Back to Journals » Psychology Research and Behavior Management » Volume 18
Correlation Between COVID-19 Recovery, Executive Function Decline, and Emotional State
Authors Velásquez Cabrera DM , De la Roca-Chiapas JM , Hernández-González MA , Reyes Pérez V, Villada C
Received 17 July 2024
Accepted for publication 8 April 2025
Published 23 April 2025 Volume 2025:18 Pages 1007—1019
DOI https://doi.org/10.2147/PRBM.S487382
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Daniela María Velásquez Cabrera,1 Jose Maria De la Roca-Chiapas,2 Martha Alicia Hernández-González,3 Verónica Reyes Pérez,2 Carolina Villada2
1Health Sciences Division, University of Guanajuato, Guanajuato, Mexico; 2Department of Psychology, University of Guanajuato, Guanajuato, Mexico; 3Department of Medicine and Nutrition, Division of Health Sciences, University of Guanajuato, Guanajuato, Mexico
Correspondence: Jose Maria De la Roca-Chiapas, Department of Psychology, University of Guanajuato, Mexico Sede San Carlos, Blvd. Puente Milenio No. 1001 Fracción del Predio San Carlos; C.P. 37670, León, Guanajuato, Mexico, Tel +52 477 267 4900 ext 3644, Email [email protected]
Objective: The aim of this study was to determine whether there is a relationship between the time since recovery from coronavirus disease 2019 (COVID-19) and alterations in executive functions. We also evaluate the emotional state of post-COVID-19 patients.
Patients and Methods: We assessed patients between 18 and 50 years old, who had a history of COVID-19 with mild, moderate, or severe illness. We used the Batería Neuropsicológica de Funciones Ejecutivas y Lóbulos Frontales-3 (BANFE-3), Mini-Mental State Examination (MMSE), and Mini-International Neuropsychiatric Interview (MINI), in addition to a semi-structured interview. Spearman’s correlation coefficient was used, with a p value < 0.05 indicating significance.
Results: We evaluated 67 patients with a mean age of 34.6± 9.6 years, most of whom had ≥ 13 years of schooling (n=55, 82.1%). Among them, 52 (77.6%) reported persistent symptoms after resolution of the condition, with fatigue being the most frequent (n=20, 29.9%). Most participants had an adequate score on the MMSE (n=60, 89.6%). However, 19 (28.4%) showed alterations in the BANFE-3 total score, with mental flexibility as the most affected function (n=25, 37.3%). In participants from the first COVID-19 wave, a negative correlation was observed between the standardized orbitofrontal area scores and the time since recovery from the infection (r=− 0.841, p=0.016), suggesting a pattern of deterioration over time, mainly in stimulus inhibition (r=0.880, p=0.021). Regarding emotional state, 45 subjects (67.2%) exhibited emotional alterations, with anxiety symptoms being the most frequent (n=33, 49.3%). Furthermore, individuals with depressive symptoms (n=32, 47.8%) were more likely to experience executive function impairment after COVID-19 (ExpB 0.302, 95% CI 0.098– 0.933, p=0.038).
Conclusion: COVID-19 could lead to alterations in executive functions, probably resulting from progressive damage to orbitofrontal area functions, mainly in stimulus inhibition. However, the generalizability of these findings is limited, highlighting the need for further research with robust methodology. Furthermore, depression appears to be an indicator of cognitive impairment in individuals recovering from COVID-19. Therefore, cognitive rehabilitation and psychological support are essential for patients affected by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection.
Keywords: coronavirus infection, cognition, executive function, affective symptoms
Introduction
Coronavirus disease 2019 (COVID-19) is caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). COVID-19 causes respiratory, digestive, and cardiovascular symptoms, as well as olfactory and gustatory alterations and hallucinations, which were not seen with previous viruses such as SARS-CoV or Middle East respiratory syndrome coronavirus (MERS-CoV). These symptoms could be caused by an affinity between SARS-CoV-2 and the central nervous system (CNS).1
In addition, COVID-19 patients experience neurological symptomatology in the second week after the onset of symptoms; for example, confusion, agitation, alterations in the corticospinal tract, inattention, disorientation, and poorly organized movements in response to command post-discharge.2 Furthermore, patients may experience enhancement in leptomeningeal spaces, bilateral frontotemporal hypoperfusion, ischemic strokes,2 and altered consciousness.3
The neurological symptoms could be the result of SARS-CoV-2 reaching the CNS through the peripheral nerves (olfactory or trigeminal)4 or via the systemic circulation, which could damage the blood–brain barrier.5 They could also could be caused by the immune system attack resulting from the cytokine storm;6 or a reduction of the oxygen supply to the brain, which will result in cognitive impairment.7
In Mexico, we had five different COVID-19 waves. A wave is a period of increased incidence of cases, compared to a previous period, due to an increase in generalized transmission. The first wave occurred between epidemiological week (EW) 8 and 29 of 2020, the second wave between EW 40 of 2020 and EW 15 of 2021, the third wave between EW 23 and 42 of 2021, the fourth wave between EW 51 of 2021 and EW 9 of 2022, and the fifth wave between EW 22 and 33 of 2022.8
After infection, 10–20% of cases had persistent symptoms.9 These symptoms, which may or may not have been present in the early part of the infection, appear within 3 months of the onset of COVID-19, last for at least 2 months, and cannot be explained by an alternative diagnosis.10 This condition is known as the post-COVID-19 condition.10,11 Fatigue and “mental fog” (problems with concentration and memory) are the key features of this condition.9,11
Previous research has reported cognitive alterations, evaluated by the Montreal Cognitive Assessment (MoCA),12,13 Mini-Mental State Examination (MMSE),12,13 Trail Making Test part B (TMT-B),7 and other objective tests.7,13–24 These alterations were present in the acute phase and from the first month after infection to 6 months. However, they were more commonly encountered in the long term.9,20
The most frequent dysfunctions in the post-acute phase include problems with working memory,14,15 attention,13,14,20,25 abstraction,13 verbal fluency,15 learning and memory,20,21 and executive functions.16–18,20,25
Executive functions are the most elevated cognitive processes, located in the frontal lobe. This area is one of the last areas to complete the myelination process and is the most developed. It is also one of the most susceptible to alterations due to environmental factors, such as infections.26 The executive functions involve the control of mental activity, emotional response, and behavior.27,28 In addition, they encompass a set of skills, including problem solving for goal achievement, organization, inhibition of actions, interference management, hypothesis generation, planning, abstraction, mental flexibility, decision making, and self-awareness.26,27,29
Alterations in executive function may lead to initiation disorders, memory disorders, hyperactivity or global hypoactivity, adaptation problems, or behaviors that do not follow social conventions (irresponsible or impulsive behaviors). In addition, cognitive deficits and dysregulation of motivational and emotional aspects sometimes precede the development of dementia in patients with neuroinflammatory and neurodegenerative diseases.30 For these reasons, it is necessary to identify cognitive and emotional sequelae after COVID-19, and, if they exist, to establish what happens over time. Our hypothesis is that there is a correlation between time since COVID-19 recovery and the executive function score. The aim of this study was to determine the correlation between time since recovery from SARS-CoV-2 with the executive function scores.
Material and Methods
Design
This observational, prospective, correlation study was conducted in two cities in Guanajuato state, Mexico, from October 2021 to September 2022.
Participants
The study evaluated 67 patients with a previous diagnosis of COVID-19, who had recovered from the acute phase of the illness, whether it had been mild, moderate, or severe, were between 18 and 50 years old, with a minimum educational level of high school, and had no previously diagnosed prefrontal syndrome, attention deficit hyperactivity disorder (ADHD), history of substance abuse, or epilepsy.
The sample size was calculated with r=0.34, α=0.05, and β=0.20. The result was 67 patients.31
The recruitment process followed two main approaches. Eligible patients at the High Specialty Medical Unit HE1 CMN Bajío, IMSS, were invited to participate in the project. In addition, hospital staff, administrative personnel, professors. and students of the University of Guanajuato were recruited through information disseminated via e-mail, posters, and university newsletters.
Procedure
A single researcher, a psychologist with 3 years of experience in administering psychometric tests, including the Mini-Mental State Examination (MMSE),32 conducted all evaluations. Specific training for the Batería Neuropsicológica de Funciones Ejecutivas y Lóbulos Frontales-3 (BANFE-3)33 was provided by a psychologist with 6 years of experience, while additional training for the Mini-International Neuropsychiatric Interview (MINI)34 was given by another investigator, with 14 years of experience.
The assessments took place in an office at the IMSS, in a private cubicle in a public library, or a suitable space at the University of Guanajuato. The evaluation process lasted between 45 and 75 minutes, and included the signing of informed consent, an identification form, developed by the authors, and application of the instruments: MMSE, MINI and, after a short break, BANFE-3. The study was conducted entirely in Spanish with Spanish-speaking individuals.
All participants were provided with information about places offering free emotional support and post-COVID rehabilitation (at the University of Guanajuato). Cases of severe emotional disturbances were referred to the IMSS psychology department for follow-up care. In addition, approximately 2–3 months after the evaluation, participants we provided with a report of their results and personalized recommendations to strengthen their cognitive skills.
Variables
The diagnostic date was the day of a positive test result or the onset of symptoms, whichever came first. All participants had a positive test result by a positive polymerase chain reaction (PCR) or an antigen test. Information on the symptoms in the acute phase and after COVID-19 was self-reported by the participants.
The COVID-19 resolution date was defined by the WHO criteria,35 the severity level used the IMSS criteria,36 and the definition of COVID-19 waves followed the epidemiological weeks of the Mexican Ministry of Health.8
Ethics
The study complied with the Declaration of Helsinki, was of minimal risk, and was approved by the Institutional Ethics Committee of the High Specialty Medical Unit HE1 CMN Bajio, IMSS (institutional registration number: R-2021-1001-052). Informed consent was requested from each participant. None of the participants received any financial compensation.
Instruments
Batería Neuropsicológica de Funciones Ejecutivas y Lóbulos Frontales-3 (BANFE-3)
BANFE is an instrument developed by Flores, Ostrosky-Solís, and Lozano. BANFE-3 is the third edition. It has an inter-applicator agreement of 0.8 and a reliability of 0.8. It consists of 15 tests divided according to anatomical–functional criteria: orbitofrontal cortex, medial prefrontal cortex, dorsolateral prefrontal cortex, and anterior prefrontal cortex. This test was standardized in Mexico in subjects between 6 and 90 years of age with schooling level from 3 years old. It provides standardization tables according to age and educational level. The scores obtained can be classified as a high normal level (116 and above), normal (85–115), mild–moderate alteration (70–84), and severe alteration (60 or less).33
Mini-Mental State Examination (MMSE)
MMSE, by Folstein (1975),32 is a screening test. It has a Cronbach’s alpha of 0.78 and the application time is approximately 15 minutes. It is used to detect cognitive deficits. It measures 11 categories: temporal orientation, spatial orientation, attention and calculation, memory, nomination, repetition, comprehension, reading, writing, and drawing. Scores of 30–27 points mean adequate cognitive status, 26–25 points possible cognitive impairment, 24–10 points mild to moderate cognitive impairment, 9–6 points moderate to severe cognitive impairment, and less than 6 points severe cognitive impairment.32
Mini-International Neuropsychiatric Interview (MINI)
MINI34 is a brief diagnostic structured interview, with standardized information from the ICD-10 criteria. It has an application time of about 15 minutes, and asks about the main psychiatric disorders of axis I of the DSM-IV and ICD-10, with yes/no answers.34
Statistical Methods
SPSS 26.0 statistical software was used for statistical analysis of the data. Qualitative variables were expressed as frequency and percentage; and quantitative variables, according to their distribution, were expressed as means and standard deviation, or median and interquartile range. The chi-squared test or Fisher’s exact test was run, when appropriate. In addition, single-factor ANOVA or Kruskal–Wallis was used to compare variables between the different groups, since the sample was divided according to the wave in which the patient had COVID-19. Finally, Spearman’s correlation coefficient and logistic regression were used.
Results
We evaluated 68 patients, of whom one was eliminated because he decided not to complete the evaluation process. The total sample consisted of 67 patients, with a mean age of 34.6±9.6 years. Forty-nine patients (73.1%) were women. Thirteen subjects (22.4%) were studying for bachelor’s degrees and two for master’s degrees (3%), and 39 subjects (58.3%) had attended psychological therapy (Table 1).
 |
Table 1 Characteristics of patients with a history of COVID-19 (N=67) |
 |
Table 2 Results of MINI, MMSE, and BANFE-3 |
The most common symptoms in the acute phase were fatigue, cough, and body pain, which were experienced by 43 (64.2%), 41 (61.2%), and 39 subjects (58.2%), respectively. Only four participants (6%) had been hospitalized, of whom one had been in the ICU (1.5%). In terms of severity, 54 (80.6%) had mild illness. The median time from COVID recovery was 235 (34–370) days. In 52 subjects (77.6%), symptoms persisted after resolution of the condition. The most frequent symptoms were fatigue (n=20, 29.9%), concentration problems (n=14, 20.9%), memory problems (n=12, 17.9%), and insomnia (n=10, 14.9%).
Table 2 presents the results of the tests applied. Anxiety disorders were the most prevalent (n=33, 49.3%), with significant difference between waves, as well as depressive symptoms. No association was found between the participants’ psychological history and alterations on the MINI (p=074).
The majority of subjects demonstrated an adequate level on the MMSE (n=60, 89.6%). Similarly, 48 participants (71.6%) scored within the normal range on the BANFE-3, one participant (1.5%) scored in the high normal range, while three patients (4.5%) exhibited severe alterations and 16 patients (23.9%) presented mild to moderate alteration.
Likewise, the scores obtained on the BANFE-3 specified which skills were impaired. Mental flexibility, metamemory, and risk–benefit balance were the most frequently altered, in 25 (37.3%), 23 (34.3%), and 19 patients (28.4%), respectively (Table 3).
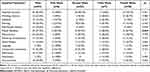 |
Table 3 Qualitative Results of the BANFE-3 |
It was determined that there is an association between severity level and alteration in the BANFE-3 total score (p=0.030). Persistent symptoms, such as fatigue, sleep problems, and agitation, were associated with alterations in the dorsolateral area (p=0.031, p=0.047, p=0.001, and p=0.035, respectively). In addition, sleep problems were associated with alterations in the BANFE-3 total score (p=0.006), and the presence of headache and loss of smell during the acute phase were associated with alterations in cognitive functions (p=0.018 and p=0.012, respectively).
We also found a correlation between the people who had COVID-19 in the first wave and the standardized orbitofrontal cortex score (r=−0.841, p=0.036). When taking each of the tests that integrate the evaluation of the orbitofrontal area, there was a negative correlation between the percentages of risk cards in the card test, which measures the ability to make decisions in uncertain situations, based on a risk–benefit balance (r=−0.812, p=0.050). This means that the longer the time elapsed after COVID-19, the lower the percentage and the better the performance.
Likewise, there was a strong positive correlation between the number of Stroop A errors and the time since COVID-19 (r=0.880, p=0.021). That is, the more days, the greater the number of errors in this subsection, which is linked to the inhibition of a highly automated response.
Similarly, regarding functions related to the prefrontal area, it was found that the longer the time since recovery from infection, the fewer positive errors occurred in the metamemory test. That is, the lower the overestimation of the number of words predicted by the subject (r=−0.926, p=0.008).
In addition, the longer the time since COVID-19, the fewer perseverations were seen in the letter classification test, which implies a probable recovery of the mental flexibility function in patients from the first COVID-19 wave (r=0.828, p=0.042).
Finally, people with depressive symptoms were 3.3 times more likely to have executive function impairment (ExpB=3.307, p=0.038, 95% CI 0.098–0.933), compared to those without.
Discussion
The present observational, prospective, correlation study found that Mexican adults who were infected with COVID-19 during the first wave exhibited lower standardized scores in the orbitofrontal area as more time elapsed after recovery, with a correlation coefficient of −0.841 (p=0.036), which implies a strong correlation.37 However, when analyzing specific cognitive functions, we observed progressive dysfunction in stimulus inhibition, evaluated by the Stroop part A (r=0.880, p=0.021). Nevertheless, decision making in uncertain situations improved over time, as evidenced by a decrease in the percentage of risk cards in the card test (r=−0.812, p=0.050).
Cognitive impairments in COVID-19 survivors, including mental flexibility (37.7%), metamemory (34.3%), risk–benefit balance in uncertain situations (28.8%), planning (26.9%), working memory (22.4%), and consecutive subtraction (22.4%), were consistent with those found in previous studies.13–15,18,38
From this, we suggest that there is an executive deficit after COVID-19 in different domains, such as verbal fluency, inhibition, cognitive flexibility, and attention, as evaluated in the inverse digit test.39,40 In addition to memory,20,21,41 attention and concentration problems,41 learning, executive function, and perceptual motor problems,20 which were also found in research with young adults, it is concluded that patients who have recovered from mild or moderate COVID-19 may have neuropsychological deficits.41
Theses cognitive alterations could be explained by neuroanatomical changes due to the infection, such as the loss of gray matter in the left orbitofrontal cortex, left parahippocampal gyrus, and left superior insula, with extension to the anterior cingulate cortex, left supramarginal gyrus, and right temporal pole.42,43 Many of these areas are related to the primary olfactory cortex,42,43 explaining the high incidence of olfactory disturbances.4
One of the possible entry routes into the CNS is by transneuronal penetration through the olfactory bulb,4,44 spreading transneuronally to other regions of the brain, and causing inflammation and demyelinating reactions.44 Persistent inflammation in the olfactory neuroepithelium has been observed 110–119 days after the first COVID-19-related symptoms in patients with persistent olfactory loss.45
In our patients, the anosmia in the acute phase was associated with cognitive dysfunction (p=0.012), consistent with findings from Almeria et al, who reported associations between loss of smell/taste and impairments in attention, memory, processing speed, and executive function.14 Similarly, Cysique et al associated cognitive impairment with objectively tested anosmia, and with a lower work capacity.46
Other affected areas in COVID-19 patients have connections with the frontal lobe and therefore influence executive functions. The hippocampus, anterior cingulate cortex, and orbitofrontal cortex play key roles in memory and emotional regulation,47 and in the processing and regulation of emotional and affective states, as well as behavior regulation.33
When discussing the expected recovery pattern in COVID-19 patients who experienced cognitive impairments, the literature shows that in non-hospitalized patients (mean patient age=45.7, SD=10.4 years) there were significant improvements in the domains of learning, memory, and executive function at 6 months after the baseline assessment.20 Similarly, Ferrucci et al found that while attention, processing speed, and verbal memory tended to improve, visuospatial memory did not appear to improve at 5 and 12 months after hospital discharge (mean patient age=56.2, SD=12 years).22 Conversely, another study reported significant improvements in visual memory, verbal and declarative memory, processing speed, executive function, and naming at 6 months after the first evaluation (mean patient age=49.1, SD=7.7 years).24 However, patients who initially had no cognitive complaints but developed them at 6 months did not show these improvements, and exhibited lower performance compared with the group with no cognitive complaints.24
A survey of individual symptom trajectories over time revealed that reports of cognitive dysfunction increased during the first 3 months, followed by a slight decline in subsequent months. Regarding memory symptoms, these increased during the first few months and persisted for up to 6 months.48 In addition, a study with a mean participant age of 45.37 (SD=20.98) years found that with a longer time since infection, patients had improvements in symptoms related to sleep, gastrointestinal and neuroendocrine pain, but progressive dysfunction in neurocognitive aspects, mainly in the ability to form words and in concentration.39
Similarly, research with follow-up at 2, 4, and 12 months post-infection in patients with mild to moderate COVID-19 found that cognitive performance was different from the normative reference at all assessment points, and that cognitive performance declined over time. The impairment profiles varied, with some patients being impaired at all of the follow-up visits (0.9%) and others showing impairment at specific time points, 2 and 12 months (2.4%), 4 and 12 months (2.4%), 2 and 4 months (3.9%), or at just one of the visits (8.7%, 13.4%, and 15% at 2, 4, and 12 months, respectively).46
A longitudinal imaging study identified greater cognitive decline between two assessment points, suggesting progressive neurodegeneration in some cases (mean patient age=65.4, SD=8.9 years).43
These findings underscore the variability in the trajectory of cognitive symptoms over time after COVID-19.20 Researchers in China have proposed four distinct post-COVID-19 cognitive profiles: early-onset deterioration, late-onset deterioration, progressive deterioration, and stable cognitive status.49
A factor that permeates the cognitive profile observed in our patients from the first wave is the fact that no vaccines were available at the time of acute infection. This is supported by research showing a higher risk of memory problems in pre-vaccination studies (RR=4.84, 95% CI 3.28–7.15 vs RR=3.02, 95% CI 1.15–7) and concentration problems in pre-vaccination studies (RR=2.39, 95% CI 0.76–7.47 vs RR=2.14, 95% CI 1.25–3.67). These findings suggest that vaccination could play a protective role in reducing the risk of long COVID.50 In this way, vaccination was associated with reduced odds of hospitalization, having more than five symptoms in the first week of illness, and a long duration of symptoms after the second dose, meaning that cases were less severe.51 In addition, it has been found that the risk of long COVID associated with infection by the omicron variant is lower, ie 50% less, compared with the delta variant.52 It has been suggested that different SARS-CoV-2 variants may induce different long COVID phenotypes.53
The progression of cognitive damage could be the result of the viral RNA remaining in the brain tissue for long periods,4 leading to neuronal loss over time; or due to a prolonged process of neuroinflammation,9,54 which causes severe hypoxia and, consequently, cerebral vasodilatation, cerebral edema, and ischemia.44
It could also be explained by anatomical changes in COVID-19 patients (average 141 days after onset), such as longitudinal differences in the functionally connected regions of the temporal piriform cortex and olfactory tubercle, or by a reduction in gray matter thickness in the left parahippocampal gyrus and lateral orbitofrontal cortex, in comparison with control patients. In addition, atrophy was present in regions such as the limbic area and crus II, with the latter being associated with cognitive decline; and there was a decrease in whole-brain volume, suggesting additional diffuse gray matter loss.43
The global gray matter volume (GMV) in COVID-19 patients (3 months after onset) was correlated slightly with lactate dehydrogenase (LDH) concentration; therefore, the decreased GMV in patients with elevated LDH may indicate atrophy due to a severe inflammatory response.55
Moreover, there could be an adverse dynamic of hypometabolism over time, which presumably is associated with severity; that is, more severe cases have more glucose disturbance and a longer duration of symptoms.41 This was identified in our results, where we observed an association between the level of severity and the presence of cognitive impairment (p=0.30).
On the other hand, the progressive recovery of functions could be attributed to an improvement in hypometabolism in the bilateral prefrontal area, ie, in the orbitofrontal, dorsolateral, and mesiofrontal cortex. This pattern is consistent with clinical frontal lobe syndrome. Follow-up of the subjects for a median of 5 months showed an improvement in the results of neurological examinations and indicated that the patients were autonomous in their activities of daily living. However, executive deficits were still constant, consistent with emotional diagnoses.56
In some patients, cerebral metabolism improved as early as 1 month after the first evaluation, and by 6 months, it had returned to levels comparable to those of the control group. In others, the improvement was moderate.56 Moreover, in certain cases, even when there was no significant decrease in cerebral metabolism, residual neocortical hypometabolism persisted in COVID-19 patients, particularly in areas that were more affected in the acute phase, so they may take longer to recover.57
Thus, further research with more robust methodological designs is needed, including control groups, larger sample sizes, and consideration of COVID-19 waves during sample size calculations, long-term studies with follow-up periods extending beyond 12 months after infection, and the use of objective methodologies to assess cognitive functions. Such research is crucial to be able to draw more robust conclusions.
Moving on to emotional alterations, the most frequent in our subjects were depression and anxiety, as reported in the literature on post-COVID syndrome.9,21,23,58 These conditions may be attributed to trauma during the infection, social isolation, and/or confinement.9 In addition, misinformation about the condition, social stigmatization, feelings of uncertainty, and the perception of loss of control could contribute to these disorders.21
In this regard, studies on the general Mexican population during the first months of the pandemic reported prevalence rates ranging from 37.7% to 65.2% for symptoms consistent with anxiety, while depression was present in 36.3–51.3% of the subjects.59,60 In our study, depression was observed in 32 (47.8%) and anxiety-related diagnoses (agoraphobia, anxiety disorder, and generalized anxiety) were present in 33 (49.3%).
Comparing these frequencies with those of the general population prior to the pandemic, National Health and Nutrition Survey (ENSANUT) data from 2018 showed that 17.3% of adults in Mexico experienced depressive symptoms,61 while anxiety was present in 14.3% of the population in 2003.62 This highlights an increase in mental health disorders due to the COVID-19 pandemic and associated lockdowns.63 In addition to other risk factors, individuals who were unemployed, had low income, lacked physical activity, were women or young adults (<35 years), were elderly, had a history of psychiatric disorders, or worked in healthcare were at a higher risk of experiencing emotional disturbances.63 64
Cognitive alterations may also have an emotional cause, as reflected in our results, in which people with depressive symptoms were 3.3 times more likely to have impaired executive function (ExpB=3.307, p=0.038, 95% CI 0.098–0.933) compared to those without these symptoms.
Research has found that depressive symptoms are associated with self-reported memory failures, and that their predictive value is higher in patients without olfactory dysfunction, as observed in most of our sample. Emotional symptoms predicted self-reported memory failures in regression models.65 Furthermore, the cognitive component of fatigue (dysfunctions in processing speed, sustained attention, and executive functions) was most strongly predicted by neuropsychiatric symptoms, such as level of depression and anxiety.66
In another study, which used the Depression Anxiety and Stress Scale-21 (DASS-21) to assess anxiety, depression, and stress, these emotional symptoms significantly influenced the majority of neuropsychological test scores, except for Test of Everyday Attention auditory reaction time and Rey figure recall.23 It has also been reported in the literature that higher scores on anxiety and depression could contribute to the lack of neurocognitive improvement at 6 months.24
There is also well-documented comorbidity between depression and cognitive impairment, including evidence that depression disorder includes abnormalities in cognitive functioning and that this mood alteration increases the risk of dementia.67 During the acute phase of depression, alterations have been observed in processing speed, learning, memory, verbal fluency, and attention. Although these deficits become less pronounced in the remission phase, attention, learning, memory, and working memory deficits may persist.68
A lower volume in the insula, superior temporal gyrus, inferior frontal gyrus, amygdala, hippocampus, and thalamus has been identified in patients with major depressive disorder (MDD) and mild cognitive impairment, potentially explaining their longitudinal comorbidity.67 In addition, inflammation, a factor associated with MDD, is a significant feature of COVID-19, which caused systemic inflammation and may contribute to the development or exacerbation of MDD.69
Limitations
This study has some limitations. First, there was no control group, owing to the high infectivity of the virus and the difficulty in identifying individuals who did not contract it. However, in BANFE-3 we utilized normative tables depending on educational level and age.
Second, the study design may be seen as a limitation. While a long-term study would have been ideal, the chosen design allowed us to identify an initial association between these quantitative variables through the correlation analysis. Third, there is a risk of sampling bias, as the use of non-probabilistic convenience sampling may lead to higher prevalence estimates than those observed in the literature. Nevertheless, the proportion of cognitive impairment observed in our study is consistent with, or even lower than, findings from other studies, which is likely to be due to the younger age of our sample. In addition, we tried to minimize the bias through the inclusion criteria, to ensure a sample with similar characteristics. Fourth, the sample size was too small, and dividing it into groups increased the probability of type II errors. This limitation affected the ability of the study to detect potential differences between groups, highlighting the need for larger sample sizes in future research to ensure sufficient statistical power. Nevertheless, the magnitude of correlation found in this study was high and statistically significant.
One of the main strengths of this research is the use of an evaluation instrument that emphasizes higher cognitive processes in a sample of the Mexican population. Furthermore, the inclusion of emotional aspects as part of the post-COVID patient profile and the control of educational level add significant value to the study. In addition, the consideration of waves during the acute phase of infection provides a way to continue exploring the pattern of cognitive recovery from different COVID-19 variants.
Recommendations
Cognitive rehabilitation is essential and several therapies have been used for post-COVID patients, including Speed of Processing Training, Instrumental Activities of Daily Living Shaping,70 and game-based cognitive training,71 such as the AKL-T01, a digital therapy provided through a videogame interface, to target attention and executive control. This approach has shown improvements in task-switching, processing speed, and reductions in total fatigue, cognitive fatigue, and anxiety.72 Other approaches include transcranial direct current stimulation,73 goal management training, which relies on metacognitive strategies to improve executive attention processes,74 and an ambulatory program with neuropsychological rehabilitation, which include cognitive treatment, training in compensatory strategies, and emotional intervention,75 all available through a telerehabilitation platform called Guttmann NeuroPersonalTrainer®,76 which includes personalized computerized cognitive exercises. This treatment has demonstrated improvements in working and verbal memory, verbal fluency, anxiety, and depression.75
Conclusion
COVID-19 can cause alterations in executive functions, the most frequent in mental flexibility. The functions located in the orbitofrontal area, mainly stimulus inhibition, could even worsen over time in patients who contracted the infection during the first wave.
In addition, depression appears to be a potential indicator of cognitive impairment in individuals who recovered from the disease.
However, the absence of a control group, the small sample size, and the lack of patient follow-up limit the generalizability of these findings. Therefore, the conclusions of this study should be interpreted with caution.
Further research is required, with a longitudinal design and a larger sample size, incorporating a control group and groups differentiated by waves or virus variants to more accurately identify the effects of infection on cognition and mental health. Moreover, the use of neuroimaging or biomarker studies is essential to understanding how COVID-19 affects brain function.
Finally, we emphasize the importance of cognitive rehabilitation and psychological support as essential components in the multidisciplinary treatment of patients who have experienced SARS-CoV-2 infection.
Acknowledgments
We thank the National Council of Science and Technology (CONACYT) for the National Scholarship 2021–2023. We also thank the General Rectory, the Rectory of the León Campus, the Division of Health Sciences, the Office for Research Support, the Graduate Studies Department of the University of Guanajuato, and the Asociación Sindical de Personal Académico y Administrativo de la Universidad de Guanajuato.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7(7):611–627. doi:10.1016/S2215-0366(20)30203-0
2. Helms J, Kremer S, Merdji H, et al. Neurologic Features in Severe SARS-CoV-2 Infection. N Engl J Med. 2020;382(23):2268–2270. doi:10.1056/nejmc2008597
3. Zhang B, Zhou X, Qiu Y, et al. Clinical characteristics of 82 death cases with COVID-19. medRxiv. 2020. doi:10.1101/2020.02.26.20028191
4. Matías-Guiu J, Gomez-Pinedo U, Montero-Escribano P, Gomez-Iglesias P, Porta-Etessam J, Matias-Guiu JA. Should we expect neurological symptoms in the SARS-CoV-2 epidemic? Neurología. 2020;35(3):170–175. doi:10.1016/j.nrleng.2020.03.002
5. Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 Virus Targeting the CNS: tissue Distribution, Host-Virus Interaction, and Proposed Neurotropic Mechanisms. ACS Chem Neurosci. 2020;11(7):995–998. doi:10.1021/acschemneuro.0c00122
6. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(January):497–506. doi:10.1016/S0140-6736(20)30183-5
7. Miskowiak K, Johnsen S, Sattler S, et al. Cognitive impairments four months after Covid-19: pattern, severity and association with illness variables. Eur Neuropsychopharmacol. 2021;46(January):39–48. doi:10.1016/j.euroneuro.2021.03.019
8. Secretaría de Salud. Subsecretaría de Prevención y Promoción de la Salud, Dirección General de Epidemiología. Informe Integral de Covid-19 En México Número. 2022;2022:1.
9. Premraj L, V. KN, Briggs J, et al. Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: a meta-analysis. J Neurol Sci. 2022;434:120162. doi:10.1016/j.jns.2022.120162
10. Organización Mundial de la Salud (OMS). Update on Clinical Long-Term Effects of Covid-19. 2021.
11. Soriano JB, Murthy S, Marshall JC, Relan P, Diaz JV. A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. 2022;22(4):e102–e107. doi:10.1016/S1473-3099(21)00703-9
12. Pistarini C, Fiabane E, Houdayer E, Vassallo C, Manera MR, Alemanno F. Cognitive and Emotional Disturbances Due to COVID-19: an Exploratory Study in the Rehabilitation Setting. Front Neurol. 2021;12(May):1–8. doi:10.3389/fneur.2021.643646
13. Alemanno F, Houdayer E, Parma A, et al. COVID-19 cognitive deficits after respiratory assistance in the subacute phase: a COVID rehabilitation unit experience. PLoS One. 2021;16(2 February):1–12. doi:10.1371/journal.pone.0246590
14. Almeria M, Cejudo JC, Sotoca J, Deus J, Krupinski J. Cognitive profile following COVID-10 infection: clinical predictors leading to neuropsychological impairment. Brain Behavior Immunity Health. 2020;9:100163. doi:10.1016/j.bbih.2020.100163
15. Méndez R, Balanzá-Martínez V, Luperdi SC, et al. Short-term neuropsychiatric outcomes and quality of life in COVID-19 survivors. J Intern Med. 2021;2021:1–11. doi:10.1111/joim.13262
16. Tay MRJ, Low YH, Lim CCT, et al. Covert Subclinical Neurocognitive Sequelae during the Rehabilitation Course of Severe Coronavirus Disease 2019. Am J Phys Med Rehabil. 2021;100(1):39–43. doi:10.1097/PHM.0000000000001633
17. Mazza MG, De Lorenzo R, Conte C, et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav Immun. 2020;89(July):594–600. doi:10.1016/j.bbi.2020.07.037
18. Beresford T, Ronan PJ, Hipp D. A 5-Minute Cognitive Assessment for Safe Remote Use in Patients With COVID-19: clinical Case series. JMIR Form Res. 2021;5(6):1–9. doi:10.2196/26417
19. Ortelli P, Ferrazzoli D, Sebastianelli L, et al. Neuropsychological and neurophysiological correlates of fatigue in post-acute patients with neurological manifestations of COVID-19: insights into a challenging symptom. J Neurol Sci. 2021;420(November 2020):117271. doi:10.1016/j.jns.2020.117271
20. Schild AK, Scharfenberg D, Regorius A, et al. Six-month follow-up of multidomain cognitive impairment in non-hospitalized individuals with post-COVID-19 syndrome. Eur Arch Psychiatry Clin Neurosci. 2024;274(8):1945–1957. doi:10.1007/s00406-024-01863-3
21. Espinar-Herranz K, Delgado-Lima AH, Villatoro BS, et al. Memory, Emotion, and Quality of Life in Patients with Long COVID-19. Brain Sci. 2023;13(12):1670. doi:10.3390/brainsci13121670
22. Ferrucci R, Dini M, Rosci C, et al. One-year cognitive follow-up of COVID-19 hospitalized patients. Eur J Neurol. 2022;29(7):2006–2014. doi:10.1111/ene.15324
23. Mattioli F, Stampatori C, Righetti F, Sala E, Tomasi C, De Palma G. Neurological and cognitive sequelae of Covid-19: a four month follow-up. J Neurol. 2021;268(12):4422–4428. doi:10.1007/s00415-021-10579-6
24. Almeria M, Cejudo JC, Deus J, Krupinski J. Long Neurocognitive and Neuropsychiatric Sequelae in Participants with Post-COVID-19 Infection: a Longitudinal Study. Neurol Int. 2024;16(4):853–868. doi:10.3390/neurolint16040064
25. Almeria M, Cejudo JC, Sanz-Santos J, Deus J, Krupinski J. Impact of COVID-19 infection on cognition and its association with neurological symptoms. Brain Behav. 2023;13(4). doi:10.1002/brb3.2902
26. Flores Lázaro JC, Ostrosky-Solís F. Neuropsicología de Lóbulos Frontales, Funciones Ejecutivas y Conducta Humana. Revista Neuropsicología Neuropsiquiatría Neurociencias. 2008;8:47–58.
27. Anderson P. Executive functions and the frontal lobes. In: Anderson V, Jacobs R, Anderson PJ, editors. Executive Functions and the Frontal Lobes. Taylor y Francis; 2008:3–22.
28. Verdejo-García A, Bechara A. Neuropsicología de las funciones ejecutivas. Psicothema. 2010;22(2):227–235.
29. Ardila A, Ostrosky F. Guía para el diagnóstico neuropsicológico. Revista Int Seguridad Soc. 2012;62(4):127–129. doi:10.1111/j.1752-1734.2009.01350.x
30. Ardila A, Lahiri D. Executive dysfunction in COVID-19 patients. Diabetes Metab Syndr. 2020;14(5):1377–1378. doi:10.1016/j.dsx.2020.07.032
31. Hulley SB, Cummings SR. Diseno de La Investigación Clínica: Un Enfoque Epidemiológico. Ediciones; 2013.
32. Folstein MF, Mchugh SE, Fanjiang PR. Examen Cognoscitivo Mini-Mental (Manual). 2002.
33. Flores JC, Ostrosky-Solís F, Lozano A. Batería de Funciones Frontales: presentación. Revista Neuropsicología Neuropsquiatría Neurociencias. 2008;8:141–158.
34. Sheehan D, McDonagh B, Bárcena JA. MINI international neuropsychiatric interview. Expert Review of Proteomics. 2010;7(1):1–3. doi:10.1586/epr.09.98
35. Organización Mundial de la Salud. Criterios para poner fin al aislamiento de los pacientes de COVID-19. Reseña Científica. 2020;2020:1–5.
36. Gobierno de México. Guía Clínicasss Para El Tratamiento de La COVID-19 En México. 2021.
37. Gignac GE, Szodorai ET. Effect size guidelines for individual differences researchers. Pers Individ Dif. 2016;102:74–78. doi:10.1016/j.paid.2016.06.069
38. Jaywant A, Vanderlind MW, Alexopoulos GS, Fridman CB, Perlis RH, Gunning FM. Frequency and profile of objective cognitive deficits in hospitalized patients recovering from COVID-19. Neuropsychopharmacology. 2021;2021:1–6. doi:10.1038/s41386-021-00978-8
39. Jason LA, Islam MF, Conroy K, et al. COVID-19 symptoms over time: comparing long-haulers to ME/CFS. Fatigue. 2021;9(2):59–68. doi:10.1080/21641846.2021.1922140
40. Crivelli L, Calandri I, Corvalán N, et al. Cognitive consequences of COVID-19: results of a cohort study from South America. Arq Neuropsiquiatr. 2022;80(3):240–247. doi:10.1590/0004-282X-ANP-2021-0320
41. Guedj E, Campion JY, Dudouet P, et al. 18F-FDG brain PET hypometabolism in patients with long COVID. Eur J Nucl Med mol Imaging. 2021;48(9):2823–2833. doi:10.1007/s00259-021-05215-4/Published
42. Douaud G, Lee S, Alfaro-Almagro F, et al. Brain imaging before and after COVID-19 in UK Biobank. medRxiv. 2021;2021:1.
43. Douaud G, Lee S, Alfaro-Almagro F, et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022;604(7907):697–707. doi:10.1038/s41586-022-04569-5
44. Wu Y, Xu X, Chen Z, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun. 2020;87(March):18–22. doi:10.1016/j.bbi.2020.03.031
45. de Melo GD, Lazarini F, Levallois S, et al. COVID-19-related anosmia is associated with viral persistence and inflammation in human olfactory epithelium and brain infection in hamsters. Sci Transl Med. 2021;13(596). doi:10.1126/scitranslmed.abf8396
46. Cysique LA, Jakabek D, Bracken SG, et al. The kynurenine pathway relates to post-acute COVID-19 objective cognitive impairment and PASC. Ann Clin Transl Neurol. 2023;10(8):1338–1352. doi:10.1002/acn3.51825
47. Lopera Restrepo F. Funciones Ejecutivas: Aspectos Clínicos. 2008;8.
48. Davis HE, Assaf GS, McCorkell L, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine. 2021;38:101019. doi:10.1016/j.eclinm.2021.101019
49. Liu YH, Chen Y, Wang QH, et al. One-Year Trajectory of Cognitive Changes in Older Survivors of COVID-19 in Wuhan, China: a Longitudinal Cohort Study. JAMA Neurol. 2022;79(5):509. doi:10.1001/jamaneurol.2022.0461
50. Marjenberg Z, Leng S, Tascini C, et al. Risk of long COVID main symptoms after SARS-CoV-2 infection: a systematic review and meta-analysis. Sci Rep. 2023;13(1). doi:10.1038/s41598-023-42321-9
51. Antonelli M, Penfold RS, Merino J, et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: a prospective, community-based, nested, case-control study. Lancet Infect Dis. 2022;22(1):43–55. doi:10.1016/S1473-3099(21)00460-6
52. Antonelli M, Capdevila Pujol J, Spector TD, Ourselin S, Steves CJ. Risks of long COVID associated with delta versus omicron variants of SARS-CoV2-2. Lancet. 2022;399(10343):2264. doi:10.1016/S0140-6736(22)00946-1
53. Spinicci M, Graziani L, Tilli M, et al. Infection with SARS-CoV-2 Variants Is Associated with Different Long COVID Phenotypes. Viruses. 2022;14(11):2367. doi:10.3390/v14112367
54. Miners S, Kehoe PG, Love S. Cognitive impact of COVID-19: looking beyond the short term. Alzheimers Res Ther. 2020;12(1). doi:10.1186/s13195-020-00744-w
55. Lu Y, Li X, Geng D, et al. Cerebral micro-structural changes in COVID-19 patients – an MRI-based 3-month follow-up study. EClinicalMedicine. 2020;25:100484. doi:10.1016/j.eclinm.2020.100484
56. Kas A, Soret M, Pyatigoskaya N, et al. The cerebral network of COVID-19-related encephalopathy: a longitudinal voxel-based 18F-FDG-PET study. Eur J Nucl Med mol Imaging. 2021;48(8):2543–2557. doi:10.1007/s00259-020-05178-y
57. Hosp JA, Dressing A, Blazhenets G, et al. Cognitive impairment and altered cerebral glucose metabolism in the subacute stage of COVID-19. Brain. 2021;144(4):1263–1276. doi:10.1093/brain/awab009
58. Graham EL, Clark JR, Orban ZS, et al. Persistent neurologic symptoms and cognitive dysfunction in non-hospitalized Covid-19 “long haulers. Ann Clin Transl Neurol. 2021;8(5):1073–1085. doi:10.1002/acn3.51350
59. Galindo-Vazquez Ó, Orozco M, Costas-Muñoz R, Mendoza-Contreras LA, Calderillo-Ruíz G, Menesses-García A. Síntomas de ansiedad, depresión y conductas de autocuidado durante la pandemia de COVID-19 en la población general. Gac Med Mex. 2020;156(4):298–305. doi:10.24875/GMM.20000266
60. Rodríguez-Hernández C, Medrano-Espinosa O, Hernández-Sánchez A. Salud mental de los mexicanos durante la pandemia de COVID-19. Gac Med Mex. 2021;157(3):220–224. doi:10.24875/gmm.20000612
61. Shamah-Levy T, Vielma-Orozco E, Heredia-Hernández O, et al. Encuesta Nacional de Salud y Nutrición 2018–19. Resultados Nacionales. 2020;2020:1.
62. Medina-Mora ME, Borges G, Lara Muñoz C, et al. Prevalencia de trastornos mentales y uso de servicios: resultados de la encuesta nacional de epidemiología psiquiátrica en méxico 1. Artemisa Medigraphic En Línea. 2003;26:1.
63. Pieh C, Budimir S, Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J Psychosom Res. 2020;136:110186. doi:10.1016/j.jpsychores.2020.110186
64. Manchia M, Gathier AW, Yapici-Eser H, et al. The impact of the prolonged COVID-19 pandemic on stress resilience and mental health: a critical review across waves. Eur Neuropsychopharmacol. 2022;55:22–83. doi:10.1016/j.euroneuro.2021.10.864
65. Llana T, Mendez M, Garces-Arilla S, Hidalgo V, Mendez-Lopez M, Juan MC. Association between olfactory dysfunction and mood disturbances with objective and subjective cognitive deficits in long-COVID. Front Psychol. 2023;14. doi:10.3389/fpsyg.2023.1076743.
66. Calabria M, García-Sánchez C, Grunden N, et al. Post-COVID-19 fatigue: the contribution of cognitive and neuropsychiatric symptoms. J Neurol. 2022;269(8):3990–3999. doi:10.1007/s00415-022-11141-8
67. Zacková ML, Jáni MM, Brázdil M, Nikolova YS, Marečková K. Cognitive impairment and depression: meta-analysis of structural magnetic resonance imaging studies. Neuroimage Clin. 2021;32:102830. doi:10.1016/j.nicl.2021.102830
68. Kriesche D, Woll CFJ, Tschentscher N, Engel RR, Karch S. Neurocognitive deficits in depression: a systematic review of cognitive impairment in the acute and remitted state. Eur Arch Psychiatry Clin Neurosci. 2023;273(5):1105–1128. doi:10.1007/s00406-022-01479-5
69. Lorkiewicz P, Waszkiewicz N. Biomarkers of post-COVID depression. J Clin Med. 2021;10(18):4142. doi:10.3390/jcm10184142
70. Taub E, McKay S. Study Details: improving Thinking in Everyday Life After Covid-19|ClinicalTrials.gov. 2020. Available from: https://clinicaltrials.gov/study/NCT04644172.
71. Ownby RL, Kim J. Computer-Delivered Cognitive Training and Transcranial Direct Current Stimulation in Patients With HIV-Associated Neurocognitive Disorder: a Randomized Trial. Front Aging Neurosci. 2021;13. doi:10.3389/FNAGI.2021.766311.
72. Victoria LW, Oberlin LE, Ilieva IP, et al. A digital intervention for cognitive deficits following COVID-19: a randomized clinical trial. Neuropsychopharmacology. 2024;50(2):472–479. doi:10.1038/s41386-024-01995-z
73. Thams F, Antonenko D, Fleischmann R, et al. Neuromodulation through brain stimulation-assisted cognitive training in patients with post-COVID-19 cognitive impairment (Neuromod-COV): study protocol for a PROBE phase IIb trial. BMJ Open. 2022;12(4):e055038. doi:10.1136/BMJOPEN-2021-055038
74. Hagen BI, Lerdal A, Søraas A, et al. Cognitive rehabilitation in post-COVID-19 condition: a study protocol for a randomized controlled trial. Contemp Clin Trials. 2022;122:106955. doi:10.1016/j.cct.2022.106955
75. García-Molina A, García-Carmona S, Espiña-Bou M, Rodríguez-Rajo P, Sánchez-Carrión R, Enseñat-Cantallops A. Neuropsychological rehabilitation for post-COVID-19 syndrome: results of a clinical program and six-month follow up. Neurologia. 2024;39(7):592–603. doi:10.1016/j.nrl.2022.06.008
76. Solana J, Cáceres C, García-Molina A, et al. Improving brain injury cognitive rehabilitation by personalized telerehabilitation services: Guttmann neuropersonal trainer. IEEE J Biomed Health Inform. 2015;19(1):124–131. doi:10.1109/JBHI.2014.2354537
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Exploring Temporal and Intensity Effects of Resistance Exercise on Inhibition: A Four-Arm Crossover Randomized Controlled Trial
Lin TY, Cheng HC, Liu HW, Hung TM
Psychology Research and Behavior Management 2024, 17:1917-1934
Published Date: 8 May 2024

