Back to Journals » Journal of Multidisciplinary Healthcare » Volume 18
Cone-Beam Computed Tomography and Magnetic Resonance Imaging in Temporomandibular Joint Disorder Diagnosis: A Comparative Study
Authors Zhang M, Sang J, Yang C, Liu H, Xiao Y, Li J, Li G
Received 7 February 2025
Accepted for publication 18 June 2025
Published 30 June 2025 Volume 2025:18 Pages 3793—3802
DOI https://doi.org/10.2147/JMDH.S521279
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Pavani Rangachari
Manli Zhang, Junzhi Sang, Chunpeng Yang, Haiyan Liu, Yang Xiao, Jinfeng Li, Guangwei Li
Department of Imaging, The Second Affiliated Hospital of Qiqihar Medical College, Qiqihar, People’s Republic of China
Correspondence: Guangwei Li, Email [email protected]
Objective: This study aimed to investigate the imaging characteristics of temporomandibular joint disorder (TMD) using cone-beam computed tomography (CBCT) and magnetic resonance imaging (MRI), and to compare their diagnostic performance.
Methods: Clinical data from 53 TMD patients and 53 healthy controls were retrospectively reviewed. All participants underwent both CBCT and MRI within a two-week interval. Key measurements included condylar dimensions and joint space assessments. The study evaluated each modality’s ability to detect TMD-related abnormalities in the temporomandibular joint (TMJ) and masticatory muscles, such as joint space narrowing, bone changes, disc displacement, and muscle pathology. Statistical analysis compared diagnostic findings between the imaging techniques.
Results: Image quality was comparable between CBCT and MRI (P > 0.05). Both modalities showed no significant differences in superior and anterior joint spaces between TMD and control groups, but the posterior joint space, condylar width, and anteroposterior diameter were significantly different (P < 0.05). Across all participants, significant differences were observed between CBCT and MRI measurements for superior and anterior joint spaces (P < 0.05). Among TMD patients, 69.81% had pain disorders and 30.19% had joint disorders. Both modalities demonstrated high inter- and intra-observer consistency (P < 0.05). CBCT showed high agreement for most bony abnormalities but only moderate for disc and muscle pathology. MRI had high agreement for most findings but was moderate in detecting bone hyperplasia and sclerosis. MRI detected significantly more soft tissue abnormalities, including disc displacement and joint effusion (P < 0.05), while CBCT was more effective in identifying bone hyperplasia, sclerosis, and condylar deformation (P < 0.05).
Conclusion: Both CBCT and MRI are highly valuable tools for differentiating and assessing TMD. CBCT excels in evaluating bone-related changes, whereas MRI is superior for assessing the articular disc and soft tissue abnormalities.
Keywords: cone-beam ct, magnetic resonance imaging, temporomandibular joint disorder, imaging characteristics, comparative study
Introduction
Temporomandibular joint disorder (TMD) is a complex condition characterized by functional disorders of the temporomandibular joint and associated structures, with diverse etiologies and clinical manifestations.1 The primary symptoms of TMD include pain in the temporomandibular joint region, joint clicking, restricted mouth opening, and joint dysfunction, which, in severe cases, can significantly impair chewing, swallowing, and speech, thereby reducing the patient’s quality of life.2,3 Epidemiological studies indicate that TMD has a prevalence of approximately 10%–15% in the general population, particularly among individuals aged 20–40 years.4,5 Given that the pathogenesis of TMD involves multiple factors, including biomechanics, inflammatory responses, psychosocial influences, and genetic predispositions,6,7 its pathophysiological changes are complex and lack specific features, posing significant challenges for early diagnosis and treatment.
Imaging examinations play a crucial role in the diagnosis of TMD by providing intuitive information on the bony structures and soft tissues of the temporomandibular joint, thus aiding in determining the nature, extent, and severity of the lesions.8 Currently, cone-beam computed tomography (CBCT) and magnetic resonance imaging (MRI) are the two most commonly used imaging modalities in the diagnosis of TMD.9 However, the differences and complementarity between these two modalities in terms of imaging characteristics and diagnostic efficacy remain inadequately elucidated. Differences in imaging resolution, operational convenience, and economic cost between the two methods necessitate further investigation to clarify their respective advantages and suitable clinical scenarios.10,11 Therefore, a systematic comparison of CBCT and MRI in the imaging diagnosis of TMD is of great importance for optimizing diagnostic workflows, improving diagnostic accuracy, and formulating individualized treatment plans. Based on this premise, the present study retrospectively analyzed the imaging data of 53 TMD patients and 53 healthy controls from our hospital and evaluated the consistency and differences in detection results between the two techniques. The aim is to provide scientific evidence for the accurate diagnosis of TMD and offer clinical guidance for selecting appropriate imaging modalities.
Materials and Methods
Basic Data
The clinical data of 53 TMD patients treated in the Department of Stomatology and Rehabilitation of our hospital from July 2022 to April 2024 were retrospectively analyzed, and 53 volunteers who received oral examination during the same period were selected as controls. These control volunteers were recruited from individuals visiting the hospital for routine dental check-ups, including oral hygiene assessments and preventive care services. Recruitment was performed consecutively and non-selectively to reduce sampling bias, and individuals were invited to participate after confirming they met the inclusion and exclusion criteria. Potential participants were informed about the nature and aims of the study and were included only after providing written informed consent. To assess whether the sample size was adequate for detecting statistically significant differences, a power analysis was performed. Assuming a significance level (α) of 0.05, a power (1 − β) of 0.80, an expected mean difference (Δ) of 0.7 mm, and a pooled standard deviation (σ) of 1.0 mm, the required sample size per group was calculated. Substituting the values yielded a minimum requirement of approximately 32 participants per group. Since our study included 53 patients with TMD and 53 control subjects, the sample size was statistically sufficient to detect moderate effect sizes with adequate power.
The inclusion criteria for this study were as follows: TMD patients who met the diagnostic criteria outlined in the Diagnostic Criteria for Temporomandibular Disorders, including conditions such as disc displacement (with or without reduction), joint dysfunction, masticatory muscle pain, and osteoarthritic changes in the temporomandibular joint (eg, condylar hyperplasia, bone destruction). Subjects aged between 18 and 65 years who were able to cooperate with imaging examinations were included. All participants underwent both CBCT and MRI examinations within two weeks, ensuring high-quality images free from significant artifacts suitable for analysis. Additionally, participants had no other diagnosed joint diseases outside the temporomandibular joint, such as rheumatoid arthritis or osteoarthritis, and all signed informed consent forms, fully understanding the study’s purpose and agreeing to cooperate with the research team.
The exclusion criteria included subjects with systemic diseases affecting temporomandibular joint function, such as systemic lupus erythematosus, rheumatoid arthritis, osteoporosis, or endocrine disorders like parathyroid dysfunction. Individuals with severe craniofacial deformities, such as congenital abnormalities (eg, cleft palate, temporomandibular joint dysplasia), or a history of significant temporomandibular joint trauma or fractures were excluded. Patients who had previously undergone surgical treatments related to the temporomandibular joint (eg, arthroscopy or condylectomy) that could affect imaging features, as well as those who had received recent orthodontic treatment or dental interventions (within six months), were also excluded. Pregnant or lactating women, individuals with severe mental disorders or cognitive impairments, and those with imaging contraindications or poor-quality images unsuitable for analysis were also excluded. The study adhered to ethical principles, was approved by the Medical Ethics Committee of the Second Affiliated Hospital of Qiqihar Medical College (No. KQYX-240012), and complied with the Declaration of Helsinki and relevant domestic ethical regulations.
Methods
Image Acquisition
CBCT Examination
The temporomandibular joint of all subjects was scanned by CBCT equipment of Korea HDX WILL. During the scan, subjects were in a natural closed-mouth position, with their heads stabilized to minimize motion artifacts. Key scan parameters included: Tube voltage: 80 kV; Tube current: 8 mA; Exposure time: 17 seconds; Scan range: Entire temporomandibular joint area. During image reconstruction, standard image processing software equipped with the system was used. Specific settings were as follows: Reconstruction slice thickness: 500 μm; Slice interval: 125 μm; Image dimensions: 30 mm × 40 mm; Pixel resolution: 125 μm × 125 μm; Image grayscale: 256 levels. To facilitate observation and analysis, the CBCT data were reconstructed in multiple planes, with emphasis on coronal images to display the bony structures of the temporomandibular joint. All images were independently evaluated by two experienced radiologists to ensure data reliability and consistency.
MRI Examination
MRI scans of the temporomandibular joint were performed using a 1.5T MRI scanner (Philips, Netherlands) equipped with an 8-channel flexible head coil. Imaging was performed in both closed-mouth and maximal-open-mouth positions, with the following scan parameters: Localization scan: Fast T1-weighted axial scans to identify the specific location of the temporomandibular joint. Oblique sagittal and coronal scans: Axial oblique sagittal parameters: TE: 50 ms; TR: 2084 ms; FOV: 130×130 mm; Slice thickness: 2.5 mm; Scan time: 2 min 14s. Axial oblique coronal parameters: TE: 50 ms; TR: 1500 ms; FOV: 130×130 mm; Slice thickness: 2.5 mm; Scan time: 2 min 3 s. Sagittal imaging: High-resolution sagittal T2-weighted imaging was performed in closed-mouth and open-mouth positions to optimize soft tissue visualization: Parameters: TE: 80 ms; TR: 3088 ms; FOV: 130×130 mm; Slice thickness: 2.5 mm; Scan time: 2 min 16s. After image acquisition, specialized image processing software was used for post-processing and analysis. To avoid observational bias, imaging data were independently evaluated and recorded by two experienced radiologists.
Image Quality Control and Management of Poor-Quality Images
All acquired CBCT and MRI images were evaluated for quality using a standardized scoring system. Images that received a quality score below 4 (indicative of severe limitations and unsuitable for diagnostic interpretation) were excluded from analysis. In such cases, the patient was recalled for repeat scanning using the same imaging protocol to ensure consistency. If repeat imaging remained insufficient or if the patient declined re-examination, the subject was excluded from the final dataset. However, in this study, all 106 participants (53 TMD patients and 53 controls) had at least one diagnostically acceptable scan following quality assessment, and no cases were excluded due to poor image quality.
Image Analysis
Image Quality Analysis
Image quality was assessed using a standardized scoring system,12 independently evaluated by two maxillofacial radiologists. Pre-designed scoring sheets were used to record evaluations based on contrast, spatial resolution, signal consistency, and anatomical clarity. Scoring criteria: Score range: 0–10 points. 0–3: Severe limitations, unclear anatomical structures, unsuitable for diagnosis. 4–6: Moderate quality, discernible major structures, unclear edges, insufficient detail. 7–8: Good quality, clear anatomical structures, sharp edges, minor inconsistencies. 9–10: Excellent quality, clear structures and details, suitable for precise diagnosis. To ensure consistency, all images were scored independently by two radiologists. Discrepancies were resolved by a third-party expert, with final scores determined by consensus.
Quantitative Measurement of Condyles and Joint Spaces
To quantify the temporomandibular joint’s anatomical structures, the following parameters were measured bilaterally: Joint spaces: anterior, superior, and posterior spaces; Condyle dimensions: mediolateral and anteroposterior diameters. All measurements were performed by trained radiologists using high-precision tools. Each parameter was measured three times, and the average value was used for analysis. To minimize bias, measurement personnel were blinded to the clinical data, and standardized protocols were followed to ensure repeatability and accuracy.
Classification of TMD and Imaging Features in CBCT and MRI
TMD was classified according to the diagnostic criteria13 into two categories: Pain-related disorders: Myalgia: localized myalgia, myofascial pain, referred myofascial pain; Arthralgia; TMD-related headache. Joint disorders: Disc displacement with reduction; Disc displacement with reduction with intermittent locking; Disc displacement without reduction with limited opening; Disc displacement without reduction without limited opening; Degenerative joint disease; Subluxation. Imaging features in CBCT and MRI included narrowed joint spaces, bone destruction, sclerosis, condylar deformation, bone cystic changes, disc displacement, joint effusion, and masticatory muscle changes. All features were independently assessed by two experienced radiologists blinded to clinical backgrounds. The first radiologist repeated the analysis after one month to evaluate intra-observer consistency.
Statistical Analysis
GraphPad Prism 8 was used for charting, and SPSS 25.0 for statistical analysis. Categorical data were expressed as percentages (%), with comparisons between groups analyzed using the χ²-test. Continuous data were expressed as  , with comparisons between groups analyzed using an independent sample t-test. Consistency of imaging features between and within observers was assessed using Kappa statistics: κ < 0.40: low consistency; 0.40 ≤ κ < 0.75: moderate consistency; κ ≥ 0.75: high consistency. A value of P < 0.05 was considered statistically significant.
, with comparisons between groups analyzed using an independent sample t-test. Consistency of imaging features between and within observers was assessed using Kappa statistics: κ < 0.40: low consistency; 0.40 ≤ κ < 0.75: moderate consistency; κ ≥ 0.75: high consistency. A value of P < 0.05 was considered statistically significant.
Results
Comparison of Basic Information
The comparison of baseline data such as gender, age, and body mass index (BMI) between the two groups showed no statistically significant differences (P > 0.05), indicating comparability (Table 1).
 |
Comparison of CBCT and MRI Image Quality
CBCT and MRI images were transmitted to the system for region-of-interest delineation and image quality assessment. Based on the scoring criteria, the image quality score for CBCT was 9.23 ± 0.56, while that for MRI was 9.11 ± 0.49. The difference was not statistically significant (t = 1.660, P = 0.098) (Figure 1).
 |
Consistency Test of CBCT and MRI Imaging Features Between Observers and within Observers
For the 106 joints of 53 TMD patients, CBCT and MRI showed good inter- and intra-observer consistency in detecting lesions (P < 0.05). CBCT demonstrated moderate inter- and intra-observer consistency in detecting disc displacement and masticatory muscle lesions, while other lesions showed high consistency (P < 0.05). MRI showed moderate inter-observer consistency in detecting osteosclerosis, while other lesions showed high consistency (P < 0.05) (Table 2).
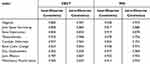 |
Table 2 Consistency Test of CBCT and MRI Imaging Features (κ Values) |
Comparison of Condylar and Joint Space Values Between CBCT and MRI
Both CBCT and MRI scans showed no statistically significant differences in the superior and anterior joint spaces between the control group and the TMD group (P > 0.05). However, significant differences were observed in the posterior joint space, condylar mediolateral diameter, and anteroposterior diameter (P < 0.05). For all participants, CBCT and MRI revealed statistically significant differences in the superior and anterior joint spaces (P < 0.05), but no significant differences were found for the posterior joint space, condylar mediolateral diameter, or anteroposterior diameter (P > 0.05) (Table 3).
 |
Table 3 Comparison of Condylar and Joint Space Values Between CBCT and MRI ( |
Comparison of Lesion Detection Between CBCT and MRI
MRI detected significantly more TMJ and masticatory muscle lesions than CBCT (P < 0.05). MRI also detected significantly more cases of disc displacement, joint effusion, and masticatory muscle edema (P < 0.05). However, CBCT detected significantly more cases of osteosclerosis and condylar deformity than MRI (P < 0.05). No significant differences were observed in detecting joint space narrowing, bone destruction, or bone cystic change between the two modalities (P > 0.05) (Table 4).
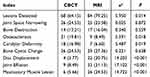 |
Table 4 Comparison of Lesion Detection Between CBCT and MRI [n (%)] |
Discussion
This study measured and analyzed the differences in the temporomandibular joint (TMJ) disc and joint space using CBCT and MRI imaging methods. The results showed that both CBCT and MRI scans demonstrated no statistically significant differences in the superior and anterior joint spaces between the control group and the TMD group. However, statistically significant differences were observed in the posterior joint space, condylar mediolateral diameter, and anteroposterior diameter (P < 0.05). This indicates that both CBCT and MRI can effectively distinguish the bony structural changes between healthy individuals and TMD patients to some extent. Furthermore, CBCT and MRI tests for all participants revealed statistically significant differences in superior and anterior joint space values, but no statistically significant differences in posterior joint space, condylar mediolateral diameter, or anteroposterior diameter. This consistency may stem from the similar foundational capabilities of the two imaging technologies in displaying bony structures.
The high spatial resolution of CBCT provides clear anatomical markers for measuring joint spaces and condylar morphology, whereas MRI, despite its relatively lower resolution for bony structures, offers high-contrast imaging of soft tissues, enabling it to infer bony changes through indirect parameters, achieving measurement accuracy comparable to CBCT. By analyzing the imaging characteristics of CBCT and MRI in TMD patients, this study found high inter-observer and intra-observer consistency for both imaging techniques, but significant differences in their ability to detect soft tissue and bony lesions. The results showed that MRI was significantly superior to CBCT in detecting soft tissue abnormalities, such as disc displacement, joint effusion, and masticatory muscle edema. On the other hand, CBCT had greater advantages in assessing bony abnormalities, such as osteosclerosis and condylar deformation. With its high resolution, low radiation dose, and fast imaging speed, CBCT can clearly display the bony structure of the TMJ, demonstrating high sensitivity in detecting osteosclerosis, hyperplasia, and condylar surface deformities.14,15 Studies have shown that CBCT not only provides precise images but also enables detailed evaluation of bony structures through accompanying measurement software, making it the preferred tool for diagnosing bony lesions.16 However, due to its limitations in soft tissue resolution, CBCT is relatively insufficient in detecting soft tissues like the articular disc and joint capsule. In contrast, MRI, characterized by its lack of radiation and high soft tissue resolution, has been widely applied in evaluating soft tissue-related abnormalities, such as disc displacement, joint effusion, and masticatory muscle disorders.10,17 Previous studies have demonstrated that MRI can clearly display the position and morphology of the articular disc, accurately determine its displacement degree and direction, and achieve high detection rates for joint effusion and masticatory muscle edema.18,19 Nevertheless, in this study, MRI images of some early-stage TMD patients did not show significant pathological features, possibly because these patients primarily exhibited functional abnormalities rather than organic lesions. For such cases, MRI may have diagnostic blind spots, suggesting that clinical diagnoses should combine patient history, physical signs, and symptoms for comprehensive assessment.20
This study compared the two imaging methods and identified their respective technical advantages and limitations. CBCT features fast scanning, simple operation, and lower cost, making it especially suitable for scenarios requiring high-resolution bony imaging.21 These attributes make CBCT a practical first-line imaging modality in clinics where rapid assessment of osseous structures is needed, such as evaluating condylar morphology, bone degeneration, or hyperplasia in suspected osteoarthritic cases. Its accessibility and efficiency also support use in general dental practices or initial consultations, especially where resources are limited.22,23
However, CBCT’s limitations include low soft tissue resolution, making it unable to clearly display pathological changes in the articular disc, joint capsule, and surrounding muscles.24 Additionally, as CBCT relies on X-ray imaging, it may pose increased radiation exposure risks during long-term follow-up.25 A further limitation of CBCT is its inadequacy in diagnosing TMD subtypes characterized by internal derangements or soft tissue inflammation. For example, CBCT cannot effectively visualize dynamic changes in disc position during mandibular movement or detect inflammatory changes in the synovial membrane or joint capsule. As a result, its utility is limited in identifying conditions such as disc displacement with or without reduction, retrodiscitis, or synovitis, which are often central to TMD subtype classification.26,27
MRI, on the other hand, is renowned for its lack of radiation and high soft tissue resolution, providing comprehensive soft tissue lesion information, particularly valuable for diagnosing disc displacement and masticatory muscle disorders.28 In clinical decision-making, this allows for more precise evaluation of soft tissue components of the temporomandibular joint complex—critical in cases presenting with pain, joint noise, or dysfunction without clear bony pathology. MRI’s ability to detect early inflammatory or internal derangement changes supports tailored, conservative management approaches before structural bone changes occur.29,30
However, MRI’s limitations include longer scanning times, higher costs, insufficient bony structure visualization, and limited applicability for certain patients, such as those with claustrophobia.31 Despite its superior capability in visualizing soft tissues, MRI may still encounter challenges in precisely distinguishing between overlapping TMD subtypes. For instance, while it can detect disc displacement, MRI may not clearly differentiate between displacement with reduction versus without reduction in cases where patient cooperation during jaw movement is suboptimal. Moreover, in chronic or degenerative cases, disc morphology may be distorted, making it difficult to determine the original pathophysiology. MRI may also lack sensitivity in detecting subtle bone marrow edema or early osteoarthritic changes compared to CBCT. These limitations can hinder accurate subclassification, which is crucial for individualized treatment planning.
A single imaging technique may have certain limitations, but combined application can address these deficiencies.32 For instance, MRI can provide accurate soft tissue lesion information for patients primarily presenting with disc displacement, while CBCT can supplement evaluations of bony structures, comprehensively revealing the pathological features of TMD. Additionally, combined imaging analysis can improve diagnostic consistency, avoiding missed or misdiagnoses associated with a single technique, and provide more comprehensive evidence for TMD classification diagnosis and precise treatment.33 However, this study did not explore the combined application of the two methods in depth due to various influencing factors.
In conclusion, we found while both imaging modalities effectively distinguished bony structural changes between healthy individuals and TMD patients, they differed in their ability to detect specific types of abnormalities. MRI was found to be superior in identifying soft tissue lesions, including disc displacement, joint effusion, and masticatory muscle edema, whereas CBCT demonstrated greater advantages in assessing bony abnormalities like osteosclerosis and condylar deformation. These findings of our study can directly inform clinical decision-making by enabling clinicians to select the most appropriate imaging modality based on the patient’s primary symptoms and suspected pathology. For instance, patients with suspected bone deformities or sclerosis may benefit from CBCT due to its superior resolution of osseous structures, while those with symptoms suggestive of disc displacement or muscle involvement may require MRI for optimal visualization. Accurate imaging assessment enhances diagnostic confidence and allows for more tailored treatment planning, such as determining the need for conservative therapy, intra-articular injections, or surgical intervention. Integrating imaging findings into clinical algorithms could also help stratify patients by severity, improving prognostication and treatment outcomes.
Limitations
Although this study provides important insights into the respective roles of CBCT and MRI in the evaluation of TMD, several limitations should be acknowledged. The sample size, comprising 53 TMD patients and 53 healthy controls, while reasonable, remains relatively limited and may restrict the generalizability of the findings; future studies with larger and more diverse populations are necessary to validate and expand upon these results. Additionally, the study did not perform detailed subgroup analyses based on specific clinical subtypes of TMD, such as distinguishing between myofascial pain and joint dysfunction variants. Conducting such analyses in future work could help clarify the imaging patterns associated with each subtype and improve diagnostic specificity. Furthermore, the study design did not incorporate dynamic imaging techniques, which are crucial for capturing the functional changes and biomechanical behavior of the temporomandibular joint over time. Including dynamic assessments—such as dynamic MRI—would enhance understanding of TMD pathophysiology and support more precise clinical evaluation. Despite these limitations, the study underscores the complementary strengths of CBCT and MRI in TMD imaging and suggests that optimal clinical application should be tailored to the lesion characteristics and specific diagnostic requirements.
Conclusion
In conclusion, both CBCT and MRI are highly valuable tools for differentiating and assessing TMD. CBCT excels in evaluating bone-related changes, whereas MRI is superior for assessing the articular disc and soft tissue abnormalities. Future research could focus on several key directions: the optimization of imaging techniques to improve CBCT’s soft tissue resolution and MRI’s ability to visualize bony structures more clearly. Additionally, emerging artificial intelligence (AI)-based image analysis tools could play a transformative role in enhancing diagnostic precision and workflow efficiency. AI technologies could enable the development of deep learning-based imaging analysis tools to automatically identify and quantify TMD-related lesions, improving diagnostic efficiency and accuracy. Furthermore, exploring multimodal imaging frameworks, including the integration of CBCT, MRI, and other imaging techniques such as ultrasound or magnetic resonance spectroscopy, could provide a more comprehensive pathological assessment of TMD. Future research should prioritize the optimization of imaging algorithms and the integration of diverse imaging modalities to pave new paths for TMD diagnosis and personalized clinical management. These efforts will contribute to more accurate diagnoses and tailored treatments, leading to improved patient outcomes in TMD care.
Funding
Qiqihar Science and Technology Plan joint guidance project LHYD-2021115.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Li C, Song ZQ, Jin X, et al. Interpretation of a clinical practice guideline on the management of chronic pain associated with temporomandibular joint disorders. Chin J Stomatol. 2024;59(10):988–997. doi:10.3760/cma.j.cn112144-20231229-00313
2. Zhang Z, Wang CC, Song LX, et al. Analysis of the clinical manifestations of 3 425 patients with orofacial pain of temporomandibular disorders. Chin J Stomatol. 2021;56(12):1244–1252. doi:10.3760/cma.j.cn112144-20210415-00178
3. Jiang T. Masticatory muscle disorders and treatment from the perspective of prosthodontics. Chin J Stomatol. 2022;57(7):682–687. doi:10.3760/cma.j.cn112144-20220408-00163
4. Hu M, Yang C, Liu HH, et al. Consensus of experts on standard items of the cohort construction and quality control of temporomandibular joint diseases. Chin J Stomatol. 2024;59(10):977–987. doi:10.3760/cma.j.cn112144-20240725-00293
5. Farhani I, Yamchi A, Madanchi H, et al. Designing a Multi-epitope Vaccine against the SARS-CoV-2 Variant based on an Immunoinformatics Approach. Curr Computer Aided Drug Design. 2024;20(3):274–290. doi:10.2174/1573409919666230612125440
6. Jiang T. Relationship between temporomandibular disorders and malocclusions: from history to present. Chin J Stomatol. 2021;56(8):734–739.
7. Luo D, Wei XX, Zhou Y, et al. Research progress in psychological factors in the diagnosis and treatment of temporomandibular joint disorders. Chin J Stomatol. 2020;55(10):794–798. doi:10.3760/cma.j.cn112144-20200307-00132
8. Naaz S, Vasu DSS, Neha DA, et al. Diagnostic imaging of temporomandibular joint-a review. Saudi J Oral Dentl Res. 2024;9(7):151–159. doi:10.36348/sjodr.2024.v09i07.004
9. Fu K, Hu M, Yu Q, et al. Experts consensus on cone-beam CT examination specification and diagnostic criteria of temporomandibular disorders. Chin J Stomatol. 2020;55(9):613–616. doi:10.3760/cma.j.cn112144-20200514-00267
10. Cheng X-G, Tian C, Hu R, et al. Evaluation of the relationship between the attachment type of lateral pterygoid muscle and the position of temporomandibular joint disc in patients with temporomandibular joint disorders based on wireless amplified MRI detector high resolution imaging. Chin J Stomatol. 2023;58(6):569–574. doi:10.3760/cma.j.cn112144-20230418-00161
11. Whyte A, Boeddinghaus R, Bartley A, et al. Imaging of the temporomandibular joint. Clin Radiol. 2021;76(1):
12. Wei Y, Wang XP, Zha KJ, et al. The application value of multi-material artifact reduction technique in maxillofacial CT images of patients with metallic dental implants. Zhonghua yi xue za zhi. 2021;101(12):841–845. doi:10.3760/cma.j.cn112137-20210110-00069
13. Wu L, Li HM, Chen ZZ, et al. Clinical investigation and research on Axis II evaluation of patients with temporomandibular disorders. Chin J Stomatol. 2022;57(1):76–84. doi:10.3760/cma.j.cn112144-20210604-00282
14. Lyu Y-S, Li Z-H. Cone beam CT imaging findings in patients with temporomandibular joint disorder syndrome and unilateral chewing. Shanghai J Stomatol. 2022;31(6):653.
15. Hilgenberg-Sydney PB, Zanlorenzi FF, Cunha CO. Comparative analysis of temporomandibular joint morphology in degenerative joint disease: a cone-beam CT study in patients with and without arthralgia. Saudi Dent J. 2024;36(5):756–760. doi:10.1016/j.sdentj.2024.03.005
16. Dumbuya A, Gomes AF, Marchini L, et al. Bone changes in the temporomandibular joints of older adults: a cone‐beam computed tomography study. Special Care Dentistry. 2020;40(1):84–89. doi:10.1111/scd.12441
17. Zhang Z, Yang JY, Xing YM, et al. MRI evaluation of condylar bone regeneration after temporomandibular joint disc reduction and suture and analysis of factors affecting bone regeneration. Chin J Stomatol. 2023;58(10):1004–1009. doi:10.3760/cma.j.cn112144-20230817-00090
18. Shipika D, Ostashko AA, Burenchev DV, et al. Clinical example of complex diagnostic and treatment of patient with temporomandibular joint internal derangements with arthroscopic surgery. Stomatologiia. 2021;100(4):109–116. doi:10.17116/stomat2021100041109
19. Jeon KJ, Lee C, Choi YJ, et al. Analysis of three-dimensional imaging findings and clinical symptoms in patients with temporomandibular joint disorders. Quant Imag Med Surg. 2021;11(5):1921. doi:10.21037/qims-20-857
20. Wu X, Zheng Y, He C, et al. Application of Machine Learning in the Diagnosis of Temporomandibular Disorders: an Overview. Oral Dis. 2025. doi:10.1111/odi.15300
21. Kijak E, Szczepek AJ, Margielewicz J. Association between anatomical features of petrotympanic fissure and tinnitus in patients with temporomandibular joint disorder using CBCT imaging: an exploratory study. Pain Res Manag. 2020;2020(1):1202751. doi:10.1155/2020/1202751
22. Doan MK, Long JR, Verhey E, et al. Cone-Beam CT of the Extremities in Clinical Practice. Radiographics. 2024;44(3):e230143. doi:10.1148/rg.230143
23. Chen W, Zhang Y, Wang X, et al. Comparative Analysis of Imaging Modalities for Diagnosing Musculoskeletal Disorders. J Innov Med Res. 2024;3(1):45–53. doi:10.56397/JIMR/2024.03.06
24. Costa J, Mendes JM, Salazar F, et al. Analysis of peri-implant bone defects by using cone beam computed tomography (CBCT): an integrative review. Oral Radiol. 2023;39(3):455–466. doi:10.1007/s11282-023-00683-w
25. Ming X, Cheng X, Tian C, et al. Evaluation of condylar osseous changes using a wireless detector with proton density–weighted imaging sequences. Quant Imagi Med Surg. 2023;13(1):17. doi:10.21037/qims-22-424
26. Gaur A, Dhillon DM, Puri DN, et al. Questionable accuracy of CBCT in determining bone density: a comparative CBCT–CT in vitro study. Dental Med Probl. 2022;59(3):413–419. doi:10.17219/dmp/143504
27. Alshomrani F. Cone-Beam Computed Tomography (CBCT)-based diagnosis of dental bone defects. Diagnostics. 2024;14(13):1404. doi:10.3390/diagnostics14131404
28. Tresoldi M, Dias R, Bracci A, et al. Magnetic Resonance Imaging Evaluation of Closed‐Mouth TMJ Disc‐Condyle Relationship in a Population of Patients Seeking for Temporomandibular Disorders Advice. Pain Res Manag. 2021;2021(1):5565747. doi:10.1155/2021/5565747
29. Kijowski R, Fritz J. Emerging technology in musculoskeletal MRI and CT. Radiology. 2023;306(1):6–19. doi:10.1148/radiol.220634
30. Sneag DB, Abel F, Potter HG, et al. MRI advancements in musculoskeletal clinical and research practice. Radiology. 2023;308(2):e230531. doi:10.1148/radiol.230531
31. Vosshenrich J, Koerzdoerfer G, Fritz J. Modern acceleration in musculoskeletal MRI: applications, implications, and challenges. Skeletal Radiol. 2024;53(9):1799–1813. doi:10.1007/s00256-024-04634-2
32. Gao S, Tian H, Yu JJ, et al. Evaluation of CT angiography vascular localization combined with refined three-dimensional printing in guiding the resection and reconstruction of complex oral cancer. Chin J Oncol. 2019;41(7):496–500. doi:10.3760/cma.j.issn.0253-3766.2019.07.003
33. Li Y-Q, Wang H-J, Zhu B-Q, et al. Diagnostic value of 3D fast spin-echo sequence scanning combined with multislice spiral CT in knee cruciate ligament injury. China J Orthopaed Traumatol. 2024;37(2):153–158. doi:10.12200/j.issn.1003-0034.20220331
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Retrospective Study on the Comparative Efficacy of Intra-Articular Injection and Photodynamic Therapy in the Treatment of TMD
Wei X, Gao J, Tian Z, Zhao F, Wang H, Yan W
Therapeutics and Clinical Risk Management 2025, 21:415-424
Published Date: 27 March 2025





