Back to Journals » Infection and Drug Resistance » Volume 18
Cross-District Transmission of Tuberculosis in a High-Mobility City in China: Implications for Regional Collaboration in Infectious Disease Control
Authors Hong C, Ge J, Gui J, Che X, Li Y, Zhuo Z, Li M, Wang F , Tan W, Zhao Z
Received 15 January 2025
Accepted for publication 13 March 2025
Published 19 March 2025 Volume 2025:18 Pages 1551—1560
DOI https://doi.org/10.2147/IDR.S516162
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Sandip Patil
Chuangyue Hong,1,* Jinjin Ge,2,* Jing Gui,1 Xiaoling Che,1 Yilin Li,1 Zhipeng Zhuo,1 Mingzhen Li,1 Feng Wang,1 Weiguo Tan,1 Zhiguang Zhao1
1Department of Tuberculosis Prevention and Control, Shenzhen Center for Chronic Disease Control; Shenzhen Institute of Pulmonology, Shenzhen, 518020, People’s Republic of China; 2National Clinical Research Center for Infectious Diseases, Shenzhen Clinical Research Center for Tuberculosis, Shenzhen Third People’s Hospital, Shenzhen, 518112, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhiguang Zhao, Department of tuberculosis prevention and control, Shenzhen Center for Chronic Disease Control; Shenzhen Institute of Pulmonology, Shenzhen, 518020, People’s Republic of China, Email [email protected]
Objective: This study aims to elucidate the transmission dynamics of tuberculosis in a Chinese city with high population mobility and to identify the associated risk factors.
Methods: We included the data from ten city-level surveillance sites in Shenzhen between 2018 and 2023. Genomic clusters were defined as having a genomic distance of 12 single nucleotide polymorphisms based on whole-genome sequencing. Cross-district clusters were characterized as clusters containing patients from at least two districts, indicating cross-district transmission. Risk factors for clustering were identified using logistic regression.
Results: Of the 2,519 enrolled patients, 263 (10.4%) were grouped into 119 genomic clusters. Notably, 52.1% (62/119) of these clusters were cross-district clusters. We analyzed the data from Shenzhen’s 10 districts separately and compared the results with a citywide combined analysis, finding that the combined analysis revealed significantly higher clustering rates across all districts (P< 0.001). Furthermore, the risk of cross-district transmission was 3.41 times higher (95% CI: 1.49– 7.80) among internal migrants than among residents. Multivariable logistic regression analysis identified significant risk factors for TB transmission, including age under 25 years (OR=3.07, 95% CI: 1.17– 8.03), age 25– 44 years (OR=2.86, 95% CI: 1.13– 7.23), and drug-resistant TB (OR=1.57, 95% CI: 1.15– 2.13).
Conclusion: Cross-district transmission is a key factor in the spread of tuberculosis in cities with high population mobility. TB control institutions at all levels must transcend regional boundaries and enhance collaboration to achieve more effective tuberculosis control.
Keywords: Mycobacterium tuberculosis, cross-district transmission, whole-genome sequencing, risk factors
Introduction
Tuberculosis (TB) remains a critical global health issue, with 10.6 million cases and 1.3 million deaths reported in 2022.1 As one of the countries with the highest TB burden, China has achieved a 3.4% annual reduction in TB incidence since 1990 through the implementation of effective prevention and control strategies. In Shenzhen, the TB incidence rate has fallen to a low-to-moderate level, reaching 27.6 per 100,000 individuals in 2023.2 However, there is still a considerable gap in meeting the World Health Organization’s (WHO) target of ending TB.3 Active case finding is a promising approach, but its success hinges on accurately identifying high-risk populations to allocate resources effectively and enhance intervention outcomes.4,5
The development genomic epidemiology of TB enables detailed mapping of TB transmission networks, analysis of risk factors, and identification of high-risk populations.6,7 Previous genomic epidemiology studies in rural China indicated that approximately 50% of clustered cases were household contacts and social contacts, suggesting the significance of the screening of close contacts.8 In urban China, genomic epidemiology studies found a lower proportion of clustered cases with confirmed epidemiological links.9–11 However, these studies focused on tuberculosis transmission in a single district, often overlooking the potential for cross-district transmission. In urban China, TB transmission chain probably frequently cross multiple districts due to the regular cross-district population movement, which may be rare in rural China.12 This limitation may result in underestimating the level of recent transmission and missing crucial transmission links, thereby failing to explain how transmission occurs. Given that over 80% of Shenzhen’s population is internal migrants, the cross-district transmission of TB is likely to be a significant factor. This highlights the urgent need for a more expansive research in urban areas to comprehensively analyze TB transmission dynamics, thereby facilitating the development of more effective prevention and control strategies.
This study leverages data from ten municipal TB surveillance sites in Shenzhen to address three critical objectives: (1) Characterize clinical and molecular profiles of TB in Shenzhen; (2) Clarify transmission dynamics of TB by mapping transmission chains between districts; (3) Identify high-risk populations associated with recent transmission. By thoroughly capturing cross-district transmission events, this study aspires to establish a robust scientific basis for the development of more precise prevention and control strategies.
Materials and Methods
Sample Source
Shenzhen, located at the southern tip of Guangdong Province, is divided into 10 districts. Each district operates a chronic disease control center serving as a tuberculosis surveillance site, tasked with the diagnosis and treatment of TB within its jurisdiction. The Shenzhen Chronic Disease Control Center (CCDC) is responsible for city-wide diagnosis and surveillance of drug-resistant tuberculosis. For high-risk drug-resistant TB patients who consented to receive treatment in Shenzhen, sputum specimens were collected and cultured. Isolates of Mycobacterium tuberculosis (MTB) obtained from positive cultures were sent to Shenzhen CCDC for drug sensitivity testing (DST) to monitor drug resistance. This study included TB patients 15 years and older who underwent drug resistance surveillance in Shenzhen between January 1, 2018 and June 30, 2023. Strains were excluded if they were duplicates from the same patient, identified as non-tuberculous mycobacteria (NTM), failed re-culture, or exhibited low-quality sequencing data (coverage <95% or depth <20×). Epidemiological data, including age, gender, occupation, and household registration status, were obtained from the China Infectious Disease Surveillance System (CIDSS). This study was approved by the Ethics Committee of the Shenzhen CCDC.
Whole-Genome Sequencing
The isolates were re-cultured and whole genome sequenced. The WGS process and data analysis were performed as previously described.13 The CTAB method was used to extract strain genomic DNA in a brief manner.14 The Illumina HiSeq 2500 platform was used to sequence 300-base-pair double-ended DNA libraries constructed for each isolate. The process involved trimming low-quality reads with Sickle and aligning them to the inferred MTB ancestral sequences using BWA-MEM. To identify single nucleotide polymorphisms (SNPs), the alignments were processed with SAMtools and Varscan. The SNPs with frequency ≥75% were considered to be fixed. Strains with differences of 12 or fewer SNPs were classified as a genomic cluster, indicating linkage through recent transmission.15 Clusters that included patients from two or more districts were termed cross-district clusters. The identified SNPs were used to build a phylogenetic tree with SAM-TB,16 utilizing the maximum likelihood method with 100 bootstraps, and it was visualized through Interactive Tree of Life (https://itol.embl.de/). Strains were grouped into distinct lineages as Liu et al.17 L2 strains, referred to as the Beijing family, were separated into L2.3, denoting “modern” Beijing, and other sub-lineages regarded as “ancient” Beijing.18
Resistance patterns for 17 anti-TB medications were forecasted using SAM-TB, based on mutations linked to resistance.19 Multidrug-resistant TB (MDR-TB) is characterized by resistance to at least the drugs isoniazid and rifampicin, pre-extreme drug-resistant TB (pre-XDR) refers to MDR strains that are additionally resistant to any fluoroquinolone, and strains classified as XDR are those MDR strains that are resistant to any fluoroquinolone and at least one more group A drug.20 Strains with mutations associated with resistance to any drugs but not MDR were termed other drug resistant (DR) TB.
Statistical Analysis
For non-normally distributed continuous data, medians and interquartile ranges (IQR) were used, while proportions described categorical variables. The Wilcoxon rank sum test or chi-square test was employed to test differences between groups. Using logistic regression, the odds ratio (OR) and 95% confidence intervals (CI) were calculated for risk factors connected to genomic clustering. In the multivariable analysis, variables with p-values under 0.2 from the univariable analysis were used to compute the adjusted odds ratios (aOR). Statistical significance in the final model was attributed to factors with a p-value less than 0.05. All analyses were carried out in Stata version 14.0.
Results
General Population Characteristics
Between January 2018 and June 2023, there were 4,020 culture-positive strains in the TB laboratory of Shenzhen CCDC. After excluding 1,021 strains from the same patient, 289 strains classified as NTM, 90 strains failing re-culture, and 101 strains with low-quality sequencing data, the final analysis included 2,519 patients along with their strains. (Figure 1A). The 2,519 TB patients originated from 10 districts in Shenzhen: Baoan District (940, 37.3%), Longhua District (383, 15.2%), Longgang District (311, 12.3%), Guangming District (213, 8.5%), Nanshan District (208, 8.3%), Luohu District (207, 8.2%), Futian District (147, 5.8%), and Pingshan District (71, 2.8%), Yantian District (24, 1.0%) and Dapeng New District (15, 0.6%) (Figure 1B).
 |
Figure 1 Sample enrollment (A) and geographic distribution (B) of patients with tuberculosis in Shenzhen, 2018–2023. The colors represents the number of patients. |
The mean age of TB patients was 33 years (IQR,26–47). Of these patients, 67.3% (1695/2519) were male, and 87.3% (2199/2519) were internal migrants. Regarding occupational distribution, domestic workers and inactive individuals constituted the largest group (45.1%, 1,135/2,519), followed by laborers (30.0%, 755/2,519). New TB patients accounted for 91.4% (2303/2519). The majority of patients (94.2%, 2,373/2,519) were identified through passive case finding.
Genotyping and Drug Resistance Prediction
Genomic analysis indicated that MTB in Shenzhen was predominantly belonged to Beijing family (73.5%, 1851/2519). Among these, 70.7% (1309/1851) belonged to modern Beijing strain, and 29.3% (542/1851) belonged to ancient Beijing strain. The remaining non-Beijing strains included 640 L4 strains, 27 L1 strains, and 1 L3 strain (Figure 2). SAM-TB identified 1772 (70.3%) strains that were susceptible to all anti-TB drugs and 747 (29.7%) strains that were resistant to at least one drug. Of these drug-resistant strains, 262 strains were MDR, 88 were pre-XDR, and one was XDR. Mutations causing resistance to clofazimine and bedaquiline were not identified (Table 1). The highest incidences of drug resistance were observed for isoniazid (17.1%) and rifampicin (15.3%). Among mutations linked to rifampicin resistance, rpoB_S450L (46.6%) was the most prevalent, while katG_S315T (68.3%) was the dominant mutation linked to isoniazid resistance (Supplementary Table S1).
 |
Table 1 Drug Resistance Profile of Mycobacterium tuberculosis Strains Isolated in Shenzhen Based on Genomic Analysis of Drug-Resistant Mutations |
 |
Figure 2 The phylogeny of 2519 Mycobacterium tuberculosis strains isolated in Shenzhen, 2018–2023. |
Risk Factors for Genomic Clustering
To gauge recent transmission levels, we computed the clustering rate. A total of 263 patients (10.4%, 263/2519) were grouped into 119 genomic clusters, of which 99 clusters containing only 2 patients and 20 clusters containing 3–5 patients (Figure 2). Risk factors for genomic clustering were analyzed (Table 2). Risk factors for recent transmission, as shown by the univariate logistic regression analysis, included age, drug resistance profile, and strain lineage. Further analysis using multivariable logistic regression analysis showed a significant difference in clustering rate among different age groups. Patients under 25 years of age (OR=3.07, 95% CI: 1.17–8.03) and aged 25–44 years (OR=2.86, 95% CI: 1.13–7.23) faced higher clustering risks compared to those aged 65 and above. Moreover, DR-TB was found to be an independent risk factor for the recent spread of tuberculosis. Patients with DR had a greater likelihood of clustering than those who were pan-susceptible (OR=1.57, 95% CI: 1.15–2.13).
 |
Table 2 Univariate and Multivariable Logistic Regression of Risk Factors for Genomic Clustering |
Cross-District Transmission
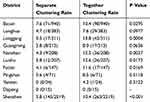
In order to determine the extent of cross-district transmission in Shenzhen, we separately analyzed the data of Shenzhen’s 10 districts and compared the results with citywide together analysis. The together analysis identified 119 clusters, of which 62 (52.1%) contained patients from different districts. Among these cross-district clusters, 5 clusters contained patients from 3 different districts and 57 contained patients from 2 different districts. Notably, 54.8% (144/263) of the 263 clustered cases were part of cross-district clusters. The most frequent cross-district transmission occurred between Bao’an and Longgang districts, representing 16.1% (10/62) of all cross-district transmissions, followed by transmissions between Bao’an and Nanshan districts, which accounted for 12.9% (8/62) (Figure 3). We compared the clustering rates analyzed separately and together (Table 3) and found that together analysis identified significantly higher clustering rates in all districts, except Dapeng District (which had no clustered cases), compared to separate analysis. To comprehend the dynamics of transmission across districts, we studied the share of internal migrants in cross-district clusters. We found that the risk of cross-district transmission was 3.41 times (95% CI:1.49–7.80) higher in internal migrants than in residents, suggesting that internal migrants are likely to be the drivers of cross-district transmission of TB in Shenzhen.
 |
Figure 3 The frequency of clustering between patients from different districts. |
Discussion
It is important to understand the transmission dynamics of TB and its risk factors to develop targeted strategies for prevention and control, including managing outbreaks and preventing the disease from spreading.8 In this study, we analyzed the recent transmission dynamics of TB in Shenzhen using data collected from citywide TB surveillance sites between 2018 and 2023. Our results indicate that more than half of the transmission events involved cross-district transmission. Consequently, restricting the analysis to a single district would have excluded a substantial number of transmission events, potentially underestimating the scale and complexity of TB transmission dynamics in Shenzhen.
Population mobility plays a key role in the transmission of infectious diseases, a fact underscored by the COVID-19 pandemic.21 Despite this, research specifically focusing on the cross - regional spread of TB remains limited. Research in the European Union highlighted that cross-border clusters comprised between 2 and 30 resistant isolates from two to six countries, showing varied RR/MDR-TB transmission patterns in Western and Eastern EU nations.22 Li et al demonstrated that internal migrants significantly contribute to cross-regional TB transmission in China Shenzhen, where the high mobility of the population often results in cross-regional transmission, pointing to the connection between mobility and transmission. However, this research solely utilized data from the Bao’an and Longhua districts in Shenzhen, without considering cross-district transmission within the city.23 Given Shenzhen’s substantial internal mobility, understanding cross - district TB transmission is key for effective prevention and control.24 Our study found frequent transmission between Shenzhen’s districts, with internal migrants as the main risk factor. This frequent transmission risks underestimating TB levels and challenges identifying and intervening in high - risk groups. In high - mobility regions, lack of cross - district coordination can lead to undetected transmission chains and inefficient resource allocation. Shenzhen’s extensive TB spread across districts underscores the importance of surpassing traditional geographic boundaries in TB management. Strengthening resource coordination and district - level collaboration is crucial to address cross - district transmission challenges.
The research discovered that the percentage of clustered cases differed notably among age groups, with individuals under 25 and those aged 25–44 showing much higher clustering risks than those over 65. This indicates that young and middle-aged people frequently transmit the disease, whereas TB in older adults is probably due to endogenous reactivation, aligning with findings from Shanghai.25 This pattern is likely due to the increased social and work activities of young and middle-aged people, who frequently act as the main income providers. Enhancing focused monitoring and educational programs for this demographic is essential to boost awareness of TB prevention and treatment. Additionally, implementing tailored control measures could help mitigate TB transmission in this population. The investigation revealed a significant clustering risk for DR-TB cases in Shenzhen, with drug-resistant TB cases showing a 1.57-fold higher risk of clustering from recent transmission than pan-susceptible cases. This is consistent with earlier research showing that patients resistant to drugs tend to form clusters.26–29 Drug resistance makes treatment more difficult, frequently resulting in longer periods of infection and higher rates of transmission. Improving diagnostic, therapeutic, and management approaches for patients with drug-resistant TB is crucial to reduce transmission.
In China, the majority of MTB strains belong to the Beijing family, which also accounted for over 70% of strains in Shenzhen. Prior studies have demonstrated that Beijing strains exhibit specific traits, including the ability to evade the protective effects of the BCG vaccine, thereby facilitating its effective transmission and contributing significantly to its widespread distribution.30 Differences in lineage distribution emphasize the necessity of adopting region-specific approaches in TB control programs. Research in Central Asia identified a significant link between Beijing strains and the spread of MDR-TB.31 Our research consistently found that Beijing strains are an independent risk factor for recent transmission, which is in agreement with other studies from China.17,32 Rifampicin and isoniazid, as commonly used first-line anti-TB drugs, exhibited the highest risk of developing resistance.33 In this study, isoniazid resistance observed in 17.1% of cases and rifampicin resistance in 15.3%. These rates are notably higher than those for other drugs, consistent with findings by Wang et al.34 Also, no gene mutations associated with resistance to clofazimine or bedaquiline were detected in this study. This finding differs from the results reported by Zhang35 and Karmakar,36 potentially due to the limited use of these two new drugs in China to date.
This study preliminarily investigated the frequency of cross-district transmission in Shenzhen. However, due to the inability to obtain culture-positive strains from all TB patients in Shenzhen for WGS, the sample representativeness in this study is limited, and the clustering rate is likely underestimated. Despite these limitations, our findings underscore that cross-regional transmission is a critical issue meriting further investigation, with important implications for the development and refinement of public health policies. To more accurately characterize this transmission dynamics, future studies should aim to incorporate a larger and more representative sample, employ rigorous data analysis methodologies, and potentially develop transmission models. Such efforts would provide robust scientific evidence to enhance our understanding of TB transmission dynamics in regions with high population mobility and inform targeted public health interventions.
In conclusion, this study analyzed the recent transmission level, risk factors, and cross-district transmission of TB in Shenzhen based on data from citywide surveillance sites. Cross-district transmission constitutes a key driver of tuberculosis spread in mobile populations. Our findings advocate for cross-jurisdictional collaboration among TB control institutions to optimize disease containment strategies.
Ethics Approval Statement
This study was approved by the Ethics Committee of the Shenzhen CCDC (SZCCC-2024-009-01-PJ). Our study complies with the Declaration of Helsinki.
Acknowledgments
We thank the tuberculosis public health teams in the Luohu District Center for Chronic Disease Control, the Futian District Center for Chronic Disease Control, the Nanshan District Center for Chronic Disease Control, the Longgang District Center for Chronic Disease Control, the Longhua District Center for Chronic Disease Control, the Baoan District Center for Chronic Disease Control, the Yantian District Center for Chronic Disease Control, the Guangming District Center for Chronic Disease Control, the Pingshan District Center for Chronic Disease Control, the Dapeng District Center for Chronic Disease Control.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by National Natural Science Foundation of China (82373641) and Guangdong Scientific and Technological Foundation (2020B1111170014).
Disclosure
The authors have declared that they have no conflicts of interest in this work.
References
1. WHO. Global Tuberculosis Report 2023.
2. Wang L, Xu C, Hu M, et al. Spatio-temporal variation in tuberculosis incidence and risk factors for the disease in a region of unbalanced socio-economic development. BMC Public Health. 2021;21(1):1817. doi:10.1186/s12889-021-11833-2
3. WHO. The end TB strategy. Available from: https://www.who.int/publications/i/item/WHO-HTM-TB-2015.19.
4. World Health Organization. WHO Consolidated Guidelines on Tuberculosis. Module 2: Screening - Systematic Screening for Tuberculosis Disease.
5. Bohlbro AS, Hvingelby VS, Rudolf F, Wejse C, Patsche CB. Active case-finding of tuberculosis in general populations and at-risk groups: a systematic review and meta-analysis. Eur Respir J. 2021;58(4):2100090. doi:10.1183/13993003.00090-2021
6. Diel R, Kohl TA, Maurer FP, et al. Accuracy of whole-genome sequencing to determine recent tuberculosis transmission: an 11-year population-based study in Hamburg, Germany. Eur Respir J. 2019;54(5):1901154. doi:10.1183/13993003.01154-2019
7. Leavitt SV, Horsburgh CR, Lee RS, Tibbs AM, White LF, Jenkins HE. What can genetic relatedness tell us about risk factors for tuberculosis transmission? Epidemiology. 2022;33(1):55–64. doi:10.1097/EDE.0000000000001414
8. Li M, Guo M, Peng Y, et al. High proportion of tuberculosis transmission among social contacts in rural China: a 12-year prospective population-based genomic epidemiological study. Emerg Microbes Infect. 2022;11(1):2102. doi:10.1080/22221751.2022.2112912
9. Yang T, Wang Y, Liu Q, et al. A population-based genomic epidemiological study of the source of tuberculosis infections in an emerging city: Shenzhen, China. Lancet Reg Health – West Pac. 2021;8:100106. doi:10.1016/j.lanwpc.2021.100106
10. Li M, Lu L, Guo M, et al. Discrepancy in the transmissibility of multidrug-resistant mycobacterium tuberculosis in urban and rural areas in China. Emerg Microbes Infect. 2023;12(1):2192301. doi:10.1080/22221751.2023.2192301
11. Mijiti P, Liu C, Hong C, et al. Implications for TB control among migrants in large cities in China: a prospective population-based genomic epidemiology study in Shenzhen. Emerg Microbes Infect. 2023;13(1):2287119. doi:10.1080/22221751.2023.2287119
12. He W, Tan Y, Song Z, et al. Transmission dynamics of tuberculosis in a high-burden area of China: an 8-year population-based study using whole genome sequencing. Int J Infect Dis. 2024;147:107210. doi:10.1016/j.ijid.2024.107210
13. Jiang Q, Liu Q, Ji L, et al. Citywide transmission of multidrug-resistant tuberculosis under China’s rapid urbanization: a retrospective population-based genomic spatial epidemiological study. Clin Infect Dis off Publ Infect Dis Soc Am. 2020;71(1):142–151. doi:10.1093/cid/ciz790
14. Schiebelhut LM, Abboud SS, Gómez Daglio LE, Swift HF, Dawson MN. A comparison of DNA extraction methods for high-throughput DNA analyses. Mol Ecol Resour. 2017;17(4):721–729. doi:10.1111/1755-0998.12620
15. Yang C, Luo T, Shen X, et al. Transmission of multidrug-resistant mycobacterium tuberculosis in shanghai, China: a retrospective observational study using whole-genome sequencing and epidemiological investigation. Lancet Infect Dis. 2017;17(3):275–284. doi:10.1016/S1473-3099(16)30418-2
16. Yang T, Gan M, Liu Q, et al. SAM-TB: a whole genome sequencing data analysis website for detection of mycobacterium tuberculosis drug resistance and transmission. Brief Bioinform. 2022;23(2):bbac030. doi:10.1093/bib/bbac030
17. Liu Q, Ma A, Wei L, et al. China’s tuberculosis epidemic stems from historical expansion of four strains of mycobacterium tuberculosis. Nat Ecol Evol. 2018;2(12):1982. doi:10.1038/s41559-018-0680-6
18. Luo T, Comas I, Luo D, et al. Southern east asian origin and coexpansion of mycobacterium tuberculosis Beijing family with han Chinese. Proc Natl Acad Sci. 2015;112(26):8136–8141. doi:10.1073/pnas.1424063112
19. Papaventsis D, Casali N, Kontsevaya I, Drobniewski F, Cirillo DM, Nikolayevskyy V. Whole genome sequencing of mycobacterium tuberculosis for detection of drug resistance: a systematic review. Clin Microbiol Infect. 2017;23(2):61–68. doi:10.1016/j.cmi.2016.09.008
20. WHO. Meeting report of the WHO expert consultation on the definition of extensively drug-resistant tuberculosis. Available from: https://www.who.int/publications/i/item/9789240018662.
21. Iyaniwura SA, Ringa N, Adu PA, et al. Understanding the impact of mobility on COVID-19 spread: a hybrid gravity-metapopulation model of COVID-19. PLOS Comput Biol. 2023;19(5):e1011123. doi:10.1371/journal.pcbi.1011123
22. Tagliani E, Anthony R, Kohl TA, et al. Use of a whole genome sequencing-based approach for mycobacterium tuberculosis surveillance in Europe in 2017–2019: an ECDC pilot study. Eur Respir J. 2021;57(1):2002272. doi:10.1183/13993003.02272-2020
23. Li M, Quan Z, Xu P, Takiff H, Gao Q. Internal migrants as drivers of long-distance cross-regional transmission of tuberculosis in China. Clin Microbiol Infect. 2024;31(1):71–77. doi:10.1016/j.cmi.2024.09.005
24. J ZW, Wei R, M CY, et al. Characteristics of drug resistance in tuberculosis patients of different ages in Guangdong Province from 2014 to 2020 and corresponding prevention and control strategies. J Pract Med. 2024;40(5):702–707.
25. Li M, Lu L, Jiang Q, et al. Genotypic and spatial analysis of transmission dynamics of tuberculosis in shanghai, China: a 10-year prospective population-based surveillance study. Lancet Reg Health – West Pac. 2023;38:100833. doi:10.1016/j.lanwpc.2023.100833
26. Nodieva A, Jansone I, Broka L, Pole I, Skenders G, Baumanis V. Recent nosocomial transmission and genotypes of multidrug-resistant mycobacterium tuberculosis. Int J Tuberc Lung Dis. 2010;14(4):427–433.
27. Yin C, Mijiti X, Liu H, et al. Molecular epidemiology of clinical mycobacterium tuberculosis isolates from southern Xinjiang, China using spoligotyping and 15-locus MIRU-VNTR typing. Infect Drug Resist. 2023;16:1313. doi:10.2147/IDR.S393192
28. Yang C, Shen X, Peng Y, et al. Transmission of mycobacterium tuberculosis in China: a population-based molecular epidemiologic study. Clin Infect Dis off Publ Infect Dis Soc Am. 2015;61(2):219. doi:10.1093/cid/civ255
29. Vyawahare C, Mukhida S, Khan S, Gandham NR, Kannuri S, Bhaumik S. Assessment of risk factors associated with drug-resistant tuberculosis in pulmonary tuberculosis patients. Indian J Tuberc. 2024;71:S44–S51. doi:10.1016/j.ijtb.2023.07.007
30. Grode L, Seiler P, et al. Increased vaccine efficacy against tuberculosis of recombinant mycobacterium bovis bacille Calmette-Guérin mutants that secrete listeriolysin. J Clin Invest. 2005;115(9):2472. doi:10.1172/JCI24617
31. Cox HS, Kubica T, Doshetov D, Kebede Y, Rüsch-Gerdess S, Niemann S. The Beijing genotype and drug resistant tuberculosis in the Aral Sea region of Central Asia. Respir Res. 2005;6(1):134. doi:10.1186/1465-9921-6-134
32. Liu Z, Li X, Xiong H, et al. Genomic and spatial analysis reveal the transmission dynamics of tuberculosis in areas with high incidence of Zhejiang, China: a prospective cohort study. Infect Genet Evol. 2024;121:105603. doi:10.1016/j.meegid.2024.105603
33. Lecai J, Leping Z, Jianwen L, et al. Prediction of drug resistance of multidrug resistant Mycobacterium tuberculosis by whole genome sequencing in Shenzhen. Chin J Tuberculosis. 2021;43(2):166–170.
34. Juhong W, Liping M. Characteristics of gene mutations associated with isoniazid and rifampicin resistance in multidrug resistant Mycobacterium tuberculosis. Inner Mongolia Med J. 2022;54(8):988–990. doi:10.16096/j.carolcarrollnkinmgyxzz.2022.54.08.026
35. Zhang L, Zhang Y, Li Y, et al. Rv1453 is associated with clofazimine resistance in mycobacterium tuberculosis. Microbiol Spectr. 2023;11(5):e00002. doi:10.1128/spectrum.00002-23
36. Karmakar M, Rodrigues CHM, Holt KE, Dunstan SJ, Denholm J, Ascher DB. Empirical ways to identify novel bedaquiline resistance mutations in AtpE. PLoS One. 2019;14(5):e0217169. doi:10.1371/journal.pone.0217169
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Comparative Study on Tuberculosis Drug Resistance and Molecular Detection Methods Among Different Mycobacterium Tuberculosis Lineages
He CJ, Wan JL, Luo SF, Guo RJ, Paerhati P, Cheng X, Duan CH, Xu AM
Infection and Drug Resistance 2023, 16:5941-5951
Published Date: 7 September 2023