BMJ. 2020;369:m1443. doi:10.1136/bmj.m1443
24. Zheng S, Zou Q, Wang X, et al. Factors associated with fatality due to avian influenza A(H7N9) Infection in China. Clin Infect Dis. 2020;71(1):128–132. doi:10.1093/cid/ciz779
25. Liu K, Wu L, Chen G, et al. Clinical characteristics of Chlamydia psittaci infection diagnosed by metagenomic next-generation sequencing: a retrospective multi-center study in Fujian, China. Infect Drug Resist. 2024;17:697–708. doi:10.2147/IDR.S443953
26. Liang Y, Dong T, Li M, et al. Clinical diagnosis and etiology of patients with Chlamydia psittaci pneumonia based on metagenomic next-generation sequencing. Front Cell Infect Microbiol. 2022;12:1006117. doi:10.3389/fcimb.2022.1006117
27. Flerlage T, Boyd DF, Meliopoulos V, Thomas PG, Schultz-Cherry S. Influenza virus and SARS-CoV-2: pathogenesis and host responses in the respiratory tract. Nat Rev Microbiol. 2021;19(7):425–441. doi:10.1038/s41579-021-00542-7
28. Clementi N, Ghosh S, De Santis M, et al. Viral respiratory pathogens and lung injury. Clin Microbiol Rev. 2021;34(3):e00103–20. doi:10.1128/CMR.00103-20
29. Wu J, Pan J, Han C, et al. Clinical and CT diagnosis of 50 cases of Chlamydia psittaci pneumonia. Quant Imaging Med Surg. 2023;13(4):2053–2064. doi:10.21037/qims-22-809
30. Ni Y, Zhong H, Gu Y, et al. Clinical features, treatment, and outcome of psittacosis pneumonia: a multicenter study. Open Forum Infect Dis. 2023;10(2):ofac518. doi:10.1093/ofid/ofac518
31. Qu JM, Cao B. Guidelines for the diagnosis and treatment of adult community acquired pneumonia in China (2016 edition) [in Chinese]. Zhonghua Jie He He Hu Xi Za Zhi. 2016;39:241–242. doi:10.3760/cma.j.issn.1001-0939.2016.04.001
32. Li Y, Lin F, Li W, et al. Comparison of clinical, laboratory and radiological characteristics between Chlamydia psittaci and adenovirus pneumonias: a multicenter retrospective study. Int J Infect Dis. 2023;126:114–124. doi:10.1016/j.ijid.2022.11.029
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




