Back to Journals » Drug Design, Development and Therapy » Volume 19
Development and Validation of a Population Pharmacokinetics Model of Perampanel for Pediatric Epilepsy Patients for Optimized Dosing
Authors Yu L , Mao F, Chen S, Liu J , Xiao J , Chen M, Luo H, Yu Z , Dai H
Received 3 October 2024
Accepted for publication 16 April 2025
Published 23 April 2025 Volume 2025:19 Pages 3119—3128
DOI https://doi.org/10.2147/DDDT.S499085
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Tamer Ibrahim
Lingyan Yu,1,2 Fengqian Mao,3 Shunan Chen,3 Jieqiong Liu,2,4 Jiayu Xiao,1 Meng Chen,1 Huan Luo,1 Zhenwei Yu,2,4 Haibin Dai1,2
1Department of Pharmacy, Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, 310009, People’s Republic of China; 2Research Center for Clinical Pharmacy, Zhejiang University, Hangzhou, 310058, People’s Republic of China; 3School of Pharmaceutical Sciences, Wenzhou Medical University, Wenzhou, 325035, People’s Republic of China; 4Department of Pharmacy, Sir Run Run Shaw Hospital, Zhejiang University School of Medicine, Hangzhou, 310016, People’s Republic of China
Correspondence: Zhenwei Yu, Sir Run Run Shaw Hospital, Zhejiang University School of Medicine, 3rd East Qingchun Road, Hangzhou, People’s Republic of China, Email [email protected] Haibin Dai, Second Affiliated Hospital, Zhejiang University School of Medicine, 88th Jiefang Road, Hangzhou, People’s Republic of China, Email [email protected]
Background: Perampanel exhibits substantial interindividual variability, and pharmacokinetic data in pediatric patients are scarce. The aim of this study was to develop a population pharmacokinetic (PPK) model to optimize the dosing of perampanel in children with epilepsy.
Methods: The PPK model was developed via a nonlinear mixed-effects modeling approach, utilizing a dataset comprising 454 plasma concentrations of perampanel obtained from 151 pediatric patients with epilepsy, 120 (79.5%) of whom were aged < 12 years. Goodness-of-fit plots and bootstrap analysis were employed to evaluate the final model. Monte Carlo simulations were utilized to suggest perampanel dosing strategies using a reference plasma concentration range of 100– 1000 ng/mL.
Results: In the final PPK models of perampanel, linear centralized age, coadministration of oxcarbazepine (OXC), carbamazepine (CBZ), and valproic acid (VPA) were covariates of clearance (CL/F), and log-transformed body weight was a covariate of the apparent distribution volume (V). The CL/F was estimated via the formula CL/F=0.177*((age+10)/8.8)1.31*1.51OXC*0.745VPA*1.88CBZ. The relative standard errors (RSEs) for each fixed effect parameter were 15.2%, 14.2%, 12.0%, 7.92%, and 16.3%, respectively. The V was estimated via the formula V=227*LGBW with an RSE of 14.1%. The model demonstrated good robustness according to goodness-of-fit plots and bootstrap analysis. The simulation analysis resulted in a dosing regimen stratified by covariates.
Conclusion: A reliable perampanel PPK model for pediatric patients was successfully developed. This result could be helpful for dosing optimization in pediatric patients receiving perampanel, especially those aged under 12 years.
Keywords: perampanel, epilepsy, NONMEM, therapeutic drug monitoring, population pharmacokinetic model
Introduction
Epilepsy is one of the most common chronic neurological problems in children and adolescents, with approximately 3/4 of epilepsy cases occurring in childhood.1–3 It can seriously affect the physical and mental health of children. Pharmacological treatment remains the major option for childhood epilepsy. However, 25–30% of pediatric patients still have poor treatment outcomes and develop refractory epilepsy.4 Therefore, novel antiseizure medications (ASMs) are sorely needed.
Perampanel is a third-generation ASM that is approved as an adjunctive treatment for focal-onset seizures with or without secondary generalization and for primary generalized tonic‒clonic seizures in patients with idiopathic generalized epilepsy.5,6 The broad-spectrum efficacy, favorable cognitive profile, once-daily formulation, and unique mechanism of action of perampanel make it particularly suitable for pediatric patients.7
Perampanel has a narrow therapeutic index and exhibits significant pharmacokinetic variability in pediatric patients, leading to significant variation in its serum concentration.8–10 Some guidelines have suggested the use of therapeutic drug monitoring (TDM) to maintain the concentration of perampanel within a certain range.11 Therefore, there is an urgent need to personalize the dosage regimen for each pediatric patient to improve the efficacy and tolerability of perampanel early, especially for hospitals in which TDM is not available.12,13
However, pharmacokinetic data concerning perampanel in pediatric patients are scarce, especially for those aged under 12 years. The phase I/II/III studies of perampanel were carried out in adults or patients aged over 12 years. Although some population pharmacokinetic (PPK) models are available, these models seldom include pediatric patients aged under 12 years, and the results are contradictory.14–16 Moreover, perampanel is metabolized mainly by CYP3A4 and CYP3A5. The coadministration of enzyme-inducing antiseizure medications (EIASMs) and enzyme-inhibiting ASMs affects the pharmacokinetics of perampanel and increases the variability of drug concentrations.14–16
Considering the need for precision dosing of perampanel in young pediatric patients, this study aimed to develop a PPK model for perampanel in pediatric patients (especially those aged under 12 years) with epilepsy and to identify patient characteristics in terms of perampanel pharmacokinetic parameters, which might facilitate its use in clinical practice.
Methods
Study Design and Ethics Approval
This was a retrospective study. Ethics approval was obtained from the ethics committee of the Second Affiliated Hospital, School of Medicine, Zhejiang University (reference number 2024–0117). The requirement for obtaining informed consent from the patients was waived because of the retrospective nature of the study. This study complied with the Declaration of Helsinki. Patients’ personal information was accessible only to authorized investigators and was not disseminated.
Patient Inclusion
Pediatric patients who had received perampanel from February 2021 to September 2023 in our hospital were retrospectively included according to preset criteria. The inclusion criteria were as follows: (1) pediatric patients who had a diagnosis of epilepsy; (2) patients who received perampanel orally; and (3) patients who underwent TDM during treatment and had at least one perampanel concentration. The exclusion criteria were as follows: (1) age >18 years and (2) insufficient data (lack of BW, height or laboratory examination data during perampanel treatment).
In this study, a comprehensive set of patient data was collected, including demographic characteristics (age, sex, weight and height), blood test results (erythrocytes, albumin, hemoglobin, blood urea nitrogen, creatinine, alanine aminotransferase, aspartate aminotransferase, etc), details of the administration regimen of perampanel (dosage, frequency, time of sampling), coadministration of ASMs, and plasma concentrations of perampanel. The plasma concentration of perampanel was obtained from routine TDM data. In our hospital, perampanel TDM is usually performed 3 weeks after the initiation of perampanel treatment, as perampanel achieves a steady state after 19 days of dosing.17 Blood samples were collected in the morning, approximately 12 h after the previous dose, and the plasma perampanel concentration was determined by the clinical laboratory via a validated HPLC method.18 The range of the method is 15–1500 ng/mL.
PPK Modeling and Validation
The perampanel plasma concentration data were analyzed through the PPK approach via nonlinear mixed effects modeling with the software NONMEM (version 7.5.0, ICON Early Phase, San Antonio, TX, USA) coupled with PsN (version 5.4.0) and Pirana (version 23.1.2, Certara, Radnor, PA, USA) on a personal computer (AMD Ryzen 7 PRO 4750U processor, 16 GM RAM). The first-order conditional estimation method with interaction (FOCE-I) was used for the parameter estimation and model construction process. The selection of the model relies on the minimum objective function value (OFV), and the model is evaluated by means of a goodness-of-fit (GOF) plot. A one- or two-compartment model of primary absorption and elimination was used to describe the pharmacokinetics of perampanel.
The covariates were selected via forward inclusion and backward elimination strategies. The screened covariates included sex, age, weight, height, BSA, BMI, albumin, total protein, alanine aminotransferase, alkaline phosphatase, aspartate aminotransferase, and the perampanel dosing regimen. In addition, the effects of enzyme-induced ASMs (including carbamazepine, oxcarbazepine, and phenytoin), enzyme-inhibited ASMs (sodium valproate), and other ASMs (lacosamide, levetiracetam, zonisamide, etc) were studied. Correlation analyses were performed before covariate modeling. If the correlation coefficient between two variables was > 0.3, one of the variables was selected for inclusion in the model on the basis of whether it was clinically relevant or easy to apply. The effects of continuous covariates were modeled via a median standardized model, whereas the effects of categorical covariates were described via a power model, with covariates included in the model on the basis of a decrease in OFV of 3.84 (p < 0.05) for forward inclusion and an increase in OFV of greater than 10.83 (p < 0.001) for backward exclusion. The final model and parameter estimates were evaluated via GOF plots, bootstrap analysis and visual predictive check (VPC).
Simulation and Dosing Regimen Optimization
On the basis of the final model, Monte Carlo simulations were performed via NONMEM software to optimize the dosing regimen. The lowest dose of perampanel used in clinical practice is 2 mg/d, and a 2 mg/d increment was suggested for adjusting the dose by label. Thus, simulations with different dosing regimens (2 mg/d, 4 mg/d, 6 mg/d, 8 mg/d, 10 mg/d, and 12 mg/d) were performed in pediatric patients stratified by covariates. Each condition was simulated 1000 times. The target stable serum concentration was 100–1000 ng/mL.19 In addition, an optimal dosing was selected when its probability target attainment (PTA) was over 90%.
Results
Patient Inclusion and Characteristics
In total, 454 plasma concentrations from 151 patients were eligible and included in the development of the PPK model. The demographic characteristics of the included patients are shown in Table 1. No included patients had severe hepatic or renal impairment. Notably, 120 (79.5%) patients were aged < 12 years.
 |
Table 1 Characteristics of Studied Pediatric Patients |
PPK Model Development
A one-compartment model with volume of distribution (V) and clearance (CL) as first-order elimination parameters better describes perampanel plasma concentrations. After forward inclusion and backward exclusion of covariates (Table S1), the final model had three covariates on CL/F and one covariate on V, which can be described via equations (1) and (2):
where 0.177 (L/h) is a typical CL/F (L/h) and 227 (L) is a typical V (L) value. Age is the age in years, and OXC, VPA and CBZ represent comedications of oxcarbazepine, sodium valproate and carbamazepine, respectively; these variables (comedication) take a value of 0 when absent and 1 when the drug is administered simultaneously with perampanel. LGBW is the log value of body weight. The detailed parameter estimates of the final model are shown in Table 2.
 |
Table 2 Final Model Estimation Parameters and Bootstrap Analysis results |
Model Validation
The final model was evaluated via GOF plots and bootstrap analysis. The GOF plots revealed acceptable visual bias (Figure 1). The parameter estimates of 1000 bootstrap runs of the final model are presented in Table 2, which are close to the final model estimates and indicate the robustness of the final model. VPC result was shown in Figure S1, which also indicated that the model was reliable.
 |
Figure 1 Goodness-of-fit figures for the final PPK model of perampanel. |
Simulation and Dosing Regimen Optimization
Table 3 shows the simulated mean steady-state plasma trough concentrations of perampanel for each daily dose simulated according to age and body weight, as well as the coadministration regimens. The mean steady-state plasma trough concentrations in patients not coadministered EIASMs were within the therapeutic range when the perampanel dose range was 2–6 mg/d. For a daily dose of 4 mg, all simulation scenarios reached the effective concentration range. The combined use of sodium valproate reduces perampanel clearance with a greater probability of being above the therapeutic range. For patients aged under 4 years, a daily dose of 2 mg seems to be appropriate from the perspective of plasma concentration.
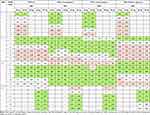 |
Table 3 Median Steady-State Plasma Concentrations (ng/mL) at Different Daily Doses of Perampanel Simulated According to Age, Body Weight and Co-Administration |
Discussion
This retrospective study successfully developed a PPK model for perampanel in pediatric patients. The pharmacokinetics of perampanel were described by a single-compartment model of first-order absorption and elimination, which included age, body weight, concomitant medication, and hepatic function as covariates. This result could be helpful for dosing optimization in pediatric patients receiving perampanel, especially those aged under 12 years.
Pediatric patients of different ages have distinct physiological characteristics and drug in vivo. Compared with other available PPK models, we found that this is the only model that includes a majority of patients aged under 12 years. Renfroe et al developed a PPK in pediatric patients via pooled Phase II and III data.21 This model included 194 patients, but only 41 were aged under 12 years. The median weight was 49.2 kg, with a range of 12.2–121 kg. Takenaka et al developed a PPK model on the basis of data from 1318 patients, of whom only 210 patients were aged 12–18 years.16 Fujita et al developed a PPK model for full ages (0–76 years). However, the sample size was limited (64 patients). The number of pediatric patients in this model is unclear, but the median weight was 50.3 kg, which was closer to that of adults. Thus, these results would be less informative for young children.20 Recently, Li et al published a PPK model focused on pediatric patients. However, the median age and body weight in our study were lower than those in Li’s model, which made our model more informative for young pediatric patients.14 We also included a small portion of patients aged 12–18 years for broader pediatric modeling.
The typical CL/F in our population was 0.177 L/h, which is approximately 50–70% lower than the typical CL/F estimated by Villanueva et al15 (0.729 L/h) and Takenaka et al16 (0.668 L/h) and Silva et al22 (0.419 L/h). This is due to the expression style of the covariate of age. When the median age was used, the typical CL/F was 0.439 L/h, which was close to the reported estimates.
Owing to the large variability of covariates in pediatric patients, we transformed the covariates according to degree of variation. Age was linearly centralized, and body weight was log-transformed and then successfully included in the final model of perampanel in this study. Age is the only physiological parameter that serves as a covariate for CL/F. Li et al’s model included body weight as a covariate for CL/F.14 We believe that these results are in accordance with our findings, as age and body weight are always linearly related in pediatric patients. Other models focused on adults or patients over 12 years of age did not include age or weight as covariates, possibly because of the distribution of patient characteristics.16,20,21 Clearly, V is affected by body weight, and the influence of body weight on V is not negligible in pediatric patients. Owing to the simple nature of current studies, it is difficult to estimate the interindividual viability of V. Some models have fixed V to a reported value or included no covariate on V.14,16,20,21 This approach may be suitable for adult models but is inappropriate for pediatric patients. The Vs of patients aged under 4 years and those aged over 12 years are clearly different. Our study included log-transformed body weight as a covariate for V, which is reasonable and suitable for pediatric patients. This result is supported by published models.22
The interaction between ASMs is an important factor affecting the pharmacokinetics of perampanel. In this study, we found that combining oxcarbazepine and carbamazepine increased the CL/F of perampanel and that combining sodium valproate decreased the CL/F of perampanel. The reason is that perampanel is metabolized predominantly by the cytochrome P450 (CYP) isoform CYP 3A4/5,23–26 and its clearance could be affected by ASMs (and other drugs) that can inhibit or induce CYP3A4/5, which has been extensively characterized and reported in PK analyses in epilepsy patient populations.27–29 Oxcarbazepine and carbamazepine are strong CYP3A4 enzyme inducers that significantly increase perampanel clearance, which is consistent with previous studies.23,30,31 Sodium valproate, an enzyme-inhibiting antiepileptic drug, was previously shown to affect the pharmacokinetics of perampanel, which is consistent with the findings of a published study.32
De Liso et al suggested that the optimal pediatric dosage range for perampanel is 4–12 mg/d, with 8 mg/d most often used.7 US approval of perampanel was based on the results of three multicenter, double-blind, randomized, parallel-group, placebo-controlled Phase III studies at doses of 2, 4, 8 and 12 mg.33–35 The incidence and severity of adverse events (including psychiatric symptoms) can be reduced by starting at a low dose and titrating slowly.7,36 The International League Against Epilepsy and International Consensus Guidelines recommend a therapeutic window for perampanel of 180–980 ng/mL.11,37 The Norwegian Clinical Pharmacology Association has newly established a treatment range of 100–1000 ng/mL.19 Therefore, until more clinical information was available, a wider range of 100–1000 ng/mL was used in this study as the optimal concentration range for perampanel treatment. To achieve blood levels within the therapeutic range, a maintenance dose of 4 mg per day is recommended for pediatric patients who are not coadministered other ASMs. On the other hand, a daily dose of 2 mg is suitable for patients aged under 4 years.
This study had several limitations. Owing to the retrospective, observational nature of this study, some bias may exist. There is no absorption constant available for pediatric patients, and an adult constant was applied in modeling. In addition, the limited sample size hindered comparisons between groups of patients who received perampanel and those who received each type of ASM. Epilepsy types were not included in the analyses. Finally, this model lacks a large number of patients for external validation, which is needed in the future.
Conclusions
A PPK model of perampanel for pediatric patients with epilepsy has been successfully developed. This model included linear centralized age and comedication as covariates for CL/F and log-transformed body weight as covariates for V. This result would be helpful for dosing optimization in pediatric patients receiving perampanel, especially those aged under 12 years.
Data Sharing Statement
All the data are within the manuscript, and further inquiries can be directed to the corresponding authors (Zhenwei Yu and Haibin Dai).
Ethics Approval Statement
Ethics approval was obtained from the ethics committee of the Second Affiliated Hospital, School of Medicine, Zhejiang University (reference number 2024-0117). This study complied with the Declaration of Helsinki. Patients’ personal information was accessible only to authorized investigators and was not disseminated.
Patient Consent Statement
The requirement for obtaining informed consent from the patients was waived as a part of the ethical approval because of the retrospective nature of the study.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Fiest KM, Sauro KM, Wiebe S, et al. Prevalence and incidence of epilepsy. Neurology. 2017;88:296–303. doi:10.1212/WNL.0000000000003509
2. Omran A, Elimam D, Yin F. MicroRNAs: new insights into chronic childhood diseases. Biomed Res Int. 2013;2013:291826. doi:10.1155/2013/291826
3. Guerrini R. Epilepsy in children. Lancet. 2006;367:499–524. doi:10.1016/s0140-6736(06)68182-8
4. Verrotti A, Loiacono G, Coppola G, et al. Pharmacotherapy for children and adolescents with epilepsy. Expert Opin Pharmacother. 2011;12:175–194. doi:10.1517/14656566.2010.517194
5. Steinhoff BJ, Ben-Menachem E, Ryvlin P, et al. Efficacy and safety of adjunctive perampanel for the treatment of refractory partial seizures: a pooled analysis of three phase III studies. Epilepsia. 2013;54:1481–1489. doi:10.1111/epi.12212
6. Leo A, Giovannini G, Russo E, et al. The role of AMPA receptors and their antagonists in status epilepticus. Epilepsia. 2018;59:1098–1108. doi:10.1111/epi.14082
7. De Liso P, Moavero R, Coppola G, et al. Current role of perampanel in pediatric epilepsy. Ital J Pediatr. 2017;43:1–6. doi:10.1186/s13052-017-0368-6
8. Iapadre G, Balagura G, Zagaroli L, et al. Pharmacokinetics and drug interaction of antiepileptic drugs in children and adolescents. Pediatr Drugs. 2018;20:429–453. doi:10.1007/s40272-018-0302-4
9. Wang H, Wang J, Lin B, et al. Effect of age, comedications, and CYP3A4/5 polymorphisms on perampanel exposure in Chinese pediatric patients with epilepsy. J Clin Pharmacol. 2024;64:737–743. doi:10.1002/jcph.2415
10. Ikemoto S, Hamano S, Hirata Y, et al. Efficacy and serum concentrations of perampanel for treatment of drug-resistant epilepsy in children, adolescents, and young adults: comparison of patients younger and older than 12 years. Seizure. 2019;73:75–78. doi:10.1016/j.seizure.2019.10.023
11. Hiemke C, Bergemann N, Clement HW, et al. Consensus guidelines for therapeutic drug monitoring in neuropsychopharmacology: update 2017. Pharmacopsychiatry. 2018;51:9–62. doi:10.1055/s-0043-116492
12. Johannessen Landmark C, Johannessen SI, Patsalos PN. Therapeutic drug monitoring of antiepileptic drugs: current status and future prospects. Expert Opin Drug Metab Toxicol. 2020;16:227–238. doi:10.1080/17425255.2020.1724956
13. Landmark CJ, Johannessen SI, Tomson T. Dosing strategies for antiepileptic drugs: from a standard dose for all to individualised treatment by implementation of therapeutic drug monitoring. Epileptic Disord. 2016;18:367–383. doi:10.1684/epd.2016.0880
14. Li S, Yi J, Tuo YL, et al. Population pharmacokinetics and dosing optimization of perampanel in children with epilepsy: a real-world study. Epilepsia. 2024;65:1687–1697. doi:10.1111/epi.17954
15. Villanueva V, Majid O, Nabangchang C, et al. Pharmacokinetics, exposure–cognition, and exposure–efficacy relationships of perampanel in adolescents with inadequately controlled partial-onset seizures. Epilepsy Res. 2016;127:126–134. doi:10.1016/j.eplepsyres.2016.08.025
16. Takenaka O, Ferry J, Saeki K, et al. Pharmacokinetic/pharmacodynamic analysis of adjunctive perampanel in subjects with partial-onset seizures. Acta Neurol Scand. 2018;137:400–408. doi:10.1111/ane.12874
17. Yu L, Chen M, Liu J, et al. Initial therapeutic target attainment of perampanel in pediatric patients with epilepsy. Front Pharmacol. 2023;14:1209815. doi:10.3389/fphar.2023.1209815
18. Franco V, Marchiselli R, Fattore C, et al. Development and validation of an HPLC-UV assay for the therapeutic monitoring of the new antiepileptic drug perampanel in human plasma. Ther Drug Monit. 2016;38:744–750. doi:10.1097/FTD.0000000000000350
19. Reimers A, Berg JA, Burns ML, et al. Reference ranges for antiepileptic drugs revisited: a practical approach to establish national guidelines. Drug Des Devel Ther. 2018;12:271–280. doi:10.2147/DDDT.S154388
20. Fujita Y, Murai M, Muraki S, et al. Population pharmacokinetic analysis of drug-drug interactions between perampanel and carbamazepine using enzyme induction model in epileptic patients. Ther Drug Monit. 2023;45:653–659. doi:10.1097/FTD.0000000000001055
21. Renfroe JB, Mintz M, Davis R, et al. Adjunctive perampanel oral suspension in pediatric patients from ≥2 to <12 years of age with epilepsy: pharmacokinetics, safety, tolerability, and efficacy. J Child Neurol. 2019;34:284–294. doi:10.1177/0883073819827407
22. Silva R, Colom H, Bicker J, et al. Population pharmacokinetic analysis of perampanel in Portuguese patients diagnosed with refractory epilepsy. Pharmaceutics. 2023;15:1704. doi:10.3390/pharmaceutics15061704
23. Patsalos PN. The clinical pharmacology profile of the new antiepileptic drug perampanel: a novel noncompetitive AMPA receptor antagonist. Epilepsia. 2015;56:12–27. doi:10.1111/epi.12865
24. Schulze-Bonhage A. Perampanel for epilepsy with partial-onset seizures: a pharmacokinetic and pharmacodynamic evaluation. Expert Opin Drug Metab Toxicol. 2015;11:1329–1337. doi:10.1517/17425255.2015.1061504
25. Franco V, Crema F, Iudice A, et al. Novel treatment options for epilepsy: focus on perampanel. Pharmacol Res. 2013;70:35–40. doi:10.1016/j.phrs.2012.12.006
26. Meirinho S, Rodrigues M, Fortuna A, et al. Study of the metabolic stability profiles of perampanel, rufinamide and stiripentol and prediction of drug interactions using HepaRG cells as an in vitro human model. Toxicol Vitr. 2022;82:105389. doi:10.1016/j.tiv.2022.105389
27. Gidal BE, Ferry J, Majid O, et al. Concentration-effect relationships with perampanel in patients with pharmacoresistant partial-onset seizures. Epilepsia. 2013;54:1490–1497. doi:10.1111/epi.12240
28. Gidal BE, Laurenza A, Hussein Z, et al. Perampanel efficacy and tolerability with enzyme-inducing AEDs in patients with epilepsy. Neurology. 2015;84:1972–1980. doi:10.1212/WNL.0000000000001558
29. de Biase S, Gigli GL, Nilo A, et al. Pharmacokinetic and pharmacodynamic considerations for the clinical efficacy of perampanel in focal onset seizures. Expert Opin Drug Metab Toxicol. 2019;15:93–102. doi:10.1080/17425255.2019.1560420
30. Patsalos PN, Gougoulaki M, Sander JW. Perampanel serum concentrations in adults with epilepsy: effect of dose, age, sex, and concomitant anti-epileptic drugs. Ther Drug Monit. 2016;38:358–364. doi:10.1097/FTD.0000000000000274
31. Lin CY, Chang CW, Tseng WEJ, et al. Therapeutic drug monitoring of perampanel: clinical utility and impact of co-medication on pharmacokinetic variability. Heliyon. 2024;10:e23962. doi:10.1016/j.heliyon.2023.e23962
32. Contin M, Bisulli F, Santucci M, et al. Effect of valproic acid on perampanel pharmacokinetics in patients with epilepsy. Epilepsia. 2018;59:e103–8. doi:10.1111/epi.14446
33. French JA, Krauss GL, Biton V, et al. Adjunctive perampanel for refractory partial-onset seizures: randomized phase III study 304. Neurology. 2012;79:589–596. doi:10.1212/WNL.0b013e3182635735
34. French JA, Krauss GL, Steinhoff BJ, et al. Evaluation of adjunctive perampanel in patients with refractory partial-onset seizures: results of randomized global phase III study 305. Epilepsia. 2013;54:117–125. doi:10.1111/j.1528-1167.2012.03638.x
35. Krauss GL, Serratosa JM, Villanueva V, et al. Randomized phase III study 306 adjunctive perampanel for refractory partial-onset seizures. Neurology. 2012;78:1408–1415. doi:10.1212/WNL.0b013e318254473a
36. Ettinger AB, LoPresti A, Yang H, et al. Psychiatric and behavioral adverse events in randomized clinical studies of the noncompetitive AMPA receptor antagonist perampanel. Epilepsia. 2015;56:1252–1263. doi:10.1111/epi.13054
37. Patsalos PN, Spencer EP, Berry DJ. Therapeutic drug monitoring of antiepileptic drugs in epilepsy: a 2018 update. Ther Drug Monit. 2018;40:526–548. doi:10.1097/FTD.0000000000000546
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



