Back to Journals » Journal of Pain Research » Volume 18
Consensus Guidelines from the American Society of Pain and Neuroscience for the Use of 60-Day Peripheral Nerve Stimulation Therapy. A NEURON Living Guideline Project
Authors Gill B , Tidwell C , Hagedorn JM , Moreira AM , Lawandy M , Boyett B , Schappell J, Latif U , Pritzlaff S , Skaribas I, Kalia H , Sheth S, Schnur M, Li S , Lester D, Ellico T, Naidu R , Russo D, Massey C , Ottestad E, Vorenkamp K, Vucetic H, Pingree MJ, Abejón D, Desai MJ , Dickerson D , Gulati A, Sayed D , Deer TR
Received 5 March 2025
Accepted for publication 5 June 2025
Published 24 June 2025 Volume 2025:18 Pages 3117—3139
DOI https://doi.org/10.2147/JPR.S521788
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Alaa Abd-Elsayed
Benjamin Gill,1 Cody Tidwell,2 Jonathan M Hagedorn,3 Alexandra M Moreira,4 Marco Lawandy,5 Benjamin Boyett,6 Justin Schappell,7 Usman Latif,8 Scott Pritzlaff,9 Ioannis Skaribas,10 Hemant Kalia,11 Samir Sheth,12 Maricela Schnur,13 Sean Li,14 Denise Lester,15,16 Trevor Ellico,17 Ramana Naidu,18 David Russo,19 Christopher Massey,20 Einar Ottestad,21 Kevin Vorenkamp,22 Henry Vucetic,23 Matthew J Pingree,3 David Abejón,24 Mehul J Desai,25 David Dickerson,26,27 Amitabh Gulati,28 Dawood Sayed,8 Timothy R Deer29
1Omaha Pain Physicians, Omaha, NE, USA; 2Department of Anesthesiology and Pain Medicine, University of Minnesota, Minneapolis, MN, USA; 3Department of Anesthesiology and Perioperative Medicine, Division of Pain Medicine, Mayo Clinic, Rochester, MN, USA; 4Department of Anesthesiology and Pain Medicine, Rush University, Chicago, IL, USA; 5Department of Physical Medicine and Rehabilitation, Montefiore Medical Center, Bronx, NY, USA; 6Department of Physical Medicine and Rehabilitation, University of Missouri, Columbia, MO, USA; 7Department of Pain Medicine, Mayo Clinic Health System, Eau Claire, WI, USA; 8Department of Anesthesiology and Pain Medicine, The University of Kansas Health System, Kansas City, KS, USA; 9Department of Anesthesiology and Pain Medicine, University of California–Davis, Sacramento, CA, USA; 10Expert Pain, Houston, TX, USA; 11Center for Research & Innovation in Spine & Pain, Rochester, NY, USA; 12Sutter Health Systems, Roseville, CA, USA; 13Department of Pain Medicine, Guthrie Clinic, Ithaca, NY, USA; 14National Spine and Pain Centers, Shrewsbury, NJ, USA; 15Department of Physical Medicine and Rehabilitation, Virginia Commonwealth University, Richmond, VA, USA; 16Department of Physical Medicine and Rehabilitation, Richmond VA Medical Center, Richmond, VA, USA; 17Department of Anesthesiology, University of Utah, Salt Lake City, UT, USA; 18MarinHealth Spine Institute, UCSF Affiliate, Larkspur, CA, USA; 19Columbia Pain Management, Hood River, OR, USA; 20Pain Specialists of America, Austin, TX, USA; 21Department of Anesthesiology, Perioperative and Pain Medicine, Stanford University School of Medicine, Stanford, CA, USA; 22Duke University Department of Anesthesiology, Durham, NC, USA; 23University Hospitals Department of Anesthesiology and Perioperative Medicine, Cleveland, OH, USA; 24Unidad de Dolor, Hospital Universitario Quironsalud Madrid, Madrid, Spain; 25International Spine, Pain & Performance Center, Washington, DC, USA; 26Department of Anesthesiology, Critical Care & Pain Medicine, Endeavor Health, Evanston, IL, USA; 27Department of Anesthesia & Critical Care, University of Chicago Pritzker School of Medicine, Chicago, IL, USA; 28Department of Anesthesiology, Memorial Sloan Kettering Cancer Center, New York, NY, USA; 29The Spine and Nerve Center of the Virginias, Charleston, WV, USA
Correspondence: Benjamin Gill, Email [email protected]
Abstract: Peripheral nerve stimulation (PNS) has evolved with various applications and durations of therapy. In recent years, extensive data has been developed on a 60-day treatment using a novel approach. Confusion exists on the use of a trial therapy, a permanent implant, and a 60-day duration treatment. The American Society of Pain and Neuroscience (ASPN) seeks to clarify the literature associated with this neuromodulation approach. A diverse group of experts was nominated to provide opinions and guidance based on evidence-graded assessment and clinical knowledge. This guidance is the first to specifically assess the clinical use of 60-day PNS and best medical practice.
Keywords: peripheral nerve stimulation, pain medicine, best practices, clinical guidelines
Objective
The ASPN 60-day PNS guideline was developed to provide clinicians with the most comprehensive review of PNS evidence, efficacy, and safety. This document will assist clinicians in patient selection and appropriate application of PNS for multiple pathologies throughout various anatomic sites.
History of PNS
Therapeutic electrical stimulation was proposed by Wall and Melzack in 1965 with the introduction of the gate control theory of pain perception.1 This led to the development of neuromodulation, the dosing of electric current by implanted electrode leads to treat pain and neurologic dysfunction. One of the earliest reports on neuromodulation was published in 1967 and involved PNS, which is defined as applying electrical stimulation directly to a named nerve. In this study, Wall and Sweet applied this theory, experimentally developed in cats and tested on their own infraorbital nerves. They reported an eight-patient case series involving neuropathic pain from a variety of etiologies. They found that two-minute electrical stimulation produced pleasant paresthesia and decreased pain, but yielded only temporary benefit.2 Despite this early application, however, the growth of PNS was limited for several decades due to impracticalities of early PNS because of the requirement for surgical dissection to the affected nerve and associated complications, including direct nerve trauma, fibrosis of surrounding tissues, lead migration, and frequent need for hardware revisions.3,4
In 1967, Shealy and Mortimer described their analgesic results with dorsal column spinal cord stimulation (SCS) using a modified electrical stimulator initially designed to stimulate the carotid sinus to treat hypertension and angina.5 Due to its success, the device was made commercially available the following year, and dorsal column stimulation became the most popular modality of electrical neuromodulation for several decades. Developing reports of improvement in symptoms of torticollis,6 spasticity in multiple sclerosis,7 increased blood flow8 and thereby decreasing painful peripheral vascular disease9 and angina10 further pushed research focus away from PNS in favor of SCS. Over that time, significant advances were made in SCS system technology, but PNS remained static with little innovation.
In 1999, however, Weiner and Reed brought attention back to PNS with a case series of 13 patients suffering from occipital neuralgia. Each patient underwent a diagnostic peripheral nerve block, a five to seven-day temporary lead trial, followed by percutaneous lead and subcutaneous implantable pulse generator (IPG) implantation. At follow-ups between one and six years, 66% of patients described >75% pain relief, and 33% described 50% relief.11 In more recent years, there has been an explosion of interest in stimulating the C- and A-delta fibers in the periphery, especially as imaging modalities (eg, ultrasound) have improved targeting of nerves and the technology has supported less invasive means of treatment to improve PNS treatment efficacy, durability, and safety.
History of Trial, 60-Day Temporary, and Permanent Implant
With renewed interest in PNS, new techniques developed with advancing technology to address previous shortcomings. Ultrasound-guided PNS was described by Huntoon et al,12–14 a technique that allows for a percutaneous and minimally invasive approach to lead placement to obviate the need for a surgical cut-down. Lead advancement has also improved significantly in recent years. Historically, PNS was offered through cylindrical leads that were designed for SCS. In the PNS application, they were large and had a high migration rate (9–25%), prohibiting implantation across joints and with increased risk of infection (3.6–17.9%).15 Patients often went to a temporary trial with percutaneous lead placement and connection to an external generator as is customary for SCS. More recently, a new proprietary lead design [SPRINT® PNS System, SPR® Therapeutics, Cleveland, Ohio, USA] was developed using a helically coiled monopolar lead (versus solid and cylindrical). This coiled design encourages fibrotic ingrowth around the lead, significantly decreasing migration and infection rates (up to 25-fold reduction).16–18 United States Food and Drug Administration (FDA)-cleared for up to 60 days of use, this system allows for extended periods of stimulation, which can act as a definitive course of treatment and possibly decrease the need for permanent systems.
The exact mechanism by which electrical stimulation of peripheral nerves provides analgesia has not fully been elucidated. Still, there has been considerable progress in our understanding since the initial gate control theory. Chronic inflammation of peripheral nerves leads to hyperexcitability and an increased rate of depolarization, a phenomenon known as peripheral sensitization. These nerves repeatedly fire an abnormal afferent signal to the wide dynamic range neurons in the dorsal column of the spinal cord. The overstimulation of wide dynamic range neurons leads to multiple changes in the spinal cord and brain, leading to central sensitization of pain. At the spinal cord, activation of glial cells increases inflammation and hyperexcitability of nociceptive pathways. In addition, glycinergic and gamma-aminobutyric acid (GABA)-ergic inhibitory neuronal activity decreases, thereby increasing abnormal afferent nociceptive signaling to the brain. A similar process then affects the supraspinal nociceptive circuits, ultimately resulting in neuroplastic changes in the somatosensory cortex. It is theorized that even short-term, 60-day modulation of this process, beginning at the peripheral nerve, should allow lasting reversal of maladaptive neurologic changes.19
Emerging literature has shown the efficacy and safety of percutaneous electrical stimulation involving chronic back pain,20–23 shoulder pain,24–29 knee pain,30,31 post-amputation pain,32–34 and neuropathic pain of various etiologies35–40 in small case studies and series. Several randomized controlled trials have shown durable therapeutic benefits even after lead removal. This combination of better mechanistic understanding, low infection rate, and prolonged post-removal analgesic efficacy discourages the traditional practice of trialing before implantation of 60-day PNS devices.34,41–43
Methods
The ASPN identified an educational need for a comprehensive clinical guideline to provide evidence-based recommendations. A multidisciplinary group of experts from the fields of physiatry, anesthesiology, and neurosurgery developed this guideline based on current publications. Literature in English was searched using Medline, EMBASE, Cochrane CENTRAL, BioMed Central, Web of Science, Google Scholar, PubMed, Current Contents Connect, meeting abstracts, and Scopus to identify and compile the evidence for 60-day applications of PNS. The identified peer-reviewed literature was critiqued using the United States Preventive Services Task Force (USPSTF) criteria (see Tables 1 and 2), and consensus points were drafted. Recommendations were then developed via consensus for specific applications of this treatment approach. These methods are in alignment with those of other ASPN guidelines.44
 |
Table 1 Quality of Evidence Ranking Using the United States Preventative Services Task Force Criteria Modified for Therapy |
 |
Table 2 Levels of Certainty Regarding Net Benefit |
Data Overview
Many neurostimulation systems for pain relief, such as those applied to the spinal dorsal columns, typically involve a brief (eg, 3–14-day) trial to assess presumed effectiveness before permanent system implantation. Patients who report ≥50% pain relief and functional improvement usually proceed to permanent implantation.45,46 Recent reviews of dorsal column SCS systems have found that lack or loss of efficacy was the primary cause of up to 38–67% of system explants, with patients undergoing explant in the first three years incurring significantly higher healthcare costs.45,47–54 Real-world trial to permanent conversion rates have been reported to be 41–65%.46,55 These low trial conversion rates and high rates of explant suggest that improved patient identification strategies are needed to better distinguish likely responders and non-responders to neurostimulation before deciding to implant a permanent system.43
The duration of conventional neurostimulation trials, as a mode of identification of presumed responders and non-responders to neurostimulation, has historically been limited to seven to 10 days due to the risk of infection associated with conventional cylindrical percutaneous leads exiting the skin interface.17,56–58 Theoretically, a longer trial may lead to an improved patient assessment of the therapy. A recent review found that fine-wire, coiled leads have an estimated 60-day infection rate of 0.1% and a 25-fold lower infection risk than conventional cylindrical leads.32 This is similar to the infection rate in published clinical trials using temporary percutaneous leads (one superficial infection at a lead exit site across 601 implanted leads, 0.17%).43,59 The most commonly reported adverse event has been adhesive-related skin irritation.58
In one study comparing responder rates (meaning the proportion of patients achieving >50% pain relief), it was found that the split between those who responded to therapy within the first 14 days of treatment and those who responded after the initial 14-day period were equivalent at 30% and 31%, respectively, when averaged across various indications for treatment (see Figure 1).43 These data could mean that approximately half of the patients who may benefit from permanent PNS system implantation would not be identified during the classic 7–10 trial period and be identified inappropriately as non-responders. Data also indicated that a smaller proportion of patients, ~7%, were identified as non-responders with more than 14 days of treatment when they had seen success with fewer than 14 days of stimulation.43 This indicates that this group would be similarly inappropriately identified with a traditional trial; however, they would have been categorized as responders when their response was not durable. This could lead to a patient who may benefit from permanent PNS implantation not getting offered that option and those who are unlikely to benefit from permanent implantation undergoing unnecessary surgery with the associated risks and costs.
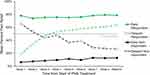 |
Figure 1 Responder Rates from Initiation of PNS Treatment. Reprinted with permission from Dove Medical Press. Naidu R, Li S, Desai MJ, Sheth S, Crosby ND, Boggs JW. 60-Day PNS Treatment May Improve Identification of Delayed Responders and Delayed Non-Responders to Neurostimulation for Pain Relief. Journal of Pain Research. 2022;15:733–743.43 |
The following sections detail the evidence regarding the use of 60-day PNS treatment. Based on a review of this data, the ASPN working group developed summary consensus guidelines (see Table 3).
 |
Table 3 Summary of Consensus Opinions Regarding Use of 60-Day PNS |
Rationale for 60-Day PNS in the Management of Chronic Back Pain
Chronic low back pain (LBP) is defined as persistent pain in the lower back lasting longer than three months. It is a major global health issue, leading to significant disability and reduced quality of life (QOL). Chronic LBP affects a substantial portion of the population, contributing to high healthcare costs and lost productivity.60 The complex interplay of physical, psychological, and social factors complicates its management. Addressing chronic LBP effectively is essential for improving patient outcomes and alleviating the burden on healthcare systems.61
Chronic LBP can arise from various etiological factors, with different interventional pain management treatment options depending on the etiology. These include myofascial pain, discogenic pain, facet-mediated pain, chronic vertebral endplate inflammation, disc herniation, and spinal stenosis without radiculopathy, as well as sacroiliac joint pain. Other less common causes are osteoporotic fractures, metastatic or primary neoplasms, infections, rheumatologic conditions such as ankylosing spondylitis, and vascular or intraabdominal conditions with referred LBP.62 One of the most common etiologies for chronic LBP is degenerative disease of the lumbar spine, specifically lumbar facet joint disease.
Chronic LBP due to lumbar facet joint disease has been treated with radiofrequency ablation (RFA) rhizotomies of the medial branches of the dorsal rami. Lumbar RFA for facetogenic LBP is generally successful; however, there is variability in outcomes, and it remains a “de facto” neuro-destructive procedure.63,64
Recently, interventional techniques for chronic LBP treatment have involved electrical modulation of the lumbar medial branch nerves.20,65 Evidence suggests that PNS of the lumbar medial branch nerves may be effective in improving pain and function in patients with chronic axial LBP, and both short and long-term follow-ups demonstrate good safety profiles.4,21,66–68 The proposed mechanism of action is primarily the modulation of the afferent pain signal and the disruption of central sensitization of pain. Secondarily, stimulation of efferent nerve signals to activate low back muscles, especially the multifidus muscle, has been implicated in the restorative action of the therapy.19 The rationale behind a 60-day trial of PNS for managing chronic lower back pain is complex and involves several factors:
- Anatomical Landmarks: The anatomical landmarks for the placement of the PNS 60-day electrode are readily identified with fluoroscopy or ultrasound guidance (medial and inferior to the facet joint).
- Preservation of Anatomy: The therapy does not involve a neuro-destructive procedure and preserves the anatomical integrity of the corresponding medial branches.
- Extended Evaluation Period: The 60-day duration allows for a comprehensive assessment of pain relief and functionality, offering a better understanding of the treatment’s long-term potential than traditional shorter trials.23
- Reduced Risk of Placebo Effects: A longer trial period reduces the likelihood of placebo effects that are more pronounced in shorter studies, providing more reliable data on the effectiveness of the treatment.
- Sustained Improvement: Evidence suggests that even up to five months following treatment and removal of the temporary 60-day trial system, 93% of patients reported sustained and clinically meaningful improvements.23,59
- Minimized Surgical Risks: The 60-day trial system does not involve permanent implants, thus reducing or even eliminating complications associated with surgical procedures, such as infection, hardware failure, and the need for additional surgeries.
- Minimized Anesthesia Risks: Because the 60-day trial system does not involve surgical procedures, anesthesia is not required, which reduces associated risks.
- Establish an Alternative to Opioid Treatment: The use of 60-day PNS presents a viable non-pharmacological option for treating chronic back pain and offers several advantages over traditional opioid pain management strategies, particularly in avoiding the harmful long-term effects associated with opioid use.69
- Less Invasive Hardware: The smaller, less invasive introducer and electrode reduce tissue trauma, minimize post-procedural pain, and enhance overall patient comfort and satisfaction.
- Flexible Treatment Pathway: If effective, the temporary trial can lead to consideration for a permanent spinal implant if clinically appropriate, offering patients a potential continuum of care based on their responses and individual clinical needs.43
- Prevention of Chronic Back Pain: A 60-day trial of PNS may serve as a preventive measure and can be employed preemptively as a prophylactic approach to reduce the risk of developing chronic back pain after surgery.30,70
- Objective Measurement of Outcomes: The structured data collection over 60 days allows for more robust statistical analysis and comparison with prior treatment modalities, aiding clinicians in making informed decisions.43
Rationale for 60-Day PNS Versus Shoulder Surgery
When conservative treatments fail, total shoulder arthroplasty (TSA) or reverse TSA is often the next step in the shoulder osteoarthritis treatment algorithm. Both techniques have been shown to improve pain, range of motion, and QOL in patients with glenohumeral osteoarthritis.71,72
Reverse TSA can also be performed in patients with severe rotator cuff injury. While both approaches are safe and cost-effective compared to non-surgical treatment, arthroscopic rotator cuff repair is more cost-effective and has better clinical outcomes than reverse TSA for massive rotator cuff tears.73,74 However, treatment of massive rotator cuff tears is complex and challenging, and data regarding outcomes is mixed.75 A 2020 meta-analysis by Narvani et al showed statistically significant improvement in pain, range of motion, and QOL in patients with degenerative tears.76 However, a Cochrane review by Karjalainen et al concluded that surgical rotator cuff repair may provide little or no clinically important benefits with respect to pain, function, overall QOL or participant‐rated global assessment of treatment success when compared with non‐operative treatment. 77 Additionally, Longo et al found no statistically significant difference in pain or function after two years.78
Delaying surgical treatment in patients with a rotator cuff tear can lead to a decreased healing rate and higher failure rates. Specifically, there was less likelihood of healing following arthroscopic rotator cuff repair in patients with multiple tendon tears, tears greater than 2.2 centimeters, and muscle retraction greater than 2.0 centimeters.79 These prognostic factors may be increased by delaying surgery since rotator cuff tears can enlarge over time, in addition to the muscle retraction, muscle atrophy, and fatty infiltration that occurs with time from injury.80 Delaying surgery for periods as short as three months post-injury has been shown to increase failure rates following rotator cuff repair, while other publications have suggested these shorter periods do not impact outcomes, but over 12 months will lead to higher retear rates.81–83
Fortunately, there is no high-quality evidence that delayed surgical treatment of advanced glenohumeral arthritis leads to worse outcomes. Intuition suggests that delayed TSA may place the patient at higher risk for the need for a reverse TSA due to rotator cuff degeneration with age and time, but this has not been proven. Regardless, patients over the age of 70 do well with either TSA or reverse TSA.77
PNS for shoulder pain secondary to musculoskeletal etiologies is considered safe, although the efficacy data is still emerging. In 2020, Mansfield et al published their case series of eight patients who underwent axillary nerve PNS for shoulder pain. Seven out of those eight patients reported more than 50% pain reduction, and 100% of them decreased their opioid utilization and recommended the treatment to other patients in the long run.84
Chitneni et al reported their experience with suprascapular nerve stimulation for chronic shoulder pain secondary to rotator cuff pathology using a 60-day temporarily implanted device and concluded that this therapy is safe, minimally invasive, and completely reversible.85
When considering PNS for certain shoulder pathologies, the patient should be given a thorough explanation of the plan of care and potential consequences.
Rationale for 60-Day PNS for Neuropathic Pain
Neuropathic pain presents a wide range of prevalence mainly due to lack of consistency in its definition, but it is estimated to comprise ~3-18% of the population.86 Pharmacologic treatments for neuropathic pain have been suboptimal, thereby emphasizing the need for evidence-based non-pharmacological treatment for neuropathic pain.87
Multiple studies are using PNS for neuropathic pain and non-neuropathic pain. Multiple studies have examined the use of permanent PNS for chronic neuropathic pain.13,68,88 However, a novel therapy uses a 60-day implant that can provide long-term therapy. Studies using the 60-day PNS system report variable efficacy rates beyond 60 days. For example, in a case series by Pagan-Rosado, the short-term treatment achieved significant pain relief during the 60-day implant phase but was not sustained in the three-patient case series.89 However, other studies employing the 60-day PNS therapy have been promising. For example, in a three-patient case series of complex regional pain syndrome patients, all patients received long-lasting pain relief lasting at least 10 months, and only one patient elected to have a permanent PNS placed.90 Additional prospective studies demonstrated efficacy at variable endpoints. Rauck et al implanted post-amputation patients for two weeks and followed up at four weeks. The majority of the patients in the study had significant pain relief and decreased analgesic use.32
In a randomized, prospective, double-blind study, Gilmore et al used 60-day PNS therapy in patients with chronic neuropathic post-amputation pain. The comparison of pain improvement at eight weeks was 58% in the PNS group to 14% in the placebo group. At 12 months, 67% of patients had >50% pain relief in the PNS group, whereas no patients in the placebo group had >50% pain relief.34 Certainly, the focus of PNS is on chronic neuropathic pain. However, a recent feasibility study examined the use of PNS in acute pain settings for amputation pain. Albright-Trainer et al performed a prospective randomized controlled single-arm study comparing PNS five days after lower extremity amputation versus standard medical treatment.91 PNS was superior in all metrics vs standard medical treatment. Notably, in addition to the reduction in the pain scores, 20% of patients were taking opioids at three months, whereas 50% of the patients in the standard medical therapy (SMT) group were still taking medications. While more research is undoubtedly needed, the current prospective data for PNS in neuropathic pain is promising.
60-Day PNS in the Treatment of Specific Pathologic States
60-day PNS treatment is appropriate after failure of prior treatments for the indications below, given that the expected benefits are more likely than not to be more beneficial than any other available standard treatments.
Inoperable Shoulder Pain (or Patient Resistant to Surgery)
Standard operative shoulder conditions include rotator cuff tears and glenohumeral arthritis. The recommended non-operative treatments for these conditions from the American Academy of Orthopaedic Surgeons (AAOS) Evidence-Based Practice Guidelines include physical therapy and corticosteroid injections with local anesthetic based on moderate and strong evidence in rotator cuff tears and consensus only in glenohumeral arthritis.71,92 Physical therapy has been shown to improve pain and range of motion, but long-term studies are limited.93,94 Additionally, multiple meta-analyses show no significant, sustained pain improvement nor change in disease progression with non-steroidal anti-inflammatory drugs (NSAIDs).95–97 As expected, the next recommended treatment from the AAOS is surgery. However, some patients may not be appropriate surgical candidates due to medical comorbidities, or they may wish to postpone surgery. Early evidence has shown that PNS is effective for treating shoulder pain. It can provide bridge therapy until patients get definitive surgery and/or in those cases where surgery would be contraindicated.
The evidence for PNS and rotator cuff tear pain is limited. In 2022, Chitneni et al reported two cases of suprascapular and axillary nerve 60-day PNS for treating rotator cuff tear pain. Both patients had been experiencing pain for more than one year. At three months post-PNS treatment, the patients were reporting 90% and 80% pain relief with a reduction in opioid usage, respectively.85 Similarly, Wilson et al described using PNS for patients with refractory pain from subacromial impingement of the rotator cuff. Adults with chronic shoulder pain for over six months and a diagnosis of subacromial impingement were recruited for the study. Ten patients were treated with three weeks of axillary nerve PNS and were followed for 12 weeks after PNS discontinuation. The ten subjects had an average overall reduction in pain of 36.6% at three weeks and 48.8% at 16 weeks compared to baseline. The subjects also showed improvements in disability and shoulder abduction range of motion.29 While this is not specifically 60-day PNS, the authors used the same 60-day PNS device, and the results suggest that PNS is a viable treatment for rotator cuff pathologies.
The only reported evidence for 60-day PNS and shoulder osteoarthritis is a case report. Mansfield and Desai reported on a 91-year-old male with primary shoulder osteoarthritis. He underwent a 60-day PNS of the axillary nerve and reported 70% pain reduction during the 60 days. Within several weeks of the PNS lead pull, the patient had returned to his baseline pain. He underwent implantation of a permanent PNS device and was reporting greater than 70% pain reduction at eight months.84 The same authors published a retrospective case series reporting their experience with axillary PNS for chronic shoulder pain. The subjects were a mixed population of shoulder pain pathologies, including rotator cuff pathology, glenohumeral joint arthritis, acromioclavicular joint arthritis, adhesive capsulitis, and biceps tendinopathy. In total, eight subjects were involved in the case series. All patients underwent a permanent PNS implantation. The authors did not report the outcomes for the specific pathologies. The average time of follow-up was 445 days post-implant. The eight subjects had an average pain reduction of 66.7%. Seven out of eight subjects had greater than 50% pain reduction. Five out of eight subjects were using opioid medications for pain management at the time of PNS implantation, and all of them had a decrease in their opioid usage.98
Most recently, a pragmatic study included over 700 patients using 60-day PNS for various types of shoulder etiology. This study demonstrated durable results beyond the 60-day period.99 It underscored the importance of temporary implants for patients, especially in those patients who are unable to tolerate anesthesia for permanent implantation of PNS systems or in patients who do not want a permanent PNS system.
In conclusion, the literature surrounding the use of 60-day PNS for treating inoperable shoulder pain is limited. Because 60-day PNS is a temporary solution for shoulder pain, an important use would be to help patients tolerate physical therapy better to help improve outcomes. It may also be an option for patients who do not want a permanent implant. At this time, we can only recommend this therapy after the failure of other conservative measures, such as physical therapy and corticosteroid injections. However, in those instances when these better-studied treatments fail, and the patient is not being recommended for surgery or does not desire surgery, 60-day PNS may be a viable treatment option. Future Level I data may show that 60-day PNS helps improve outcomes and delay the need for surgery in many patients with shoulder pathologies.
Inoperable Knee Pain (or Patient Resistant to Surgery)
Knee osteoarthritis is the most common cause of knee pain and affects more than 27 million Americans and 250 million people worldwide. The major risk factors for the development of knee osteoarthritis include obesity, female sex, and advanced age.100–102 Due to the destructive nature of the disease process, total knee arthroplasty (TKA) is the only definitive treatment. For patients unable or unwilling to proceed with surgery, a variety of less invasive options are available.
The AAOS and the American College of Rheumatologists strongly recommend weight loss and exercise for initial management. Oral and topical NSAIDs are endorsed as first-line medical therapies by both organizations. Evidence of efficacy for acetaminophen, duloxetine, and opioids appears to be inconclusive, and recommendations involve individualized patient situations. Consensus guidance regarding intra-articular administration of corticosteroids, viscosupplemental (hyaluronic acid) materials, and regenerative medicine injectates (such as platelet-rich plasma [PRP]) is indeterminate due to variable, limited and contradictory literature.100
Non-surgical interventional management of chronic knee pain has primarily relied on blocks and RFA of the genicular nerves. There is sparse literature involving PNS for inoperable chronic knee pain. The largest case series involving 19 patients found improved pain scores sustained at two months following the explant of 60-day PNS.103 In a similar case series of 17 patients, 14 non-surgical candidates showed 50% or greater pain reduction after explantation at 60 days, with durable results at six months.104 A case series of three patients found an increase in functional capacity and a decrease in analgesic use after temporary PNS stimulator placement; the third patient required explantation shortly after lead placement due to intolerable muscle cramping.105 Finally, a case study involving PNS lead placement along the saphenous nerve in the adductor canal in a medically refractory patient showed significant improvement in pain scores and function.106
Post-Operative Knee Pain
Despite improvements in total joint replacement surgery, 10–34% of patients experience persistent pain after knee arthroplasty.107 PNS is an additional therapy option that targets the corresponding nerves distal to the dorsal root ganglion. Recent advancements in PNS technology and favorable reimbursement policies have made it possible to use dedicated stimulation equipment for peripheral nerves. When patients continue to experience knee pain after total joint replacement surgery, PNS has been shown to provide long-term pain relief as an alternative to medications and injections. Interestingly, due to their distinct mechanisms of action, the lack of pain relief with diagnostic nerve block is not a contraindication for PNS therapy.
Several nerve targets have been described to treat chronic knee pain, including the femoral and sciatic nerves and their distal branches, such as saphenous and genicular. Introducing the temporary 60-day PNS option has challenged our traditional paradigm of performing a trial followed by permanent implantation.
A temporary 60-day PNS was first introduced to treat post-stroke shoulder pain.25 The potential indications for temporary PNS have since expanded to include post-surgical knee pain. Ilfeld et al demonstrated in a feasibility study that a novel percutaneous PNS device placed before TKA provided peri-operative pain relief until removal at six weeks.30
Goree et al later conducted a multi-center randomized, placebo-controlled trial evaluating the use of 60-day PNS in treating persistent post-operative knee pain.108 In this study, subjects with chronic refractory knee pain after TKA were randomized 1:1 to undergo 60-day PNS (29/56) versus a placebo (sham) stimulation (27/56) targeting the femoral and sciatic nerves. Subjects and evaluators were unblinded one month after the removal of PNS leads. Control-arm patients were allowed to cross over and receive active PNS therapy (10/20). This study showed significant pain relief and improvement in walking with 60-day PNS therapy at the primary endpoint (weeks five to eight). At three months, 70% (14/20) of the active PNS group reported holistic response compared to the 30% (6/20) in the placebo arm. This ongoing study is designed to follow subjects for up to 12 months, with early data suggesting long-term sustained pain relief.
The COMFORT trial is an ongoing multi-center, randomized-controlled study designed to evaluate using a micro-IPG PNS for treating post-surgical pain.109 The patients with refractory post-surgical pain were randomized 2:1 with conventional medical management as the control arm. The study included 16/77 participants in the modified intention-to-treat population for knee pain. The saphenous nerve within the adductor canal was the surgical target for patients with post-surgical knee pain. The active arm had a reported 88% responder rate at six months. Secondary endpoints of the study included improvements in disability and QOL. This study includes other chronic post-surgical pain indications and is scheduled to follow up with the subjects for three years.
Früh et al described using an externally powered, electromagnetically coupled PNS device targeting the infrapatellar saphenous nerve to treat refractory post-surgical knee pain.110 This was a retrospective review of 33 patients from Germany. Of these, 25 were implanted with the PNS device (six were explanted for lack of efficacy and two for wound infection). At six months post-implantation, n=25 subjects reported significant improvement in pain, QOL, and sleep, with a reduction in opioid intake. The remaining nine patients reported sustained benefit at 12 months. In this study, patients were implanted without a trial, with a high failure rate of 18.2%.
As the need for joint replacement surgery continues to increase with an aging population, PNS has emerged as a valuable therapy modality in the treatment of chronic knee pain following surgery. Early clinical trials have illustrated the potential benefits of PNS targeting various peripheral nerves with positive clinical outcomes.
Post-Operative Foot or Ankle Pain
Background and Rationale
Foot and ankle surgery remains among the most common surgical areas in orthopedics and podiatry. Foot and ankle disorders are common reasons for orthopedic surgical intervention and common causes of persistent post-operative pain.111 These surgical procedures can include hallux valgus repairs (bunionectomy), arthroscopies, foot and ankle fracture repairs, Achilles tendon repairs, ankle arthrodesis, and total ankle replacements.
The nerves that innervate the foot and ankle are predominantly branches of the sciatic nerve (distal branches include common peroneal, deep peroneal, superficial peroneal, sural, and tibial nerves) and, to a lesser degree, the femoral nerve (saphenous nerve). These terminal peripheral nerves are small and course superficially as they run toward the foot and ankle. They are vulnerable to trauma, stretch, and compression injuries.112
Historically, the sciatic and femoral/saphenous nerves have been blocked using regional anesthesia in patients undergoing foot and ankle surgery. With PNS, these same nerves can be targeted to provide focal, robust relief while preserving motor function and allowing for participation in rehabilitation therapies, including physical therapy, movement, and desensitization.
Anatomic Considerations
When considering PNS for lower extremity nerves, it is crucial to avoid lead placement across large joints, such as the hip or knee, to minimize the risk of lead migration. The ergonomics and wearability of the IPG should also be assessed, with particular attention to avoiding locations like the posterior thigh or pelvic area, which may interfere with sitting and physical activities.112 In cases of lower extremity amputation surgery, consideration for future prosthetic placement should be part of the PNS lead placement planning. Ideally, the lead should be proximal to the amputation site to avoid mechanical compression or stresses from dressings and/or prosthetic devices.
Evidence for PNS in Foot and Ankle Post-Operative Pain
Orthopedic procedures have been reported to have the highest incidence of pain compared to other types of operations.111 The benefits of intensive and early post-operative therapy cannot be overstated since the intensity of acute post-operative pain correlates with the risk of developing a persistent chronic pain state.113
Recently, clinical research has demonstrated PNS’s effectiveness in managing chronic pain4,114–117 and acute post-operative pain.41,70,118–123 This novel post-operative pain management method after foot and ankle surgery holds great promise since it can reduce opioid requirements, avoid pharmacological dependence, and improve surgical outcomes and overall patient satisfaction.124,125
In a recent multicenter, randomized controlled trial with 60-day PNS therapy, patients undergoing ambulatory lower extremity surgery, including hallux valgus correction and ankle arthrodesis or arthroscopy, were implanted with a PNS lead on the sciatic nerve. They were randomized to active or sham stimulation for 14 days postoperatively. Active sciatic nerve stimulation resulted in substantially lower opioid use, average and maximum pain scores, and less pain-related interference compared to sham treatment during the post-operative period.70
A secondary analysis was further supported using percutaneous, temporary PNS in the lower extremity. Patients who received sciatic nerve stimulation after surgery experienced significant pain relief and needed fewer opioids compared to those given a sham treatment. Throughout the first week post-op, the group with active sciatic stimulation reported lower pain scores and reduced opioid consumption. They also had dramatically less physical and emotional interference due to pain during the treatment phase as well as the day following lead explantation.120
Approaches for Foot and Ankle Surgery
Temporary PNS for foot and ankle surgery is a novel approach, and optimal lead placement remains uncertain, influenced by patient anatomy and operator experience.118 Leads can be inserted anywhere along the sciatic nerve and its primary branches. Studies typically described an insertion point between the sciatic bifurcation and the subgluteal region. Distal branches of the sciatic, including the common peroneal and posterior tibial nerves, can be targeted at the popliteal fossa or more distally. For medial ankle pain, PNS of the saphenous nerve with the common peroneal or posterior tibial nerve can enhance analgesic coverage for the foot and ankle.69,126,127
The posterior tibial nerve provides sensory and motor innervation to the foot and ankle and can be the sole target for PNS in surgical procedures. The posterior tibial artery serves as a significant anatomical and sonographic landmark, typically located dorsal to the medial malleolus, with the nerve lying just posterior to the artery and nearer to the Achilles tendon.
Ultrasound guidance, with or without fluoroscopy, is essential for accurate lead placement and to promote safety during the procedure. When selecting the PNS nerve target, it is important to consider the proximity of adjacent vascular and anatomical structures and ease of access. This includes deciding between accessing the sciatic nerve in the subgluteal region versus the popliteal fossa and below, considering the potential for electrode migration and dislodgement.69,118,126
Post-Operative Shoulder Pain
Total shoulder arthroplasties in the United States are growing at an unprecedented rate. From 2011 to 2017, there has been a rise of greater than 103% in shoulder arthroplasties in the United States, with even higher growth in reverse total shoulder rates.128 Part of this growth stems from improvements in surgical technique, implant design, and expansion of surgical candidacy, including a younger patient demographic.129,130 Unfortunately, pain after shoulder surgery is commonplace, with an estimated rate of greater than 10%.130 The etiology of pain after shoulder surgery remains multifactorial and can stem from infection, prosthetic failure, metal hypersensitivity, or medical conditions predisposing to pain.130,131
Overall, the evidence for treatment of post-surgical pain with a 60-day PNS system is low (see Table 4). In a case report by Pierson et al, a 64-year-old patient with chronic right shoulder pain underwent arthroscopic subacromial decompression with rotator cuff repair, distal clavicle excision, and biceps tenodesis with profound initial improvement followed by subsequent return of pain.132 She then underwent a reverse total shoulder replacement without significant pain relief. At 11 months post-surgery, the patient underwent placement of an axillary 60-day PNS system. Following removal of the system at 60 days, she continued to experience sustained pain relief and improved function (reduced shoulder pain and disability index) for more than one year and did not require any further treatment.
 |
Table 4 Literature Associated with PNS Treatment of Post-Operative Shoulder Pain |
Valimahomed et al performed a retrospective, pragmatic analysis of patients implanted with one or two leads targeting the axillary and/or suprascapular nerve in a larger study.99 Of the 768 patients, 206 had chronic post-surgical shoulder pain, the second-largest subgroup). Most of the data and analysis were combined for all shoulder pain etiologies (osteoarthritis, post-stroke, etc). However, percentage responder rates for the post-operative chronic pain subgroup were independently calculated and compared to the other subgroups in key domains such as improved pain, QOL, physical function, and sleep. They concluded the procedure to be safe with reported adverse events of about 5.9%, with the most common events being skin irritation, suspected infection, painful stimulation, or change in sensation/location stimulation, concluding the risk of the 60-day PNS system for treatment of shoulder pain to be low.99
In 2018, Ilfeld et al published their proof-of-concept study demonstrating that percutaneous PNS of the brachial plexus was feasible for ambulatory shoulder surgery, especially in rotator cuff repairs, but immediate postoperative pain relief was not as potent as local anesthetic. They did show a decrease in opioid utilization in the postoperative period.118
Chronic Back Pain After Return of Pain Following RFA
The return of LBP after lumbar RFA is a significant concern in clinical practice, particularly for patients with chronic LBP due to lumbar facet syndrome. RFA, a minimally invasive procedure, alleviates pain by disrupting the neural signals (commonly carried by lumbar medial branch nerves) responsible for pain transmission. While thermal ablation of the medial branch nerves may relieve pain, these nerves regenerate into the joint and surrounding musculature, leading to painful symptoms returning within a year.133
PNS of the medial branch nerve is an attractive treatment option for managing chronic axial back pain in patients whose symptoms persist after RFA. A prospective multicenter study focused on PNS targeting the medial branch nerves found significant improvements in patients suffering from chronic axial back pain following RFA treatment after six months. The study reported that 67% of participants experienced a clinically significant reduction in average pain intensity after just two months of PNS treatment.20
Furthermore, improvements in functional outcomes were notable, with 87% of patients showing enhanced disability measures and 80% experiencing reduced pain interference. Remarkably, 93% of participants reported clinically meaningful improvements across one or more outcome measures five months after the initiation of PNS, suggesting that PNS can provide substantial relief even when previous interventions like RFA have failed.20
The resurgence of lumbar chronic LBP after RFA therapy may result from ongoing degeneration in the lumbar spine, degenerative disc disease or spinal instability, and incomplete thermal ablation of the neural targets due to anatomic variability in neural anatomy.134–136 Additionally, about 70% of patients with chronic back pain show signs of muscle atrophy (especially after RFA of the medial branch nerves), which weakens spine stability and makes them more vulnerable to recurring pain.137
PNS has also shown potential for long-term relief. One case series found that patients could sustain pain reduction for up to a year after a short-term PNS implant.23 There is further validation by a multicenter study that consistently reports positive outcomes in pain reduction and QOL improvements. The primary endpoints of a multicenter study on 60-day PNS for chronic axial back pain indicated significant efficacy in managing this condition.21 Such broad validation across multiple centers underscores PNS as a reliable treatment option for chronic LBP, particularly in individuals experiencing pain recurrence after RFA. Regarding cost-effectiveness, PNS can be more economical than repeated invasive procedures.138
The growing body of evidence suggests that PNS is an effective therapy for chronic LBP, especially in patients whose pain recurs following RFA. PNS’s documented efficacy, long-term relief, alignment with patient preferences, and cost-effectiveness make it an attractive option for managing chronic back pain. The combined insights from various studies create a compelling case for integrating PNS into treatment plans for chronic LBP patients.
Chronic Back Pain with Suspected Centralization of Pain
Management of chronic axial LBP starts with staying active and exercise.139 Data from a recent systematic review supports that the first line of non-pharmacological treatment for chronic LBP is physical therapy.140 When patients have failed or exhausted physical therapy as a treatment option, the next step is pharmacological intervention with NSAIDs. Topical analgesics can also be trialed; however, this also can reach a plateau in efficacy over time.139 In addition to the aforementioned conservative measures, acetaminophen, skeletal muscle relaxants, acupuncture, superficial heat, interdisciplinary rehabilitation, spinal manipulation, brief individualized educational interventions, massage, and yoga have all been found to have a moderate net benefit.139 Opioids and benzodiazepines should be limited to rare situations where other modalities have been exhausted, and the risks associated with these medications are measured and monitored.
Interventional pain physicians offer procedures to ameliorate conditions once conservative care has failed. First introduced by Shealy, a neurosurgeon, in 1975, RFA of targeted nerves was found to help offer pain relief for several patients with chronic LBP.141 RFA is a procedure that includes an electrical current that runs through an insulated needle leaving an exposed “active tip” thermal activity. At the active tip, the electric field causes molecular movement, which results in thermal energy. Thermal energy creates a small lesion of denaturizing protein, which ultimately disrupts the transmission of nociception. The nerves in the low back targeted in patients with axial LBP are the medial branch nerves that innervate the facet joints, accounting for approximately one-third of axial LBP.
Increasing evidence suggests that axial LBP can be treated with regenerative medicine. A recent narrative review evaluated the roles and applications of mesenchymal stem cells, growth factors, PRP, and prolotherapy in patients with chronic LBP. Despite their promising therapeutic applications, clinical evidence in this area is still limited, and further clinical trials are required to evaluate the efficacy and safety of these methods compared with current standard treatments.142
PNS of the medial branch nerves has demonstrated positive outcomes. A recent prospective clinical trial showed that percutaneous PNS offers an effective clinical alternative for treating chronic axial back pain in patients beyond six months from a lumbar medial branch RFA. This study showed that percutaneous PNS provides a nondestructive, nonsurgical, non-opioid, motor-sparing treatment for axial back pain that can provide durable relief. Percutaneous PNS may also be considered for patients with axial back pain who have failed medial branch blocks, wherein RFA is not indicated, and the subsequent treatment option is often unclear. Percutaneous PNS has the potential to shift the pain management paradigm by providing an effective neuromodulation treatment earlier on the care continuum than has previously been considered.20
PNS is well established as a potential treatment for centralized LBP. Deer et al proposed a theory of peripherally induced reconditioning of the central nervous system to explain sustained reductions in pain that persist beyond the PNS treatment period.19 The authors propose that selective large-diameter afferent fiber activation may reverse some of the processes that result in chronic pain.
A review by Gilmore et al in 2020 noted that both 60-day PNS and permanent PNS showed promising results.66 Cohen et al, in 2019, found that six out of nine patients with LBP responded to PNS, with an average pain relief of 80%.143 Overall, 83% of patients were able to reduce analgesic medication consumption by at least 50%. This study was consistent with case reports and small series published or presented at society meetings around that time.
In 2020, Gilmore et al published a prospective, multicenter study with 74 subjects, of which 67% reported substantial, clinically significant reductions in average pain intensity (≥50%) at the end of treatment compared to baseline with medial branch PNS for axial LBP.23 Twelve months later, 57% of patients had ≥50% reduction in pain intensity and an average 32-point reduction in Oswestry Disability Index scores. Gilmore et al published in 2023 that 91% of patients with axial LBP undergoing 60-day PNS had clinically meaningful improvement in at least one outcome (pain intensity, disability, pain interference) with PNS, and this improvement persisted in 91% of subjects after two months and 77% at 14 months.59
Chronic Occipital Neuralgia
Headache disorders are considered one of the most common causes of pain and disability worldwide.144 One common headache subset, occipital neuralgia, is defined by the International Headache Society as unilateral or bilateral paroxysmal, shooting, or stabbing pain in the posterior scalp over the distribution of occipital nerves, often accompanied by local tenderness.145 Patients will frequently describe this pain as occurring in a “ram horn” distribution across the scalp. The exact pathophysiology underlying occipital neuralgia is unknown; however, it has been postulated to be due to direct occipital nerve irritation by muscular and neurogenic causes.146,147 Common treatment options for occipital neuralgia include physical therapy, medication (gabapentinoids, SNRIs, NSAIDs), nerve blocks, RFA, and surgical decompression.146–148 None of these interventions are without risk, with one study showing RFA at the level of the C2-3 and the third occipital nerve, having a 19% chance of post-ablation neuritis.149 In this study, symptom length varied greatly, with an average of 2.6 months. Unlike neurostimulation, nerve ablation results in loss of function, leading to numbness over the scalp and neck until the nerve regenerates.
PNS specifically targeting the occipital nerves has been reported for several decades.148 Many studies have focused on the stimulation of the occipital nerves for the treatment of a multitude of headache types, including occipital neuralgia, migraine headache, cluster headache, short-lasting unilateral neuralgiform headache attacks, hemicrania continua, and cervicogenic headaches.146,150 High-level evidence exists for treating chronic, intractable migraine headaches with occipital nerve stimulation. Many studies have focused on unilateral or bilateral leads implanted with an IPG.150 Although there is evidence for the efficacy of occipital nerve stimulation, hardware-related adverse events using off-label percutaneous SCS leads are high, with 40.7–45% requiring surgery to address hardware complications in two studies.151 Evidence for using a 60-day temporary PNS system to treat occipital neuralgia is comparatively sparse.
A case report by Moman et al published in 2022 discussed a singular case of a patient for which a unilateral 60-day PNS system provided 12 months of relief following removal of the lead, demonstrating the possibility of long-term benefit following device removal.147
In one of the largest studies, Pingree et al performed a cross-sectional study on real-world patients at least three months after PNS system removal. Patients were sorted into subsets of pain, with approximately 86 patients sorted into ulnar, median, radial, brachial plexus, ilioinguinal, intercostal, pudendal, occipital, and lateral femoral cutaneous groups. The primary goal of this study was to assess long-term patient outcomes after 60-day PNS treatment. Overall, at the time of the survey, 50% of patients reported a substantial (50% or greater) sustained benefit or improvement in QOL.41 Additionally, 35% of patients were reported to decrease or stop opioid use after 60-day PNS stimulation.41 Likewise, 32% of patients on anticonvulsants such as gabapentin and pregabalin reported a dosage reduction or cessation.41 See Table 5.
 |
Table 5 Literature Associated with PNS Treatment for Occipital Neuralgia |
Chronic Neck Pain
Chronic neck pain is a prevalent condition that significantly impacts QOL and functional ability. Conventional treatments, such as physical therapy, medications, facet injections, and medial branch RFA, may provide relief for some patients but are not always completely effective. In recent years, PNS has emerged as a promising option for managing chronic pain, including neck pain.
A notable case series explored the use of subcutaneous PNS for axial neck and LBP. The study reported positive outcomes in pain relief and functional improvement among ten patients who underwent a trial of subcutaneous PNS, with six opting for permanent implantation. The average patient-reported pain relief at the last follow-up was 45%. Half of the implanted patients preferred stimulation settings that included inter-lead stimulation, suggesting enhanced efficacy through targeting multiple pain pathways. This research highlights the potential of subcutaneous PNS for chronic neck pain, demonstrating its ability to provide meaningful pain relief and improve function in patients suffering from this condition.14
Further supporting the use of PNS, a prospective multicenter study focused on 60-day percutaneous medial branch PNS for chronic axial back pain. The results indicated significant pain reduction and QOL improvements for participants. While the study specifically addressed back pain, the similar underlying pain pathways involved in neck and back pain suggest that these techniques could be effectively adapted for managing chronic neck pain.21
Long-term efficacy is another critical consideration when evaluating PNS as a treatment option. A case series reported that patients receiving PNS for chronic LBP experienced sustained relief for up to one year following a short-term implant. Given the similarities in chronic axial neck and back pain, it is reasonable to infer that PNS could provide similar long-term benefits for those suffering from chronic neck pain.22
Additionally, a retrospective case series examined the clinical outcomes of PNS across various pain conditions, including neck pain. The results indicated improvements in pain scores and functionality among patients treated with PNS, supporting its use as a viable option for chronic neck pain management.152 A related retrospective review further corroborated these findings, demonstrating significant pain reduction and improved patient-reported outcomes following 60-day PNS for chronic pain, including neck pain.42
The collective evidence from these studies underscores several key points regarding PNS for chronic neck pain. First, PNS has shown efficacy for chronic pain conditions, including neck pain, with numerous studies indicating positive outcomes. Second, the long-term relief observed in similar pain conditions implies that patients with chronic neck pain may also benefit from sustained pain relief through PNS. Third, the real-world effectiveness demonstrated in various case series highlights the practical applicability of PNS in clinical settings, reinforcing its role as a reliable treatment option. Moreover, the techniques used in PNS for back pain, such as medial branch stimulation and inter-lead stimulation, can be adapted for addressing neck pain. These similarities provide a rationale for utilizing PNS to target the overlapping pain pathways involved in both conditions.
Neuropathic Pain within the Distribution of Up to Two Nerves
Neuropathic pain is defined as pain caused by a lesion or disease of the somatosensory nervous system. It is a “clinical description (and not a diagnosis) which requires a demonstrable lesion or a disease that satisfies established neurological diagnostic criteria”.153 Notably, recognized painful neuropathic conditions include post-herpetic neuralgia (PHN), painful diabetic neuropathy (PDN), and post-amputation pain.
PHN develops after the reactivation of the herpes zoster virus from its latent state. The virus is kept in a latent state in the dorsal root ganglion by the body’s cell-mediated immunity.154 Commonly affected regions include ophthalmic (32%), thoracic (16.5%), and facial (16%) distributions.155 Two primary pathophysiologic mechanisms of PHN pain include sensitization and deafferentation. Both gabapentin156 and pulsed radiofrequency of the dorsal root ganglion157 have demonstrated benefit in patients with PHN. When these are ineffective, PNS may be considered. Likewise, PDN affects millions of patients in the United States, and medications have shown mixed benefits. Amitriptyline, gabapentin, duloxetine, and pregabalin have all shown some benefit in studies,154 as has topical capsaicin.158
When neuropathic pain persists despite pharmacologic interventions, psychological support, and physical and other interventional therapies, neuromodulation may be considered. SCS and PNS are valuable options for patients with persistent neuropathic pain. These therapies reduce pain perception and improve functional outcomes by modulating the electrical signals within nerve pathways. SCS has been particularly effective in treating complex regional pain syndrome and post-surgical pain, while PNS offers targeted relief for specific nerve injuries.154,159
Post-Amputation Pain
Gilmore et al conducted a multi-center, randomized, double-blind, placebo-controlled trial with 28 traumatic lower extremity amputation patients with residual or phantom limb pain.34 Patients were randomized to eight weeks of PNS or four weeks of placebo followed by four weeks of PNS. Leads targeting the femoral and sciatic nerves were placed under ultrasound guidance. Greater than 50% pain relief was achieved in 67% of patients in the PNS group compared to 0% in the other group at the end of the placebo period (see Figure 2). Pain interference was reduced by greater than 50% in 56% of patients in the PNS group, while reduction in depression was also reduced in a statistically significant manner.
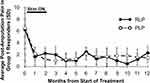 |
Figure 2 Pain Response to PNS in Post-Amputation Pain. Reprinted from Gilmore CA, Ilfeld BM, Rosenow JM et al. Percutaneous 60-day peripheral nerve stimulation implant provides sustained relief of chronic pain following amputation: 12-month follow-up of a randomized, double-blind, placebo-controlled trial. Regional Anesthesia & Pain Medicine. 2020;45(1):44–51. Creative Commons.34 |
A more recent single-center, prospective, randomized, controlled pilot study was conducted with patients receiving either PNS and SMT or SMT alone in the acute and subacute period immediately after amputation surgery.91 A total of 16 patients were allocated 1:1 and followed for three months. The PNS group had much higher rates of responders with ≥50% pain relief, with phantom limb pain patients at 76% vs 29% in the SMT group and residual limb pain patients at 86% vs 52% in the SMT group. Additionally, fewer patients with PNS were using opioids compared to the SMT group at each time point in the study. Thirty-day readmission rates were 0% in the PNS group and 25% in the SMT group. A study by Rauck et al investigated the efficacy of PNS in 14 patients with moderate-to-severe post-amputation pain.32 There was a 30% greater reduction in residual limb pain and a 34% greater reduction in phantom limb pain compared to placebo.
A retrospective study of 126 patients with either temporary or permanent PNS found that both groups had statistically significant pain reduction at all time points and that there was no significant difference in outcomes between 60-day PNS and permanently implanted PNS.160
Conclusion
PNS platforms represent significant opportunities to address a wide variety of pain conditions throughout the body. 60-day PNS therapy affords multiple unique advantages. The efficacy of this treatment approach has been demonstrated, with durability extending beyond the removal of the system. This manuscript details current evidence associated with several specific conditions and provides consensus guidelines for the use of 60-day PNS therapy in relation to the strength of the evidence. Further studies are needed to elucidate the optimal application of 60-day PNS treatment.
Abbreviations
AAOS, American Academy of Orthopaedic Surgeons; ASPN, American Society of Pain and Neuroscience; GABA, Gamma-aminobutyric acid; HA, Hyaluronic acid; IPG, Implantable pulse generator; LBP, Low back pain; NSAID, Non-steroidal anti-inflammatory drug; PDN, Painful diabetic neuropathy; PHN, Post-herpetic neuralgia; PNS, Peripheral nerve stimulation; PRP, Platelet-rich plasma; QOL, Quality of life; RFA, Radiofrequency ablation; SCS, Spinal cord stimulation; SMT, Standard medical therapy; TKA, Total knee arthroplasty; TSA, Total shoulder arthroplasty; FDA, United States Food and Drug Administration; USPSTF, United States Preventive Services Task Force.
Acknowledgments
Editing was provided by Allison Foster, PhD, of Foster Medical Communications.
Funding
Development of this guideline was supported by an unrestricted educational grant from SPR Therapeutics.
Disclosure
Usman Latif: Consultant: Abbott, Brixton Biosciences, Hydrocision, Nalu Medical, Nevro, Omnia Medical, Saluda, Spinal Simplicity, SPR Therapeutics, Stryker, Vertos Medical, Vivex Biologics; Research funding: Mainstay Medical, Spinal Simplicity, Vivex Biologics; Stock: InFormed Consent, Spinal Simplicity. Scott Pritzlaff: Consultant SPR Therapeutics, Bioventus, Nalu Medical; Education grants from Abbott, Biotronik, Medtronic, and Nevro; Royalties from Wolters Kluwer. Ioannis Skaribas: Consultant Abbott, Nalu. Hemant Kalia: Consultant Abbott, Averitas, Nalu, Curonix, SPR Therapeutics, Nervonik, Virdio Health. Samir Sheth: Consultant SPR, Medtronic, Vertos, Boston Scientific, SI Bone; Royalties from Wolters Kluwer. Madi Schnur: Consultant SPR Therapeutics. Sean Li: Consultant Abbott, Avanos, Averitas Pharma, Boston Scientific, Biotronik, Medtronic, Nalu Medical, PainTeq, Presidio, Saluda, SPR Therapeutics, Stryker; Research funding Avanos, Averitas Pharma, Nevro, Presidio, SPR Therapeutics, Stock options NeuroOne, Nalu Medical. Denise Lester: the Primary Investigator for the RESET trial; Research funding from SPR Therapeutics. Ramana Naidu: Consultant Abbott, Avanos, Boston Scientific, Bioventus, Biotronik, Medtronic, Nalu Medical, Nervonik, SPR Therapeutics. Royalties from McGraw-Hill. David Russo: Consultant Nalu, Nevro. Einar Ottestad: Consultant for BioVentus, SPR Therapeutics, Coloplast; Stock options for Restera Medical; Co-founder Altamont Medical. Henry Vucetic: Consultant Abbott, SPR Therapeutics, Vertos, Saluda, Boston Scientific. David Abejón: Proctor Abbott, Medtronic, Boston Scientific, Cardiva, MBA, Saluda Medical. Mehul Desai: Consultant Medtronic, Nalu Medical Stock Options AllaiHealth, HypreVention, SPR Therapeutics, SynerFuse, Virdio Health, Royalties Oxford Medical. David Dickerson: Consultant SPR, Stryker, Nalu, Vertos, Vertex, Abbott, Biotronik; Research support Abbott, SPR. Amitabh Gulati: Consultant for SPR therapeutics, Nalu Medical, Medtronic, AIS healthcare, Neurovasis, Tersera Medical, Hinge Health, Menda Health, Veritas Pharma. Sayed Dawood: Stock Options Spr, Painteq, Mainstay; personal fees from Abbott, Saluda. Timothy Deer: consultant research Abbott, SpineThera, Saluda Medical, Cornerloc, Boston Scientific, personal fees, Pain Teq, Spinal Simplicity, Biotronik, Aurora, Nervonik, SPR Therapeutics, outside the submitted work; In addition, Dr Timothy Deer has a patent pending to Abbott. The other authors report no conflicts of interest in this work.
References
1. Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150(3699):971–979. doi:10.1126/science.150.3699.971
2. Wall PD, Sweet WH. Temporary abolition of pain in man. Science. 1967;155(3758):108–109. doi:10.1126/science.155.3758.108
3. Deer TR, Levy RM, Verrills P, Mackey S, Abejon D. Perspective: peripheral nerve stimulation and peripheral nerve field stimulation birds of a different feather. Pain Med. 2015;16(3):411–412. doi:10.1111/pme.12662
4. Strand N, D’Souza RS, Hagedorn JM, et al. Evidence-based clinical guidelines from the American society of pain and neuroscience for the use of implantable peripheral nerve stimulation in the treatment of chronic pain. J Pain Res. 2022;15:2483–2504. doi:10.2147/JPR.S362204
5. Gildenberg PL. History of electrical neuromodulation for chronic pain. Pain Med. 2006;7(s1):S7–S13.
6. Gildenberg PL. Treatment of spasmodic torticollis by dorsal column stimulation. Appl Neurophysiol. 1978;41(1–4):113–121.
7. Cook AW. Electrical stimulation in multiple sclerosis. Hosp Pract. 1976;11(4):51–58. doi:10.1080/21548331.1976.11706516
8. Dooley DM. Spinal cord stimulation. AORN J. 1976;23(7):1209–1212. doi:10.1016/S0001-2092(07)64597-9
9. Augustinsson LE, Carlsson CA, Holm J, Jivegard L. Epidural electrical stimulation in severe limb ischemia: pain relief, increased blood flow, and a possible limb-saving effect. Ann Surg. 1985;202(1):104–110. doi:10.1097/00000658-198507000-00017
10. Murphy DF, Giles KE. Dorsal column stimulation for pain relief from intractable angina pectoris. Pain. 1987;28(3):365–368. doi:10.1016/0304-3959(87)90070-4
11. Weiner RL, Reed KL. Peripheral neurostimulation for control of intractable occipital neuralgia. Neuromodulation. 1999;2(3):217–221. doi:10.1046/j.1525-1403.1999.00217.x
12. Huntoon M, Huntoon E, Obray J, Lamer T. Feasibility of ultrasound-guided percutaneous placement of peripheral nerve stimulation electrodes in a cadaver model: part one, lower extremity. Reg Anesth Pain Med. 2008;33(6):551–557. doi:10.1016/j.rapm.2008.04.007
13. Huntoon MA, Burgher AH. Ultrasound-guided permanent implantation of peripheral nerve stimulation (PNS) system for neuropathic pain of the extremities: original cases and outcomes. Pain Med. 2009;10(8):1369–1377. doi:10.1111/j.1526-4637.2009.00745.x
14. Burgher AH, Huntoon MA, Turley TW, Doust MW, Stearns LJ. Subcutaneous peripheral nerve stimulation with inter-lead stimulation for axial neck and low back pain: case series and review of the literature. Neuromodulation: Technol Neural Interface. 2012;15(2):100–107. doi:10.1111/j.1525-1403.2011.00388.x
15. Corriveau M, Lake W, Hanna A. Nerve stimulation for pain. Neurosurg Clin N Am. 2019;30(2):257–264. doi:10.1016/j.nec.2018.12.008
16. Singh V. A comparison of various peripheral nerve stimulators available currently on the market. ASRA News. 2022;47(4). doi:10.52211/asra110122.045
17. Ilfeld BM, Gabriel RA, Saulino MF, et al. Infection rates of electrical leads used for percutaneous Neurostimulation of the peripheral nervous system. Pain Pract. 2017;17(6):753–762. doi:10.1111/papr.12523
18. Cohen SP, Gilmore CA, Rauck RL, et al. Percutaneous peripheral nerve stimulation for the treatment of chronic pain following amputation. Mil Med. 2019;184(7–8):e267–e274. doi:10.1093/milmed/usz114
19. Deer TR, Eldabe S, Falowski SM, et al. Peripherally induced reconditioning of the central nervous system: a proposed mechanistic theory for sustained relief of chronic pain with percutaneous peripheral nerve stimulation. J Pain Res. 2021;14:721–736. doi:10.2147/JPR.S297091
20. Deer TR, Gilmore CA, Desai MJ, et al. Percutaneous peripheral nerve stimulation of the medial branch nerves for the treatment of chronic axial back pain in patients after radiofrequency ablation. Pain Med. 2021;22(3):548–560. doi:10.1093/pm/pnaa432
21. Gilmore CA, Desai MJ, Hopkins TJ, et al. Treatment of chronic axial back pain with 60‐day percutaneous medial branch PNS: primary end point results from a prospective, multicenter study. Pain Pract. 2021;21(8):877–889. doi:10.1111/papr.13055
22. Gilmore CA, Kapural L, McGee MJ, Boggs JW. Percutaneous Peripheral Nerve Stimulation (PNS) for the treatment of chronic low back pain provides sustained relief. Neuromodulation: Technol Neural Interface. 2019;22(5):615–620. doi:10.1111/ner.12854
23. Gilmore CA, Kapural L, McGee MJ, Boggs JW. Percutaneous peripheral nerve stimulation for chronic low back pain: prospective case series with 1 year of sustained relief following Short-term implant. Pain Pract. 2020;20(3):310–320. doi:10.1111/papr.12856
24. Chae J, Wilson RD, Bennett ME, Lechman TE, Stager KW. Single‐lead percutaneous peripheral nerve stimulation for the treatment of hemiplegic shoulder pain: a Case series. Pain Pract. 2013;13(1):59–67. doi:10.1111/j.1533-2500.2012.00541.x
25. Chae J, Yu DT, Walker ME, et al. Intramuscular electrical stimulation for hemiplegic shoulder pain: a 12-month follow-up of a multiple-center, randomized clinical trial. Am J Phys Med Rehabil. 2005;84(11):832–842. doi:10.1097/01.phm.0000184154.01880.72
26. Renzenbrink GJ, Ijzerman MJ. Percutaneous neuromuscular electrical stimulation (P-NMES) for treating shoulder pain in chronic hemiplegia. effects on shoulder pain and quality of life. Clin rehabilitat. 2004;18(4):359–365. doi:10.1191/0269215504cr759oa
27. Wilson RD, Gunzler DD, Bennett ME, Chae J. Peripheral nerve stimulation compared with usual care for pain relief of hemiplegic shoulder pain: a randomized controlled trial. Am J Phys Med Rehabil. 2014;93(1):17–28. doi:10.1097/PHM.0000000000000011
28. Yu DT, Chae J, Walker ME, Fang ZP. Percutaneous intramuscular neuromuscular electric stimulation for the treatment of shoulder subluxation and pain in patients with chronic hemiplegia: a pilot study. Arch Phys Med Rehabil. 2001;82(1):20–25. doi:10.1053/apmr.2001.18666
29. Wilson RD, Harris MA, Gunzler DD, Bennett ME, Chae J. Percutaneous peripheral nerve stimulation for chronic pain in subacromial impingement syndrome: a case series. Neuromodulation: Technol Neural Interface. 2014;17(8):771–776. doi:10.1111/ner.12152
30. Ilfeld BM, Ball ST, Gabriel RA, et al. A feasibility study of percutaneous peripheral nerve stimulation for the treatment of postoperative pain following total knee arthroplasty. Neuromodulation. 2019;22(5):653–660. doi:10.1111/ner.12790
31. Ilfeld BM, Gilmore CA, Grant SA, et al. Ultrasound-guided percutaneous peripheral nerve stimulation for analgesia following total knee arthroplasty: a prospective feasibility study. J Orthop Surg Res. 2017;12(1):4. doi:10.1186/s13018-016-0506-7
32. Rauck RL, Cohen SP, Gilmore CA, et al. Treatment of post-amputation pain with peripheral nerve stimulation. Neuromodulation: Technol Neural Interface. 2014;17(2):188–197. doi:10.1111/ner.12102
33. Gilmore C, Ilfeld B, Rosenow J, et al. Percutaneous peripheral nerve stimulation for the treatment of chronic neuropathic postamputation pain: a multicenter, randomized, placebo-controlled trial. Reg Anesth Pain Med. 2019;44(6):637–645. doi:10.1136/rapm-2018-100109
34. Gilmore CA, Ilfeld BM, Rosenow JM, et al. Percutaneous 60-day peripheral nerve stimulation implant provides sustained relief of chronic pain following amputation: 12-month follow-up of a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med. 2020;45(1):44–51. doi:10.1136/rapm-2019-100937
35. Mirone G, Natale M, Rotondo M. Peripheral median nerve stimulation for the treatment of iatrogenic complex regional pain syndrome (CRPS) type II after carpal tunnel surgery. J Clin Neurosci. 2009;16(6):825–827. doi:10.1016/j.jocn.2008.09.006
36. Hegarty D, Goroszeniuk T. Peripheral nerve stimulation of the thoracic paravertebral plexus for chronic neuropathic pain. Pain Physician. 2011;14(3):295–300.
37. Yakovlev AE, Peterson AT. Peripheral nerve stimulation in treatment of intractable postherpetic neuralgia. Neuromodulation. 2007;10(4):373–375. doi:10.1111/j.1525-1403.2007.00126.x
38. Mainkar O, Singh H, Gargya A, Lee J, Valimahomed A, Gulati A. Ultrasound-guided peripheral nerve stimulation of cervical, thoracic, and lumbar spinal nerves for dermatomal pain: a case series. Neuromodulation: Technol Neural Interface. 2021;24(6):1059–1066. doi:10.1111/ner.13334
39. Finneran JJ, Furnish T, Curran BP, Ilfeld BM. Percutaneous peripheral nerve stimulation of the brachial plexus for intractable phantom pain of the upper extremity: a case report. A&A Practice. 2020;14(14):e01353. doi:10.1213/XAA.0000000000001353
40. Langford B, Mauck WD. Peripheral nerve stimulation: a new treatment for meralgia paresthetica. Pain Med. 2021;22(1):213–216. doi:10.1093/pm/pnaa326
41. Pingree MJ, Hurdle MF, Spinner DA, Valimahomed A, Crosby ND, Boggs JW. Real-world evidence of sustained improvement following 60-day peripheral nerve stimulation treatment for pain: a cross-sectional follow-up survey. Pain Management. 2022;12(5):611–621. doi:10.2217/pmt-2022-0005
42. Huntoon M. A retrospective review of real-world outcomes following 60-day peripheral nerve stimulation for the treatment of chronic pain. Pain Physician J. 2023;26(3):273–281. doi:10.36076/ppj.2023.26.273
43. Naidu R, Li S, Desai MJ, Sheth S, Crosby ND, Boggs JW. 60-day PNS treatment may improve identification of delayed responders and delayed non-responders to neurostimulation for pain relief. J Pain Res. 2022;15:733–743. doi:10.2147/JPR.S349101
44. Deer TR, Grider JS, Pope JE, et al. Best practices for minimally invasive lumbar spinal stenosis treatment 2.0 (MIST): consensus guidance from the American Society Of Pain And Neuroscience (ASPN). J Pain Res. 2022;15:1325–1354. doi:10.2147/JPR.S355285
45. Pope JE, Deer TR, Falowski S, et al. Multicenter retrospective study of neurostimulation with exit of therapy by explant. Neuromodulation: Technol Neural Interface. 2017;20(6):543–552. doi:10.1111/ner.12634
46. Murphy KR, Han JL, Hussaini SMQ, et al. The volume-outcome effect: impact on trial-to-permanent conversion rates in spinal cord stimulation. Neuromodulation: Technol Neural Interface. 2017;20(3):256–262. doi:10.1111/ner.12526
47. Van Buyten JP, Wille F, Smet I, et al. Therapy-related explants after spinal cord stimulation: results of an international retrospective chart review study. Neuromodulation. 2017;20(7):642–649. doi:10.1111/ner.12642
48. Hayek SM, Veizi E, Hanes M. Treatment-limiting complications of percutaneous spinal cord stimulator implants: a review of eight years of experience from an academic center database. Neuromodulation: Technol Neural Interface. 2015;18(7):603–609. doi:10.1111/ner.12312
49. Dupré DA, Tomycz N, Whiting D, Oh M. Spinal cord stimulator explantation: motives for removal of surgically placed paddle systems. Pain Pract. 2018;18(4):500–504. doi:10.1111/papr.12639
50. McJunkin T, Lynch P, Srejic E. Complications of peripheral nerve stimulation: open technique, percutaneous technique, and peripheral nerve field stimulation. In: Reducing Risks and Complications of Interventional Pain Procedures. Saunders/Elsevier; 2012.
51. Weigel R, Capelle HH, Krauss JK. Failure of long-term nerve root stimulation to improve neuropathic pain. J Neurosurg. 2008;108(5):921–925. doi:10.3171/JNS/2008/108/5/0921
52. Kumar K, Wilson JR. Factors affecting spinal cord stimulation outcome in chronic benign pain with suggestions to improve success rate. Acta Neurochir Suppl. 2007;97(Pt 1):91–99.
53. Han JL, Murphy KR, Qasim hussaini SM, et al. Explantation rates and healthcare resource utilization in spinal cord stimulation. Neuromodulation. 2017;20(4):331–339. doi:10.1111/ner.12567
54. Reddy RD, Moheimani R, Yu GG, Chakravarthy KV. A review of clinical data on salvage therapy in spinal cord stimulation. Neuromodulation: Technol Neural Interface. 2020;23(5):562–571. doi:10.1111/ner.13067
55. Huang KT, Martin J, Marky A, et al. A national survey of spinal cord stimulation trial-to-permanent conversion rates. Neuromodulation: Technol Neural Interface. 2015;18(2):133–140. doi:10.1111/ner.12199
56. North R, Desai MJ, Vangeneugden J, et al. Postoperative infections associated with prolonged spinal cord stimulation trial duration (PROMISE RCT). Neuromodulation: Technol Neural Interface. 2020;23(5):620–625. doi:10.1111/ner.13141
57. Chincholkar M, Eldabe S, Strachan R, et al. Prospective analysis of the trial period for spinal cord stimulation treatment for chronic pain. Neuromodulation: Technol Neural Interface. 2011;14(6):523–529. doi:10.1111/j.1525-1403.2011.00384.x
58. North RB, Calodney A, Bolash R, et al. Redefining spinal cord stimulation “trials”: a randomized controlled Trial using single-stage wireless permanent implantable devices. Neuromodulation: Technol Neural Interface. 2020;23(1):96–101. doi:10.1111/ner.12970
59. Gilmore CA, Deer TR, Desai MJ, et al. Durable patient-reported outcomes following 60-day percutaneous peripheral nerve stimulation (PNS) of the medial branch nerves. Interventional Pain Med. 2023;2(1):100243. doi:10.1016/j.inpm.2023.100243
60. Knezevic NN, Candido KD, Vlaeyen JWS, Van Zundert J, Cohen SP. Low back pain. Lancet. 2021;398(10294):78–92. doi:10.1016/S0140-6736(21)00733-9
61. Murray CJL, Atkinson C, Bhalla K, et al. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608. doi:10.1001/jama.2013.13805
62. Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American college of physicians and the American pain society. Ann Internal Med. 2007;147(7):478. doi:10.7326/0003-4819-147-7-200710020-00006
63. Cohen SP, Bhaskar A, Bhatia A, et al. Consensus practice guidelines on interventions for lumbar facet joint pain from a multispecialty, international working group. Reg Anesth Pain Med. 2020;45(6):424–467. doi:10.1136/rapm-2019-101243
64. Sayed D, Grider J, Strand N, et al. The American Society of Pain and Neuroscience (ASPN) evidence-based clinical guideline of interventional treatments for low back pain. J Pain Res. 2022;15:3729–3832. doi:10.2147/JPR.S386879
65. Tieppo Francio V, Westerhaus BD, Rupp A, Sayed D. Non-spinal neuromodulation of the lumbar medial branch nerve for chronic axial low back pain: a narrative review. Front Pain Res. 2022;3:835519. doi:10.3389/fpain.2022.835519
66. Gilmore CA, Patel J, Esebua LG, Burchell M. A review of peripheral nerve stimulation techniques targeting the medial branches of the lumbar dorsal rami in the treatment of chronic low back pain. Pain Med. 2020;21(Suppl 1):S41–S46. doi:10.1093/pm/pnaa084
67. Abd-Elsayed A, Keith MK, Cao NN, Fiala KJ, Martens JM. Temporary peripheral nerve stimulation as treatment for chronic pain. Pain Ther. 2023;12(6):1415–1426. doi:10.1007/s40122-023-00557-3
68. Helm S, Shirsat N, Calodney A, et al. Peripheral nerve stimulation for chronic pain: a systematic review of effectiveness and safety. Pain Ther. 2021;10(2):985–1002. doi:10.1007/s40122-021-00306-4
69. Ilfeld BM, Gelfand H, Dhanjal S, et al. Ultrasound-guided percutaneous peripheral nerve stimulation: a pragmatic effectiveness trial of a nonpharmacologic alternative for the treatment of postoperative pain. Pain Med. 2020;21(Suppl 2):S53–S61. doi:10.1093/pm/pnaa332
70. Ilfeld BM, Plunkett A, Vijjeswarapu AM, et al. Percutaneous peripheral nerve stimulation (neuromodulation) for postoperative pain: a randomized, sham-controlled pilot study. Anesthesiology. 2021;135(1):95–110. doi:10.1097/ALN.0000000000003776
71. American Academy of Orthopaedic Surgeons (AAOS). Management of Glenohumeral Joint Osteoarthritis: Evidence-Based Clinical Practice Guideline; 2020. Available from: https://www.aaos.org/globalassets/quality-and-practice-resources/glenohumeral/gjo-cpg.pdf.
72. O’Donnell EA, Fury MS, Maier SP, Bernstein DN, Carrier RE, Warner JJP. Outpatient shoulder arthroplasty patient selection, patient experience, and cost analyses: a systematic review. JBJS Rev. 2021;9(11). doi:10.2106/JBJS.RVW.20.00235
73. Makhni EC, Swart E, Steinhaus ME, et al. Cost-effectiveness of reverse total shoulder arthroplasty versus arthroscopic rotator cuff repair for symptomatic large and massive rotator cuff tears. Arthroscopy. 2016;32(9):1771–1780. doi:10.1016/j.arthro.2016.01.063
74. Galvin JW, Kim R, Ment A, et al. Outcomes and complications of primary reverse shoulder arthroplasty with minimum of 2 years’ follow-up: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2022;31(11):e534–e544. doi:10.1016/j.jse.2022.06.005
75. Kovacevic D, Suriani RJ, Grawe BM, et al. Management of irreparable massive rotator cuff tears: a systematic review and meta-analysis of patient-reported outcomes, reoperation rates, and treatment response. J Shoulder Elbow Surg. 2020;29(12):2459–2475. doi:10.1016/j.jse.2020.07.030
76. Narvani AA, Imam MA, Godenèche A, et al. Degenerative rotator cuff tear, repair or not repair? A review of current evidence. Ann Royal Coll Surg Engl. 2020;102(4):248–255. doi:10.1308/rcsann.2019.0173
77. Karjalainen TV, Jain NB, Heikkinen J, Johnston RV, Page CM, Buchbinder R. Surgery for rotator cuff tears. Cochrane Database Syst Rev. 2019;12(12):CD013502. doi:10.1002/14651858.CD013502
78. Longo UG, Risi Ambrogioni L, Candela V, et al. Conservative versus surgical management for patients with rotator cuff tears: a systematic review and META-analysis. BMC Musculoskeletal Disor. 2021;22(1):50. doi:10.1186/s12891-020-03872-4
79. Wylie JD, Baran S, Granger EK, Tashjian RZ. A comprehensive evaluation of factors affecting healing, range of motion, strength, and patient-reported outcomes after arthroscopic rotator cuff repair. Orthopaedic Jl Sports Med. 2018;6(1):2325967117750104. doi:10.1177/2325967117750104
80. Sambandam SN, Khanna V, Gul A, Mounasamy V. Rotator cuff tears: an evidence based approach. World J Orthop. 2015;6(11):902–918. doi:10.5312/wjo.v6.i11.902
81. Clinker C, Smith KM, Ishikawa H, Joyce C, Tashjian RZ, Chalmers PN. Three-month delay in rotator cuff repair: 2-year follow-up. J Am Acad Orthop Surg Glob Res Rev. 2024;8(1). doi:10.5435/JAAOSGlobal-D-23-00283
82. Van Der List JP, Kok LM, Alta TDW, Van Der List MPJ, Van Noort A. Role of delay between injury and surgery on the outcomes of rotator cuff repair: a systematic review and meta-analysis. American J Sports Med. 2023;51(5):1328–1339. doi:10.1177/03635465211069560
83. Fu MC, O’Donnell EA, Taylor SA, et al. Delay to arthroscopic rotator cuff repair is associated with increased risk of revision rotator cuff surgery. Orthopedics. 2020;43(6):340–344. doi:10.3928/01477447-20200923-02
84. Mansfield JT, Desai MJ. Axillary peripheral nerve stimulation for painful end-stage primary osteoarthritis of the shoulder: a case report. Neuromodulation: Technol Neural Interface. 2020;23(6):878–880. doi:10.1111/ner.13089
85. Chitneni A, Hasoon J, Urits I, Viswanath O, Berger A, Kaye AD. Peripheral nerve stimulation for chronic shoulder pain due to rotator cuff pathology. Orthopedic Rev. 2022;14(3). doi:10.52965/001c.37494
86. Baskozos G, Hébert HL, Pascal MMV, et al. Epidemiology of neuropathic pain: an analysis of prevalence and associated factors in UK biobank. PAIN Rep. 2023;8(2):e1066. doi:10.1097/PR9.0000000000001066
87. van Velzen M, Dahan A, Niesters M. Neuropathic pain: challenges and opportunities. Front Pain Res. 2020;1:1. doi:10.3389/fpain.2020.00001
88. Slavin KV. Peripheral nerve stimulation for neuropathic pain. Neurotherapeutics. 2008;5(1):100–106. doi:10.1016/j.nurt.2007.11.005
89. Pagan-Rosado R, Smith BJ, Smither FC, Pingree MJ, D’Souza RS. Peripheral nerve stimulation for the treatment of phantom limb pain: a case series. Case Rep Anesthesiol. 2023;2023:1558183. doi:10.1155/2023/1558183
90. Gutierrez GJ, Zurn CA, Crosby ND. Sustained relief of Complex Regional Pain Syndrome (CRPS) pain following a 60-day peripheral nerve stimulation: a report of three cases. Cureus. 2024;16(2):e54458. doi:10.7759/cureus.54458
91. Albright-Trainer B, Phan T, Trainer RJ, et al. Peripheral nerve stimulation for the management of acute and subacute post-amputation pain: a randomized, controlled feasibility trial. Pain Management. 2022;12(3):357–369. doi:10.2217/pmt-2021-0087
92. American Academy of Orthopaedic Surgeons (AAOS). Management of Rotator Cuff Injuries: Evidence-Based Clinical Practice Guideline. 2019. Available from: https://www.aaos.org/globalassets/quality-and-practice-resources/rotator-cuff/rotator-cuff-cpg-final-12-20-19.pdf.
93. Mertens MG, Meert L, Struyf F, Schwank A, Meeus M. Exercise therapy is effective for improvement in range of motion, function, and pain in patients with frozen shoulder: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2022;103(5):998–1012.e14. doi:10.1016/j.apmr.2021.07.806
94. Pieters L, Lewis J, Kuppens K, et al. An update of systematic reviews examining the effectiveness of conservative physical therapy interventions for subacromial shoulder pain. J Orthop Sports Phys Ther. 2020;50(3):131–141. doi:10.2519/jospt.2020.8498
95. Wang W, Shi M, Zhou C, et al. Effectiveness of corticosteroid injections in adhesive capsulitis of shoulder: a meta-analysis. Medicine. 2017;96(28):e7529. doi:10.1097/MD.0000000000007529
96. Buchbinder R, Green S, Youd JM. Corticosteroid injections for shoulder pain. Cochrane musculoskeletal group, ed. Cochrane Database Syst Rev. 2003. doi:10.1002/14651858.CD004016
97. Mohamadi A, Chan JJ, Claessen FMAP, Ring D, Chen NC. Corticosteroid injections give small and transient pain relief in rotator cuff tendinosis: a meta-analysis. Clin Orthopaedics Related Res. 2017;475(1):232–243. doi:10.1007/s11999-016-5002-1
98. Mansfield JT, Desai MJ. Axillary peripheral nerve stimulation for chronic shoulder pain: a retrospective case series. Neuromodulation: Technol Neural Interface. 2020;23(6):812–818. doi:10.1111/ner.13096
99. Valimahomed A, Dickerson D, Vucetic H, et al. Real-world evidence of durable multi-dimensional improvement after 60-day peripheral nerve stimulation treatment used for shoulder pain. Pain Management. 2024;14(7):355–364. doi:10.1080/17581869.2024.2371779
100. Mora JC, Przkora R, Cruz-Almeida Y. Knee osteoarthritis: pathophysiology and current treatment modalities. Journal of Pain Research. 2018;11:2189–2196. doi:10.2147/JPR.S154002
101. Allen KD, Thoma LM, Golightly YM. Epidemiology of osteoarthritis. Osteoarthritis Cartilage. 2022;30(2):184–195. doi:10.1016/j.joca.2021.04.020
102. Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020;29-30:100587. doi:10.1016/j.eclinm.2020.100587
103. Vangeison CT, Bintrim DJ, Helms J, Saha AK, Samant AN, Chung M. The role of peripheral nerve stimulation in refractory non-operative chronic knee osteoarthritis. Pain Management. 2023;13(4):213–218. doi:10.2217/pmt-2023-0025
104. Kelly TD, Pazzol ML, Rahimi Darabad R. Peripheral nerve stimulation in chronic knee pain: a case series. Cureus. 2023;15(12):e50127. doi:10.7759/cureus.50127
105. Zhu CC, Gargya A, Haider N. A case report of three patients who underwent temporary peripheral nerve stimulation for treatment of knee pain secondary to osteoarthritis. Cureus. 2023;15(6):e40473. doi:10.7759/cureus.40473
106. Hasoon J, Chitneni A, Urits I, Viswanath O, Kaye AD. Peripheral stimulation of the saphenous and superior lateral genicular nerves for chronic knee pain. Cureus. 2021;13(4):e14753. doi:10.7759/cureus.14753
107. Cohen SP, Mishra P, Wallace M, Sellers A, Veizi E, Hurley RW. Emperor’s nakedness exposed: unmasking fairytales for genicular nerve radiofrequency ablation in knee osteoarthritis. Reg Anesth Pain Med. 2023;48(5):193–195. doi:10.1136/rapm-2022-104319
108. Goree JH, Grant SA, Dickerson DM, et al. Randomized placebo-controlled trial of 60-day percutaneous peripheral nerve stimulation treatment indicates relief of persistent postoperative pain, and improved function after knee replacement. Neuromodulation. 2024;27(5):847–861. doi:10.1016/j.neurom.2024.03.001
109. Hatheway J, Hersel A, Engle M, et al. Clinical study of a micro-implantable pulse generator for the treatment of peripheral neuropathic pain: 12-month results from the COMFORT-randomized controlled trial. Reg Anesth Pain Med. doi:10.1136/rapm-2024-106099
110. Früh A, Sargut TA, Hussein A, et al. Peripheral nerve stimulation for the treatment of chronic knee pain. Sci Rep. 2023;13(1):15543. doi:10.1038/s41598-023-42608-x
111. Chou LB, Wagner D, Witten DM, et al. Postoperative pain following foot and ankle surgery: a prospective study. Foot Ankle Int. 2008;29(11):1063–1068. doi:10.3113/FAI.2008.1063
112. Hanyu-Deutmeyer A, Pritzlaff SG. Peripheral nerve stimulation for the 21st century: sural, superficial peroneal, and tibial nerves. Pain Med. 2020;21(Suppl 1):S64–S67. doi:10.1093/pm/pnaa202
113. Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006;367(9522):1618–1625. doi:10.1016/S0140-6736(06)68700-X
114. Chow RM, Lee RY, Rajput K. Peripheral nerve stimulation for pain management: a review. Curr Pain Headache Rep. 2023;27(9):321–327. doi:10.1007/s11916-023-01143-0
115. Deer TR, Esposito MF, McRoberts WP, et al. A systematic literature review of peripheral nerve stimulation therapies for the treatment of pain. Pain Med. 2020;21(8):1590–1603. doi:10.1093/pm/pnaa030
116. Xu J, Sun Z, Wu J, et al. Peripheral nerve stimulation in pain management: a systematic review. Pain Physician. 2021;24(2):E131–E152.
117. Pritzlaff SG, Latif U, Rosenow JM, et al. A review of prospective studies regarding percutaneous peripheral nerve stimulation treatment in the management of chronic pain. Pain Manag. 2024;14(4):209–222. doi:10.1080/17581869.2024.2352398
118. Ilfeld BM, Gabriel RA, Said ET, Monahan AM. Ultrasound-guided percutaneous peripheral nerve stimulation neuromodulation of the sciatic nerve for postoperative analgesia following ambulatory foot surgery, a proof-of-concept study. Reg Anesth Pain Med. 2018;43(6):580–589.
119. Kaye AD, Plaisance TR, Smith SA, et al. Peripheral nerve stimulation in postoperative analgesia: a narrative review. Curr Pain Headache Rep. 2024;28(7):691–698. doi:10.1007/s11916-024-01257-z
120. Ilfeld BM, Plunkett A, Vijjeswarapu AM, et al. Percutaneous neuromodulation of the brachial plexus and sciatic nerve for the treatment of acute pain following surgery: secondary outcomes from a multicenter, randomized, controlled pilot study. Neuromodulation. 2023;26(3):638–649. doi:10.1111/ner.13492
121. Gabriel RA, Ilfeld BM. Acute postoperative pain management with percutaneous peripheral nerve stimulation: the SPRINT neuromodulation system. Expert Rev Med Devices. 2021;18(2):145–150. doi:10.1080/17434440.2021.1877134
122. Gabriel RA, Swisher MW, Ilfeld BM. Percutaneous peripheral nerve stimulation for acute postoperative pain. Pain Manag. 2019;9(4):347–354. doi:10.2217/pmt-2018-0094
123. Castroman P, Quiroga O, Mayoral Rojals V, et al. Reimagining how we treat acute pain: a narrative review. Cureus. 2022;14(4):e23992. doi:10.7759/cureus.23992
124. Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL. Prescription opioid analgesics commonly unused after surgery: a systematic review. JAMA Surg. 2017;152(11):1066–1071. doi:10.1001/jamasurg.2017.0831
125. Merrill HM, Dean DM, Mottla JL, Neufeld SK, Cuttica DJ, Buchanan MM. Opioid consumption following foot and ankle surgery. Foot Ankle Int. 2018;39(6):649–656. doi:10.1177/1071100718757527
126. Horn JL, Pitsch T, Salinas F, Benninger B. Anatomic basis to the ultrasound-guided approach for saphenous nerve blockade. Reg Anesth Pain Med. 2009;34(5):486–489. doi:10.1097/AAP.0b013e3181ae11af
127. Hansen E, Eshelman MR, Cracchiolo A. Popliteal fossa neural blockade as the sole anesthetic technique for outpatient foot and ankle surgery. Foot Ankle Int. 2000;21(1):38–44. doi:10.1177/107110070002100107
128. Wagner ER, Farley KX, Higgins I, Wilson JM, Daly CA, Gottschalk MB. The incidence of shoulder arthroplasty: rise and future projections compared with hip and knee arthroplasty. J Shoulder Elbow Surg. 2020;29(12):2601–2609. doi:10.1016/j.jse.2020.03.049
129. Twomey-Kozak J, Adu-Kwarteng K, Lunn K, et al. Recent advances in the design and application of shoulder arthroplasty implant systems and their impact on clinical outcomes: a comprehensive review. Orthop Res Rev. 2024;16:205–220. doi:10.2147/ORR.S312870
130. Fossati C, Vitale M, Forin Valvecchi T, Gualtierotti R, Randelli PS. Management of painful shoulder arthroplasty: a narrative review. Pain Ther. 2020;9(2):427–439. doi:10.1007/s40122-020-00186-0
131. Compagnoni R, Gualtierotti R, Luceri F, Sciancalepore F, Randelli PS. Fibromyalgia and shoulder surgery: a systematic review and a critical appraisal of the literature. J Clin Med. 2019;8(10):1518. doi:10.3390/jcm8101518
132. Pierson CJ, Javed N, Jain NB, Konda C. Peripheral nerve stimulation of the axillary nerve improves chronic shoulder pain and dysfunction following reverse total shoulder arthroplasty: a case report. Am J Phys Med Rehabil. 2014. doi:10.1097/PHM.0000000000002582
133. Tantawy M, Hosam-Eldin A, Atallah A. Outcome of combined radiofrequency medial branch rhizotomy and steroid nerve block in lumbar facet arthropathy: a randomized controlled clinical trial. Med J Cairo Univer. 2022;90(12):2557–2563. doi:10.21608/mjcu.2022.295332
134. DePalma MJ, Ketchum JM, Saullo TR. Etiology of chronic low back pain in patients having undergone lumbar fusion. Pain Med. 2011;12(5):732–739. doi:10.1111/j.1526-4637.2011.01098.x
135. Shi W, Tian D, Liu D, Yin J, Huang Y. The comparison of measurement between ultrasound and computed tomography for abnormal degenerative facet joints: a STROBE-compliant article. Medicine. 2017;96(31):e7680. doi:10.1097/MD.0000000000007680
136. Tran J, Peng P, Loh E. Anatomical study of the medial branches of the lumbar dorsal rami: implications for image-guided intervention. Reg Anesth Pain Med. 2022;47(8):464–474. doi:10.1136/rapm-2022-103653
137. D’hooge R, Cagnie B, Crombez G, Vanderstraeten G, Dolphens M, Danneels L. Increased intramuscular fatty infiltration without differences in lumbar muscle cross-sectional area during remission of unilateral recurrent low back pain. Manual Ther. 2012;17(6):584–588. doi:10.1016/j.math.2012.06.007
138. Sheth SJ, Mauck WD, Russo DP, et al. Potential cost savings with 60-day peripheral nerve stimulation treatment in chronic axial low back pain. Pain Ther. 2024;13(5):1187–1202. doi:10.1007/s40122-024-00630-5
139. Kreiner DS, Matz P, Bono CM, et al. Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of low back pain. Spine J. 2020;20(7):998–1024. doi:10.1016/j.spinee.2020.04.006
140. Searle A, Spink M, Ho A, Chuter V. Exercise interventions for the treatment of chronic low back pain: a systematic review and meta-analysis of randomised controlled trials. Clin rehabilitat. 2015;29(12):1155–1167. doi:10.1177/0269215515570379
141. Leggett LE, Soril LJJ, Lorenzetti DL, et al. Radiofrequency ablation for chronic low back pain: a systematic review of randomized controlled trials. Pain Res Manag. 2014;19(5):e146–153. doi:10.1155/2014/834369
142. Wang F, Cheung CW, Wong SSC. Regenerative medicine for the treatment of chronic low back pain: a narrative review. J Int Med Res. 2023;51(2):3000605231155777. doi:10.1177/03000605231155777
143. Cohen S, Gilmore C, Kapural L, et al. Percutaneous peripheral nerve stimulation for pain reduction and improvements in functional outcomes in chronic low back pain. Mil Med. 2019;184(Suppl 1):537–541. doi:10.1093/milmed/usy310
144. GBD. 2017 disease and injury incidence and prevalence collaborators. global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1789–1858. doi:10.1016/S0140-6736(18)32279-7
145. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629–808. doi:10.1177/0333102413485658
146. Kollenburg L, Kurt E, Mulleners W, et al. Four decades of occipital nerve stimulation for headache disorders: a systematic review. Curr Pain Headache Rep. 2024;28(10):1015–1034. doi:10.1007/s11916-024-01271-1
147. Moman RN, Olatoye OO, Pingree MJ. Temporary, percutaneous peripheral nerve stimulation for refractory occipital neuralgia. Pain Med. 2022;23(2):415–420. doi:10.1093/pm/pnab128
148. Deuel D, Sandgren A, Nelson EO, et al. Conservative management of occipital neuralgia supported by physical therapy: a review of available research and mechanistic rationale to guide treatment. Curr Pain Headache Rep. 2024;28(12):1321–1331. doi:10.1007/s11916-024-01288-6
149. Gazelka HM, Knievel S, Mauck WD, et al. Incidence of neuropathic pain after radiofrequency denervation of the third occipital nerve. J Pain Res. 2014;195. doi:10.2147/JPR.S60925
150. Cadalso R, Daugherty J, Holmes C, Ram S, Enciso R. Efficacy of electrical stimulation of the occipital nerve in intractable primary headache disorders: a systematic review with meta-analyses. J Oral Facial Pain Headache. 2018;32(1):40–52. doi:10.11607/ofph.1784
151. Dodick DW, Silberstein SD, Reed KL, et al. Safety and efficacy of peripheral nerve stimulation of the occipital nerves for the management of chronic migraine: long-term results from a randomized, multicenter, double-blinded, controlled study. Cephalalgia. 2015;35(4):344–358. doi:10.1177/0333102414543331
152. Warner NS, Schaefer KK, Eldrige JS, et al. Peripheral nerve stimulation and clinical outcomes: a retrospective case series. Pain Pract. 2021;21(4):411–418. doi:10.1111/papr.12968
153. International Association for the Study of Pain (IASP). Taxonomy working group. classification of chronic pain. descriptions of chronic pain syndromes and definitions of pain terms. Available from: https://www.iasp-pain.org/publications/free-ebooks/classification-of-chronic-pain-second-edition-revised/.
154. Hurley RW, Adams MCB, Benzon HT. Neuropathic pain: treatment guidelines and updates. Curr Opinion Anaesthesiol. 2013;26(5):580–587. doi:10.1097/ACO.0b013e328363b4bf
155. Gabutti G, Serenelli C, Sarno O, Marconi S, Corazza M, Virgili A. Epidemiologic features of patients affected by herpes zoster: database analysis of the Ferrara University Dermatology Unit, Italy. Médecine et Maladies Infectieuses. 2010;40(5):268–272. doi:10.1016/j.medmal.2009.09.005
156. Zhang L, Rainka M, Freeman R, et al. A randomized, double-blind, placebo-controlled trial to assess the efficacy and safety of gabapentin enacarbil in subjects with neuropathic pain associated with postherpetic neuralgia (PXN110748). J Pain. 2013;14(6):590–603. doi:10.1016/j.jpain.2013.01.768
157. Ke M, Yinghui F, Yi J, et al. Efficacy of pulsed radiofrequency in the treatment of thoracic postherpetic neuralgia from the angulus costae: a randomized, double-blinded, controlled trial. Pain Physician. 2013;16(1):15–25.
158. Kulkantrakorn K, Lorsuwansiri C, Meesawatsom P. 0.025% capsaicin gel for the treatment of painful diabetic neuropathy: a randomized, double‐blind, crossover, placebo‐controlled trial. Pain Pract. 2013;13(6):497–503. doi:10.1111/papr.12013
159. Szok D, Tajti J, Nyári A, Vécsei L, Trojano L. Therapeutic approaches for peripheral and central neuropathic pain. Behav Neurol. 2019;2019:1–13. doi:10.1155/2019/8685954
160. West T, Hussain N, Bhatia A, et al. Pain intensity and opioid consumption after temporary and permanent peripheral nerve stimulation: a 2-year multicenter analysis. Reg Anesth Pain Med. 2024. doi:10.1136/rapm-2024-105704
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

