Back to Journals » Journal of Pain Research » Volume 18
Comparison of Closed Irrigation and Drainage vs Repeated Wound Dressing Changes for Iliac Crest Bone Donor Site Infection in Spine Surgery
Received 8 December 2024
Accepted for publication 19 March 2025
Published 9 April 2025 Volume 2025:18 Pages 1935—1943
DOI https://doi.org/10.2147/JPR.S511091
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Alaa Abd-Elsayed
Xiaodan Li,1 Qiang Xiao,2 Ji-Huan Zeng2
1School of Health Management, Nanchang Medical College, Nanchang, People’s Republic of China; 2Department of Orthopaedics, Jiangxi Provincial People’s Hospital, The First Affiliated Hospital of Nanchang Medical College, Nanchang, People’s Republic of China
Correspondence: Ji-Huan Zeng, Department of Orthopaedics, Jiangxi Provincial People’s Hospital, 92 AiGuo Road, Donghu District, Nanchang, 330006, People’s Republic of China, Tel/Fax +86 791 86896216, Email [email protected]
Objective: Bone donor site infection (BDSI) is a main complication of bone harvest in spine surgery. Traditionally, repeated wound dressing changes (RWDC) after debridement are commonly used to treat BDSI but are associated with significant pain and largely prolonged hospitalization. This study retrospectively compared the effectiveness of closed irrigation and drainage (CIAD) with RWDC in treating BDSI.
Methods: A total of 21 cases of BDSI secondary to different spinal procedures in a period of 15 years were included. Twelve cases were treated by RWDC in the earlier study period, and the other 9 cases were treated by CIAD in the later period. Detailed information about pre- and intra-operative characters, laboratory results, pathogens results, duration of antibiotics use, visual analog scale (VAS) score of donor site pain, total hospital stay, cost after primary operation, and final outcomes of the BDSI were collected.
Results: No significant difference was found among the included baseline characters. All patients obtained wound healing and no reinfection was found during a minimum of one year’s follow-up. However, compared to RWDC, CIAD was associated with reduced hospital stay (16.5 ± 3.8 days versus 23.7 ± 4.9 days, P < 0.05), shorter duration of antibiotic use (5.3 ± 1.7 weeks versus 6.7 ± 2.0 weeks) and lower medical cost after primary operation (5040 ± 678 yuan versus 7280 ± 701 yuan, P < 0.05). While the VAS scores of donor site pain on the day a BDSI was diagnosed did not differ in the two groups, they were significantly lower on day 3, day 7, and even on the discharge day in the CIAD group.
Conclusion: CIAD displays significant superiority to RWDC for the treatment of BDSI in terms of hospital stay, antibiotic duration, cost, and pain relief.
Keywords: bone donor site infection, pain, spine surgery, complications, wound healing
Introduction
Bone grafting is frequently used in spine procedures. It is estimated that more than two million cases of bone grafting are carried out annually worldwide.1 Despite increasing options of bone substitutes, autologous bone is still considered the “gold standard” source for its osteo-conductive, osteo-inductive, and osteogenic properties.2 However, graft harvesting introduces a second surgical site and brings donor site morbidities, such as pain, infection, neurovascular injury, hematoma, incisional hernia, fracture and sacroiliac joint injury.3 Both regarded as major complications of autologous bone grafting, while donor site pain has been well documented in the literature, bone donor site infection (BDSI) is poorly investigated.4–6 BDSI is not a rare complication,7 and is associated with prolonged hospital stay, increased medical cost, and poor clinical outcomes.8
Repeated wound dressing changes (RWDC) sequenced to debridement are commonly used to deal with BDSI. It is an effective but time-consuming method. Closed irrigation and drainage (CIAD) technique was first developed to treat osteomyelitis decades ago and is now widely used in the treatment of spinal surgical site infections, showing excellent results in shortening hospital stays and reducing medical costs.9–14 To the most of our knowledge, there was minimal data discussing CIAD in treating BDSI. Here, we performed a retrospective study to compare the effectiveness of CIAD with RWDC in treating BDSI.
Materials and Methods
Study Design
The current retrospective, observational study was approved by the Ethics Committee of the Jiangxi Provincial People’s Hospital, and all methods were performed in accordance with the Declaration of Helsinki. Informed consent to the treatment measures adopted was obtained from all patients.
A BDSI was diagnosed according to the criteria based on the 1999 Centers for Disease Control and Prevention National Health Safety Network criteria.15 In this study, BDSI was defined as deep tissue infection, and superficial infections that were restricted to the skin were excluded. Patients who met one of the following criteria were diagnosed as a BDSI: (1) donor site wound presenting purulent drainage, coupled with signs of aggravating pain, erythema, localized swelling; (2) abscess aspirated from donor site wound, and bacteria culture was positive; (3) tissue obtained from debridement procedures or suction fluid was positively cultured; (4) histopathologic evidence of infection. Unexpected elevated C-reactive protein and ESR were important clues of BDSI. The inclusion criteria were as follows: 1) Diagnosed with BDSI; 2) treated by CIAD or RWDC; and 3) a minimal follow-up of 12 months. All cases of BDSI that satisfied the inclusion criteria were divided into CIAD or RWDC groups according to the treatment they received. Pre- and intra-operative characteristics of patients with BDSI, including gender, age, comorbidity, BMI, smoking status, initial diagnosis, primary surgical site, surgical time, estimated blood loss, donor site location, and donor site incision size, were documented. Detailed data about the BDSIs, including clinical manifestations, laboratory results, pathogens results, antibiotic regimens, hospital stay, cost after the first operation and outcomes of the BDSI were collected. Specifically, the visual analog scale (VAS) score of the donor site pain at four time points during hospitalization, the first day a BDSI was diagnosed, day 3, day 7, and the discharge day, were recorded. Follow-up information was also collected to learn whether there were recurrent infection cases (Figure 1).
 |
Figure 1 Flow chart of this study. |
Treatment Protocol
Upon the diagnosis of BDSI, all patients received thorough debridement. Typically, after local anesthesia was finished, the initial sutured incision was opened to expose the wound, and samples were obtained for histopathologic staining, bacteria culture, and antibiotic sensitivity test. Necrotic tissue in the bone cavity, in the gaps between normal soft tissues and ilium tables, was removed. Lavage was continued to wash away debris from the wound.
For patients in CIAD group, a 14F inflow silicone tube for continuous irrigation was introduced through a subcutaneous tunnel to the cephalad portion of the wound from normal skin, another 16F outflow silicone tube for drainage, with two side holes in its proximal tip, was placed to the cavity caudally. The wound was tightly closed by layers with interrupted sutures. Then, the inflow tube was connected to normal saline, and the outflow tube was connected to a sterile drainage bag. Thus, a closed irrigation and drainage system was ready for use (Figure 2A and B). Normal saline without antibiotic agents was used for irrigation, the inflow volume was set at 3000 mL for every 24 hours. Drainage volume was monitored closely for early identification of possible leakage of the system. When the aspirated fluid became clean, it was collected for microbiological examination. CPR and ESR were also monitored. If the bacteria culture was negative continuously two times, coupling with decreased CPR and ESR levels, the inflow tube was removed, and 12 hours later, the outflow tube was also removed.
For patients in the RWDC group, the wounds were left unclosed after the debridement, and the wound dressing was changed every day. When the infection was controlled and the bony cavity was fully filled with granulation tissues, the wound was finally sutured.
Intravenous broad-spectrum antibiotic was initiated empirically on the diagnosis of BDSI and was maintained or changed based on the results of susceptibility testing. Intravenous antibiotic administration was continued during hospitalization. The time of discharge was generally 2 days after removal of the suction and drainage system in the CIAD group and 1 day after suture of the wound in the RWDC group. After discharge, oral administration of antibiotics lasts for another 4 weeks in all patients. Treatment success of a BDSI was defined as healing of the wound with no recurrence in one year’s follow-up.
Statistical Analysis
All statistical analyses were performed using the Statistical Packages for Social Sciences v22.0 (SPSS, Chicago, IL). Means and standard deviations were calculated for quantitative variables. Differences were tested using the t-test for symmetrically distributed continuous variables and the nonparametric Wilcoxon test for those that were not. Repeated measures ANOVA was used for comparisons between different time points, and LSD-t-test was used for multiple comparisons. For categorical variables, Fisher’s exact tests were used. A P <0.05 was accepted as significant.
Results
From January 2007 to December 2021, 647 spine procedures containing anterior or posterior iliac crest bone harvesting were conducted in the study hospital. A total of 23 cases of BDSI were diagnosed, reaching an occurrence rate of 3.55%. Patients diagnosed with BDSI presented with wound drainage (56.6%), wound dehisces (43.2%), and aggravated local pain (69.6%). Only 1 patient presented with a fever (>37.3°C). For laboratory tests, all BDSI patients showed significantly increased CRP, associated with elevated erythrocyte sedimentation rate (ESR) rate in 19 patients. Increased WBC count was found in 8 patients.
Two cases were excluded from the study for a follow-up of less than 12 months or receiving other treatment measures. Of the remaining 21 cases, 12 cases were divided into the RWDC group and 9 cases to the CIAD group. Atlantoaxial dislocation, spinal infection, and tumors were the initial diagnosis of primary surgeries needing autologous bone grafting. The baseline data of pre- and intra-operative characters in the two groups are shown in Table 1. No significant differences were found in characteristics regarding age, gender, diabetes, BMI, smoking status, initial diagnosis, primary surgical level, primary surgical time and estimated blood loss, donor site location, and donor site incision size (p > 0.05, Table 1).
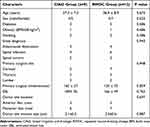 |
Table 1 Pre- and Intra-Operative Characters of Patients in CIAD and RWDC Group |
Microbiological findings were positive in 14 cases, with 6 cases in the CIAD group and 8 cases in the RWDC group. There were 5 strains of gram-positive pathogens, including 2 strains of Staphylococcus epidermidis and 3 strains of Staphylococcus aureus. Meanwhile, 9 strains of gram-negative pathogens were identified, including 4 strains of Escherichia coli, 2 strains of Acinetobacter baumannii, 2 strains of Enterobacter cloacae, and 1 strain of Klebsiella pneumonia. The duration of antibiotics for treating BDSI was 5.3 ± 1.7 weeks in the CIAD group, while it was 6.7 ± 2.0 weeks in the RWDC group (Table 2).
 |
Table 2 Microbiological Findings |
All BDSI cases were successfully treated by either CIAD or RWDC (Figure 3). However, patients in the CIAD group experienced a much faster wound-healing process. The mean length of hospital stay after the primary operation in the CIAD group was 16.5 ±3.8 days, compared to 23.7 ± 4.9 in the RWDC group (P < 0.001). In addition, CIAD significantly decreased the cost of treating BDSI. As was shown, costs after the primary operation in CIAD and RWDC group were 5040 ± 678 yuan and 7280 ± 701 yuan, respectively (p = 0.018) (Table 3).
 |
Table 3 Treatment Details and Outcome in CIAD and RWDC Group |
 |
Figure 3 The same patient with BDSI obtained primary healing of his wound by receiving CIAD treatment. |
The donor site pain since the diagnosis of a BDSI was also investigated. We found that while the VAS scores of the pain on the first day did not differ in the two groups, they were significantly lower on day 3, day 7, and even on the discharge day in the CIAD group (Figure 4). The average follow-up time was 43.7 ± 18.6 months, and no recurrence of infection was found during the follow-up.
 |
Figure 4 VAS scores of different time points in CIAD and RWDC group. * P<0.05. Abbreviations: CIAD, closed irrigation and drainage; RWDC, repeated wound dressing change. |
Discussion
Complications secondary to bone graft harvesting are generally categorized into minor and major complications. Minor complications such as superficial infection, temporary sensory loss, and mild pain, require no or minimal treatment and result in no significant harm to patients, while major complications may require a longer hospital stay, re-visit to the operation room, or even result in disabilities.16 Donor site pain and deep infection are both listed as major complications. While tremendous studies had discussed donor site pain, there was sparse literature concentrated on donor site infection. The limited existing studies reported an incidence of 1.69% to 2.48% of donor site infection after bone harvesting in various orthopedic procedures.7,16,17 The prevalence rate of BDSI was 3.55% in this study, which was slightly higher than in previous studies. Our finding suggested that BDSI was actually not scarce events secondary to bone harvesting in spine surgery. Since BDSI is an iatrogenic complication and is more likely to result in dissatisfaction, patients should be adequately counseled about this complication before spine surgeries scheduled for autografting.
It is not difficult to diagnose a BDSI if typical symptoms such as wound drainage, and wound dehiscing already happen. However, it may take several days for a BDSI to display typical symptoms since its onset. Therefore, it is essential to discover a BDSI as early as possible. We found that donor site pain was an important early symptom of a BDSI, 69.6% of patients in this study complained of unrelieved or aggravating donor site pain postoperatively. Fever was a poor indicator of BDSI, only 1 patient was found presenting fever, this might be explained by the relatively small and superficial donor site wound and a resulting mild inflammatory response. Laboratory tests were important for finding a BDSI. CRP and ESR seemed to be sensitive indicators, a large section of BDSI patients in the current study presented anomalous elevated levels of CRP and ESR. However, there was a lack of sensitivity for the WBC count in deciding on a BDSI. As was shown in the present study, only 8 BDSI patients presented increased WBC counts. Microbiological findings are important for diagnosing and treating an infection. Nevertheless, positive cultures can only be obtained in part BDSI cases. In this study, 14 samples collected from BDSI patients were positively cultured, yielding a positive rate of 66.7%, which was consistent with that in surgical site infection of primary spine surgeries.9,10
Antibiotics were the fundamental therapy for surgical site infection. While antimicrobial therapy should be started empirically once a BDSI was diagnosed, it was important to make an adjustment of the antibiotic drugs according to bacteria culture and sensitivity test. It is still controversial about an optimal duration of antibiotic treatment in treating surgical site infection following spine surgeries.18 Many researchers argued that the antibiotic therapy should last at least 6 weeks intravenously and another several weeks orally in primary surgical site infection.19,20 However, no previous study has discussed the antibiotic strategy in treating BDSI. In this study, intravenous antibiotic administration was sustained during hospitalization, it was then switched to oral administration for another 2 weeks after discharge. All BDSI were successfully cured with no reoccurrence. This course of antibiotic treatment seemed to be adequate in treating a BDSI since there are no implants and the wound is relatively small.
Aggressive debridement plays a key role in the treatment of any kind of surgical site infection,21 and so does in BDSI. In this study, patients with BDSI in both groups received thorough surgical debridement first. After that, a BDSI was conventionally managed by wound dressing changes. All BDSI cases were treated in this way during the early period of this study. It is an effective but time-consuming method. Closed irrigation technique was first described by Smith-Peterson et al for the treatment of osteomyelitis in 1945,22 and it is now widely used to treat instrumented spinal infection by curing the wound with one single surgical intervention.13 In this study, the continuously closed irrigation and drainage system was introduced for the treatment of BDSI. Our data showed that CIAD was effective in treating BDSI and significantly reduced total hospital stay, antibiotic consumption, and medical costs when compared to RWDC. The merits of CIAD derived from continuous flushing with large volumes of sterile saline and primary closure of the wound. On one hand, the uses of CIAD remove the necrotic tissues, inflammatory factors, and bacteria in the wound. On the other hand, the relatively closed space the CIAD created reduces re-contamination of the wound and is beneficial to granulation growth. Third, there is no need for a secondary closure of the wound in patients who received CIAD. Data in the present study also showed that RWDC was associated with remarkable pain at the donor site during treatment, which may significantly lower the quality of life of patients. In contrast, patients in the CIAD group experienced much less pain since day 3 after the debridement, which may be due to a faster wound healing process and less irritation to the wound. Findings of the current study indicated that compared to RWDC, CIAD represented a more efficient and economical method in treating BDSI.
Limitations
This study was limited in its retrospective design. In addition, the analysis of our results was based on a small case series, only 21 cases of BDSI were included. Although no significant difference was found in baseline characteristics such as gender, age, comorbidity, smoke status, levels of surgery, surgical duration, and estimated blood loss, due to the small study sample, it was unable for us to compare other important baseline characters, such as type of primary procedure, severity of surgical site infections. Thus, some bias might be induced. In addition, potential confounding factors, such as patient compliance, may have influenced the study outcomes.
Conclusion
BDSI was an infrequent but not a rare complication after spine surgeries with bone harvesting. Both CIAD and RWDC are effective means in treating BDSI, but CIAD displays significant superiority to RWDC in terms of hospital stay, antibiotic duration, cost and pain relief.
Data Sharing Statement
The raw data that support the findings of the current study are available from the corresponding author upon reasonable request.
Ethical Approval and Consent to Participate
The current study protocol was approved by the Ethics Committee of Jiangxi Provincial People's Hospital. Informed consent was obtained from all patients.
Funding
Science and technology plan project of Jiangxi Provincial Health Commission (202510138).
Disclosure
The authors declare that they have no conflict of interest.
References
1. Campana V, Milano G, Pagano E, et al. Bone substitutes in orthopaedic surgery: from basic science to clinical practice. J Mater Sci Mater Med. 2014;25:2445–2461. doi:10.1007/s10856-014-5240-2
2. Bauer TW, Muschler GF. Bone graft materials. An overview of the basic science. Clin Orthop Relat Res. 2000;371:10–27. doi:10.1097/00003086-200002000-00003
3. Myeroff C, Archdeacon M. Autogenous bone graft: donor sites and techniques. J Bone Joint Surg Am. 2011;93:2227–2236. doi:10.2106/JBJS.J.01513
4. Kim DH, Rhim R, Li L, et al. Prospective study of iliac crest bone graft harvest site pain and morbidity. Spine J. 2009;9:886–892. doi:10.1016/j.spinee.2009.05.006
5. Schwartz CE, Martha JF, Kowalski P, et al. Prospective evaluation of chronic pain associated with posterior autologous iliac crest bone graft harvest and its effect on postoperative outcome. Health Qual Life Outcomes. 2009;7:49. doi:10.1186/1477-7525-7-49
6. Dusseldorp JR, Mobbs RJ. Iliac crest reconstruction to reduce donor-site morbidity: technical note. Eur Spine J. 2009;18:1386–1390. doi:10.1007/s00586-009-1108-4
7. Arrington ED, Smith WJ, Chambers HG, Bucknell AL, Davino NA. Complications of iliac crest bone graft harvesting. Clin Orthop Relat Res. 1996;329:300–309. doi:10.1097/00003086-199608000-00037
8. Anderson PA, Savage JW, Vaccaro AR, et al. Prevention of surgical site infection in spine surgery. Neurosurgery. 2017;80:S114–23. doi:10.1093/neuros/nyw066
9. Zeng J, Sun X, Sun Z, et al. Negative pressure wound therapy versus closed suction irrigation system in the treatment of deep surgical site infection after lumbar surgery. World Neurosurg. 2019;127:e389–e395.
10. Yuan W, Liu X, Zhou X, Pei L, Zhu Y. Management of early deep wound infection after thoracolumbar instrumentation: continuous irrigation suction system versus vacuum-assisted closure system. Spine. 2018;43:E1089–95. doi:10.1097/BRS.0000000000002615
11. Takizawa T, Tsutsumimoto T, Yui M, Misawa H. Surgical site infections caused by methicillin-resistant Staphylococcus epidermidis after spinal instrumentation surgery. Spine. 2017;42:525–530. doi:10.1097/BRS.0000000000001792
12. Lian XF, Xu JG, Zeng BF, et al. Continuous irrigation and drainage for early postoperative deep wound infection after posterior instrumented spinal fusion. J Spinal Disord Tech. 2014;27:E315–7. doi:10.1097/BSD.0000000000000122
13. Vender JR, Hester S, Houle PJ, Choudhri HF, Rekito A, McDonnell DE. The use of closed-suction irrigation systems to manage spinal infections. J Neurosurg Spine. 2005;3:276–282. doi:10.3171/spi.2005.3.4.0276
14. Cao L, Zeng R, Sun K, Fan H. Ultrasound-guided percutaneous micro-drainage tube irrigation combined with high negative pressure tube drainage versus debridement with closed suction irrigation for treating deep surgical site infection after spinal surgery. Int Wound J. 2023;21. doi:10.1111/iwj.14435
15. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999;20:
16. Younger EM, Chapman MW. Morbidity at bone graft donor sites. J Orthop Trauma. 1989;3:192–195. doi:10.1097/00005131-198909000-00002
17. Goulet JA, Senunas LE, DeSilva GL, Greenfield ML. Autogenous iliac crest bone graft. Complications and functional assessment. Clin Orthop Relat Res. 1997;339:76–81. doi:10.1097/00003086-199706000-00011
18. Dubee V, Lenoir T, Leflon-Guibout V, Briere-Bellier C, Guigui P, Fantin B. Three-month antibiotic therapy for early-onset postoperative spinal implant infections. Clin Infect Dis. 2012;55:1481–1487. doi:10.1093/cid/cis769
19. Watanabe M, Sakai D, Matsuyama D, Yamamoto Y, Sato M, Mochida J. Risk factors for surgical site infection following spine surgery: efficacy of intraoperative saline irrigation. J Neurosurg Spine. 2010;12:540–546. doi:10.3171/2009.11.SPINE09308
20. Hegde V, Meredith DS, Kepler CK, Huang RC. Management of postoperative spinal infections. World J Orthop. 2012;3:182–189. doi:10.5312/wjo.v3.i11.182
21. Anderson DJ. Surgical site infections. Infect Dis Clin North Am. 2011;25:135–153. doi:10.1016/j.idc.2010.11.004
22. Smith-Petersen MN, Larson CB, Cochran W. Local chemotherapy with primary closure of septic wounds by means of drainage and irrigation cannulae: M. N. Smith-Petersen MD (1886–1953), Carroll B. Larson MD, Williams Cochran MD. The 12th president of the AAOS 1943 (MNS-P). Clin Orthop Relat Res. 2008;466:104–112. doi:10.1007/s11999-007-0023-4
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
The Relationship of Postoperative Pain and Opioid Consumption to Postoperative Delirium After Spine Surgery
Sica R, Wilson JM, Kim EJ, Culley DJ, Meints SM, Schreiber KL
Journal of Pain Research 2023, 16:287-294
Published Date: 28 January 2023


