Back to Journals » Journal of Pain Research » Volume 18
Cortical Activation and Functional Connectivity Response to Different Interactive Modes of Virtual Reality (VR)-Induced Analgesia: A Prospective Functional Near-Infrared Spectroscopy (fNIRS) Study
Authors Deng X , Jiang N, Huang Z , Wang Q
Received 25 September 2024
Accepted for publication 7 January 2025
Published 6 March 2025 Volume 2025:18 Pages 1095—1108
DOI https://doi.org/10.2147/JPR.S492361
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jonathan Greenberg
Xue Deng,1,2 Naifu Jiang,3 Zhaoying Huang,4 Qi Wang5
1Department of Rehabilitation Medicine, The 8th Affiliated Hospital of Sun Yat-Sen University, Shenzhen, Guangdong Province, People’s Republic of China; 2Division of Occupational Therapy, Decker College of Nursing and Health Sciences, Binghamton University, Johnson City, NY, 13902, USA; 3CAS Key Laboratory of Human-Machine intelligence-Synergy Systems, Shenzhen Institutes of Advanced Technology (SIAT), Chinese Academy of Sciences (CAS), Shenzhen, Guangdong Province, People’s Republic of China; 4Department of Rehabilitation, Children’s Hospital of Chongqing Medical University, Chongqing Municipality, People’s Republic of China; 5Prime Physiotherapy Doncaster East, Melbourne, Victoria State, 3109, Australia
Correspondence: Xue Deng, Email [email protected]
Aim: Virtual reality (VR) can be analgesic through intercortical modulation. This study investigated neural activities and correlates during different interactive modes.
Methods: Fifteen healthy participants (4M, 11F, age 21.93 ± 0.59 years) underwent functional near-infrared spectroscopy (fNIRS) to compare cortical activation and functional connectivity (FC) across brain regions of interest (ROI) and channels (CH) during VR experiences. In the active mode (AM), participants engaged with the virtual environment through motor actions. In the passive mode (PM), participants stood still with their eyes closed, listening to the virtual environment’s music.
Results: A better analgesic effect was observed in the AM (t = 3.572, p = 0.001) with higher visual-sensorimotor cortical activation (t = 2.59 to 3.99, p = < 0.001 to 0.015, p-FDR < 0.05). AM showed significant correlations between ratings (pain level and immersion) of VR questionnaire and visual-motor ROIs (r = 0.547 to 0.595, p = 0.013 to 0.038). PM only correlated with pain level and CH 37 (r = 0.608, p = 0.016). FC between S1 and visual-motor-auditory regions was lower in the AM (t = − 4.64 to − 3.53, p = 0.029 to 0.049).
Conclusion: VR-induced analgesia occurs via augmenting the visual-sensorimotor-auditory cortical activation, reducing S1 connectivity and weakening pain processing.
Keywords: virtual reality, analgesia, functional near-infrared spectroscopy, VR, fNIRS, brain mechanism, functional connectivity, cortical activation
Introduction
Virtual reality (VR) is a cutting-edge technological system that can engage users in a virtual world through a variety of equipment, including a head-mounted display (HMD), headphones, and a pair of controllers for interacting with the virtual world.1 By immersing in a completely virtual context, a sensation of real presence in the virtual world can be facilitated by visual, aural, tactile, and olfactory inputs through translocating the user into an immersive 3D virtual context.1,2
In recent years, VR has been found to attenuate pain, and this effect has been called “VR-induced analgesia”.3,4 The majority of its research has been conducted in medical settings to reduce discomfort, anxiety, and pain perception, such as wound care, chemotherapy, dental work, and regular medical checkups and pain management.5–8 Despite this, most of those findings were obtained via subjective reports and clinical evaluation. Since the cortical brain areas have a network of circuits involved in the top-down, bottom-up, and inter-cortical processing of painful signals, there can be a great deal of debate in the absence of a comprehensive explanation of the brain process.1,9
To reveal how the pain circuit works during VR interaction, researchers have only lately started to explore the patient and disorder characteristics, particularly the neural mechanisms that underlie VR, with a small number of clinical studies being conducted via neuroimaging techniques. However, considering the dynamic feature in an open environment during VR interaction, to date, few studies have addressed how VR attenuates pain beyond the basic distraction. Even though a small number of studies using neuroimaging techniques to delineate the brain mechanism of VR-induced analgesia have been conducted, the technical drawbacks cannot be ignored. For instance, functional magnetic resonance imaging (fMRI) as a neuroimaging technique for observing VR interaction can be constrained due to its poor temporal resolution and closed testing environment.10 On the other hand, electroencephalography (EEG) cannot be considered an optimal tool for VR-related mobile tasks in terms of its poor spatial resolution and excessive motion artifacts during mobile tasks.11
In light of this, functional near-infrared spectroscopy (fNIRS), which measures cortical activity and functional connectivity across various brain regions in an open environment by providing complete temporal and spatial resolution, has been developed recently to monitor dynamic, real-time mobile tasks.12 By comparing the subjectively reported pain ratings corresponding to the neural activity in those pain-related cortical brain regions under different interactive modes, our prior research has successfully determined the best VR interactive mode for pain relief.13 Nevertheless, it is yet unknown how the intercortical modulation by VR produces analgesia.
In this study, our main goal is primarily aimed at investigating the properties of intercortical neural activity and correlates under different interactive modes via fNIRS. Its secondary goal was to explore the relationship between subjectively reported VR experience and intercortical activity changes. We hypothesized that inter-cortical activity and correlates involved in pain processing are modulated to produce VR-induced analgesia.
Methodology
This prospective study was approved by the ethical committee of the eighth affiliated hospital of Sun Yat-Sen University, with the clinical trial registered on the Chinese Clinical Trials Registry (reference number: ChiCTR2200061536). Written informed consent was obtained from all participants before the start of the study. The study was conducted under the principles of the Declaration of Helsinki. The null hypothesis posits that there is no significant difference between the two interventions in VR-induced analgesia, which is associated with its cortical activation and functional connectivity.
Subjects
The clinical trial period was performed from Jan 1st, 2022, to March 30th, 2022. We used the data in our previous study for further investigation, with the detailed inclusion/exclusion criteria delineated.13 After enrollment by convenience sampling, a briefing session was facilitated by the researcher to educate participants about the experimental procedures, manipulation of the VR device, and safety precautions. A VR questionnaire (VRQ) consisting of PART I (pre-VR task), PART II (during VR task), and PART III (post-VR task) was provided. Before each round of the VR experimental session, the participant was asked to accomplish part I of the VRQ to report his/her current pain status via the visual-analog scale (VAS) for pain level. Soon after accomplishment of each VR experimental session, they were required to finish part II by recalling his/her VR experience in dimensions of pain level (VRQ_P), attention (VRQ_A), immersion (VRQ_I), and pain distraction (VRQ_PD) as well as part III to report his/her post-VR pain status.
Experimental Paradigm
In this study, the active and passive modes were extracted from our previous study for comparison.13 To avoid the carry-over effect, the interval between each mode was at least 1 day (24 hours). The active mode requires the participant to wield a pair of glowing sabers, slashing a stream of approaching blocks in sync with the song’s beats and notes. Whereas in the passive mode, the participants were required to listen to the music only, with eyes closed and physical motion absent.
The three components of this block study design are the 30-second rest, the 190-second VR task, and the 60-second recovery. Participants were required to remain motionless for 30 seconds while closing their eyes and counting upwards from 1 to 30 seconds. During the 190-second task session, participants were required to follow the interactive guidelines to interact with the VR gaming task: Beat Saber (Beat Games, Czech). At the end, there was a 60-second recovery period. Again, participants were required to remain motionless while counting onward from 1 to 60 seconds while keeping their eyes closed. Throughout each experimental session, the task was performed under continuous electrical stimulation.
fNIRS Measurement
The participant was required to stand comfortably in the laboratory room, with the HMD headset (HTC VIVE Cosmos, HTC/Valve Co.) and the fNIRS cap fixed over his/her head (Figure 1A and B). The 44-channel distribution (18 emission sources, 16 detectors, source-detector separation distance: 3cm) was arranged over the frontal, parietal, temporal and occipital regions, with a brain map displayed in Figure 2.13 A portable and multi-channel near-infrared optical imaging system (NirSmart-6000A, Danyang Huichuang Medical Equipment Co., Ltd., China) was used for observing the hemodynamic response (Sampling frequency: 11Hz, wavelengths: 850mm and 760mm) (Figure 1C). An electric stimuli equipment (YRKJ-F1002, Yirui Co. Ltd., China) was used to generate the noxious stimuli equivalent of 4/10 subjectively reported via visual analog scale (VAS), with two electrical pads placed at the subject’s lumbar L5/S1 level (frequency rate: 1Hz, frequency width: 1ms) (Figure 1A and D).
 |
Figure 2 Channel distribution of the brain map.13 |
fNIRS Data Pre-Processing
The NIRspark (Version 1.7.3, Huichuang, China) based on Matlab (MathWorks, Natick) was used to analyze the experimental data collected by fNIRS. The data was pre-processed in the following steps:
where β ∈ RM×L (where L is the number of measurement channels) represents the relevant response signal strength for either HbO2 or HbR parameters, and X ∈ RN×M indicates the design matrix (where M is the number of data points during the recording period and N is the number of β dimensions).
 |
Figure 3 Illustration of data correction for motion artifact. (A) Before removal of motion artifact, (B) After removal of motion artifact. |
Statistical Analysis
The outcome of active and passive modes in our previous study was extracted for further analysis and comparison.13 SPSS (V24.0, IBM, USA) was utilized for statistical analysis, while GraphPad Prism 8 and the NirSpark software program were used to generate the figures and graphs. To control for the false discovery rate (FDR) in multiple comparisons, we used the Benjamini–Hochberg method, with the adjusted p-values calculated using the formula:
where p represents the smallest p-value in the ordered list, i represents the rank of p(i) in the sorted list, m represents the total number of hypotheses tested and q indicates the desired level of FDR.
The data normality was checked by the Shapiro–Wilk test. Multiple paired t-tests by false discovery rate (FDR) (p < 0.05) were performed to assess cortical activation and functional connectivity between two modes across various ROIs/channels. The association between VRQ items and cortical activation was investigated using Spearman’s rho correlation test.
Results
Demographic Characteristics
As was shown in Table 1, there were 15 right-hand dominant participants, including 4 male and 11 female subjects (average age: 21.93±.59 years) who were enrolled, with no one dropping out throughout the experiment. The mean intensity of electrical stimuli was 23.67±5.69 mA in the active mode and 24.53±5.19 mA in the passive mode, respectively (t=−1.65, p=0.12). Under the consistent intensity of electric stimuli, participants subjectively reported 4/10 via the VAS rating scale during the rest period in each mode, with a diagram in Figure 4 presented in our previous study.13
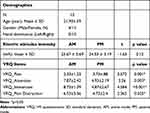 |
Table 1 Descriptive Characteristics13 |
 |
Figure 4 VR questionnaire between active and passive modes. *p<0.05. Abbreviations: VRQ_P, pain level; VRQ_A, attention; VRQ_Imm, immersion; VRQ_PD, pain distraction. |
During VR task period, a better analgesic effect was found in the active mode (VAS: 2.33/10) compared to the passive mode (VAS: 3.73/10) (t=3.572, p<0.001). In addition, a higher level of attention (t=3.26, p=0.003), immersion (t=4.584, p<0.001) and pain distraction (t=2.365, p=0.025) were overall reported in the active mode compared to the passive mode (Table 1 and Figure 4).
Cortical Activation and Its Correlation with VRQ Items
The cortical activation among different brain regions of interest (ROI) associated with its corresponding channels (CH) and Broadman area (BA) in line with the coordinates of Montreal Neurological Institute and Hospital (MNI) between active and passive modes was described in Table 2, Figure 5A and B respectively. By comparing the two modes, significant difference was found in the visual-sensorimotor cortical area, including left dorsolateral prefrontal cortex (LDLPFC [CH16], t=3.05, p=0.005), right dorsolateral prefrontal cortex (RDLPFC [CH14, 15 and 24], t=2.49, p=0.019), left occipital lobe (LOL [CH20-22, 27 and 28], t=0.399, p<0.001), left premotor cortex (LPMC [CH 11 and 17], t=3.31, p=0.003) and left somatosensory cortex (LS1[CH8 and 12], t=2.59, p=0.015) (Table 2, Figure 5A and B). No significant difference was found in the superior temporal gyrus (STG) at both hemispheres (t=0.23 to 1.1, p=0.28 to 0.82).
 |
Table 2 Cortical Activation Between Active and Passive Modes |
 |
Figure 5 Cortical activation between active and passive modes. (A) ROI, (B) Channel. |
On the other hand, Figure 6A and B delineated the correlations between ROI and VRQ items in the active and passive modes, respectively. In the active mode, significant correlations were found between pain level (VRQ_P) and right primary motor cortex (RM1, r=0.595, p=0.022) and right premotor cortex (RPMC, r=0.547, p=0.038), respectively. It was also found that immersion (VRQ_Imm) was significantly correlated with right occipital lobe (ROL, r=0.636, p=0.013) associated with its corresponding CH 17 (r=0.276, p=0.043) and CH 19 (r=0.364, p=0.007) respectively. Whereas in the passive mode, only pain level (VRQ_P) and channel 37 were found significantly correlated (r=0.608, p=0.016).
 |
Figure 6 Heat map of correlation between cortical activation/channel and VRQ items. (A) Active mode, (B) Passive mode. |
Functional Connectivity
The findings are summarized in Tables 3 and 4 and visualized in Figures 7–9, which illustrate both the overall reduction in connectivity and the specific connections affected. The mean functional connectivity in the active mode was significantly lower (ROI-to-ROI: 0.34 ± 0.137; CH-to-CH: 0.185 ± 0.188) than that in the passive mode (ROI-to-ROI: 0.573 ± 0.12; CH-to-CH: 0.415 ± 0.195), indicating reduced connectivity strength during active engagement. This reduction was observed across 17 channel pairs and 14 ROI pairs (CH: t = −4.64 to −3.53, p = 0.029 to 0.049; ROI: t = −4.29 to −2.83, FDR-corrected p = 0.025 to 0.047).
 |
Table 3 Channel-to-Channel Connectivity Strength Between Active and Passive Modes |
 |
Table 4 ROI-to-ROI Connectivity Strength Between Active and Passive Modes |
 |
Figure 7 Connectivity strength between active and passive modes (CHs). (A) Active mode, fc= 0.185 ±0.188), (B) Passive mode (fc= 0.415±0.195). |
 |
Figure 8 Connectivity strength between active and passive modes (ROIs). (A). Active mode (fc= 0.34±0.137), (B) Passive mode (fc=0.573±0.12). |
Specifically, diminished functional connectivity between the primary somatosensory cortex (S1) and visual-motor-auditory regions was evident. These included connections involving:
● Occipital lobe (OL): LS1-ROL (t = −2.93, p = 0.044); RS1-LOL (t = −2.78, p = 0.048).
● Premotor cortex (PMC): LS1-RPMC (t = −3.71, p = 0.033).
● Superior temporal gyrus (STG): LS1-LSTG (t = −2.83, p = 0.047); RS1-LSTG (t = −3.11, p = 0.04).
This reduced functional connectivity suggests that the visual-sensorimotor-auditory cortical regions in the active mode exhibit increased local processing and engagement with the VR environment, leading to a diminished coupling with S1. This decoupling likely disrupts ascending pain signals to S1, thereby contributing to analgesic effects. By contrast, in the passive mode, stronger connectivity might reflect less engagement and a greater reliance on sensory inputs, allowing more pain-related signals to reach S1.
Figures 7–9
- Figure 7A, B, 8A and B display the overall functional connectivity patterns for active and passive modes, demonstrating the interplay between regional activation and functional decoupling.
- Figure 9A and B focus on specific connections, such as S1’s diminished connectivity with visual-motor-auditory areas, highlighting significant ROI-to-ROI and CH-to-CH differences.
These findings align with the hypothesis that active VR engagement alters cortical networks to prioritize dynamic and immersive processing, thereby diminishing pain perception.
Discussion
Previous researchers have examined the neural activities and correlations between brain cortices and neurochemistry as well as the emotional, cognitive, and attention factors to understand the brain mechanism underneath VR-induced analgesia.1 Unlike many prior studies that focus on either active or passive VR experiences with solely subjective questionnaire, our study systematically compares active and passive modes in modulating pain perception using fNIRS, suggesting that active VR reinforces sensorimotor cortical activations, which may play a dual role in pain modulation through physical engagement and cognitive distraction. This dual mechanism provides a nuanced view that reconciles the activation of sensorimotor regions associating an overall diminished functional connectivity with S1, offering novel perspectives on how VR dynamically interacts with pain-processing networks. This finding was in accord with another fNIRS study which examined the analgesic effectiveness of VR versus traditional mindfulness breathing exercises as an analgesic, showing that VR-induced analgesia increases the visual-motor cortical activation while decreasing the functional connection with S1.15 Furthermore, successive studies of VR-induced analgesia using fMRI by Hoffman et al repeatedly demonstrated brain activity increases in regions usually substantially engaged by experimental thermal pain stimulation, which supported the subjective reported pain reduction.16–18 Additionally, an increased activity in the anterior cingulate cortex (ACC) and orbito-frontal regions of the brain may coincide with a general decrease in activity in the pain matrix.3 It is speculated that the pain matrix at the cortical area can be modulated through a comprehensive multi-sensory interaction with the virtual context.
In our experiment, the participants in the active mode were required to slash the virtual blocks in time with the heart-pounding music. It requires judging the speed and direction of the fast-moving virtual blocks and mobilizing their arms at the right time, in the right direction, and to the right location. The analgesia occurs during this complex process, in which pain is modulated through a reconciled process in sensorimotor and cognitive pathways, as evidenced by the increased activity in the DLPFC, PMC, M, and S1 cortical areas. Recent fNIRS studies have shown that physical activities can effectively reduce pain by modulating the motor-related brain region.19–21 On the other hand, a theory of pain attenuation via cognitive distraction proposed by Bantick et al’s fMRI study, revealed a reduction in pain perception associated with a general decline in BOLD signal during the cognitive distraction task, the Stroop test in the insula, thalamus, hippocampus, and mid-cingulate region of the ACC.22 Our findings indicate that the active VR mode can increase sensorimotor activation, while a general decrease in pain-related brain activity may coexist because the two processes may target different neural networks to generate analgesic effect. In other words, the elements of cognitive distraction and physical engagement embedded in the VR context can work in tandem, resulting in a shift of brain activity from pain-related brain regions to sensorimotor regions, thus inhibiting pain processing which aligns with and further extending the existing findings in the VR-induced analgesia studies.3,15
On the other hand, by correlating subjective pain ratings (VAS scores) with neural activity measures (eg, functional connectivity and cortical activation patterns), our study bridges the gap between subjective and objective metrics of pain modulation. This multimodal approach is underexplored in the current literature and adds robustness to the findings. We discovered that in the active mode, there was a substantial correlation between immersion and OL, but not in the passive mode. The OL was activated in the active mode because it required the participants to maintain eye tracking on the moving blocks in the virtual context before precisely cutting the blocks under the active mode, in which a certain level of visual attention is required. It is speculated that individuals may have experienced analgesia as a result of being preoccupied with the rapidly moving virtual blocks. Whereas under the passive mode, the OL was not engaged since the participants closed their eyes during the VR interactive process. Since immersion was found to be strongly connected with both attention and pain distraction in the VRQ, it may suggest that the feeling of immersion can also aid in pain relief. This method was analogous to those cognitive VR tasks that distracted users and reduced their experience of discomfort, with consistent results obtained.23–25
Not to mention, since the gaming rhythm was the same in both modes without blocking auditory processing, no discernible difference in cortical activities of the STG was discovered between the two modes. Based on our experimental design, we assumed that the visual-sensorimotor-auditory cortical area was involved in the active mode, while only the auditory cortex was involved in the passive mode. Our finding was consistent with the assumption of our experimental design. It further implies that a more comprehensive multisensory input within the virtual environment may enhance the effectiveness of the analgesic effects of virtual reality.
In addition to the neural activities in the pain-related ROIs discussed above, we also looked into the functional connectivity that was relevant to VR-induced analgesia to learn more about the brain mechanism involved. The visual-sensorimotor-auditory ROIs showed a closer working relationship in the passive mode. On the other hand, in the active mode, we saw fewer connections among those ROIs. The participants’ visual-sensorimotor-auditory cortical activations were reinforced by the dynamic and immersive virtual experience, depriving the S1 processing of ascending pain inputs. Comparably, Hu et al’s fNIRS study also discovered that individuals with dissociated visual-auditory-DLPFC and PMC areas had reduced pain sensitivity.15 Another fMRI study similarly demonstrated that mediators with dissociated executive and pain-relevant brain areas showed reduced pain sensitivity in a resting state.26 It indicates that a weaker connection between cortical pain-related areas and other areas may prevent the processing of pain.
While it is known that there is top-down modulation of pain signaling via modulating cortical activities and connections by the VR task, there can be something beyond motor and cognitive factors that contribute to VR-induced analgesia. A unique feature of VR which can discriminate it from the conventional approaches is that the virtual context bears the ability to manipulate a far more intricate range of cognitive and affective states. In our experimental scenario, before starting the VR task, the participants were first submerged in a surreal virtual setting with a dark, high-tech background and soothing music, which helped to calm and relax them, successfully separating them from the actual world. When the virtual reality game began, the participants were highly engaged in a very dynamic environment with a heart-pounding pace, requiring them to slice the flying blocks in a mood of excitement and concentration. Naturally, the interaction of the traditional mechanisms or something else entirely could be the source of VR-induced analgesia, in which all those personal (emotion, cognition, and motor) and contextual (task loading, controllability, and rhythm) elements could contribute to pain alleviation.27–30
There were some limitations in this study. The promising result can be biased as the enrolled subjects were all young and healthy. Those brain ROIs we investigated also respond more or less to a range of aversive to non-aversive stimuli and a wide range of task-driven attention, distraction, or affective conditions. The weight of the HMD headset and the fNIRS cap over the scalp may generate some discomfort, yet it can be technically challenging to discriminate the painful stimuli located at the scalp and the lumbar L4/L5 in those studied cortical ROIs. To reduce the influence, a period of 1–2 minutes for adaptation was provided when the devices were put on the scalp. On the other hand, to minimize the statistical interference, semi-automatic detection, and reduction of movement artifacts, a popular data-processing method, was performed based on moving standard deviation and spline interpolation.14 Nevertheless, based on our findings, it is believed that a consistent and more eloquent result can be obtainable when a larger sample size with broader representatives can be enrolled.
Conclusion
VR-induced analgesia occurs when the activities in the pain-related visual-sensorimotor-auditory cortical circuit are augmented, which diminishes its functional connectivity with S1 and consequently weakens the pain processing in S1. The distinction between active and passive VR modes has direct implications for tailoring VR interventions in clinical settings. Our findings suggest that active VR may be particularly effective for engaging sensorimotor pathways, which could inform rehabilitation strategies for conditions like chronic pain or motor impairments.
Data Sharing Statement
The authors confirm their intention to share individual de-identified participant data. The following specific data will be shared: quantitative test scores including participants’ demographics, questionnaire, cortical activation, and functional connectivity measured by functional near-infrared spectroscopy (fNIRS). In addition to the data, the study protocol and informed consent form will be made available. These data and documents will be accessible upon reasonable request via Dr. Xue Deng: [email protected]. Data sharing will commence from the publication date of the article and will remain available for three years.
Funding
This study is sponsored by the Shenzhen Science and Technology Program (Ref. No.: JCYJ20210324115014038), Shenzhen, Guangdong Province of China, and the faculty startup fund by Binghamton University, 13902, New York State, the United States of America.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Li A, Montaño Z, Chen VJ, et al. Virtual reality and pain management: current trends and future directions. Pain Manag. 2011;1(2):147–157. doi:10.2217/pmt.10.15
2. Ansado J, Chasen C, Bouchard S, et al. How brain imaging provides predictive biomarkers for therapeutic success in the context of virtual reality cognitive training. Neurosci Biobehav Rev. 2021;120:583–594. doi:10.1016/j.neubiorev.2020.05.018
3. Gold JI, Belmont KA, Thomas DA. The neurobiology of virtual reality pain attenuation. Cyberpsychol Behav. 2007;10(4):536–544. doi:10.1089/cpb.2007.9993
4. Rutter CE, Dahlquist LM, Weiss KE. Sustained efficacy of virtual reality distraction. J Pain. 2009;10(4):391–397. doi:10.1016/j.jpain.2008.09.016
5. Hoffman HG, Patterson DR, Seibel E, Soltani M, Jewett-Leahy L, Sharar SR. Virtual reality pain control during burn wound debridement in the hydrotank. Clin J Pain. 2008;24(4):299–304.
6. Schneider SM, Workman ML. Effects of virtual reality on symptom distress in children receiving chemotherapy. Cyberpsychol Behav. 1999;2(2):125–134.
7. Alshatrat SM, Alotaibi R, Sirois M, et al. The use of immersive virtual reality for pain control during periodontal scaling and root planing procedures in dental hygiene clinic. Int J Dent Hyg. 2019;17(1):71–76. doi:10.1111/idh.12366
8. Gold JI, SooHoo M, Laikin AM, et al. Effect of an immersive virtual reality intervention on pain and anxiety associated with peripheral intravenous catheter placement in the pediatric setting: a randomized clinical trial. JAMA Netw Open. 2021;4(8):e2122569–e2122569. doi:10.1001/jamanetworkopen.2021.22569
9. Urien L, Wang J. Top-down cortical control of acute and chronic pain. Psychosomatic Med. 2019;81(9):851–858. doi:10.1097/PSY.0000000000000744
10. Hennig J, Speck O, Koch MA, et al. Functional magnetic resonance imaging: a review of methodological aspects and clinical applications. J Magn Reson Imaging. 2003;18(1):1–15. doi:10.1002/jmri.10330
11. Beres AM. Time is of the essence: a review of electroencephalography (EEG) and event-related brain potentials (ERPs) in language research. Appl Psychophysiol Biofeedback. 2017;42(4):247–255. doi:10.1007/s10484-017-9371-3
12. Yücel MA, Selb JJ, Huppert TJ, et al. Functional near infrared spectroscopy: enabling routine functional brain imaging. Curr Opin Biomed Eng. 2017;4:78–86. doi:10.1016/j.cobme.2017.09.011
13. Deng X, Jian C, Yang Q, et al. The analgesic effect of different interactive modes of virtual reality: a prospective functional near-infrared spectroscopy (fNIRS) study. Front Neurosci. 2022;16:1033155. doi:10.3389/fnins.2022.1033155
14. Scholkmann F, Spichtig S, Muehlemann T, et al. How to detect and reduce movement artifacts in near-infrared imaging using moving standard deviation and spline interpolation. Physiol Meas. 2010;31(5):649. doi:10.1088/0967-3334/31/5/004
15. Hu X-S, Beard K, Sherbel MC, et al. Brain mechanisms of virtual reality breathing versus traditional mindful breathing in pain modulation: observational functional near-infrared spectroscopy study. J Med Internet Res. 2021;23(10):e27298. doi:10.2196/27298
16. Hoffman HG, Richards TL, Van Oostrom T, et al. The analgesic effects of opioids and immersive virtual reality distraction: evidence from subjective and functional brain imaging assessments. Anesthesia Analg. 2007;105(6):1776–1783. doi:10.1213/01.ane.0000270205.45146.db
17. Hoffman HG, Richards TL, Coda B, et al. Modulation of thermal pain-related brain activity with virtual reality: evidence from fMRI. Neuroreport. 2004;15(8):1245–1248. doi:10.1097/01.wnr.0000127826.73576.91
18. Hoffman HG, Richards TL, Bills AR, et al. Using FMRI to study the neural correlates of virtual reality analgesia. CNS Spectr. 2006;11(1):45–51. doi:10.1017/S1092852900024202
19. Öztürk Ö, Algun ZC, Bombacı H, et al. Changes in prefrontal cortex activation with exercise in knee osteoarthritis patients with chronic pain: an fNIRS study. J Clin Neurosci. 2021;90:144–151. doi:10.1016/j.jocn.2021.05.055
20. Gentile E, Brunetti A, Ricci K, et al. Movement observation activates motor cortex in fibromyalgia patients: a fNIRS study. Sci Rep. 2022;12(1):4707. doi:10.1038/s41598-022-08578-2
21. Kim H, Jung J, Lee S. Prefrontal cortex activation during diaphragmatic breathing in women with fibromyalgia: an fNIRS case report. Phys Ther Rehabil Sci. 2023;12(3):334–339. doi:10.14474/ptrs.2023.12.3.334
22. Bantick SJ, Wise RG, Ploghaus A, et al. Imaging how attention modulates pain in humans using functional MRI. Brain. 2002;125(2):310–319. doi:10.1093/brain/awf022
23. Piskorz J, Czub M. Distraction of attention with the use of virtual reality. Influence of the level of game complexity on the level of experienced pain. Pol Psychol Bull. 2014;45(4):480–487. doi:10.2478/ppb-2014-0058
24. Lee SY, Cha JY, Yoo JW, et al. Effect of the application of virtual reality on pain reduction and cerebral blood flow in robot-assisted gait training in burn patients. J Clin Med. 2022;11(13):3762. doi:10.3390/jcm11133762
25. Ang S, Montuori M, Trimba Y, et al. Recent applications of virtual reality for the management of pain in burn and pediatric patients. Curr Pain Headache Rep. 2021;25(1):4. doi:10.1007/s11916-020-00917-0
26. Grant JA, Courtemanche J, Rainville P. A non-elaborative mental stance and decoupling of executive and pain-related cortices predicts low pain sensitivity in Zen meditators. Pain. 2011;152(1):150–156. doi:10.1016/j.pain.2010.10.006
27. Seminowicz DA, Davis KD. Interactions of pain intensity and cognitive load: the brain stays on task. Cereb Cortex. 2007;17(6):1412–1422. doi:10.1093/cercor/bhl052
28. Villemure C, Bushnell MC. Mood influences supraspinal pain processing separately from attention. J Neurosci. 2009;29(3):705–715. doi:10.1523/JNEUROSCI.3822-08.2009
29. Salomons TV, Johnstone T, Backonja MM, et al. Perceived controllability modulates the neural response to pain. J Neurosci. 2004;24(32):7199–7203. doi:10.1523/JNEUROSCI.1315-04.2004
30. Keltner JR, Furst A, Fan C, et al. Isolating the modulatory effect of expectation on pain transmission: a functional magnetic resonance imaging study. J Neurosci. 2006;26(16):4437–4443. doi:10.1523/JNEUROSCI.4463-05.2006
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.







