Back to Journals » Journal of Pain Research » Volume 18
Comparison of Costotransverse Foramen Block with Thoracic Paravertebral Block and Erector Spinae Plane Block for Patients Undergoing Video-Assisted Thoracoscopic Surgery: A Randomized Controlled Non-Inferiority Trial
Authors Li J, Shao P, Wen H, Ma D, Yang L, He J, Jiang J
Received 20 January 2025
Accepted for publication 8 May 2025
Published 13 May 2025 Volume 2025:18 Pages 2427—2438
DOI https://doi.org/10.2147/JPR.S518558
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Jinlei Li
Jing Li,1,* Peiqi Shao,2,* Hong Wen,3 Danxu Ma,2 Lina Yang,3 Jianshuai He,4 Jia Jiang3
1Department of Anesthesiology, Beijing Tongzhou District Hospital of Integrated TCM and Western Medicine, Beijing, People’s Republic of China; 2Department of Anesthesiology, Beijing Friendship Hospital, Capital Medical University, Beijing, People’s Republic of China; 3Department of Anesthesiology, Beijing Chaoyang Hospital, Capital Medical University, Beijing, People’s Republic of China; 4Department of Anesthesiology, the Affiliated Hospital of Qingdao University, Shandong, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jia Jiang, Department of Anesthesiology, Beijing Chaoyang Hospital, Capital Medical University, No. 8, Gongtinan Road, Chaoyang District, Beijing, 100020, People’s Republic of China, Email [email protected]
Purpose: This study aimed to investigate the safety and efficacy of costotransverse foramen block for postoperative analgesia in video-assisted thoracoscopic surgery (VATS).
Patients and Methods: Seventy-five patients undergoing elective VATS under general anaesthesia were recruited to this double-blind, non- inferiority trial and randomized to preoperatively receive a thoracic paravertebral block (TPVB group), a costotransverse foramen block (CTFB group), or an erector spinae plane block (ESPB group) with 0.5% ropivacaine 20 mL at T5 level. The primary outcome was the postoperative numerical rating scale pain score assessed at 6 h. Secondary outcomes included pain scores at other time points, total opioids consumption at 24 h postoperatively, time to first patient-controlled analgesia pump bolus, number of patients requiring rescue analgesia, dermatomal coverage at 30 min after block, time to perform the block, satisfaction scores of the analgesic effect, block-related side effects, and other complications. The health-related quality of life was evaluated one month after surgery.
Results: The pain scores at 6 h after surgery were 0 (0, 3) in the TPVB group, 0 (0, 2) in the CTFB group, and 4 (3, 4) in the ESPB group. The 95% CI of median difference was 0 to 0 comparing CTFB with TPVB and − 4 to − 2 comparing CTFB with ESPB. Both the upper 95% CI limits were lower than the predefined noninferiority margin of 1. The pain scores at postanaesthesia care unit, 1 h, 6 h and 12 h after surgery, number of block dermatomes, patient satisfaction scores, time to perform the block as well as the time to first analgesia pump bolus were significantly different between the CTFB group and ESPB group. No differences were detected in other secondary outcomes.
Conclusion: Ultrasound-guided CTFB provided noninferior analgesia compared to TPVB at 6 h after VATS. Additionally, CTFB might provide better analgesia to ESPB although larger confirmatory researches for superiority are further warranted.
Keywords: postoperative analgesia, thoracoscopic surgery, ultrasound, regional anesthesia
Introduction
Video-assisted thoracic surgery is a minimally invasive procedure, which is, however, often associated with moderate-to-severe postoperative pain involving both somatic and visceral components, leading to delayed recovery and higher incidence of complications such as atelectasis and pulmonary infection due to ineffective breathing and clearing of secretions.1,2 Effective postoperative pain management may reduce these complications and the risk of chronic pain.
The thoracic paravertebral block has long been the preferred effective regional anaesthesia for thoracic surgery.3 It is a demanding technique with potential risks of several complications. Even with an ultrasound, the risk of pneumothorax and unexpected spread of local anesthetic into the epidural space cannot be avoided.4 Moreover, the thoracic paravertebral block needs to pierce the superior costotransverse ligaments, the resultant opening pressure in the paravertebral space will cause patients feel uncomfortable.
Interest in ultrasound-guided fascial plane blocks has been steadily increasing in recent years. Proxy blocks like the erector spinae plane block,5,6 retrolaminar block,7 the mid‐point transverse process to pleura block,8 and the thoracic paravertebral block multiple‐injection costotransverse block9 have provided alternatives to thoracic paravertebral block. These superficial blocks have a minimal risk of pneumothorax without actually piercing the superior costotransverse ligaments and placing the needle tip inside the thoracic paravertebral space close to the pleura. Although they are expected to achieve a similar analgesic effect compared to thoracic paravertebral block, the mechanisms of these novel blocks have not been clarified and their clinical value is still controversial. Theoretically, the success of these blocks depends on whether the local anesthetic can spread through superior costotransverse ligaments or through the costotransverse foramen, finally reaching the paravertebral space.10–12
A novel technique called the costotransverse foramen block was first described by Shibana et al recently.10 Cadaveric and case studies demonstrated that a solution injected directly into costotransverse foramen can consistently spread to paravertebral space.10 However, there have been no studies published comparing the costotransverse foramen block to the thoracic paravertebral block or erector spinae plane block for patients undergoing video-assisted thoracic surgery. The intent of the current study was to compare the safety and analgesic efficacy of these blocks under the hypothesis that the costotransverse foramen block would provide noninferior postoperative analgesia to thoracic paravertebral block and erector spinae plane block following video-assisted thoracic surgery. The primary outcome was the numerical rating scale pain score at 6 h after surgery.
Materials and Methods
Study Design
The trial was approved by the ethics committee of Beijing Chao-Yang Hospital (2019-ke-369) and performed at the department of Anesthesiology, Beijing Chao-Yang Hospital, Capital Medical University between January 2021 and January 2022. The study was registered with Chinese Clinical Trial Registry (ChiCTR2100041815) on January 6, 2021. All patients provided written informed consent before the day of surgery. Our study complies with the Consolidated Standards of Reporting Trials guidelines and the Declaration of Helsinki.13 Patients scheduled to undergo video-assisted thoracic surgery were eligible for enrolment in this study if they were between 18 years and 65 years and had an American Society of Anesthesiologists (ASA) physical status of I to III. We excluded the patients with puncture site infection, coagulopathy, allergy to local anesthetic, body mass index >40 kg m−2, incompatibility of body position, lack of consent for the procedure, decreased pulmonary reserve, major cardiac disorders, liver and renal dysfunction, pre-existing neurological deficits, or psychiatric illness.
Patient Grouping, Blinding, and Randomization
Based on a computer-generated randomized number, eligible patients were randomly allocated in a 1:1:1 ratio to receive costotransverse foramen block (CTFB group), thoracic paravertebral block (TPVB group), or erector spinae plane block (ESPB group). Random numbers were concealed in sequentially numbered opaque envelopes that were opened by anesthesiologists before the nerve block. Only the anesthesiologists who performed the block and assisted with the procedure were aware of the allocation. The patients and study personnel responsible for postoperative data collection were blinded to group allocation.
Block Interventions
Before the operation, patients were taught how to use the numerical rating scale (0–10, a modified version, Table S1) to score the pain intensity. In the preoperative preparation room, SpO2, electroencephalography, and non-invasive blood pressure were monitored for the patients. Venous vascular access was established and oxygen was given. Patients were premedicated with intravenous midazolam (0.02 to 0.03 mg.kg−1) and sufentanil (0.05 to 0.1 μg.kg−1) titrated at the discretion of the anesthesiologists. The blocks were performed by one of the three skilled anesthesiologists (Jia Jiang, Hong Wen, or Danxu Ma).
All the blocks were performed at T5 vertebral level under ultrasound guidance with patients in prone position. Using an in-plane or an out-plane technique, a high-frequency linear or a low-frequency convex ultrasound transducer (Navi Series, Wisonic Medical Technology Co. Ltd., Shenzhen, China) covered with a sterile sleeve was placed in a sagittal orientation lateral to the posterior midline to identify the T5 transverse process. The skin was disinfected with iodophor, and 1 mL of 2% lidocaine was injected intradermal for local anaesthesia. A 22G 80-mm needle (Stimuplex D, B. Braun, Melsungen AG, Germany) was chosen for all blocks.
In the CTFB group, according to the technique described by Shibata et al, the transducer was shifted lateral-to-medial to identify the neck of sixth rib, the base of the T5 transverse process, the laminar, and the pleura if possible.10 The needle was advanced caudal-to-cephalad until the needle tip contacted the anteroinferior part of the base of the T5 transverse process. The correct needle tip position was confirmed by a test dose of 1–5 mL of 0.9% normal saline solution to visualize the spreading of local anesthetic in an anterior direction rather than a backward spread of the injectate resulting in a bulging of the erector spinae muscle or the muscle fascial plane (Figure 1A–C).
In the TPVB group, the transducer was tilted obliquely to locate the superior costotransverse ligaments between the T5 transverse process and the T6 transverse process. Using a caudal‐cranial needle trajectory, the needle pierced the superior costotransverse ligaments and the correct needle tip position was confirmed by a test dose of 1–5 mL of 0.9% normal saline solution to visualize the ventral movement of the parietal pleura (Figure 1B–D).
In the ESPB group, the needle was inserted in a caudal-cranial direction deep to the erector spinae muscle (Figure 1E). The correct position of the needle tip was controlled with administration of 1 mL of local anesthetic distributed as both cranial and caudal directions.
After negative aspiration, patients in three arms of the study received the same local anesthetic (20 mL of 0.5% ropivacaine). Dermatomal distribution with pinprick sensation was monitored on the anterolateral chest every 5 min for 30 min after the completion of the block.
General Anesthesia Management
Anesthesia was conducted in accordance with a standardized protocol. After the blocks, all patients were taken from the preparation area directly to the operation room, where the SpO2, electroencephalography and the invasive arterial blood pressure were monitored during surgery. The depth of sedation and the degree of brain response to nociceptive stimuli during surgery were monitored using multifunction combination monitor HXD‑I (Beijing Easymonitor Technology Co., Ltd., Beijing, China). General anaesthesia was induced with sufentanil 0.2 to 0.3 μg.kg−1, and propofol 2 to 3 mg.kg−1. Rocuronium bromide 0.6 to 0.8 mg.kg−1 was administered to facilitate double-lumen tracheal intubation. Anesthesia was maintained by infusion of propofol (0.1 to 0.15 mg kg-1 min-1) and remifentanil (0.1 to 0.3 g kg-1 min-1), and targeted for a wavelet index of 36 to 60 and pain threshold index of 40 to 60. At the conclusion of surgery, patients were extubated and transported to the postanaesthesia care unit (PACU).
Postoperative Analgesia
On arrival at the PACU, all patients were connected to an intravenous patient-controlled analgesia (PCA) pump containing sufentanil 1 μg.mL−1 with the following settings: background infusion 1 μg.h−1, demand dose 2 μg, and lockout time of 15 min. Patients were instructed to administer a bolus whenever numerical rating scale pain scores >3. The standard postoperative analgesic regime consisted of 50 mg flurbiprofen axetil intravenously at the end of surgery, 50 mg flurbiprofen axetil intravenously every 12 h after surgery. For patients with a numerical rating scale pain score remained >3 after two consecutive sufentanil bolus, oral ibuprofen-codeine tablets (each tablet containing ibuprofen 0.2 g and codeine 12.5 mg; two tablets for the first use and no more than 6 tablets per day) were administered as rescue analgesia.
Outcome Measures
The primary outcome was numerical rating scale pain score at 6h after surgery. The secondary outcomes included numerical rating scale pain scores at other time-points, cumulative oral morphine equivalent consumption within the first 24 h after surgery, time to first PCA bolus, number of patients requiring rescue analgesia, total doses of rescue analgesia (expressed as oral morphine equivalents), dermatomal coverage at 30 min after block, patient satisfaction score (4 = “very dissatisfied”, 3 = “dissatisfied”, 2 = “satisfied”, 1 = “very satisfied”), block-related side effects (unexpected epidural anaesthesia, pneumothorax, total spinal anaesthesia, or local anesthetic intoxication), postoperative complications (postoperative nausea and vomiting (PONV), drowsiness, or dyspnea), and length of hospital stay (days from surgery to discharge). Intraoperative and postoperative complications were assessed according to the classifications of intraoperative adverse events (ClassIntra) version 1.014 and the Clavien-Dindo surgical complication classifications (CD classification), respectively, within seven days after surgery or before discharge.15 The health-related quality of life was also evaluated by using the EQ-5D-3L questionnaire one month after surgery. The information derived from the EQ-5D was converted into a single summary index (EQ-5Dindex or EQ-5D Time Trade-Off Value (TTO) with UK scoring (Table S2).16,17
Sample Size Calculation
This study was designed to assess the noninferiority of analgesic effect in CTFB cohorts compared to TPVB and ESPB groups undergoing video-assisted thoracic surgery. The sample size calculation was determined according to the primary outcome of numerical rating scale pain score at 6 h after surgery. According to previous literature, the non-inferiority margin was determined a priori to be 1.18,19 In pilot study, we observed 5 patients in each CTFB, TPVB, and ESPB group, and mean numerical rating scale scores at 6 h after surgery were 0.8, 0.8, and 3.6, respectively, with a similar SD of 1.0. One-tailed power analysis indicated that a sample size of 21 subjects per group would provide at least 80% power with an alpha of 0.0125 to demonstrate the noninferiority of costotransverse foramen block to thoracic paravertebral block and erector spinae plane block. Bonferroni method was used for the correction for Type I error. Taking into account about 20% of the loss to follow-up rate, 75 (25 in each group) patients should be enrolled.
Statistical Analysis
Statistical analysis was performed using GraphPad Prism version 9.5 (GraphPad Software Inc., San Diego, CA, USA) and IBM SPSS statistics for Windows version 26.0 (IBM Corp., Armonk, New York, USA). Categorical variables were reported as number (percentage) and continuous variables as mean (SD) or median (IQR [range]) according to the distribution characteristics of the data. The normality of distribution of continuous variables was analyzed by the Kolmogorov–Smirnov test. Normally distributed continuous data were analyzed using one-way analysis of variance (ANOVA), while nonnormal data were analyzed with Kruskal–Wallis test across groups. If the significant difference was indicated among three groups, pairwise comparisons (CTFB group vs TPVB group, and CTFB group vs ESPB group) were performed according to appropriate post-hoc tests with p <0.025 adjusted Bonferroni correction. Mann–Whitney U-test was used for pairwise analysis of continuous data. Comparisons of categorical variables were performed using Chi-Square test or Fisher exact test. For the data that could not be statistically analyzed, such as the dermatomal coverage of sensory block, a descriptive result was planned.
Non-inferiority testing was done by comparing the 95% CI of median/mean difference using the Hodges–Lehmann method between groups to the prespecified noninferiority margin. We compared both intention-to-treat analysis and per protocol analysis. If noninferiority was met, superiority of costotransverse foramen block was to be tested using the intention-to-treat population. Superiority was achieved if the upper limit of the 95% CI of the median difference was lower than 0.
Results
Between January 2021 and January 2022, 255 patients were assessed for eligibility, of which 75 patients were enrolled and allocated randomly. Six patients were excluded from final per protocol analysis because one was converted to open thoracotomy for severe adhesion, two were failed to block and three were lost to follow-up due to transfer to ICU (Figure 2). Block failure occurred in one patient in the CTFB group with the needle tip displaced at lamina, and one in the ESPB group for noncooperation with the block procedure. There was no imbalance in demographic data and surgical data among three groups (Table 1).
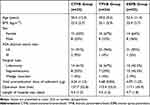 |
Table 1 Baseline Characteristics and Procedure Data of Patients Receiving Costotransverse Foramen Block, Thoracic Paravertebral Block, or Erector Spinae Plane Block for Thoracic Surgery |
 |
Figure 2 CONSORT flow diagram of patients. |
The costotransverse foramen block was demonstrated to be non-inferior to both the thoracic paravertebral block and the erector spinae plane block, based on a predefined non-inferiority margin of 1. For per protocol population, the numerical rating scale score at 6 h after surgery was 0 (0, 1) for CTFB group and 0 (0, 3) for TPVB group with a median difference 0 (95% CI, 0 to 0) in the comparison of CTFB and TPVB groups. Comparing the CTFB group with ESPB group, the numerical rating scale pain scores were 0 (0, 1) for CTFB group and 4 (3, 4) for ESPB group with a median difference −3 (95% CI, −4 to −2). Both upper limits of the 95% CI were less than the predetermined noninferiority margin of 1. For intention-to-treat analysis, the numerical rating scale pain scores at 6 h after surgery were 0 (0, 1.5), 0 (0, 3), 4 (3, 4) for CTFB, TPVB and ESPB groups, respectively. The median difference was 0 (95% CI, 0 to 0) between the CTFB group and TPVB group, and −3 (95% CI, −4 to −2) between the CTFB group and ESPB group. Both analyses indicated that costotransverse foramen block was noninferior to thoracic paravertebral block and erector spinae plane block. After establishing noninferiority, costotransverse foramen block was also confirmed as superior to erector spinae plane block, since the upper limit of the 95% CI was lower than 0 (Figure 3).
As indicated in Table 1, numerical rating scale pain scores at PACU, 1 h, 6 h and 12 h after surgery were significantly different among three groups. These differences were statistically significant between CTFB group and ESPB group, but not for CTFB group vs TPVB group. No differences in numerical rating scale pain scores at 24 h and 48 h were detected. Moreover, no significant difference in numerical rating scale pain scores was found between CTFB group and TPVB group at all time points. The CTFB group exhibited a significantly longer duration until the initial request for PCA bolus compared to ESPB group (median difference, 8; 95% CI, 4–9; P = 0.001; Table 2). Patients in ESPB group showed significantly higher satisfaction score compared to CTFB group (P = 0.019; Table 2). Cumulative oral morphine equivalent consumption at 24 h postoperatively, total dose of rescue analgesics, and the number of patients requiring analgesia were comparable among the three groups (Table 2).
 |
Table 2 Efficacy Outcomes of Patients Receiving Costotransverse Foramen Block, Thoracic Paravertebral Block, or Erector Spinae Plane Block for Thoracic Surgery |
Two patients in CTFB and TPVB groups had unexpected epidural spread of the local anesthetic without any serious consequences. There were no significant differences in block-related side effects and complications in these groups (Table 3). ClassIntra and CD classifications were comparable among groups. Eighteen patients in CTFB group,19 patients in TPVB group and 17 patients in ESPB group completed the one-month follow-up, and EQ-5Dindex was similar for three interventions at one month after surgery (P = 0.965; Table 3).
 |
Table 3 Complications and Recovery Quality of Patients Receiving Costotransverse Foramen Block, Thoracic Paravertebral Block, or Erector Spinae Plane Block for Thoracic Surgery |
The median (IQR) highest sensory levels were both T3 (T3-T4) in CTFB and TPVB groups, while the lowest levels were T7 (T6-T8) in CTFB group and T8 (T6-T8.75) in TPVB group. T3 to T7 dermatomes were covered in more than 60% patients in CTFB and TPVB groups. For patients with epidural spread, the range of the sensory block dermatomes (affected side/non-affected side) were: CTFB group-T3-T10/T3-T10, T3-T12/T3-T12; TPVB group-T4-T10/T5-T8, T4-T12/T4-T9. The sensory block level was detected in only eight patients in ESPB group, ranged from the highest T3 and lowest T8 (Figure 4). The costotransverse foramen block blocked more dermatomes compared with erector spinae plane block (median difference, 4; 95% CI, 3–5; P < 0.001), but similar count compared with thoracic paravertebral block. The costotransverse foramen block procedure was more time-consuming than the thoracic paravertebral block (median difference, 7; 95% CI, 5–8; P < 0.001) and erector spinae plane block (median difference, 7; 95% CI, 7–8; P < 0.001).
Discussion
Our findings demonstrated that ultrasound-guided CTFB achieved non-inferior early postoperative analgesia compared to TPVB, while exhibiting superior analgesic efficacy relative to ESPB at 6 h after surgery with a multimodal analgesia regimen after video-assisted thoracic surgery. There were significantly different in numerical rating scale pain scores at other time points (PACU, 1 h, 12 h), time for first PCA demand, patient satisfaction score and dermatomal coverage between CTFB group and ESPB group. Notably, to our knowledge, this was the first randomized controlled study to compare costotransverse foramen block with thoracic paravertebral block and erector spinae plane block on analgesic effect after video-assisted thoracic surgery.
The costotransverse foramen is a fissure between the neck of the rib and the superior costotransverse ligaments, which allows the dorsal ramus and accompanying blood vessels through. It is defined medially by the thoracic lamina, laterally by the superior costotransverse ligaments, cranially to the base of the transverse process, caudally to the neck of the rib below, posteriorly to the intertransverse ligament, and anteriorly continuous with the paravertebral space.10,20 Therefore, local anesthetic injected into the costotransverse foramen will theoretically penetrate into the paravertebral space without any obstacles. One cadaveric study showed that costotransverse foramen block resulted in a consistent anterior spread of dye into the paravertebral space.10 Our study verified that sensory assessment of anterior chest wall revealed a dermatome coverage with costotransverse foramen block from T3 to T7 on the affected side in more than 60% of the patients, which was comparable to the thoracic paravertebral block. These observations align with the recent findings by Oh et al.21
We chose the numerical rating scale (NRS) pain score at 6 h postoperatively as the primary outcome to ensure that the effects of all nerve blocks remained active during assessment, allowing us to accurately evaluate their early analgesic efficacy. In recent years, people have been trying to find proxy methods to replace the paravertebral block.22,23 Among which, erector spinae plane block with its relatively simple technique and superficial anatomical landmarks is being rapidly adopted clinically.5 The mechanism of the erector spinae plane block has been scrutinized, yet far less clarified.24 The considerable discrepancy in clinical efficacy echoes the unpredictable dissemination of the injectate in cadaveric studies.9,11,25,26 This can be explained by the complexity of the paravertebral structures.27 Although the superior costotransverse ligament is not completely continuous, the local anesthetic in the erector spinae plane block has to traverse the intertransverse tissue complex before entering the paravertebral space.28 In addition, the exact needle tip position, the volume administered, patients’ respiration, the tonicity of the musculature, the depth of the anaesthesia, as well as the disposition and composition of the ligaments along the spinal column, will all affect the spread of the local anesthetic.29,30 According to the mechanisms of costotransverse foramen block and erector spinae plane block, we planned to test for superiority if costotransverse foramen block was found to be noninferior to erector spinae plane block. The superiority efficacy of costotransverse foramen block in our study provides initial evidence that supports its use in patients undergoing video-assisted thoracic surgery. However, clinical trials directly comparing the superiority of costotransverse foramen block compared to erector spinae plane block are warranted using proper margins.
Some other techniques were attempted to be closer to the endpoint to overcome the resistance of the intertransverse tissue complex. The mid‐point transverse process to pleura block and multiple‐injection costotransverse block are two similar alternative techniques to the thoracic paravertebral block. Both injection points are within the intertransverse tissue complex and posterior to the superior costotransverse ligament. Cadaveric studies on both mid‐point transverse process to pleura block and multiple‐injection costotransverse block demonstrated a consistent spread of injectate into the paravertebral space.9,28 However, very little studies focused on the analgesic effects of the two techniques, it is therefore too early to draw any conclusion for its clinical value. One more medial method called retrolaminar block was first described in 2006.31 Several injectate pattern studies confirmed that the injectate in retrolaminar block can spread to the paravertebral space, but the spread was substantially variable, strongly volume dependent, and was more limited compared with the thoracic paravertebral block.32–34 A newly published cadaveric study indicated that there was a similarity between the costotransverse foramen block and the retrolaminar block in terms of the dye spreading into the paravertebral space. Even though, the authors emphasized that a minimal difference of injection targets performed in the paraspinal area can affect the spread pattern, and thus influencing the clinical effect.34 The clinical reports on the use of retrolaminar block are still very limited, and the results were controversial.35–37
The costotransverse foramen block is theoretically considered a superficial and safer technique, as it does not require penetration of the superior costotransverse ligament and keeps the needle tip away from critical structures such as the pleura.10 However, our results showed, for the experienced anaesthesiologists, the costotransverse foramen block was more time-consuming than the thoracic paravertebral block. The limited target area at the base of the transverse process, the steep needle trajectory, and the need for fine-tuned ultrasound guidance can make the block technically demanding. Even small movements of the ultrasound probe may shift the anatomical landmarks, increasing the difficulty of needle positioning. Therefore, even the block has clear safety advantages, we recommend that it be performed by experienced practitioners who are familiar with detailed sonoanatomy.
Other advantages like lower risks of pleural puncture, intercostal nerve and vessels injury, or dorsal ramus injury are actually not unique to the costotransverse foramen block. Any method that without direct puncture the superior costotransverse ligament will remain distant from the pleura, subcostal vessels, and ventral rami. Certainly, there could be an even lower incidence of pneumothorax because the pleural structure has moved deeper and away from the transverse process at the base of the transverse process. Unlike Shibana et al’ s observation,29 some patients in our CTFB group still complained of a mild heaviness sensation in the chest during procedure. This may be due to a fast injection leading to an opening pressure in the paravertebral space.
The costotransverse foramen block with a caudal‐to‐cranial needle trajectory and the tip of the needle in a bony area avoid the risk of accidentally entering the epidural space. However, bilateral extensive block occurred in two patients in each group of our study. In fact, even with an erector spinae plane block, a radiological imaging study and case reports have observed this uncommon but possible epidural spread.38,39 Hence, in any paraspinal blocks, a high volume and over-fast injection should be avoided, and close monitoring is needed for any sign of an extensive epidural block.
This study has some limitations. First, the sensory block was not reassessed after surgery. The injected local anesthetic needs to penetrate the costotransverse foramen indirectly into the paravertebral space, and then spread craniocaudally through the adipose tissue at the anteromedial corner of the thoracic paravertebral space.40 The diminished sensory dermatomes might not be the same before and after surgery. Second, the sample size is relatively small in our study. Finally, although cost-transverse foramen block was also confirmed as superior to erector spinae plane block in this trial, further studies with larger population directly comparing the superiority of costotransverse foramen block compared to erector spinae plane block are further warranted using proper clinically important margins.
Conclusion
In conclusion, the ultrasound-guided costotransverse foramen block is an effective alternative to thoracic paravertebral block or erector spinae plane block in patients undergoing video-assisted thoracic surgery. Future researches should compare this novel technique with other paraspinal blocks such as retrolaminar block.
Data Sharing Statement
We all agree to share all the data for this article. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Funding
This work was supported by the Beijing Municipal Science & Technology Commission, PR China (Z181100001718222).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Homma T, Doki Y, Yamamoto Y, et al. Risk factors of neuropathic pain after thoracic surgery. J Thorac Dis. 2018;10:2898–2907. doi:10.21037/jtd.2018.05.25
2. Bendixen M, Jørgensen OD, Kronborg C, Andersen C, Licht PB. Postoperative pain and quality of life after lobectomy via video-assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: a randomised controlled trial. Lancet Oncol. 2016;17:836–844.
3. Marshall K, McLaughlin K. Pain management in thoracic surgery. Thorac Surg Clin. 2020;30:339–346. doi:10.1016/j.thorsurg.2020.03.001
4. Schnabel A, Reichl SU, Kranke P, Pogatzki-Zahn EM, Zahn PK. Efficacy and safety of paravertebral blocks in breast surgery: a meta-analysis of randomized controlled trials. Br J Anaesth. 2010;105:842–852. doi:10.1093/bja/aeq265
5. Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621–627. doi:10.1097/AAP.0000000000000451
6. Taketa Y, Irisawa Y, Fujitani T. Comparison of ultrasound-guided erector spinae plane block and thoracic paravertebral block for postoperative analgesia after video-assisted thoracic surgery: a randomized controlled non-inferiority clinical trial. Reg Anesth Pain Med. 2019; 10–5.
7. Murouchi T, Yamakage M. Retrolaminar block: analgesic efficacy and safety evaluation. J Anesth. 2016;30:1003–1007. doi:10.1007/s00540-016-2230-1
8. Costache I, de Neumann L, Ramnanan CJ, et al. The mid-point transverse process to pleura (MTP) block: a new end-point for thoracic paravertebral block. Anaesthesia. 2017;72:1230–1236. doi:10.1111/anae.14004
9. Nielsen MV, Moriggl B, Hoermann R, Nielsen TD, Bendtsen TF, Børglum J. Are single-injection erector spinae plane block and multiple-injection costotransverse block equivalent to thoracic paravertebral block? Acta Anaesthesiol Scand. 2019;63:1231–1238. doi:10.1111/aas.13424
10. Shibata Y, Kampitak W, Tansatit T. The novel costotransverse foramen block technique: distribution characteristics of injectate compared with erector spinae plane block. Pain Physician. 2020;23:E305–E314.
11. Yang HM, Choi YJ, Kwon HJ, Cho TH, Kim SH, Kim SH. Comparison of injectate spread and nerve involvement between retrolaminar and erector spinae plane blocks in the thoracic region: a cadaveric study. Anaesthesia. 2018;73:1244–1250. doi:10.1111/anae.14408
12. Vidal E, Giménez H, Forero M, Fajardo M. Erector spinae plane block: a cadaver study to determine its mechanism of action. Rev Esp Anestesiol Reanim. 2018;65:514–519. doi:10.1016/j.redar.2018.07.004
13. Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c869. doi:10.1136/bmj.c869
14. Dell-Kuster S, Gomes NV, Gawria L, et al. Prospective validation of classification of intraoperative adverse events (ClassIntra): international, multicentre cohort study. BMJ. 2020;370:m2917. doi:10.1136/bmj.m2917
15. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi:10.1097/01.sla.0000133083.54934.ae
16. Rabin R, de Charro F. EQ-5D: a measure of health status from the euroqol group. Ann Med. 2001;33:337–343. doi:10.3109/07853890109002087
17. Galvagno SM. Assessing health-related quality of life with the EQ-5D: is this the best instrument to assess trauma outcomes? Air Med J. 2011;30:258–263. doi:10.1016/j.amj.2011.04.006
18. Zhang F, Zhang J, Chen J, Yu L, Wang S. Comparison of ultrasound-guided rhomboid intercostal and subserratus plane block versus thoracic paravertebral block for analgesia in thoracoscopic surgery: a randomized, controlled, non-inferiority trial. Minerva Anestesiol. 2024;90:520–529. doi:10.23736/S0375-9393.24.17927-8
19. Wang Y, Shi M, Huang S, He X, Gu X, Ma Z. Ultrasound-guided serratus anterior plane block versus paravertebral block on postoperation analgesia and safety following the video-assisted thoracic surgery: a prospective, randomized, double-blinded non-inferiority clinical trial. Asian J Surg. 2023;46:4215–4221. doi:10.1016/j.asjsur.2022.11.125
20. Luyet C, Eichenberger U, Greif R, Vogt A, Szücs Farkas Z, Moriggl B. Ultrasound-guided paravertebral puncture and placement of catheters in human cadavers: an imaging study. Br J Anaesth. 2009;102:534–539. doi:10.1093/bja/aep015
21. Oh C, Chong Y, Kang M-W, et al. Comparison between costotransverse foramen block and thoracic paravertebral block for VATS pulmonary resection: a randomized noninferiority trial. J Clin Anesth. 2023;88:111127. doi:10.1016/j.jclinane.2023.111127
22. Helander EM, Webb MP, Kendrick J, et al. PECS, serratus plane, erector spinae, and paravertebral blocks: a comprehensive review. Best Pract Res Clin Anaesthesiol. 2019;33:573–581. doi:10.1016/j.bpa.2019.07.003
23. Chin KJ. Thoracic wall blocks: from paravertebral to retrolaminar to serratus to erector spinae and back again - A review of evidence. Best Pract Res Clin Anaesthesiol. 2019;33:67–77. doi:10.1016/j.bpa.2019.02.003
24. Tsui BCH, Fonseca A, Munshey F, McFadyen G, Caruso TJ. The erector spinae plane (ESP) block: a pooled review of 242 cases. J Clin Anesth. 2019;53:29–34. doi:10.1016/j.jclinane.2018.09.036
25. Ivanusic J, Konishi Y, Barrington MJ. A cadaveric study investigating the mechanism of action of erector spinae blockade. Reg Anesth Pain Med. 2018;43:567–571. doi:10.1097/AAP.0000000000000789
26. Aponte A, Sala-Blanch X, Prats-Galino A, Masdeu J, Moreno LA, Sermeus LA. Anatomical evaluation of the extent of spread in the erector spinae plane block: a cadaveric study. Can J Anaesth. 2019;66:886–893. doi:10.1007/s12630-019-01399-4
27. Jiang H, Raso JV, Moreau MJ, Russell G, Hill DL, Bagnall KM. Quantitative morphology of the lateral ligaments of the spine. Assessment of their importance in maintaining lateral stability. Spine. 1994;19:2676–2682. doi:10.1097/00007632-199412000-00015
28. Costache I, Sinclair J, Farrash FA, et al. Does paravertebral block require access to the paravertebral space? Anaesthesia. 2016;71:858–859. doi:10.1111/anae.13527
29. Schwartzmann A, Peng P, Maciel MA, Alcarraz P, Gonzalez X, Forero M. A magnetic resonance imaging study of local anesthetic spread in patients receiving an erector spinae plane block. Can J Anaesth. 2020;67:942–948. doi:10.1007/s12630-020-01613-8
30. Dautzenberg KHW, Zegers MJ, Bleeker CP, et al. Unpredictable injectate spread of the erector spinae plane block in human cadavers. Anesth Analg. 2019;129:e163–e166.
31. Pfeiffer G, Oppitz N, Schöne S, Richter-Heine I, Höhne M, Koltermann C. Analgesia of the axilla using a paravertebral catheter in the lamina technique. Der Anaesthesist. 2006;55:423–427. doi:10.1007/s00101-005-0969-0
32. Adhikary SD, Bernard S, Lopez H, Chin KJ. Erector spinae plane block versus retrolaminar block: a magnetic resonance imaging and anatomical study. Reg Anesth Pain Med. 2018;43:756–762. doi:10.1097/AAP.0000000000000798
33. Sabouri AS, Crawford L, Bick SK, Nozari A, Anderson TA. Is a retrolaminar approach to the thoracic paravertebral space possible?: a human cadaveric study. Reg Anesth Pain Med. 2018;43:864–868. doi:10.1097/AAP.0000000000000828
34. Ohgoshi Y, Kawagoe I, Ichimura K. Real time observation of paravertebral spread during costotransverse foramen and retrolaminar blocks: a cadaveric study. J Clin Anesth. 2021;71:110260. doi:10.1016/j.jclinane.2021.110260
35. Voscopoulos C, Palaniappan D, Zeballos J, Ko H, Janfaza D, Vlassakov K. The ultrasound-guided retrolaminar block. Can J Anaesth. 2013;60:888–895. doi:10.1007/s12630-013-9983-x
36. Sugiyama T, Kataoka Y, Shindo K, et al. Retrolaminar block versus paravertebral block for pain relief after less-invasive lung surgery: a randomized, non-inferiority controlled trial. Cureus. 2021;13:e13597. doi:10.7759/cureus.13597
37. Hwang B-Y, Kim E, Kwon J-Y, et al. The analgesic efficacy of a single injection of ultrasound-guided retrolaminar paravertebral block for breast surgery: a prospective, randomized, double-blinded study. Korean J Pain. 2020;33:378–385. doi:10.3344/kjp.2020.33.4.378
38. Schwartzmann A, Peng P, Maciel MA, Forero M. Mechanism of the erector spinae plane block: insights from a magnetic resonance imaging study. Can J Anaesth. 2018;65:1165–1166. doi:10.1007/s12630-018-1187-y
39. Elkoundi A, Eloukkal Z, Bensghir M, Belyamani L. Priapism following erector spinae plane block for the treatment of a complex regional pain syndrome. Am J Emerg Med. 2019;37:796.e793–796.e794. doi:10.1016/j.ajem.2019.01.012
40. Seidel R, Wree A, Schulze M. Thoracic-paravertebral blocks: comparative anatomical study with different injection techniques and volumes. Reg Anesth Pain Med. 2020;45:102–106. doi:10.1136/rapm-2019-100896
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
The Use of a New Device-Assisted Needle Guidance versus Conventional Approach to Perform Ultrasound Guided Brachial Plexus Blockade: A Randomized Controlled Study
Vydyanathan A, Agrawal P, Shetty N, Nair S, Shilian N, Shaparin N
Local and Regional Anesthesia 2022, 15:61-69
Published Date: 25 July 2022




