Back to Journals » Research Reports in Clinical Cardiology » Volume 15
Construction of a Column Chart Prediction Model for the Risk of Left Ventricular Thrombosis After PCI in Patients with Acute ST Segment Elevation Myocardial Infarction
Authors Bai X, Luo A, Liu Q, Ma X
Received 29 March 2024
Accepted for publication 18 September 2024
Published 24 September 2024 Volume 2024:15 Pages 63—73
DOI https://doi.org/10.2147/RRCC.S471428
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Kones
Xianglian Bai,1 Aiwu Luo,2 Qin Liu,1 Xiaofeng Ma1
1The Affiliated Nanhua Hospital, Department of Cardiology, Hengyang Medical School, University of South China, Hengyang City, Hunan Province, 421001, People’s Republic of China; 2Department of Health Education, Hengyang Center for Disease Control and Prevention, Hengyang City, 421002, People’s Republic of China
Correspondence: Xiaofeng Ma, The Affiliated Nanhua Hospital, Department of Cardiology, Hengyang Medical School, University of South China, Dongfeng Street, Zhuhui District, Hengyang City, Hunan Province, People’s Republic of China, Tel + 8613786437543, Email [email protected]
Objective: To explore the influencing factors of left ventricular thrombosis after percutaneous coronary intervention (PCI) in patients with acute ST segment elevation myocardial infarction (STEMI) and construct a column chart model.
Methods: A retrospective study was conducted on 331 STEMI patients who underwent PCI between July 2020 and January 2024. According to the principle of approximately 3:1, patients were randomly separated into 245 in the modeling group and 86 in the validation group, and clinical data of patients were collected. Multivariate logistic regression was applied to screen for risk factors. R software was applied to draw column charts. Bootstrap method was applied for internal validation. Hosmer-Lemeshow (H-L) was applied to test the fitting degree of the column chart model. Calibration curve and ROC curve were applied to verify calibration and discrimination, respectively. DCA curve was applied to analyze the clinical practicality of the column chart model.
Results: A history of angina pectoris, ventricular aneurysm, alcohol abuse, postoperative TIMI grade ≤ 2, LVEF, and total ischemic time were influencing factors for left ventricular thrombosis in STEMI patients after PCI (P< 0.05). The predicted probabilities of the internal and external validation calibration curves were highly consistent with the actual probabilities, the concordance index of the ROC curve was 0.962 (95% CI: 0.931– 0.994) and 0.958 (95% CI: 0.926– 0.990), respectively, indicating high model calibration and discrimination; H-L inspection showed χ2=11.977, 9.757 (P=0.152, 0.282). DCA curve showed that when the probability range of the high-risk threshold was 0.02~0.99, the column chart model performed better and had a higher net return.
Conclusion: The column chart model constructed by risk factors such as history of angina, ventricular aneurysm, history of alcohol abuse, postoperative TIMI ≤ grade 2, LVEF, and total ischemic time has high predictive value and can effectively predict left ventricular thrombosis in STEMI patients after PCI.
Keywords: acute ST-segment elevation myocardial infarction, percutaneous coronary intervention, left ventricular thrombosis, influencing factors, column chart
Introduction
Acute ST-segment elevation myocardial infarction (STEMI) is a disease with high incidence and mortality rates, and its incidence has been continuously rising in recent years, posing a serious threat to human life and health.1 Despite improvements in the survival rate of STEMI patients due to percutaneous coronary intervention (PCI) and antiplatelet therapy over the past 20 years, post-infarction complications remain a significant cause of high mortality and morbidity.2,3 The formation of left ventricular thrombus is one of the common complications of STEMI, with an incidence as high as 46%. Although surgical treatments have improved the situation, the severity remains concerning. If not treated promptly, it can lead to embolism and sudden death, increasing the total hospital stay and healthcare resource usage, thereby adding to the social, economic, and medical burden.4,5 Although there are many studies on the risk factors of left ventricular thrombus in STEMI patients, the results vary and need further evaluation.6,7 Currently, there is insufficient clinical evidence for the prevention of left ventricular thrombosis after PCI in STEMI patients, and it is imperative to develop effective strategies for its prevention. Nomograms are visual risk prediction tools constructed based on influencing factors. They integrate high-risk factors into the model and effectively predict the risk of disease occurrence for patients according to the weight of different factors. They have been widely used in clinical practice. For example, Li et al8 developed and validated a nomogram for predicting the risk of left atrial thrombus in patients with non-valvular atrial fibrillation. However, there is still a lack of risk prediction models specifically for left ventricular thrombus in STEMI patients. Therefore, this study conducts a logistic regression analysis on the occurrence and risk factors of left ventricular thrombosis after PCI in STEMI patients, constructs a nomogram model, aiming to provide a reference for high-quality research on the prevention and treatment of left ventricular thrombosis.
Subjects and Methods
Subjects
Compared to the incidence of left ventricular thrombus in STEMI patients reported in previous literature, with 1-α set at 0.95 and β at 0.1, sample size calculation was performed using PASS 15.0 software. The results indicate that at least 264 samples are required for this study. Accounting for a follow-up loss rate of 15%, the final sample size needed is 304 cases.A retrospective selection of 331 STEMI(The infarct locations are all in the left ventricular lateral wall, corresponding to the area supplied by the left circumflex artery) patients who underwent PCI from July 2020 to January 2024 was made as the study subjects, randomly divided into a modeling group of 245 patients and a validation group of 86 patients, following an approximate 3:1 ratio. Simultaneously, the modeling group was divided into two subgroups based on the presence of left ventricular thrombus: 182 cases in the non-left ventricular thrombus group and 63 cases in the left ventricular thrombus group.
Inclusion criteria: ① Patients conforming to the diagnostic and treatment standards,9 confirmed by clinical, imaging, and laboratory examinations, and all patients with left ventricular thrombus were found to have thrombus through transthoracic echocardiography.; ② Age ≥18 years, with detailed and complete data without any loss; ③ Patients admitted within 12 hours of onset for PCI treatment; ④ The study has been approved by the hospital’s ethics committee. Exclusion criteria: ① Patients with cardiovascular diseases such as dilated cardiomyopathy, hypertrophic cardiomyopathy, rheumatic heart disease, myocarditis, or pulmonary heart disease; ② Patients with contraindications for antiplatelet or anticoagulant therapy; ③ Patients with autoimmune diseases, blood disorders, or liver/kidney dysfunction; ④ Patients with a history of venous thrombosis; ⑤ Pregnant or breastfeeding women; ⑥ Patients who had major trauma or surgery within the last 3 months. See Figure 1 for the case collection flow chart.
 |
Figure 1 Case Collection Process Diagram. |
Collection of Clinical Data
Review the patients’ outpatient and inpatient records to collect their clinical data.The clinical data of the patients included gender, age, body mass index (BMI), systolic blood pressure, diastolic blood pressure, history of angina, old MI, ventricular aneurysm, smoking history, alcohol abuse history, chronic underlying diseases (hypertension, diabetes, hyperlipidemia), preoperative TIMI grade 0, postoperative TIMI grade ≤2, single-vessel disease, no collateral circulation, white blood cell count, creatinine, low-density lipoprotein cholesterol (LDL-C), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), total cholesterol (TC), peak cardiac troponin I (cTnI), peak creatine kinase-MB (CK-MB), blood potassium, left ventricular ejection fraction (LVEF), adjunct medications [statins, β-blockers, low molecular weight heparins, angiotensin-converting enzyme inhibitors (ACEI)], ≥4 leads ST-segment elevation, total ischemia time, mitral regurgitation, and pericardial effusion.
Statistical Analysis
Data processing was performed using IBM-SPSS 25.0 software. Continuous data (±) were analyzed using the independent sample t-test; categorical data [n (%)] were analyzed using the χ2 test. Multifactorial logistic regression analysis was used to screen for risk factors of left ventricular thrombus formation after PCI in STEMI patients. R 4.3.3 software was used to create nomograms for visualizing the results of the logistic regression analysis. Internal validation was conducted using the Bootstrap method (with 100 resamples), and the Hosmer-Lemeshow (H-L) test assessed the fit of the nomogram model. Calibration curves and ROC curves were used to verify the calibration and discriminative ability, respectively. Decision Curve Analysis (DCA) was employed to assess the clinical utility of the nomogram model. A P-value of <0.05 was considered statistically significant.
Results
Comparison of Demographic and Disease-Related Data Between the Modeling and Validation Groups
No significant differences were found between the modeling and validation groups in terms of gender, age, BMI, systolic blood pressure, diastolic blood pressure, history of angina, old MI, ventricular aneurysm, smoking history, alcohol abuse history, chronic underlying diseases (hypertension, diabetes, hyperlipidemia), preoperative TIMI grade 0, postoperative TIMI grade ≤2, single-vessel disease, no collateral circulation, white blood cell count, creatinine, LDL-C, TG, HDL-C, TC, peak cTnI, peak CK-MB, blood potassium, LVEF, adjunct medications (statins, β-blockers, low molecular weight heparins, ACEI), ≥4 leads ST-segment elevation, total ischemia time, mitral regurgitation, and pericardial effusion (P>0.05). See Table 1.
 |
Table 1 Comparison of Demographic and Disease Related Data Between the Modeling and Validation Groups[( |
Screening for Risk Factors of Left Ventricular Thrombus Formation After PCI in STEMI Patients in the Modeling Group
No significant differences were found between the non-left ventricular thrombus group and the left ventricular thrombus group in gender, age, BMI, systolic blood pressure, diastolic blood pressure, old MI, smoking history, chronic underlying diseases (hypertension, diabetes, hyperlipidemia), preoperative TIMI grade 0, single-vessel disease, no collateral circulation, white blood cell count, creatinine, LDL-C, TG, HDL-C, TC, peak cTnI, peak CK-MB, blood potassium, adjunct medications (statins, β-blockers, low molecular weight heparins, ACEI), ≥4 leads ST-segment elevation, mitral regurgitation, and pericardial effusion (P>0.05). The left ventricular thrombus group had a higher incidence of angina history, ventricular aneurysm, alcohol abuse history, postoperative TIMI grade ≤2, and total ischemia time, and a lower LVEF than the non-left ventricular thrombus group (P<0.05). See Table 2.
 |
Table 2 Screening of Risk Factors for Left Ventricular Thrombosis After PCI in Modeling Group STEMI Patients[( |
Multifactorial Logistic Regression Analysis of Left Ventricular Thrombus Formation After PCI in STEMI Patients in the Modeling Group
Based on the statistically significant factors identified in the results of 2.2, history of angina (yes=1, no=0), ventricular aneurysm (yes=1, no=0), alcohol abuse history (yes=1, no=0), postoperative TIMI grade ≤2 (yes=1, no=0), LVEF, and total ischemia time were included as independent variables in the multifactorial logistic analysis. The results showed that history of angina, ventricular aneurysm, alcohol abuse history, postoperative TIMI grade ≤2, LVEF, and total ischemia time were influencing factors for the formation of left ventricular thrombus after PCI in STEMI patients (P<0.05). See Table 3.
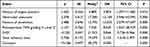 |
Table 3 Multivariate Logistic Regression Analysis of Left Ventricular Thrombosis After PCI in Modeling Group STEMI Patients |
Development and Evaluation of the Nomogram Model for the Risk of Left Ventricular Thrombus Formation After PCI in STEMI Patients
Including the aforementioned six indicators: history of angina, ventricular aneurysm, alcohol abuse history, postoperative TIMI grade ≤2, LVEF, and total ischemia time, the nomogram model for the risk of left ventricular thrombus formation after PCI in STEMI patients was constructed using the rms package in R 4.3.3 software, as shown in Figure 2. In internal validation, the calibration curve showed high consistency between predicted and actual probabilities, with an concordance index of the ROC curve being 0.962 (95% CI: 0.9310.994), indicating high model calibration and discrimination; the H-L test χ2=11.977 (P=0.152). See Figure 3A and B. In external validation, the calibration curve also showed high consistency between predicted and actual probabilities, with an concordance index of the ROC curve being 0.958 (95% CI: 0.9260.990), indicating high model discrimination and calibration; the H-L test χ2=9.757 (P=0.282). See Figure 4A and B.
 |
Figure 3 Correction curves (A) and ROC curves (B) of the risk nomogram for left ventricular thrombosis after PCI in the modeling group. |
 |
Figure 4 Correction curves (A) and ROC curves (B) of the risk nomogram for left ventricular thrombosis after PCI in the validation group. |
Clinical Utility Evaluation of the Nomogram Model for the Risk of Left Ventricular Thrombus Formation After PCI in STEMI Patients
The All line represents the assumption that all STEMI patients develop left ventricular thrombus after PCI, while the None line represents the assumption that no STEMI patients develop left ventricular thrombus early after PCI. The DCA curve shows that the nomogram model performs better in the high-risk threshold probability range of 0.02~0.99, yielding a higher net benefit. See Figure 5.
 |
Figure 5 DCA curve of nomogram for left ventricular thrombosis after PCI. |
Discussion
The clinical hazard of left ventricular thrombosis mainly lies in the rupture and detachment of thrombi, leading to embolism in peripheral arteries and critical organs, presenting a high risk of disability or death to patients.10 Therefore, identifying the incidence and risk factors of left ventricular thrombosis in STEMI patients and providing early treatment for high-risk patients to prevent severe embolic events are of great significance. Cardiac magnetic resonance imaging is the gold standard for diagnosing left ventricular thrombosis, but it is costly and not widely available.11,12 Moreover, given that left ventricular thrombosis is a complex disease involving various pathophysiological mechanisms, binary diagnostic and predictive methods, such as cardiac magnetic resonance imaging, cannot reflect the complexity of the patient’s condition.13 Thus, a quantitative model based on multiple factors to determine the risk of left ventricular thrombosis is needed.
Multifactorial analysis revealed that history of angina, ventricular aneurysm, alcohol abuse history, postoperative TIMI grade ≤2, LVEF, and total ischemia time are influencing factors for left ventricular thrombosis after PCI in STEMI patients. (1) History of angina. Angina is mainly caused by coronary artery stenosis due to arteriosclerosis leading to myocardial ischemia.14,15 It is hypothesized that STEMI patients with a history of angina have relatively severe coronary stenosis, increasing the risk of left ventricular thrombosis. (2) Ventricular aneurysm. The presence of ventricular aneurysms can lead to weakened or absent myocardial motion in the affected area, slowing blood flow within the aneurysm, causing stasis, and increasing the risk of left ventricular thrombosis.16 (3) Alcohol abuse history. Excessive alcohol intake can lead to various complications in the liver, myocardium, pancreas, etc., causing reduced blood flow and a hypercoagulable state, which can trigger thrombosis.17 Furthermore, excessive alcohol consumption can directly increase the risk of venous thrombosis. Excessive alcohol intake can cause oxidative stress damage, stimulate platelet aggregation, and activate various inflammatory cytokines, thereby increasing the risk of left ventricular dilation and thrombosis. (4) Postoperative TIMI grade ≤2 and total ischemia time. In this study, a postoperative TIMI grade ≤2 added an impact weight of 17.21 points, and each additional 2 hours of total ischemia time increased the impact weight on left ventricular thrombosis by 12.5 points. Previous studies have shown that a postoperative TIMI grade ≤2 indicates continuous myocardial ischemia, decreased left ventricular contractile function, slowed left ventricular blood flow, and a significant increase in platelet activation factors and inflammatory cytokines,18 all of which can lead to the formation of left ventricular thrombosis. (5) LVEF. Studies by Wang et al19 found that STEMI patients with lower LVEF after PCI had larger MI areas, reduced myocardial contractility, significant pump dysfunction, and left ventricular blood stasis, tending towards left ventricular thrombosis. A similar conclusion was drawn in this study: lower LVEF after PCI in STEMI patients increased the risk of left ventricular thrombosis, with each 5% decrease in LVEF adding 8.42 points to the impact weight in the nomogram. However, due to the limitations of the data included in this study, LVEF was not stratified for analysis, and therefore its threshold value could not be determined.
The nomogram model, based on the results of logistic proportional hazards or logistic regression analysis, graphically and visually predicts individual disease risks, making it more intuitive and easier to implement in clinical practice.20 Compared with traditional risk scoring systems, the nomogram model integrates more risk factors and provides numerical probabilities of the target event, quantifying risks more accurately and offering more flexible application.21,22 This study developed an easy-to-use nomogram model, integrating six clinically accessible and routinely collected indicators, providing an accurate and effective tool for predicting left ventricular thrombosis after PCI. Both internal and external validations showed that the nomogram had good predictive performance, high discrimination and calibration, with concordance index of 0.962 and 0.958, respectively, and the H-L test results indicated no bias between the predicted and actual values of the nomogram model. In the study by Li et al23 the nomogram demonstrated strong predictive accuracy for left ventricular thrombus in patients with non-valvular atrial fibrillation, with C-index values of 0.836 in the training group and 0.794 in the validation group. Another study by Li et al24 showed a C-index of 0.92 for predicting ventricular thrombus in patients with dilated cardiomyopathy, based on internal validation. The results of the present study exceed those reported in the previous studies. Clinicians can utilize the nomogram developed in this research to identify high-risk STEMI patients who may develop left ventricular thrombus, enabling closer monitoring, early diagnosis, and targeted prevention and treatment. Furthermore, the newly constructed nomogram model may serve as a potential alternative to transthoracic echocardiography for STEMI patients who are unable to tolerate the procedure.
In conclusion, the incidence of left ventricular thrombosis is high in STEMI patients after PCI treatment, with history of angina, ventricular aneurysm, alcohol abuse history, postoperative TIMI grade ≤2, LVEF, and total ischemia time being its risk factors. The nomogram model constructed from these risk factors has high predictive value for left ventricular thrombosis after PCI in STEMI patients. Clinicians should pay close attention to patients at high risk for left ventricular thrombosis predicted by the nomogram model, actively provide appropriate treatment, and increase the frequency of examinations and follow-ups to reduce the occurrence of further complications.
Limitations
This study still has some limitations. First, as a cross-sectional retrospective study, the argument is not comprehensive enough, and whether the identified risk factors are merely markers of left ventricular thrombosis or have a causal relationship still needs further determination. Second, due to the limitations of small sample analysis and variability in follow-up time, the results may exhibit high heterogeneity. Third, the collinearity of related risk factors, such as history of angina and LVEF, which can both cause myocardial damage and exacerbate each other, may affect the analysis results of this study. Fourth, as a retrospective analysis, this study may have selection bias in the sample selection process. Lastly, all patients included in this study were from the same hospital and race, so factors like medical standards and race might influence the outcomes.
Data Sharing Statement
The original contributions presented in the study are included in the article.
Ethics Approval
This study involving human participants were reviewed and approved by the ethical standards of the Medical Ethics Committee of The Affiliated Nanhua Hospital, Hengyang Medical School, University of South China and with the 1964 helsinki Declaration. And obtain the informed consent form of the patient or their guardian, and sign on the informed consent form.
Funding
Hunan Provincial Clinical Medical Research Center for Cardiac Interventional Therapy (2020SK4007; Key Guiding Projects of Hunan Provincial Health Commission for 2020 (20201905).
Disclosure
Authors declared no conflict of interest.
References
1. Elendu C, Amaechi DC, Elendu TC, et al. Comprehensive review of ST-segment elevation myocardial infarction: understanding pathophysiology, diagnostic strategies, and current treatment approaches. Medicine. 2023;102(43):e35687. doi:10.1097/MD.0000000000035687
2. Van De Werf F, Ristić AD, Averkov OV, et al. STREAM-2: half-dose tenecteplase or primary percutaneous coronary intervention in older patients with ST-segment-elevation myocardial infarction: a randomized, open-label trial. Circulation. 2023;148(9):753–764. doi:10.1161/CIRCULATIONAHA.123.064521
3. Thrane PG, Olesen KKW, Thim T, et al. Mortality trends after primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2023;82(10):999–1010. doi:10.1016/j.jacc.2023.06.025
4. Puymirat E, Soulat G, Fayol A, et al. Rationale and design of the direct oral anticoagulants for prevention of left ventricular thrombus after anterior acute myocardial infarction (APERITIF) trial. Am Heart J. 2023;2023:266.
5. Khaled S, Hachicha Z, Elkhateeb O. Left ventricular thrombus in myocardial infarction after successful primary percutaneous coronary intervention: prevalence and predictors-a middle eastern single-centre experience. CJC Open. 2020;2(3):104–110. doi:10.1016/j.cjco.2020.02.001
6. Kwok CS, Bennett S, BorovaC JA, et al. Predictors of left ventricular thrombus after acute myocardial infarction: a systematic review and meta-analysis. Coron Artery Dis. 2023;34(4):250–259. doi:10.1097/MCA.0000000000001223
7. Boivin-Proulx LA, Ieroncig F, Demers SP, et al. Contemporary incidence and predictors of left ventricular thrombus in patients with anterior acute myocardial infarction. Clin Res Cardiol. 2023;112(4):558–565. doi:10.1007/s00392-023-02158-8
8. Li Z, Pan L, Deng Y, et al. Development and validation of a nomogram for estimation of left atrial thrombus or spontaneous echo contrast risk in non-valvular atrial fibrillation patients with low to borderline CHA2DS2-VASc scoreInt. J Gen Med. 2022;15:7329–7339.
9. Anderson HVS, Masri SC, Abdallah MS, et al. 2022 ACC/AHA key data elements and definitions for chest pain and acute myocardial infarction: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Data Standards. J Am Coll Cardiol. 2022;80(17):1660–1700. doi:10.1016/j.jacc.2022.05.012
10. Honan KA, Jogimahanti A, Khair T. An updated review of the efficacy and safety of direct oral anticoagulants in treatment of Left Ventricular Thrombus. Am J Med. 2022;135(1):17–23.
11. Chaosuwannakit N, Makarawate P. Left ventricular thrombi: insights from cardiac magnetic resonance imaging. Tomography. 2021;7(2):180–188. doi:10.3390/tomography7020016
12. Levine GN, Mcevoy JW, Fang JC, et al. Management of patients at risk for and with left ventricular thrombus: a scientific statement from the American heart association. Circulation. 2022;146(15):e205–e23. doi:10.1161/CIR.0000000000001092
13. Camaj A, Fuster V, Giustino G, et al. Left ventricular thrombus following acute myocardial infarction: JACC state-of-the-art review. J Am Coll Cardiol. 2022;79(10):1010–1022. doi:10.1016/j.jacc.2022.01.011
14. Welén Schef K, TOrnvall P, Alfredsson J, et al. Prevalence of angina pectoris and association with coronary atherosclerosis in a general population. Heart. 2023;109(19):1450–1459. doi:10.1136/heartjnl-2023-322345
15. Shao C, Wang J, Tian J, et al. Coronary artery disease: from mechanism to clinical. PracticeAdv Exp Med Biol. 2020;2020:1177.
16. Tayal M, Dhingra V, Sharma P, et al. COVID myocardial involvement presenting as left ventricular aneurysm and clot associated with normal coronary anatomy, deep vein thrombosis, and abnormal brachial artery flow-mediated dilatationJ. Family Med Prim Care. 2022;11(5):2217–2219. doi:10.4103/jfmpc.jfmpc_1658_21
17. Stettler GR, Moore EE, Nunns GR, et al. Do not drink and lyse: alcohol intoxication increases fibrinolysis shutdown in injured patientsEur. J Trauma Emerg Surg. 2021;47(6):1827–1835. doi:10.1007/s00068-020-01328-x
18. Gao N, Qi X-Y. Risk factors for in-hospital death in acute ST-segment elevation myocardial infarction after emergency percutaneous coronary intervention: a multicenter retrospective study. Ann Palliat Med. 2021;10(11):11756–11766. doi:10.21037/apm-21-2722
19. Wang P, Ye X, Yan D, et al. Incidence and risk factors of left ventricular thrombus in acute ST-segment elevation myocardial infarction treated by primary percutaneous coronary intervention: a meta-analysis. Med Princ Pract. 2022;31(5):415–423. doi:10.1159/000525943
20. Fang C, Chen Z, Zhang J, et al. Construction and evaluation of nomogram model for individualized prediction of risk of major adverse cardiovascular events during hospitalization after percutaneous coronary intervention in patients with acute ST-segment elevation myocardial infarction. Front Cardiovasc Med. 2022;9:1050785. doi:10.3389/fcvm.2022.1050785
21. Zheng X, Huang R, Liu G, et al. Development and verification of a predictive nomogram to evaluate the risk of complicating ventricular tachyarrhythmia after acute myocardial infarction during hospitalization: a retrospective analysisAm. J Emerg Med. 2021;46:462–468.
22. Wang Y, Wang W, Jia S, et al. Development of a nomogram for the prediction of in-hospital mortality in patients with acute ST-elevation myocardial infarction after primary percutaneous coronary intervention: a multicentre, retrospective, observational study in Hebei province. China BMJ Open. 2022;12(2):e056101. doi:10.1136/bmjopen-2021-056101
23. Li Z, Liu Q, Liu F, et al. Nomogram to predict left atrial thrombus or spontaneous echo contrast in patients with non-valvular atrial fibrillation. Front Cardiovasc Med. 2021;8:737551. doi:10.3389/fcvm.2021.737551
24. X-L L, Adi D, Wu Y, et al. A nomogram to predict ventricular thrombus in dilated cardiomyopathy patients. J Thromb Thrombolysis. 2024;57(1):29–38. doi:10.1007/s11239-023-02846-2
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




