Back to Journals » Therapeutics and Clinical Risk Management » Volume 21
Construction and Validation of Risk Scoring Model for Inadequate Bowel Preparation in Elderly Patients Undergoing Colonoscopy
Authors Xu Y, Ou S, Yuan X, Yao J, Yang T
Received 28 October 2024
Accepted for publication 24 April 2025
Published 11 June 2025 Volume 2025:21 Pages 885—894
DOI https://doi.org/10.2147/TCRM.S503389
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Yun Xu, Shan Ou, Xiu Yuan, Jie Yao, Tianwen Yang
Department of Gastroenterology, The First Hospital Affiliated of Chongqing Medical and Pharmaceutical College, Chongqing, 400060, People’s Republic of China
Correspondence: Tianwen Yang, Email [email protected]
Objective: To establish a prediction model for the risk of inadequate bowel preparation for colonoscopy in the elderly, and to validate the model to test its prediction effect.
Methods: A total 927 patients who underwent colonoscopy in the First Affiliated Hospital to Chongqing Medical and Pharmaceutical College from January to December 2023 were selected as the modeling group, and were divided into the success group (839 patients) and failure group (88 patients) according to whether or not inadequate bowel preparation occurred, and then a logistic regression prediction model was established and transformed into a risk scoring system. The area under the ROC curve and the Hosmer-Lemeshow test were used for model differentiation and calibration, respectively, and the 10-fold cross-validation method was used for internal validation of the model. A total of 548 patients who underwent colonoscopy in our hospital from January to June 2024 were selected for external validation of the model.
Results: Logistic regression analysis showed that age ≥ 65 years, diabetes mellitus, exercise habits, Bristol stool characterization scale, frailty, and ambulatory functional status were independent factors influencing the inadequate bowel preparation for colonoscopy in the elderly. The area under the ROC curve for the modeling group was 0.806, and the Hosmer-Lemeshow test showed p=0.870. The area under the ROC curve of the validation group was (0.785± 0.090). The area under the ROC curve of the validation group was 0.824, and the Hosmer-Lemeshow test showed P=0.907, with a sensitivity of 73.13%, a specificity of 80.70%, and a Jordon’s index of 0.538.
Conclusion: The predictive model of the risk of inadequate bowel preparation for colonoscopy in elderly people can predict the risk of inadequate bowel preparation in elderly people, and can be used as a tool for clinical caregivers to screen the high-risk group of inadequate bowel preparation in the elderly.
Keywords: elderly, colonoscopy, inadequate bowel preparation, predictive modeling, risk score
China is a nation with a high incidence rate of colorectal cancer.1,2 Colonoscopy, regarded as the gold standard for colorectal cancer screening, has been extensively employed in clinical practice, and its operational safety and therapeutic efficacy are closely associated with the quality of bowel preparation.3,4 As the population of China keeps aging and life expectancy keeps rising, elderly individuals have emerged as a principal demographic for colorectal cancer screening, with colonoscopy attaining enhanced prevalence among those aged 65 and above.5,6 The incidence rate of inadequate bowel preparation among the elderly ranges from 34.6% to 65.0%.7 This not only elevates the pain and medical cost of secondary examinations but also gives rise to missed diagnoses of polyps and increases the chance of perforation or hemorrhage on repeat colonoscopy.8 Therefore, it is particularly important to screen and intervene early in elderly people who are at risk of inadequate bowel preparation. Currently, there are limitations in previous studies regarding the risk of inadequate bowel preparation in patients before colonoscopy, and no quality assessment tool for bowel preparation in older adults has been performed to the best of our knowledge. In this study, we will analyze the influencing factors of inadequate bowel preparation in the elderly, establish a risk prediction model, and validate the model internally and externally, in order to provide clinical caregivers with an effective tool for early identification of elderly patients with inadequate bowel preparation, and to provide theoretical guidance for prospective preventive studies.
Methods
Subjects
Elderly patients who underwent colonoscopy in our hospital from January 2022 to December 2023 were selected for modeling and validation, respectively. Inclusion criteria: (1) age ≥60 years old; (2) outpatients and inpatients who underwent colonoscopy; (3) informed consent. Exclusion criteria: (1) patients with emergency colonoscopy; (2) patients with severe cardiopulmonary diseases; (3) patients with unconsciousness and communication disorders; (4) patients with intestinal obstruction, intestinal perforation and intestinal stenosis. Eliminate criteria: (1) poor adherence to the bowel preparation program, which means that the patient’s adherence is judged to be poor if he/she has not taken the full dose of medication (less than 2L), taken the medication at the wrong time, or has not consumed one of the low residue/low fiber diets for 1d prior to the operation; (2) laxative followed by an enema as a remedial measure; (3) The colonoscopy was discontinued due to an obstructing mass or luminal narrowing caused by a stricture.; (4) incomplete or doubtful quality scores of bowel preparation; (5) poor adherence to the program. The study was approved by the Medical Ethics Committee of The First Affiliated Hospital to Chongqing Medical and Pharmaceutical College (No: 2022098).
In this study, 18 candidate factors were ultimately included through literature review,9–13 consultation with experts and professional judgment. Based on the literature review14 and the comments by local experts, we estimated the appropriate number of patients needed to allow a robust statistical evaluation. Because the rate of inadequate bowel preparation in the elderly is about 40%, and we included 18 variables in the study, we calculated the sample size to be 450 patients and then increased that number to 495 to account for an estimate of a 10% failure rate. In the external validation of the prediction model, the sample size was calculated based on the precision (ie, expected statistic, standard error, and event rate),15 and 60~170 outcome events were needed to obtain a better model precision, so the required sample size was at least 60/0.4=150 cases, and 165 cases were needed to be included to consider the 10% failure rate.
Methods
Research Tools
General Information and Clinical Data
A general information and clinical data questionnaire was self-designed, encompassing sex, age, body mass index, the number of bowel movements per week, the regularity of bowel movements, exercise habits, dietary preferences, the time of checkups, the history of abdominal surgeries, medical consultations (outpatient/inpatient), and comorbidities (chronic constipation, diabetes mellitus, hypertension, coronary heart disease, and cirrhosis of the liver).
The Bristol Stool Form Scale (BSFS)
The Bristol Stool Form Scale (BSFS) classifies stools into types 1 to 7 based on their consistency. The BSFS, which was developed and validated by Heaton et al16 is a visualization scale. The BSFS is categorized into types 1–7 in accordance with the nature of the stool and its continuity, and collects the types of stools excreted by the patient in the past 7 days. Types 1 and 2 in the BSFS are constipated stools, types 3–5 are normal stools, and types 6 and 7 are diarrheal stools. The scale demonstrated good reliability and validity, with a Cronbach’s alpha coefficient of 0.76.
Frailty Screening Inventory (FRAIL)
FRAIL consists of 5 items: fatigue, resistance, decreased free movement, coexistence of multiple illnesses, and weight loss. 3 or more of the 5 items are considered to be frail; 1 or 2 are considered to be in the pre-frail stage; and 0 are considered to be non-frail. Domestic scholars conducted reliability and validity studies on the FRAIL scale, and all of them indicated that the scale had good reliability and validity, with a Cronbach′s α coefficient of 0.826.17
Holen Walking Function Scale
Holen Walking Function Scale is used to assess the walking function of patients, which is graded from 0 to V. Grade 0 to III is poor walking function, and grade IV and V is normal walking function.
Barthel Index
The Barthel Index evaluates functional independence through 10 activities of daily living, with each item scored ordinally based on performance level (0, 5, 10, or 15 points). The scoring criteria are as follows:
(1) Feeding: 10 = Independent (can use utensils, no assistance needed), 5 = Needs help (eg, cutting food, setup), 0 = Unable (full dependence); (2) Bathing: 5 = Independent (can wash entire body), 0 = Needs assistance (partial or full help); (3) Grooming: 5 = Independent (brushing teeth, hair, shaving), 0 = Needs assistance; (4) Dressing: 10 = Independent (including buttons, zippers); 5 = Needs help (eg, with fasteners), 0 = Unable (full dependence); (5) Toileting: 10 = Independent (transfers, cleaning, clothing), 5 = Needs help (balance, wiping), 0 = Unable (full assistance); (6) Bowel Control, 10 = Full control (no accidents), 5 = Occasional accidents (<1/week), 0 = Incontinent or requires enema/catheter. (7) Bladder Control: 10 = Full control (or managed independently), 5 = Occasional accidents (<1/day), 0 = Incontinent or catheter-dependent; (8) Ambulation (Walking 50+ meters): 15 = Independent (no aids); 10 = Uses cane/walker, 5 = Needs supervision (unsteady), 0 = Non-ambulatory (or <50m); (9) Chair/Bed Transfers: 15 = Independent (no physical help), 10 = Minor help (eg, verbal cues), 5 = Needs one-person assist, 0 = Unable (two-person lift or hoist); (10) Stair Climbing: 10 = Independent (no rails or with rails), 5 = Needs help/supervision, 0 = Unable. Total Score Interpretation: ≤40 = Severe dependence; 41–60 = Moderate dependence; 61–99 = Mild dependence; 100 = Fully independent. The scale demonstrates good reliability (Cronbach’s α = 0.88).
Bowel Preparation Regimen
All patients received standardized bowel preparation according to the Chinese guideline for bowel preparation for colonoscopy (2019, Shanghai).18 A low-fiber diet was initiated 3 days prior to colonoscopy, transitioning to a clear liquid diet 1 day before the procedure. The bowel preparation regimen consisted of oral administration of 2L polyethylene glycol electrolyte solution (PEG-ELS, Wanhe, Shenzhen Wanhe Pharmaceutical Co., Ltd.) starting 6–8 hours before colonoscopy, with 250 mL consumed every 15 minutes until completion. Patients were encouraged to drink ≥500 mL of additional clear fluids during preparation and maintained a clear liquid diet until the procedure. Enemas were not routinely administered unless inadequate preparation was observed. All patients received both written and verbal instructions, and nursing staff monitored preparation quality through patient interviews and documentation.
Bowel Preparation Quality Evaluation Indexes
In this study, the internationally recognized Boston Bowel Preparation Scale (BBPS) was used to evaluate the quality of patients’ bowel preparation.19 The BBPS assesses bowel cleanliness by dividing the colon into three anatomical segments (right colon, transverse colon, and left colon), with each segment scored from 0 to 3 based on mucosal visualization: 0 = unprepared colon with mucosa not visible due to solid stool; 1 = portion of mucosa visible but other areas obscured by staining, residual stool, or opaque fluid; 2 = minor amount of residual staining, small fragments of stool, and/or opaque fluid but mucosa clearly visible; 3 = entire mucosa clearly visible with no residual staining, small fragments of stool, or opaque fluid. The total BBPS score ranges from 0 to 9 by summing the scores of all three segments.
Definition of outcome variables: inadequate bowel preparation in this study was defined as a total BBPS score of <6 for all bowel segments or <2 for any one bowel segment. To ensure the objectivity of the evaluation results, the scoring was performed by a clinically experienced endoscopist and a nurse with 3 years of experience in gastrointestinal endoscopy nursing, both of whom had participated in the departmental BBPS scoring training and demonstrated proficiency in the scoring method through standardized testing.
Data Collection Methods
Firstly, signing the informed consent form after obtaining the patient’s consent at the time of appointment, collecting information by face-to-face questioning, and all questionnaires were collected by the researcher herself. Secondly, on the day of consultation and examination, patients were asked about their medication and dietary adherence, and some patients with poor adherence were excluded. After the data were collected, the researcher conducted a comprehensive and detailed check to confirm the missing or inaccurate information in the questionnaire.
Statistical Methods
The collected data were double-checked and entered into Excel software to ensure data accuracy. SPSS25.0, R4.1.1 statistical software was used for statistical analysis, the quantitative data of normal distribution were expressed as mean ± standard deviation ( ); qualitative data were expressed as frequency and percentage. According to the results of univariate analysis, variables with P<0.05 were included in logistic regression analysis to establish risk prediction models. The area under the curve of subjects’ work characteristics (ROC) and the Hosmer-Lemeshow test (H-L test) were used to evaluate the discrimination and calibration of the model. The predictive model was internally validated in the modeling group using the 10-fold cross-validation method, and externally validated in the validation group for the time period.
); qualitative data were expressed as frequency and percentage. According to the results of univariate analysis, variables with P<0.05 were included in logistic regression analysis to establish risk prediction models. The area under the curve of subjects’ work characteristics (ROC) and the Hosmer-Lemeshow test (H-L test) were used to evaluate the discrimination and calibration of the model. The predictive model was internally validated in the modeling group using the 10-fold cross-validation method, and externally validated in the validation group for the time period.
Results
General Information of the Study Population
A total of 927 patients were included in the modeling group, and the incidence of inadequate bowel preparation was 9.49% (88/927), among which 454 (48.96%) were male and 473 (51.04%) were female; the age was (65.42 ± 8.37) years. In the validation group, a total of 528 patients were incorporated, and the incidence of inadequate bowel preparation was 9.28% (49/528), among which 275 (52.08%) were males and 253 (47.92%) were females; the age was (67.25 ± 5.97) years.
Univariate Analysis of Predictors of Risk for Inadequate Bowel Preparation for Colonoscopy in the Elderly
This study used optimal cutoff point analysis to convert age into a categorical variable, which facilitated the establishment of a risk scoring system. The results of the univariate analysis are shown in Table 1.
 |
Table 1 Univariate Analysis of Predictive Factors for Inadequate Bowel Preparation in Elderly Patients Undergoing Colonoscopy |
Multifactorial Analysis of Predictors of Risk of Inadequate Bowel Preparation for Colonoscopy in the Elderly
Logistic regression analyses were performed with whether the patient experienced the inadequate bowel preparation as the dependent variable and variables that were statistically significant in the univariate analyses as independent variables, with a variance inflation factor of <5 and a tolerance value of >0.1 for each of the independent variables, and no multicollinearity between variables. Assignment of Independent Variables: Age ≥65 years, No=0, Yes=1; Diabetes mellitus, No=0, Yes=1; Exercise habit (Dummy variable in the model, Always exercise as reference): Occasionally (1, 0), never (0, 1); BSFS type (Dummy variable in the model, BSFS type 3–5 as reference), BSFS type 6–7 (1, 0), BSFS type 1–2 (0, 1); Frailty (Dummy variable in the model, No Frailty as reference). The results showed that age ≥65 years, diabetes, exercise habits, BSFS type 1 or 2, frailty, and poor walking function were independent risk factors for inadequate bowel preparation in colonoscopy in the elderly, while BSFS type 6–7 was a protective factor for inadequate bowel preparation, as shown in Table 2.
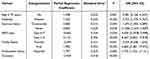 |
Table 2 Results of Logistic Regression Analysis on Predictive Factors for Inadequate Bowel Preparation in Elderly Patients Undergoing Colonoscopy |
Predictive Modeling of the Risk of Failed Bowel Preparation for Colonoscopy in the Elderly
Regression equations were constructed based on logistic regression analysis: Logit(P) = −4.128 + 1.335 × Age ≥65 + 1.012 × Diabetes + Exercise habits (0.545 × Occasionally + 0.724 × never) + BSFS types (−0.664×Type 6–7 + 2.116× type 1–2) + 1.934 × Frailty + 1.7587 × poor walking function. Referring to the logistic scoring method, the risk prediction model was converted into a risk scoring system. The smallest partial regression coefficient (0.584) in the logistic regression equation was taken as the base and assigned a score of 1. The remaining variables were assigned scores as the integer part obtained by dividing the partial regression coefficients of each independent variable by the smallest partial regression coefficient, with the scores ranging from −1 to 15, and the specific scores are presented in Table 3. The optimal cut-off value of the scoring system was 3, and at this time, the model sensitivity was 61.83%, the specificity was 85.11%, and the Jordon’s index was 85.11%. The optimal cut-off value of the scoring system was 3, and the sensitivity of the model was 61.83%, the specificity was 85.11%, the Jordon’s index was 0.469, the positive predictive value was 59.1%, and the negative predictive value was 86.5%.
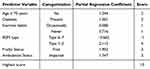 |
Table 3 Risk Prediction Scoring System for Inadequate Bowel Preparation Before Colonoscopy in Elderly Patients |
Validation of the Risk Prediction Model for Inadequate Bowel Preparation in Colonoscopy in the Elderly
The area under the ROC curve of the risk prediction model in the modeling group was 0.806 [0.760, 0.852], P < 0.001. See Figure 1. The H-L test result was P = 0.870. In the modeling group, a 10-fold cross-sectional validation was conducted for internal validation of the model. The results show that the average performance of the multi-factor logistic regression model in this study on the validation set, namely, the area under the ROC curve is (0.785 ± 0.090). The validation group carried out the time period external validation of the model. The results showed that the area under the ROC curve was 0.824 [0.760, 0.887], P < 0.001. See Figure 2. The H-L test result was P = 0.907. The model sensitivity was 73.13%, the specificity was 80.70%, the Youden index was 0.538, and the positive predictive value was 59.75% and the negative predictive value was 88.46%.
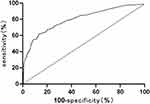 |
Figure 1 ROC curve of the modeling group risk prediction model group. |
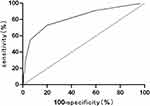 |
Figure 2 ROC curve of the risk prediction model for the validation group. |
Discussion
The results of this study showed that the risk of inadequate bowel preparation in patients aged ≥65 years was 3.581 times higher than that in patients 60–65 years, which is consistent with the results of the study conducted by Seinelä et al.20 The risk of inadequate bowel preparation multiplies with increasing age.21 The quality of bowel preparation in the elderly is related to their functional status and co-morbidities. With age, especially in the elderly, aging leads to functional decline, decreased skeletal muscle strength, decreased mobility, and slower gastrointestinal motility, all of which increase the risk of inadequate bowel preparation. Therefore, it is suggested that medical personnel should pay attention to the bowel preparation situation of the elderly and give predictive intervention strategies. For elderly patients aged ≥65 years, healthcare professionals should utilize diversified health education methods, and require family members to accompany them to help the elderly take medications correctly and improve bowel preparation adherence.
Diabetes mellitus is more recognized as an independent predictor of inadequate bowel preparation in national and international studies. The results of this study showed that the risk of inadequate bowel preparation in diabetic patients was 2.733 times higher than that in patients without diabetes, which is consistent with the results of a previous study.22 It has been suggested that diabetes causes changes in the enteric nervous system and enterocyte microenvironment, leading to oxidation and apoptosis of gastrointestinal cells, triggering damage to gastrointestinal neurons, resulting in impaired gastric emptying and delayed intestinal functioning. When diabetic patients take laxatives, the transmission of laxatives in the gastrointestinal tract is delayed compared with that of normal patients, thus affecting the quality of intestinal preparation. In addition, diabetic patients are prone to hypoglycemia, electrolyte disorders and other accidents during bowel preparation. Therefore, for elderly diabetic patients, healthcare providers should offer tailored dietary and hypoglycemic medication guidance, arrange optimal examination schedules to reduce waiting time, instruct patients to prepare oral rock candy as a precaution against hypoglycemia during the waiting period, and develop individualized bowel preparation protocols.
The results of this study showed that the risk of inadequate bowel preparation in elderly people who never or occasionally exercised was 2.128 or 1.675 times higher than that of patients who exercised regularly. This may be related to changes in secretion of digestive glands and gastrointestinal hormones, as well as enhanced gastrointestinal motility and transit, which could facilitate the effects of the laxative—though this remains speculative without further evidence, Kim et al23 also suggested that regular aerobic exercise increases the rate of intestinal peristalsis, and may promote the effect of polyethylene glycol electrolyte spreading (PEG-ELS) to enhance the quality of intestinal preparation in patients. quality of bowel preparation.
The results of this study showed that BSFS type 1 or 2 can be used as a predictor of inadequate bowel preparation in patients, and the risk of inadequate bowel preparation in patients with BSFS type 1 or 2 (constipated) was 8.267 times higher than that in patients with type 3–5 (normal), which is consistent with the results of the study conducted by Manes et al.24 The reason for this is that patients with constipation have a slow colonic transport speed, which increases the risk of inadequate bowel preparation. Therefore, clinicians can learn the BSFS type of patients before colonoscopy and provide additional interventions for patients with type 1 or 2 constipation, including: (1) extended bowel preparation duration with additional laxatives, (2) dietary modifications with increased fluid intake, and (3) prokinetic agent administration when necessary. In addition, BSFS type 6 or 7 (diarrhea) was found to be a protective factor against inadequate bowel preparation, suggesting that patients with diarrhea may have better quality bowel preparation. However, it is also important to consider whether diarrhea patients tolerate high volume laxatives well, and healthcare professionals should be aware of the need to assess the incidence of nausea, vomiting, and other adverse effects in patients.
With the rapid development of China’s aging population, the number of elderly people undergoing colonoscopy is increasing. The results of this study suggest that frailty is an independent risk factor for inadequate bowel preparation in elderly patients, and the risk of inadequate bowel preparation in a frail patient is 6.682 times higher than that in a non-frail patient. This may be due to the decreased gastrointestinal motility and delayed excretion of laxatives in the elderly due to inactivity, which increases the risk of inadequate bowel preparation. Therefore, additional promotional measures, such as exercise interventions during medication administration, can be added to bowel preparation for the frail elderly.
The findings of this study reveal that elderly patients with ambulatory difficulties face a 5.735 times higher risk of bowel preparation failure compared to those with normal walking function. This elevated risk may be attributed to the fact that mobility-impaired elderly patients often develop apprehension about frequent defecation after taking laxatives due to their inability to access toilet facilities independently, which subsequently discourages adequate consumption of high-volume purgatives and ultimately compromises bowel preparation quality. For such patients with walking difficulties, healthcare providers should implement fall prevention measures during repeated toilet visits by recommending family accompaniment and providing bedside commodes. Under safe conditions, caregivers can further assist patients with appropriate ambulation or positional adjustments during medication administration to enhance laxative efficacy.
From the perspective of model differentiation, the model is well differentiated in the 10-fold cross-validation and external validation, indicating that the model has a certain degree of internal stability and extrapolation. From the calibration of the model, the p-value of the H-L test in both the risk prediction model and the external validation of the model was greater than 0.05, indicating that there was no significant difference between the model prediction of inadequate bowel preparation and the actual occurrence of inadequate bowel preparation, and that the model prediction had good consistency. It can be seen that the model has good predictive performance through rigorous internal and external validation, the construction methodology is rigorous, and the model has a certain degree of scientific validity. Second, the transformation of the prediction model into a risk scoring system improved the clinical operability of the model. In the model development cohort, when the score is ≥3, the high-risk group, the sensitivity of the model is 61.83%, and the specificity is 85.11%. The model maintains the effective sensitivity while the specificity is high, which can effectively reduce the misjudgement and avoid the waste of medical resources. In the validation cohort, the model still maintained good sensitivity and specificity. The risk scoring system for colonoscopy preparation failure in the elderly is simple and quick to use, and it can help healthcare professionals to effectively screen out the high-risk groups of possible inadequate bowel preparation, and give prospective preventive measures to improve the quality of bowel preparation in the elderly.
When contextualizing our findings within real-world clinical practice, several implementation considerations emerge. First, our risk scoring system’s components (Bristol stool scale, ambulatory status, etc) align with parameters routinely documented in electronic health records, enabling seamless integration into clinical workflows without additional data collection – a critical advantage confirmed by similar implementation studies.13 Second, the model’s moderate sensitivity (73.1%) and high specificity (80.7%) strategically balance clinical priorities: minimizing unnecessary interventions while effectively identifying high-risk patients, a pragmatic approach validated in real-world colonoscopy quality improvement programs. Notably, our frailty assessment protocol using routine clinical parameters differs from research-grade tools like Fried’s criteria, but this simplification enhances real-world applicability – a strategy successfully employed in emergency department risk stratification systems. Future implementation should monitor two real-world metrics: 1) Nurse compliance with scoring documentation (target >85%), and 2) Time-from-scoring-to-intervention (<2hrs), both identified as critical success factors in pragmatic trials of bowel prep optimization (NCT03945773).
While this study provides valuable insights into risk factors for inadequate bowel preparation in elderly patients (≥60 years), several limitations should be acknowledged. First, our focus on this age group, though justified by their higher incidence of inadequate preparation and unique geriatric risk factors (eg, frailty, polypharmacy), precludes direct comparisons with younger cohorts (eg, 40–59 years). Future studies should expand the age spectrum to evaluate whether similar or distinct risk factors apply across younger age groups, particularly given reports of inadequate preparation in middle-aged populations. Second, our single-center design and modest sample size may limit generalizability. Multicenter studies with larger, age-diverse cohorts are needed to validate and refine our risk prediction model. Finally, while we identified actionable risk factors (eg, frailty, ambulatory difficulty), real-world implementation of interventions (eg, exercise protocols, tailored laxative regimens) warrants further investigation in broader clinical settings. These limitations highlight opportunities for future research to optimize bowel preparation strategies across all at-risk age groups. Also, Future iterations should incorporate validated neurological/nephrological assessment tools to capture these clinically significant covariates.
The risk prediction model constructed in this study has good predictive efficacy, is easy to use, and is highly operable, which can provide a reference for the risk assessment and early intervention prevention of inadequate bowel preparation in colonoscopy in the elderly. However, the data collection in this study is limited to this unit, and the sample size is small. In the future, we need to apply the model to multi-center institutions, carry out external spatial validation of the model, and test the extrapolation of the model to further improve and optimize the model.
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Medical Ethics Committee of The First Affiliated Hospital to Chongqing Medical and Pharmaceutical College (No: 2022098). Informed consent was acquired from each patient.
Funding
This work was supported by the Chongqing Municipal Science and Health Joint Medical Research General Project 2022 [Grant Number 2022MSXM130].
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Wang Z, Dan W, Zhang N, Fang J, Yang Y. Colorectal cancer and gut microbiota studies in China. Gut Microbes. 2023;15(1):2236364. doi:10.1080/19490976.2023.2236364
2. Qu R, Ma Y, Zhang Z, Fu W. Increasing burden of colorectal cancer in China. Lancet Gastroenterol Hepatol. 2022;7(8):700. doi:10.1016/S2468-1253(22)00156-X
3. Kastenberg D, Bertiger G, Brogadir S. Bowel preparation quality scales for colonoscopy. World J Gastroenterol. 2018;24(26):2833–2843. doi:10.3748/wjg.v24.i26.2833
4. Mahadeva S. Improving adherence towards bowel preparation for colonoscopy. JGH Open. 2023;7(9):597–598. doi:10.1002/jgh3.12975
5. Kim SY, Kim HS, Park HJ. Adverse events related to colonoscopy: global trends and future challenges. World J Gastroenterol. 2019;25(2):190–204. doi:10.3748/wjg.v25.i2.190
6. Hashimoto Y, Kuribayashi S, Itoi Y, et al. Safety of full bowel preparation and colonoscopy in elderly patients with ulcerative colitis: a real-world multicenter retrospective cohort study. DEN Open. 2024;4(1):e275. doi:10.1002/deo2.275
7. Cheng Y, Zhong C, Wu W, et al. Association between anxiety, depression, and bowel air bubbles at colonoscopy: a prospective observational study. Ann Palliat Med. 2021;10(3):3247–3257. doi:10.21037/apm-21-540
8. Zhang N, Xu M, Chen X. Establishment of a risk prediction model for bowel preparation failure prior to colonoscopy. BMC Cancer. 2024;24(1):341. doi:10.1186/s12885-024-12081-4
9. Shahini E, Sinagra E, Vitello A, et al. Factors affecting the quality of bowel preparation for colonoscopy in hard-to-prepare patients: evidence from the literature. World J Gastroenterol. 2023;29(11):1685–1707. doi:10.3748/wjg.v29.i11.1685
10. Feng L, Guan J, Dong R, et al. Risk factors for inadequate bowel preparation before colonoscopy: a meta-analysis. J Evid Based Med. 2024;17(2):341–350. doi:10.1111/jebm.12607
11. Beran A, Aboursheid T, Ali AH, et al. Risk factors for inadequate bowel preparation in colonoscopy: a comprehensive systematic review and meta-analysis. Am J Gastroenterol. 2024;119(12):2389–2397. doi:10.14309/ajg.0000000000003073
12. Mahmood S, Farooqui SM, Madhoun MF. Predictors of inadequate bowel preparation for colonoscopy: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2018;30(8):819–826. doi:10.1097/MEG.0000000000001175
13. Zhang Y, Wang L, Wu W, et al. Predictors of inadequate bowel preparation in older patients undergoing colonoscopy: a systematic review and meta-analysis. Int J Nurs Stud. 2024;149:104631. doi:10.1016/j.ijnurstu.2023.104631
14. Ogundimu EO, Altman DG, Collins GS. Adequate sample size for developing prediction models is not simply related to events per variable. J Clin Epidemiol. 2016;76:175–182. doi:10.1016/j.jclinepi.2016.02.031
15. Pavlou M, Qu C, Omar RZ, et al. Estimation of required sample size for external validation of risk models for binary outcomes. Stat Methods Med Res. 2021;30(10):2187–2206. doi:10.1177/09622802211007522
16. Heaton KW, Ghosh S, Braddon FE. How bad are the symptoms and bowel dysfunction of patients with the irritable bowel syndrome? A prospective, controlled study with emphasis on stool form. Gut. 1991;32(1):73–79. doi:10.1136/gut.32.1.73
17. Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16(7):601–608. doi:10.1007/s12603-012-0084-2
18. Digestive Endoscopy Special Committee of Endoscopic, Physicians Branch of Chinese Medical Association, et al. [Chinese guideline for bowel preparation for colonoscopy (2019, Shanghai)]. Zhonghua nei ke za zhi. 2019;58(7):485–495. doi:10.3760/cma.j.issn.0578-1426.2019.07.002
19. Calderwood AH, Jacobson BC. Comprehensive validation of the Boston Bowel Preparation Scale. Gastrointest Endosc. 2010;72(4):686–692. doi:10.1016/j.gie.2010.06.068
20. Seinelä L, Pehkonen E, Laasanen T, Ahvenainen J. Bowel preparation for colonoscopy in very old patients: a randomized prospective trial comparing oral sodium phosphate and polyethylene glycol electrolyte lavage solution. Scand J Gastroenterol. 2003;38(2):216–220. doi:10.1080/00365520310000726
21. Ray-Offor E, Jebbin N. Risk factors for inadequate bowel preparation during colonoscopy in Nigerian patients. Cureus. 2021;13(8):e17145. doi:10.7759/cureus.17145
22. Fuccio L, Frazzoni L, Spada C, et al. Factors that affect adequacy of colon cleansing for colonoscopy in hospitalized patients. Clin Gastroenterol Hepatol. 2021;19(2):339–348.e7. doi:10.1016/j.cgh.2020.02.055
23. Kim YS, Song BK, Oh JS, Woo SS. Aerobic exercise improves gastrointestinal motility in psychiatric inpatients. World J Gastroenterol. 2014;20(30):10577–10584. doi:10.3748/wjg.v20.i30.10577
24. Manes G, Repici A, Hassan C. Randomized controlled trial comparing efficacy and acceptability of split- and standard-dose sodium picosulfate plus magnesium citrate for bowel cleansing prior to colonoscopy. Endoscopy. 2014;46(8):662–669. doi:10.1055/s-0034-1365800
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Enhancing Colonoscopy Preparation in Elderly Constipation Patients: A Personalized Approach with PEG and Exercise - A Case Study
Zhang L, Huang L, Liu S, Sun X
International Medical Case Reports Journal 2024, 17:341-346
Published Date: 15 April 2024

