Back to Journals » Psychology Research and Behavior Management » Volume 18
Clinical Traits of Adult Depression with ADHD Comorbidity
Authors Dong L , Sun T, Tong P, Ke X
Received 6 March 2025
Accepted for publication 13 June 2025
Published 23 June 2025 Volume 2025:18 Pages 1471—1480
DOI https://doi.org/10.2147/PRBM.S526615
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Bao-Liang Zhong
Liping Dong,1,2 Ting Sun,2 Ping Tong,2 Xiaoyan Ke1
1Affifiliated Nanjing Brain Hospital, Nanjing Medical University, Nanjing, 210029, People’s Republic of China; 2Department of Clinical Psychology, Northern Jiangsu People’s Hospital, Yangzhou, 225001, People’s Republic of China
Correspondence: Ping Tong, Department of Clinical Psychology, Northern Jiangsu People’s Hospital, No. 98, Nantong West Road, Yangzhou, 225001, People’s Republic of China, Email [email protected] Xiaoyan Ke, Affiliated Nanjing Brain Hospital, Nanjing Medical University, 264 Guangzhou Road, Nanjing, Jiangsu Province, 210029, People’s Republic of China, Email [email protected]
Background: Comorbidity between attention-deficit/hyperactivity disorder (ADHD) and depression in adults is frequently observed and is associated with more complex clinical presentations and poorer prognoses. Greater emphasis is therefore warranted on identifying the distinguishing clinical characteristics of this comorbid condition.
Objective: To examine the clinical differences between adults diagnosed with depression with and without comorbid ADHD.
Methods: A cross-sectional comparative analysis was conducted involving patients with MDD, with and without comorbid ADHD. Sociodemographic and clinical variables were collected. Multivariate logistic regression analysis was performed to identify factors independently associated with ADHD comorbidity.
Results: A total of 197 patients were included in the final analysis. Significant differences in both sociodemographic and clinical variables were observed between the two groups. Multivariate logistic regression revealed that earlier age of onset (OR = 1.86, 95% CI: 1.25– 7.31), lower educational attainment (OR = 0.43, 95% CI: 0.22– 0.86), higher PHQ-9 scores (OR = 2.31, 95% CI: 1.58– 6.52), poor emotional impulsivity control (OR = 4.55, 95% CI: 2.58– 8.01), and maladaptive emotion regulation strategies (OR = 3.24, 95% CI: 2.07– 7.45) were significantly associated with the presence of ADHD in patients with depression.
Conclusion: Adults with comorbid depression and ADHD demonstrate distinct clinical features compared to those with depression alone. Key predictive factors include earlier onset of depression, lower levels of education, more severe depressive symptoms, greater difficulties in emotional impulsivity control, and the use of maladaptive emotion regulation strategies. These findings underscore the need for comprehensive assessment of emotion regulation in depressive patients, as such difficulties may signal the presence of comorbid ADHD. Interventions targeting emotional regulation may enhance diagnostic accuracy and improve treatment outcomes in this population.
Keywords: depression, ADHD, comorbidity, emotion dysregulation
Introduction
Depression is a prevalent and highly heterogeneous mental disorder, presenting significant variability in clinical manifestations.1,2 Despite extensive research, its diagnosis remains challenging, largely due to comorbidity.3,4 Attention-deficit/hyperactivity disorder (ADHD) is another common mental disorder in adults. Previous studies suggested that ADHD was limited to childhood. However, current research has clearly demonstrated that ADHD can persist into adolescence and adulthood, with approximately 30%–50% of affected children continuing to experience symptoms in adulthood.5 The prevalence has been reported to be as high as 5%.6,7 Comorbidity between depression and ADHD is frequent. According to the National Comorbidity Survey, the prevalence of depression among adults with ADHD is 18.6%,8 while adults with depression have a 9%–16% chance of also having ADHD.9,10 The comorbidity of ADHD and adult depression presents a complex clinical challenge that not only affects the mental well-being of patients but also poses a substantial economic burden on healthcare systems worldwide.11 It has been estimated that the healthcare costs associated with managing these comorbid conditions are considerable, with implications for both direct medical expenses and indirect costs related to lost productivity and impaired functioning.12 Additionally, studies have shown that depression comorbid with ADHD leads to more severe psychosocial impairment than either condition alone.13,14 Despite the increasing recognition of this comorbidity, current diagnostic and treatment approaches frequently fall short of addressing the multifaceted nature of both disorders, leading to inadequate management and poorer outcomes for patients.15
Epidemiological and clinical studies have demonstrated a close relationship between depression and ADHD.13 A four-year follow-up study on adult depression found that individuals who experienced depression before the age of 21 had a higher risk of being diagnosed with ADHD compared to those whose depression onset occurred after 21. Additionally, their depressive episodes tended to last longer.16 Research has also shown that compared to individuals with depression alone, those with comorbid depression and ADHD exhibit greater resistance to antidepressants, a higher risk of suicide, and an increased likelihood of psychiatric hospitalization.17,18 A prospective cohort study of 148 middle-aged women with recurrent depressive disorder found that ADHD symptoms were associated with an earlier onset, greater severity, and more frequent episodes of depression, along with higher irritability, increased suicide risk, a greater likelihood of hospitalization, and a higher probability of requiring non-first-line antidepressants.19 A survey study suggested that undiagnosed ADHD may be a predictor of treatment-resistant depression and that addressing underlying ADHD could improve the prognosis of patients with refractory depression.20 A one-year longitudinal study in Taiwan found that patients with comorbid depression and ADHD had a significantly higher risk of developing treatment-resistant depression than those with depression alone, while regular ADHD treatment helped reduce this risk.18 In conclusion, comorbidity leads to more severe clinical symptoms, poorer prognosis, and greater impairment in social functioning.
Several factors may explain the high prevalence of ADHD in individuals with depression. First, genome-wide association studies indicate that ADHD and depression share genetic risk factors,21 which may contribute to their frequent co-occurrence. Second, common environmental influences, such as childhood maltreatment, poverty, and low socioeconomic status, are associated with a higher likelihood of developing both ADHD22,23 and depression.22,24 Third, ADHD may increase susceptibility to mood disorders through indirect pathways. For example, ADHD-related challenges can undermine self-esteem,25 a well-established risk factor for mood disorders.26 However, challenges remain in understanding and managing this comorbidity. Overlapping symptoms make diagnosis difficult, leading to underdiagnosis or misdiagnosis. Treatments for one condition may not work well for the other, and effective therapies for comorbid patients are still unclear.
To address the gaps in understanding the clinical characteristics of patients with depression, this study aims to systematically examine the differences in clinical traits between individuals with depression alone and those with comorbid ADHD. The insights gained from this research are expected to contribute significantly to the existing literature by enhancing clinical recognition and informing treatment strategies for affected individuals.
Methods
Participants and Setting
Sample size estimation was performed using G*Power software. For this case-control study, an effect size of 0.5, a significance level (α) of 0.05, and a statistical power (1−β) of 0.9 were selected. This calculation indicated a minimum of 86 participants per group.
A total of 197 patients diagnosed with depression (including both first-episode and recurrent cases) who visited the Clinical Psychology Department of Northern Jiangsu People’s Hospital between March 2022 and June 2023 were recruited.
The inclusion criteria were: (1) Diagnosis of depression according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), confirmed by at least two psychiatrists or senior physicians; (2) Age between 18 and 35 years; (3) A Hamilton Depression Rating Scale (HAMD-17) score of ≥17; (4) Han Chinese ethnicity and right-handedness; (5) Recurrent patients must have been off psychotropic medications for at least four weeks; (6) Voluntary participation with signed informed consent.
Exclusion criteria included: (1) Mental disorders resulting from physical diseases or organic brain disorders; (2) Diagnosis of bipolar disorder; (3) Pregnant, breastfeeding, or postpartum individuals.
All 197 patients were further assessed for adult ADHD based on DSM-5 criteria and confirmed using the Conners’ Adult ADHD Diagnostic Interview. They were divided into two groups: 96 in the comorbidity group (depression with ADHD) and 101 in the pure depression (control) group. To minimize the potential impact of age and gender on the research outcomes, this study employed a matching strategy, ensuring that both groups were matched on age and gender. Statistical analysis indicated no significant differences between the two groups in terms of age and gender (p > 0.05).
Ethical Considerations
This study was approved by the Ethics Committee of Northern Jiangsu People’s Hospital and conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants prior to enrollment.
Measurements
Sociodemographic Characteristics
Gender, age, education level, marital status, monthly income, and employment status.
Clinical Characteristics
Age of depression onset, number of episodes, medication history, hospitalizations, diagnosis of treatment-resistant depression, use of non-first-line antidepressants, and history of suicide attempts.
Depressive Symptoms
Depressive symptoms were assessed using the Patient Health Questionnaire-9 (PHQ-9),27 a widely used tool for identifying depression. The PHQ-9 consists of nine items, each rated from 0 to 3, yielding a total score between 0 and 27. Higher scores indicate greater severity of depression. The PHQ-9 has demonstrated excellent internal consistency, with Cronbach’s alpha typically ranging from 0.86 to 0.89 in both clinical and general population samples.
Anxiety Symptoms
Anxiety symptoms were assessed using the Generalized Anxiety Disorder-7 (GAD-7) scale,28 which includes seven items rated from 0 to 3. The total score ranges from 0 to 21, with higher scores indicating greater severity of anxiety. The GAD-7 has demonstrated excellent internal consistency, with Cronbach’s alpha typically reported between 0.89 and 0.92 in both clinical and general population samples.
ADHD Symptoms
The Adult ADHD Self-Report Scale (ASRS)29 is a self-screening tool developed by the World Health Organization (WHO) to identify ADHD symptoms in adults. It is widely utilized in both clinical and research contexts. The ASRS consists of 18 items aligned with DSM-IV criteria for ADHD and includes two subscales: inattention and hyperactivity/impulsivity. It has demonstrated good internal consistency, with Cronbach’s alpha values typically ranging from 0.86 to 0.89 for the full scale, 0.84–0.87 for the inattention subscale, and 0.78–0.85 for the hyperactivity/impulsivity subscale.
Emotion Dysregulation
The Difficulties in Emotion Regulation Scale (DERS)30 is a self-report questionnaire developed by Gratz and Roemer in 2004 to assess challenges individuals face in regulating their emotions. It is commonly used in clinical and research settings to measure various dimensions of emotional regulation difficulties. The scale includes six subscales: use of emotion regulation strategies, goal-directed behavior, emotional clarity, emotional awareness, impulse control in response to emotions, and acceptance of emotional responses. Comprising 36 items, it utilizes a 5-point Likert scale from 1 (almost never) to 5 (almost always), with some items requiring reverse scoring. Higher total scores indicate greater difficulties in emotional regulation.
Suicide Risk
Suicide risk was assessed using specific modules of the Chinese version of the MINI Plus 5.0.0,31 a brief standardized diagnostic interview based on the criteria from the Diagnostic and Statistical Manual of Mental Disorders (DSM) or the International Classification of Diseases (ICD). Developed by trained psychologists, the MINI evaluates suicide risk and categorizes it as low (score 1–5), moderate (score 6–9), or high (score ≥ 10). The total score for the MINI suicide module ranges from 0 to 33, with higher scores indicating a greater risk of suicide.
Statistical Analysis
Demographic data were presented as frequencies and percentages. For categorical variables, chi-square tests were performed. For continuous variables, we first tested for normality using the Shapiro–Wilk test. Based on the results, Student’s t-test were used as appropriate. To account for multiple comparisons, p-values were adjusted using the Bonferroni correction where applicable. Multivariate logistic regression identified the MDD characteristics associated with ADHD, and odds ratios with 95% confidence intervals were calculated. Data analysis was performed using SPSS software (version 26.0; SPSS, Inc., Chicago, IL, USA), with statistical significance set at p < 0.05.
Results
Comparison of Demographic Characteristics Between the Two Groups
In the comorbidity group, there were 14 males (14/96, 14.58%), with an average age of 31.17 ± 2.70 years, showing no significant difference compared to the pure depression group. However, the comorbidity group exhibited a significantly lower education level (χ² = 24.105, P < 0.001), a reduced proportion of married individuals (χ² = 3.127, P = 0.043), and lower personal monthly income (χ² = 34.602, P < 0.001) compared to the pure depression group. Refer to Table 1 for details.
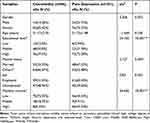 |
Table 1 Characteristics of Demographic Variables |
Comparison of Clinical Characteristics Between the Two Groups
Clinical data indicate that the comorbidity group had a younger age of onset (t = −7.58, P < 0.001), a longer duration of illness (t = 3.16, P = 0.002), and more frequent episodes (t = 3.71, P < 0.001) compared to the pure depression group. Additionally, this group had a higher proportion of patients using non-SSRI antidepressants (χ² = 4.47, P = 0.035), a greater rate of treatment-resistant depression (χ² = 27.57, P < 0.001), and more suicide attempts (χ² = 15.31, P < 0.001). They also exhibited significantly higher MINI suicide risk scores (t = 10.50, P < 0.001), PHQ-9 scores (t = 10.17, P < 0.001), and ASRS-I (t = 20.45, P < 0.001), ASRS-HI (t = 8.65, P < 0.001), and overall ASRS scores (t = 16.23, P < 0.001). In contrast, GAD-7 scores showed no significant difference (t = −1.25, P = 0.214).
Regarding emotion dysregulation, the comorbidity group had significantly higher scores in the use of emotion regulation strategies (t = 15.66, P < 0.001), target behavior activation (t = 1.98, P = 0.048), emotional understanding (t = 4.35, P < 0.001), emotional impulse control (t = 10.94, P < 0.001), and emotional response acceptance (t = 12.53, P < 0.001). They also had a higher total score (t = 12.59, P < 0.001), all statistically significant. However, scores for emotion perception showed no significant difference between the two groups (t = 1.83, P = 0.068). Refer to Table 2 for details.
 |
Table 2 Characteristics of Clinical Variables |
Multifactor Logistic Regression Analysis of Influencing Factors in Patients with Depression Comorbid with ADHD
The risk factors for patients with depression comorbid with ADHD were assessed by multiple logistic regression analyses. As shown in Table 3, independent predictors included Age of onset, Educational level, GAD-7, Emotional impulsivity control and Emotion regulation strategies. To ensure the reliability of the model, we tested for multicollinearity among the independent variables. The variance inflation factors (VIFs) for all included predictors were below 2, indicating that multicollinearity was not a concern and the model estimates were stable Refer to Table 3 for details.
 |
Table 3 Multifactor Logistic Regression Analysis of Influencing Factors for Comorbidity |
Discussion
Univariate analysis identified significant differences between the comorbidity group and the pure depression group across several factors. Demographic differences included education level, marital status, and monthly income. Clinical factors encompassed age of onset, illness duration, number of episodes, use of non-SSRI medications, prevalence of treatment-resistant depression, history of suicide attempts, MINI Suicide Risk Assessment score, PHQ-9 score, GAD-7 score, and subscales of the DERS, except for the emotional awareness subscale. However, after conducting multiple logistic regression analysis, only age of onset, education level, GAD-7 score, emotional impulsivity control scores, and the use of emotion regulation strategies remained significant as independent predictors.
Our findings indicate that individuals with comorbid ADHD experience the onset of depressive episodes at a significantly earlier age. This observation aligns with existing literature that suggests a complex interplay between ADHD and mood disorders, where the presence of ADHD may exacerbate the vulnerability to depression. Both epidemiological and clinical studies report links between early-onset depression and neurodevelopmental disorders, particularly ADHD.16 Some studies suggest that certain individuals with ADHD may experience a distinct form of depression with neurodevelopmental characteristics. This type of depression is characterized by an early onset, persistent symptoms over time, and a significant overlap with neurodevelopmental traits, including symptoms commonly associated with ADHD.32,33 Other studies suggest that the genetic architecture of early-onset depression may be primarily neurodevelopmental, with a stronger association to genetic risks linked to neurodevelopmental disorders including ADHD.34,35 Our findings appear to confirm the association between early-onset depression and ADHD. This suggests that clinical psychologists should pay particular attention to the presence of ADHD symptoms when diagnosing and treating early-onset depression. Since ADHD may exacerbate the onset and progression of depression, it is especially important to adopt an integrated treatment approach for patients with both ADHD and depression.
Previous studies have shown that children with both ADHD and depression are at higher risk for low self-esteem and poor academic performance.36 Additionally, students with ADHD are more vulnerable to risk factors such as bullying, low academic achievement, and social isolation, which contribute to higher absenteeism rates among 5 to 19-year-olds with ADHD compared to their peers.37,38 Research on adult ADHD similarly indicates that the proportion of college attendance is significantly lower in individuals with ADHD than in the general population.39 These findings collectively suggest that ADHD is associated with notable academic impairments. Of course, there are also studies with inconsistent conclusions. A Japanese study on adults with depression found no significant difference in educational attainment between those with comorbid ADHD symptoms and those without.40 Another smaller-scale study also reported similar findings.41 In contrast, our study found a significant difference in educational attainment between individuals with depression and those with comorbid ADHD. Those with lower educational levels were more likely to have ADHD. We speculate that ADHD, which typically begins in childhood, plays a key role. ADHD-related symptoms such as inattention, poor organizational skills, and executive function deficits can hinder academic performance, which in turn affects educational outcomes. Moreover, individuals with undiagnosed or untreated ADHD may miss critical opportunities for academic support, exacerbating their academic struggles and increasing dropout rates. Reduced educational achievement can have long-term socioeconomic consequences, including limited employment opportunities, lower income levels, and reduced access to social support. These socioeconomic disadvantages may, in turn, worsen mental health outcomes, creating a negative cycle that amplifies the symptom burden and functional impairment in individuals with comorbid ADHD and depression.
Consistent with previous research findings,40,41 we observed a significant difference in depression severity between the comorbid and non-comorbid groups. After controlling for other variables, severe depression was found to be a predictor of increased risk for comorbid ADHD. ADHD comorbidity may intensify depression severity through several mechanisms. There are strong longitudinal links between ADHD and depression, with childhood ADHD predicting higher depression levels into adulthood.42,43 A key factor in depression onset is self-generated stress.44 In children, life stressors like concentration difficulties, poor exam performance, or impulsive actions, such as saying hurtful things, strongly predict depressive symptoms and MDD episodes.45 These stressors are vulnerability factors, and ADHD symptoms can increase the likelihood of such stressors, worsening depressive symptoms.46 In adulthood, ADHD is linked to poor socio-economic outcomes, including lower education levels, higher unemployment, and greater risk of marital problems, criminality, and accidents.47–49 This ongoing stress and repeated sense of failure can further amplify depressive symptoms. Furthermore, several studies have found that emotion dysregulation (ED), characterized by low frustration tolerance, irritability, heightened sensitivity to negative emotions, and emotional instability, is highly prevalent among children, adolescents, and adults with ADHD.50 This difficulty in regulating emotions makes it harder for individuals to cope with daily stressors and negative experiences, further intensifying their depressive symptoms.
The study found that emotional impulsivity control and the use of emotion regulation strategies, as measured by the DERS scale, were the strongest predictors included in the multivariate logistic regression model. Among the five significant risk factors associated with comorbidity, these two variables exhibited the highest odds ratios, underscoring the pivotal role of ED in the identification and understanding of depression comorbid with ADHD. ED is the ability to modify the expression, experience, and physiology of an emotion to meet situational demands.51 While ED is a recognized feature of both depression and ADHD, its manifestations and mechanisms differ between the two disorders. Notably, existing literature has predominantly focused on ED in the context of ADHD. In individuals with ADHD, ED has been proposed as a potential core symptom or, at minimum, a distinct subtype characterized by impairments in temper control, affective lability, emotional overreactivity, impulsivity, and deficient emotional self-regulation.52–55 A meta-analysis has shown that emotional lability is a key factor distinguishing individuals with ADHD from healthy controls, with significant associations between negative emotionality and ADHD symptom severity.56 Additionally, research by Skirrow and Asherson reported that emotional lability contributes independently to functional impairment in adults with ADHD.57 It has also been estimated that approximately 70% of adults with ADHD experience ED or emotional lability.54 In this context, ED in ADHD typically involves heightened emotional reactivity, instability, and impulsivity, often reflected in abrupt shifts between emotional states and disproportionate affective responses.52 Conversely, individuals with depression also exhibit marked difficulties in emotion regulation, particularly in the modulation of negative affect. Those with a vulnerability to depression are more likely to demonstrate maladaptive regulatory patterns in response to adverse life events, thereby increasing their susceptibility to depressive episodes.58,59 These individuals often rely on dysfunctional strategies such as rumination and expressive suppression, which may further exacerbate mood symptoms and hinder emotional recovery.60,61
When ADHD and depression co-occur, deficits in emotion regulation tend to be more pronounced, resulting in heightened clinical severity and functional impairment. Emotional impulsivity or lability and persistent negative affect may interact synergistically, forming a maladaptive cycle in which emotional instability exacerbates depressive symptoms, while sustained low mood further impairs emotional control. This bidirectional dynamic may help explain the elevated levels of psychological distress, increased risk of self-harm, and poorer treatment outcomes observed in individuals with comorbid ADHD and depression compared to those with either disorder alone.
Limitations
This study has several limitations: Firstly, the study included only 197 patients, which may limit the generalizability of findings to broader populations. Secondly, matching and controlling for the variables of age and gender may influence the study results, as they could be potential influencing factors. Thirdly, key measures such as PHQ-9 scores and emotion regulation strategies rely on self-reported data, which may be subject to recall bias and social desirability effects. Finally, the study design prevents establishing causality between ADHD comorbidity and clinical characteristics in depression. A longitudinal study would better clarify the temporal relationships.
Conclusion
This study explored the clinical characteristics of adult depression comorbid with ADHD, with a particular focus on the role of emotion-related features. Significant differences were observed between patients with depression alone and those with comorbid ADHD. Earlier age of onset, lower educational attainment, higher depression severity (PHQ-9 scores), greater emotional impulsivity, and maladaptive emotion regulation strategies were identified as factors associated with ADHD comorbidity. The logistic regression model demonstrated a satisfactory capacity to distinguish between the two groups, indicating potential clinical relevance. While emotion dysregulation emerged as a key associated feature, it should be interpreted with caution given the nature of the measurement tools used. Future research using diverse assessment approaches is warranted to further clarify the role of emotional factors in the comorbidity of depression and ADHD. Interventions targeting emotional regulation may nonetheless hold promise for improving both diagnostic and therapeutic strategies in this population.
Ethics Approval and Consent to Participate
The study adhered to the guidelines of the Declaration of Helsinki and received approval from the Medical Ethics Committee of Northern Jiangsu People’s Hospital. Informed consent was obtained from all participants.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders.
2. van Eeden WA, van Hemert AM, Carlier IVE, Penninx BW, Giltay EJ. Severity, course trajectory, and within-person variability of individual symptoms in patients with major depressive disorder. Acta Psychiatr Scand. 2019;139(2):194–205. doi:10.1111/acps.12987
3. Biesheuvel-Leliefeld KE, Kok GD, Bockting CL, et al. Non-fatal disease burden for subtypes of depressive disorder: population-based epidemiological study. BMC Psychiatry. 2016;16(1):139. doi:10.1186/s12888-016-0843-4
4. Lam RW, McIntosh D, Wang J, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 Clinical Guidelines for the Management of Adults with Major Depressive Disorder: section 1. Disease Burden and Principles of Care. Can J Psychiatry. 2016;61(9):510–523. doi:10.1177/0706743716659416
5. Andreas K, Kahl Kai G. Attention-deficit/hyperactivity disorder (ADHD) in adulthood. Psychother Psychosom Med Psychol. 2004;54(3–4):124–136. doi:10.1055/s-2003-814860
6. Bonvicini C, Faraone SV, Scassellati C. Attention-deficit hyperactivity disorder in adults: a systematic review and meta-analysis of genetic, pharmacogenetic and biochemical studies. Mol Psychiatry. 2016;21(7):872–884. [published correction appears in Mol Psychiatry. 2016;21(11):1643. doi: 10.1038/mp.2016.128.]. doi:10.1038/mp.2016.74.
7. Fischer AG, Bau CH, Grevet EH, et al. The role of comorbid major depressive disorder in the clinical presentation of adult ADHD. J Psychiatr Res. 2007;41(12):991–996. doi:10.1016/j.jpsychires.2006.09.008
8. Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163(4):716–723. doi:10.1176/ajp.2006.163.4.716
9. Cumyn L, Kolar D, Keller A, Hechtman L. Current issues and trends in the diagnosis and treatment of adults with ADHD. Expert Rev Neurother. 2007;7(10):1375–1390. doi:10.1586/14737175.7.10.1375
10. Torgersen T, Gjervan B, Rasmussen K. ADHD in adults: a study of clinical characteristics, impairment and comorbidity. Nord J Psychiatry. 2006;60(1):38–43. doi:10.1080/08039480500520665
11. Hinnenthal JA, Perwien AR, Sterling KL. A comparison of service use and costs among adults with ADHD and adults with other chronic diseases. Psychiatr Serv. 2005;56(12):1593–1599. doi:10.1176/appi.ps.56.12.1593
12. Fava M, Rankin MA, Wright EC, et al. Anxiety disorders in major depression. Compr Psychiatry. 2000;41(2):97–102. doi:10.1016/s0010-440x(00)90140-8
13. Joseph B, Ball Sarah W, Monuteaux Michael C, et al. New insights into the comorbidity between ADHD and major depression in adolescent and young adult females. J. Am Acad Child Adolesc Psychiatry. 2008;47(4):426–434. doi:10.1097/CHI.0b013e31816429d3
14. Chronis-Tuscano A, Molina Brooke SG, Pelham William E, et al. Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Arch. Gen Psychiatry. 2010;67(10):1044–1051. doi:10.1001/archgenpsychiatry.2010.127
15. Bokor G, Anderson PD. Attention-Deficit/Hyperactivity Disorder. J Pharm Pract. 2014;27(4):336–349. doi:10.1177/0897190014543628
16. Bron Tannetje I, Denise B, Judith V, et al. Prevalence of ADHD symptoms across clinical stages of major depressive disorder. J Affect Disord. 2016;197:29–35. doi:10.1016/j.jad.2016.02.053
17. Biederman J, Faraone S, Milberger S, et al. A prospective 4-year follow-up study of attention-deficit hyperactivity and related disorders. Arch Gen Psychiatry. 1996;53(5):437–446. doi:10.1001/archpsyc.1996.01830050073012
18. Chen MH, Pan TL, Hsu JW, et al. Attention-deficit hyperactivity disorder comorbidity and antidepressant resistance among patients with major depression: a nationwide longitudinal study. Eur Neuropsychopharmacol. 2016;26(11):1760–1767. doi:10.1016/j.euroneuro.2016.09.369
19. Powell V, Agha SS, Jones RB, et al. ADHD in adults with recurrent depression. J Affect Disord. 2021;295:1153–1160. doi:10.1016/j.jad.2021.09.010
20. Fabbri C, Hagenaars SP, John C, et al. Genetic and clinical characteristics of treatment-resistant depression using primary care records in two UK cohorts. Mol Psychiatry. 2021;26(7):3363–3373. doi:10.1038/s41380-021-01062-9
21. Lee PH, Anttila V, Won H, et al. Genomic Relationships, Novel Loci, and Pleiotropic Mechanisms across Eight Psychiatric Disorders. Cell. 2019;179(7):1469–1482.e11.
22. Dvir Y, Ford JD, Hill M, Frazier JA. Childhood maltreatment, emotional dysregulation, and psychiatric comorbidities. Harv Rev Psychiatry. 2014;22(3):149–161. doi:10.1097/HRP.0000000000000014
23. Drew N, Knapp M, Funk M. Mental health, poverty and development. J Public Ment Health. 2012;11(4):166–185. doi:10.1108/17465721211289356
24. Pavlova B, Perroud N, Cordera P, Uher R, Dayer A, Aubry JM. Childhood maltreatment and comorbid anxiety in people with bipolar disorder. J Affect Disord. 2016;192:22–27. doi:10.1016/j.jad.2015.12.002
25. Newark PE, Elsässer M, Stieglitz RD. Self-Esteem, Self-Efficacy, and Resources in Adults With ADHD. J Atten Disord. 2016;20(3):279–290. doi:10.1177/1087054712459561
26. Henriksen IO, Ranøyen I, Indredavik MS, Stenseng F. The role of self-esteem in the development of psychiatric problems: a three-year prospective study in a clinical sample of adolescents. Child Adolesc Psychiatr Ment Health. 2017;11(1):68. doi:10.1186/s13034-017-0207-y
27. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi:10.1046/j.1525-1497.2001.016009606.x
28. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi:10.1001/archinte.166.10.1092
29. Kessler RC, Adler L, Ames M, et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35(2):245–256. doi:10.1017/s0033291704002892
30. Gratz K, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. 2008;30(4):315. doi:10.1007/s10862-008-9102-4
31. Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59 Suppl 20(20):22–57.
32. Jaffee SR, Moffitt TE, Caspi A, Fombonne E, Poulton R, Martin J. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Arch Gen Psychiatry. 2002;59(3):215–222. doi:10.1001/archpsyc.59.3.215
33. Rice F, Riglin L, Thapar AK, et al. Characterizing Developmental Trajectories and the Role of Neuropsychiatric Genetic Risk Variants in Early-Onset Depression. JAMA Psychiatry. 2019;76(3):306–313. doi:10.1001/jamapsychiatry.2018.3338
34. Musliner KL, Mortensen PB, McGrath JJ, et al. Association of Polygenic Liabilities for Major Depression, Bipolar Disorder, and Schizophrenia With Risk for Depression in the Danish Population. JAMA Psychiatry. 2019;76(5):516–525. doi:10.1001/jamapsychiatry.2018.4166
35. Power RA, Tansey KE, Buttenschøn HN, et al. Genome-wide Association for Major Depression Through Age at Onset Stratification: major Depressive Disorder Working Group of the Psychiatric Genomics Consortium. Biol Psychiatry. 2017;81(4):325–335. doi:10.1016/j.biopsych.2016.05.01
36. Cuffe SP, Visser SN, Holbrook JR, et al. ADHD and Psychiatric Comorbidity: functional Outcomes in a School-Based Sample of Children. J Atten Disord. 2020;24(9):1345–1354. doi:10.1177/1087054715613437
37. Elliott JG, Place M. Practitioner Review: school refusal: developments in conceptualisation and treatment since 2000. J Child Psychol Psychiatr. 2019;60(1):4–15. doi:10.1111/jcpp.12848
38. Vildalen VU, Brevik EJ, Haavik J, Lundervold AJ. Females With ADHD Report More Severe Symptoms Than Males on the Adult ADHD Self-Report Scale. J Atten Disord. 2019;23(9):959–967. doi:10.1177/1087054716659362
39. Kato M, Tsuda H, Chen Y, Tsuji T, Nishigaki N. The Burden of Attention-Deficit/Hyperactivity Disorder Traits in Adult Patients with Major Depressive Disorder in Japan. Neuropsychiatr Dis Treat. 2023;19:1055–1067. doi:10.2147/NDT.S399915
40. Sadeghian Nadooshan MR, Shahrivar Z, Mahmoudi Gharaie J, Salehi L. ADHD in adults with major depressive or bipolar disorder: does it affect clinical features, comorbidity, quality of life, and global functioning? BMC Psychiatry. 2022;22(1):707. doi:10.1186/s12888-022-04273-8
41. Meinzer MC, Pettit JW, Waxmonsky JG, Gnagy E, Molina BS, Pelham WE. Does Childhood Attention-Deficit/Hyperactivity Disorder (ADHD) Predict Levels of Depressive Symptoms during Emerging Adulthood? J Abnorm Child Psychol. 2016;44(4):787–797. doi:10.1007/s10802-015-0065-0
42. Rabiner DL, Anastopoulos AD, Costello J, Hoyle RH, Swartzwelder HS. Adjustment to college in students with ADHD. J Atten Disord. 2008;11(6):689–699. doi:10.1177/1087054707305106
43. Daviss WB. A review of co-morbid depression in pediatric ADHD: etiology, phenomenology, and treatment. J Child Adolesc Psychopharmacol. 2008;18(6):565–571. doi:10.1089/cap.2008.032
44. Colodro-Conde L, Couvy-Duchesne B, Zhu G, et al. A direct test of the diathesis-stress model for depression. Mol Psychiatry. 2018;23(7):1590–1596. doi:10.1038/mp.2017.130
45. Hammen C. Risk Factors for Depression: an Autobiographical Review. Annu Rev Clin Psychol. 2018;14(1):1–28. doi:10.1146/annurev-clinpsy-050817-084811
46. Ibrahim AK, Kelly SJ, Adams CE, Glazebrook C. A systematic review of studies of depression prevalence in university students. J Psychiatr Res. 2013;47(3):391–400. doi:10.1016/j.jpsychires.2012.11.015
47. Wender PH, Wolf LE, Wasserstein J. Adults with ADHD. An overview. Ann N Y Acad Sci. 2001;931:1–16.
48. Weis MD, Weiss JR. A guide to the treatment of adults with ADHD. J Clin Psychiatry. 2004;65(3):27–37.
49. Biederman J, Faraone SV, Spencer TJ, Mick E, Monuteaux MC, Aleardi M. Functional impairments in adults with self-reports of diagnosed ADHD: a controlled study of 1001 adults in the community. J Clin Psychiatry. 2006;67(4):524–540. doi:10.4088/jcp.v67n0403
50. Graziano PA, Garcia A. Attention-deficit hyperactivity disorder and children’s emotion dysregulation: a meta-analysis. Clin Psychol Rev. 2016;46:106–123. doi:10.1016/j.cpr.2016.04.011
51. Gross JJ, Thompson RA. Emotion regulation: conceptual foundations. In: Gross JJ, editor. Handbook of Emotion Regulation. New York, NY: The Guilford Press; 2007:3–24.
52. Faraone SV, Rostain AL, Blader J, et al. Practitioner Review: emotional dysregulation in attention-deficit/hyperactivity disorder - implications for clinical recognition and intervention. J Child Psychol Psychiatr. 2019;60(2):133–150. doi:10.1111/jcpp.12899
53. Marchant BK, Reimherr FW, Wender PH, Gift TE. Psychometric properties of the Self-Report Wender-Reimherr Adult Attention Deficit Disorder Scale. Ann Clin Psychiatry. 2015;27(4):267–282.
54. Skirrow C, Asherson P. Emotional lability, comorbidity and impairment in adults with attention-deficit hyperactivity disorder. J Affect Disord. 2013;147(1–3):80–86. doi:10.1016/j.jad.2012.10.011
55. Reimherr FW, Roesler M, Marchant BK, et al. Types of Adult Attention-Deficit/Hyperactivity Disorder: a Replication Analysis. J Clin Psychiatry. 2020;81(2):19m13077. doi:10.4088/JCP.19m13077
56. Beheshti A, Chavanon ML, Christiansen H. Emotion dysregulation in adults with attention deficit hyperactivity disorder: a meta-analysis. BMC Psychiatry. 2020;20(1):120. doi:10.1186/s12888-020-2442-7
57. Skirrow C, McLoughlin G, Kuntsi J, Asherson P. Behavioral, neurocognitive and treatment overlap between attention-deficit/hyperactivity disorder and mood instability. Expert Rev Neurother. 2009;9(4):489–503. doi:10.1586/ern.09.2
58. Joormann J, Stanton CH. Examining emotion regulation in depression: a review and future directions. Behav Res Ther. 2016;86:35–49. doi:10.1016/j.brat.2016.07.007
59. Yaroslavsky I, Bush AH, France CM. Emotion regulation deficits mediate childhood sexual abuse effects on stress sensitization and depression outcomes. Dev Psychopathol. 2022;34(1):157–170. doi:10.1017/S095457942000098X
60. Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking Rumination. Perspect Psychol Sci. 2008;3(5):400–424. doi:10.1111/j.1745-6924.2008.00088.x
61. Forkmann T, Scherer A, Böcker M, Pawelzik M, Gauggel S, Glaesmer H. The relation of cognitive reappraisal and expressive suppression to suicidal ideation and suicidal desire. Suicide Life Threat Behav. 2014;44(5):524–536. doi:10.1111/sltb.12076
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

