Back to Journals » Infection and Drug Resistance » Volume 18
Distribution and Antibiotic Resistance Analysis of 13,048 Clinically Common Isolates
Authors Zhao J, Yue P, Li ZJ, Xu T, Xing GZ, Shao Y, Yu HY
Received 10 December 2024
Accepted for publication 11 February 2025
Published 24 February 2025 Volume 2025:18 Pages 1071—1081
DOI https://doi.org/10.2147/IDR.S510193
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Jing Zhao,1,* Peng Yue,2,* Zhi-jie Li,3,* Ting Xu,1 Guo-zheng Xing,1 Yan Shao,1 Hong-yuan Yu1
1Department of Clinical Laboratory, Beijing Aerospace General Hospital, Beijing, People’s Republic of China; 2Northern Medical Branch of PLA General Hospital, Haidian, Beijing, 100080, People’s Republic of China; 3Obstetrics and Gynecology, Beijing Aerospace General Hospital, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hong-yuan Yu, Email [email protected]
Objective: This study investigated the distribution and antibiotic resistance profiles of common bacteria isolated from clinical specimens at a hospital’s microbiology laboratory between 2020 and 2022.
Methods: A retrospective analysis was conducted on microbial culture results from clinical specimens collected over three years, including sample types, departmental distribution, pathogen species, and resistance profiles.
Results: A total of 13,048 unique pathogenic strains were isolated, predominantly from respiratory and urine specimens. Secretion specimens exhibited the highest positive detection rate (73.6%), while blood specimens showed a lower rate (9.7%). The five most frequently isolated pathogens were: Klebsiella pneumoniae (K. pneumoniae) (19.6%), Pseudomonas aeruginosa (P. aeruginosa) (14.7%), Escherichia coli (E. coli) (9.2%), Acinetobacter baumannii (A. baumannii) (8.0%), and Candida albicans (C. albicans) (7.0%). Gram-negative bacteria constituted 53.7% of all isolates (7009/13,048). A total of 7590 multidrug-resistant organisms (MDRO) were identified, corresponding to a detection rate of 21.3% (7590/35,613). The detection rates of carbapenem-resistant Enterobacteriaceae (CRE) increased annually: 7.2% (2020), 8.6% (2021), and 14.4% (2022).
Conclusion: The annual detection rate of CRE increased during the study period, while the rate of methicillin-resistant Staphylococcus aureus (MRSA) declined. Timely and effective interventions targeting pathogenic bacteria are essential for controlling and mitigating nosocomial infection risks.
Keywords: multidrug-resistant organisms, monitoring, hospital infection, prevention and control, CRE
Introduction
The emergence of antibiotic resistance and MDRO has become a critical global public health threat.1,2 Bacteria entering the bloodstream via intestinal mucosa or intravenous catheters encounter selective pressures distinct from those colonizing the skin or gut, such as nutrient availability, host immune responses, and antibiotic concentrations.3,4 The frequent use of central venous catheters, invasive procedures, and surgeries in hospital settings provides pathways for hospital-acquired pathogens to enter the bloodstream. While bacterial resistance occurs naturally, the misuse of antimicrobial agents in humans and animals has significantly accelerated the development of antibiotic resistance.5 As major pathogens in hospital-acquired infections, MDROs remain a critical focus of infection control efforts,6 leading to higher inpatient mortality rates, severe complications, increased healthcare costs, prolonged hospital stays, and worse prognoses.7 The resistance patterns and distribution of clinically isolated bacteria differ across countries, regions, and hospitals.8,9 Enterococcus species are major pathogens commonly associated with urinary tract infections and surgical site infections.10,11 Vancomycin-resistant Enterococcus faecium (VREfm) has shown an increasing prevalence in multiple countries,12–15 particularly colonizing and infecting patients undergoing hematopoietic stem cell transplantation and chemotherapy.16 Vancomycin resistance may be associated with a higher mortality rate.17 Fungal resistance is also a significant concern; studies have reported that the increase in Candida glabrata (C. glabrata) infections may be linked to the rising use of fluconazole, particularly among hematological patients receiving prophylactic treatment.18 There are regional differences in species distribution; in China, Candida tropicalis(C. tropicalis) ranks third in the frequency of isolation from candidemia, accounting for 18.7%.19 The aging hospitalized population may contribute to rising resistance rates, as older patients are often colonized by these strains in their gastrointestinal tracts. The persistent presence of MDRO in hospital environments poses a significant threat to patient safety. We noted a lack of standardization in result reporting, healthcare cost information, and advanced microbial species identification methods, which should be addressed in future studies. This study retrospectively analyzed the distribution and resistance patterns of major pathogens isolated between 2020 and 2022, aiming to identify prevalence trends, evaluate infection control measures, and provide guidance for the rational use of antibiotics in clinical practice.
Materials and Methods
Data Source
This study employed a retrospective survey method, selecting 13,048 isolates from various clinical specimens submitted to the microbiology laboratory of a tertiary hospital between 2020 and 2022. The selected specimen types included sputum, blood, urine, bronchoalveolar lavage fluid (BALF), catheter and wound secretions from patients. For specimens that are small and difficult to collect, sterile cotton swabs are used to obtain samples. Duplicate strains from the same patient for the same specimen type were excluded, with only the first result being recorded. Statistical analysis was performed on the types of positive cultures collected and their corresponding clinical departments.
Methods
Antimicrobial susceptibility testing (AST) was performed using the Vitek 2-Compact automated system (bioMérieux, France) with AST-N335, AST-N334, and AST-GN639 cards. Bacterial identification was conducted using the same system with corresponding Gram-positive and Gram-negative identification cards.
Specimen pre-processing and bacterial culture were conducted according to the “National Clinical Laboratory Operating Procedures”. Antimicrobial susceptibility testing adhered to the guidelines set by the Clinical and Laboratory Standards Institute (CLSI).20 MDR bacteria were defined as those resistant to three or more structurally unrelated antimicrobial agents. ESBL determination was based on the results of third- and fourth-generation cephalosporins using a detection panel, with tested antibiotics including cefepime (FEP), cefotaxime (CTX), ceftazidime (CAZ), cefepime/clavulanic acid (FEP/CA), ceftazidime/clavulanic acid (CAZ/CA), and cefotaxime/clavulanic acid (CTX/CA). Phenotypic confirmation tests were conducted using the K-B disk diffusion method in accordance with CLSI M100 guidelines. CRE are defined as organisms resistant to at least one of the carbapenems: imipenem (IPM), meropenem (MEM), or ertapenem (ETP). Interpretative criteria were categorized into three levels: susceptible(S), intermediate(I), and resistant(R).
Statistical Analysis
Bacterial resistance data were processed using the WHONET 2023 software, and statistical analysis was performed on the specimen sources, species, composition, departmental distribution, antimicrobial susceptibility results, and resistance patterns of the clinical isolates. Categorical data were presented as frequencies or percentages. The χ²-test was applied to analyze the differences in resistance rates using R × C tables. Linear association χ² values were used to assess trends across different years. A P-value of <0.05 was considered statistically significant.
Results
Distribution of Isolated Pathogenic Bacteria
Between 2020 and 2022, the COVID-19 pandemic and related control measures significantly reduced public mobility, leading to a notable decline in the number of people seeking medical care. A total of 35,613 clinical specimens were submitted for examination, yielding 13,048 unique isolates, resulting in an overall positivity rate of 36.6%. Among these, respiratory specimens accounted for 61.6%, urine samples for 22.9%, blood cultures for 8.8%, secretions for 4.7%, catheters for 1%, and pleural/peritoneal fluid for 0.6% (Table 1). Notably, secretions exhibited the highest positivity rate at 73.6%, whereas blood cultures had a lower positivity rate of only 9.7%. The primary sources of specimens were the Respiratory Department (20.1%), the Geriatrics (16.5%), the Intensive Care Unit (ICU) (13.6%), the Neurology Department (10.7%), the Respiratory Intensive Care Unit (RICU) (9.0%), and the Neurosurgery Department (7.5%) (Figure 1).
 |
Table 1 Bacterial Culture Positive Rates and Distribution of Isolated Bacteria |
Distribution Characteristics of Isolated Strains
Among the 13,048 isolated strains, the top 10 pathogens included five Gram-negative bacteria, totaling 7009 strains (53.7%), four Gram-positive bacteria with 2560 strains (19.6%), and 917 fungal strains (7.0%). The five most prevalent Gram-negative bacteria were K. pneumoniae (19.6%, 2132/13,048), P. aeruginosa (14.7%, 1922/13,048), E. coli (9.2%, 1198/13,048), A. baumannii (8.0%, 1048/13,048), and Pseudomonas maltophilia (P. maltophilia) (5.4%, 709/13,048). The four most common Gram-positive bacteria were Enterococcus faecium(E. faecium) (6.6%), Staphylococcus epidermidis(S. epidermidis) (5.0%), Staphylococcus aureus(S. aureus) (4.6%), and Staphylococcus haemolyticus (S. haemolyticus) (3.5%). The predominant fungal species identified was C. albicans, ranking fifth with a total of 917 strains.
Comparative Antimicrobial Susceptibility Results of Major Gram-Negative Bacteria
The resistance rates of isolated bacteria to antimicrobial agents vary significantly, as demonstrated in Table 2, which presents the average resistance rates of major isolated Gram-negative bacteria. Susceptibility testing results indicate that clinical strains of K. pneumoniae exhibit a resistance rate exceeding 30.0% to various antimicrobial agents, with multiple resistant strains detected for commonly used carbapenems. Analysis of isolated E. coli strains reveals high resistance rates to piperacillin (PIP) (75.5%), ciprofloxacin (CIP) (74.9%), ampicillin/sulbactam (SAM) (72.0%), levofloxacin (LVX) (67.8%), and ceftriaxone (CRO) (64.1%), all exceeding 60%, suggesting avoidance in clinical use. A total of 93 strains of imipenem-resistant (IPM) bacteria (7.8%) and 51 strains of meropenem-resistant (MEM) bacteria (4.2%) were identified. While the overall resistance rate remains relatively low, it is still higher than the national average of 1.5% reported by China Antimicrobial Resistance Surveillance System (CARSS) for E. coli resistance to carbapenems in 2022. P. aeruginosa shows a generally low overall resistance rate, below 30.0%, with no resistant strains of polymyxin B detected. In contrast, A. baumannii exhibits an overall resistance rate exceeding 45.0%, though it shows lower resistance rates to trimethoprim-sulfamethoxazole (SXT), minocycline (MDO), and tigecycline (TGC) (37.6%, 16.0%, and 4.0%, respectively), making these options preferable for clinical use.
 |
Table 2 Average Resistance Rates of Gram-Negative Bacteria to Common Antimicrobials |
Comparative Antimicrobial Susceptibility Results of Major Gram-Positive Bacteria
The average resistance rates of major isolated Gram-positive bacteria are presented in Table 3, indicating significant variability in resistance to various antimicrobial agents. Susceptibility testing results reveal that the average resistance rate of S. aureus to penicillin G (PEN) is 84.6%, lower than the CARSS-reported rate of 91.4% in 2022, with no vancomycin-resistant S. aureus (VRSA) detected. S. epidermidis exhibits high resistance rates to benzylpenicillin (OXA) (92.9%), PEN (97.8%), and LEV (71.9%), rendering them unsuitable for clinical use. The isolated S. haemolyticus demonstrates high resistance rates to Penicillins, Fluoroquinolones, and Macrolides. Notably, all three Staphylococcus species showed 100% susceptibility to linezolid (LNZ) and tigecycline (TGC), as well as high susceptibility to vancomycin (VAN). In contrast, E. faecium displays a VAN resistance rate of 10.6%. Detailed susceptibility results are shown in Table 3.
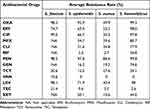 |
Table 3 Average Resistance Rates of Gram-Positive Bacteria to Common Antimicrobial Agents |
Antimicrobial Susceptibility Analysis of Key Multidrug-Resistant Organisms (MDRO)
Over three years, a total of 7590 MDRO were identified, with a detection rate of 21.3% (7590/35,613) (Table 4). K. pneumoniae was the most frequently detected species, with significant increases in 2021 compared to the other two years, along with E. faecium, S. epidermidis, and Proteus mirabilis (P. mirabilis). A downward trend was observed in 2022. The resistance rate of P. aeruginosa in 2021 was lower than in 2020 (9.1% vs 11.4%), but it surged to 12.8% in 2022. A. baumannii, E. cloacae, and Enterococcus faecalis (E. faecalis) exhibited a steady increase year by year (Figure 2). The prevalence of S. aureus showed a slight increase in 2022, remaining below the overall three-year proportion (8.8% vs 9.4%). Among them, methicillin-resistant Staphylococcus aureus (MRSA) accounted for 381 strains over three years, with respective proportions of 6.2% (134/2176), 5.2% (139/2689), and 4.0% (108/2725), demonstrating a declining trend.
 |
Table 4 Trends of MDRO Detection Rates From 2020 to 2022 [n (%)] |
Analysis of Trends in Carbapenem-Resistant Organism (CRO)
The detection of CRE yielded 157, 230, and 392 strains in the respective years, corresponding to detection rates of 7.2%, 8.6%, and 14.4%, indicating a progressive annual increase (Figure 3). Trend chi-square tests were performed to statistically analyze the resistance patterns of K. pneumoniae, E. coli, P. aeruginosa, and A. baumannii against IPM and MEM over the three years, using all detected strains (without exclusion of duplicates). The resistance rate of Carbapenem-Resistant K. pneumoniae (CRKP) to MEM increased sharply from 36% in 2020 to 74.9% in 2021, with a slight decrease in 2022 (74.1% vs 74.9%) (Figure 4A). The resistance of Carbapenem-Resistant E. coli (CREC)showed a consistent year-over-year decline (Figure 4B). Carbapenem-Resistant P. aeruginosa (CRPA) demonstratedin 2021, compared to 2020 and 2022, with relatively stable changes over the three years (Figure 4C). The Carbapenem-Resistant Acinetobacter baumannii (CRAB) exhibited a yearly increase in resistance to MEM, with a significant rise in resistance to IPM in 2022 compared to 2021 (69.1% vs 53.3%) (Figure 4D). Pearson’s chi-square test showed no statistically significant difference in E. coli resistance to MEM, while the resistance rates of IPM and MEM for the other three bacteria were statistically significant (P < 0.05), suggesting that the resistance to these antibiotics varied among the three species (Table 5). Linear association tests indicated a linear increasing trend in the resistance rates of IPM and MEM against K. pneumoniae, P. aeruginosa, and A. baumannii, and a linear increase in the resistance rate of E. coli to IPM over the three years.
 |
Table 5 Three-year Trends in CRO |
 |
Figure 3 The detection of CRE among MDRO from 2020 to 2022 shows the number of CRE detected each year among the main MDRO in clinical specimens submitted for testing. |
Discussion
The global spread of COVID-19 has heightened awareness of antimicrobial resistance, underscoring the importance of antibiotic stewardship. Health authorities must enforce regulations on antibiotic use, while healthcare institutions should take responsibility for their appropriate use to minimize unnecessary prescriptions. Clinical microbiology laboratories must enhance the positive detection rates of pathogens to provide comprehensive diagnostic information for timely diagnosis and treatment. This study identifies 13,048 unique strains isolated from a hospital between 2020 and 2022, with an overall positivity rate of 36.6%. Sputum specimens accounted for the highest positivity rate at 55.0%, followed by secretions at 73.6%. Notably, blood and urine samples showed significantly lower submission rates compared to respiratory specimens. Compared with national data, the quantities and positivity rates of sputum and urine samples were similar,21,22 while the blood positivity rate was only 8.8%. Various domestic studies report blood culture positivity rates between 5.30% and 9.96%,23,24 indicating a consistently low level. Blood cultures, considered the “gold standard” for diagnosing bloodstream infections, are influenced by the volume of blood collected. Clinicians must familiarize themselves with the indications for blood culture collection and ensure timely submission per standard to facilitate effective antibiotic selection.
Analysis of specimen results revealed that the primary pathogens in blood samples were K. pneumoniae (19.0%), E. coli (18.0%), and S. aureus (14.0%). While S. aureus is a normal skin commensal, its relatively high detection rate necessitates caution in specimen collection and treatment decisions to avoid misinterpretation due to false positives. Data from specimen submission departments indicated that the highest pathogen isolation rates were from the respiratory department (20.1%), geriatric department (16.5%), and ICU (13.6%), primarily sourced from respiratory illnesses, geriatric patients, and critically ill individuals, who are often at higher risk for colonization and infection. Over the three-year period, the detection rate of Gram-negative bacteria remained consistently high, with minimal fluctuations. Major pathogens associated with hospital infections included K. pneumoniae, P. aeruginosa, E. coli, A. baumannii, and E. faecium. Notably, the isolation rate of E. faecium surpassed that of S. aureus in other large teaching hospitals,25 which may relate to regional pathogen prevalence and variations in clinical prescribing practices.
The detection rate of MDRO is a vital indicator of the prevalence of resistance within hospitals.26 This study indicates an overall MDRO detection rate of 21.3%, higher than findings from other hospitals.27 Specifically, 5066 multidrug-resistant strains were identified in sputum, predominantly K. pneumoniae (23.0%). In midstream urine, E. coli (27.0%) led, followed closely by K. pneumoniae and E. faecium, confirming the dominance of Gram-negative bacteria. Importantly, the positive detection rate of MRSA declined annually, significantly below the national average of 28.9% reported by CARSS in 2022. This trend may correlate with environmental factors, distribution patterns of hospital pathogens, clinical prescribing habits, and infection control measures.
Despite the low isolation rate of E. faecium in clinical specimens, its high resistance to common antibiotics remains a concern. Molecular techniques to detect Van A and Van B resistance genes could provide rapid guidance for antibiotic selection. The resistance mechanisms of Gram-negative bacteria are complex, posing a significant challenge, particularly with ESBL-producing strains, which considerably limit clinical treatment options. Resistance genes may spread via plasmids among bacteria, increasing the risk of clinical MDRO infections and complicating infection control efforts.
Regarding carbapenem antibiotics, these are the most effective β-lactam agents for treating severe infections caused by multidrug-resistant Enterobacteriaceae.28 The study indicates a consistent annual increase in CRE detection rates at the hospital (7.2%, 8.6%, 14.4%), with a significant rise. Among them, CRAB showed a notable increase in MEM resistance in 2022 compared to 2021 (69.1% vs 53.3%), while CRKP exhibited a rapid rise in MEM resistance from 36% in 2020 to 74.9% in 2021. This rate is significantly higher than the national average of approximately 20% for K. pneumoniae resistance to IPM and MEM based on the 49,150 strains reported by 2004 China Antimicrobial Surveillance Network (CHINET) in 2021. This trend may be linked to the concentration of specimen submissions from the respiratory, geriatric, and ICU departments distribution is relatively concentrated, where patients tend to be elderly, immunocompromised, and have prolonged hospital stays, thereby increasing the risk of K. pneumoniae infections. To address the rise in resistant strains and significant rates of multidrug resistance, a thorough analysis of the underlying causes is essential, including compliance with specimen collection protocols and potential incidences of nosocomial infections or laboratory contamination. Infection control departments should prompt clinical units to review the distribution of pathogens and changes in resistance rates, adjusting control strategies accordingly. Ensuring compliance with specimen collection requirements and adapting clinical antibiotic strategies based on culture and sensitivity results is crucial. This study found that the resistance rate of K. pneumoniae to Carbapenem drug MEM has remained high since 2021 (74.9% and 74.1%). The resistance rates of E. coli, P. aeruginosa, and A. baumannii have shown an upward trend, and are higher than the national average. Lucia Boccabella et al15 indicated that during the COVID-19 pandemic, the use of personal protective equipment (PPE) initially masked the scale and proportion of antimicrobial resistance (AMR). In the early stages of the SARS-CoV-2 pandemic, the overuse and misuse of antibiotics, increased preventive measures, and PPE shortages, which led to untimely replacement, contributed to uncontrolled transmission of resistant microorganisms. As lockdown measures were reduced and lifted, the indiscriminate transmission of resistant microorganisms occurred, leading to the emergence of new multidrug-resistant strains. The diagnosis and treatment of resistant microorganisms remain challenging; the regulation of antibiotic use should be sustained, and strict infection control measures, including environmental disinfection, hand hygiene, and bedside isolation, must be strictly implemented.29 The data collected in this study cover a relatively short period of time. We will continue to gather post-pandemic antimicrobial resistance information in the future to provide more valuable insights for clinical treatment and the control of resistant bacteria.
Globally, the struggle between bacterial resistance and antibiotic development continues. In clinical practice, effective communication among departments is vital to promptly understand antibiotic use in complex and critically ill patients, allowing for more precise adjustments in antibiotic therapy. Additionally, efforts should be made to shorten the turnaround time (TAT) for microbiological reports. All professional groups should actively participate in infection control initiatives, establishing long-term strategies for rational antibiotic use. The pharmacy department should lead joint oversight of antibiotic stewardship, while clinical units must enhance cleaning and disinfection of frequently touched surfaces and conduct screening for at-risk individuals upon admission, reinforcing infection control guidance and management responsibilities. Moreover, timely adjustments to antibiotic usage guidelines are necessary to further strengthen infection control measures and ensure effective management of hospital-associated infections.
Conclusion
This study demonstrates that the antimicrobial resistance status of clinical isolates in the hospital has been severe over the past three years, with the detection rate of CRE increasing annually and that of MRSA decreasing yearly. This may be related to timely and effective targeted actions against MRSA in the early stages, which effectively controlled and reduced its hospital transmission. During the pandemic, overuse and misuse of antibiotics, increased preventive measures, and PPE shortages leading to untimely replacement contributed to the annual rise of CRE. In the future, implementing appropriate infection control measures and prudent antibiotic use remain crucial in combating antimicrobial resistance.
Ethics Statement
The strains in this study are part of the routine diagnosis and treatment procedures in hospitals. The use of these samples has been applied for no informed consent by the Ethics Committee of Beijing Aerospace General Hospital, without the informed consent of patients. The informed consent was waived by the ethics committee, and the approval number was Clinical No. 2 of 2025. This study was carried out in accordance with the Declaration of Helsinki, conducted in accordance with the local legislation and institutional requirements.
Funding
The authors declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the General Hospital Innovation Fund Project (2020-610, 2023-720).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Maeda T, Iwasawa J, Kotani H, et al. High-throughput laboratory evolution reveals evolutionary constraints in Escherichia coli. Nat Commun. 2020;11(1):5970. doi:10.1038/s41467-020-19713-w
2. Fontana C, Favaro M, Campogiani L, et al. Ceftazidime/avibactam-resistant Klebsiella pneumoniae subsp. pneumoniae isolates in a tertiary Italian hospital: identification of a new mutation of the carbapenemase type 3 (KPC-3) gene conferring ceftazidime/avibactam resistance. Microorganisms. 2021;9(11). doi:10.3390/microorganisms9112356
3. Van Tyne D, Gilmore MS. Raising the alarmone: within-host evolution of antibiotic-tolerant enterococcus faecium. mBio. 2017;8(1). doi:10.1128/mBio.00066-17
4. Chilambi GS, Nordstrom HR, Evans DR, et al. Evolution of vancomycin-resistant Enterococcus faecium during colonization and infection in immunocompromised pediatric patients. Proc Natl Acad Sci U S A. 2020;117(21):11703–11714. doi:10.1073/pnas.1917130117
5. Network NBRM. Surveillance report on antibiotic resistance of common clinical isolates in elderly patients (2014-2019). Chin J Infect Control. 2021;02:112–123.
6. Song Z. The current status and trends of multi-drug resistant organisms in hospital infections at a comprehensive hospital. Cont Med Educ. 2022;2:93–96.
7. Yang X, Guo R, Zhang B, et al. Retrospective analysis of drug resistance characteristics and infection related risk factors of multidrug-resistant organisms (MDROs) isolated from the orthopedics department of a tertiary hospital. Sci Rep. 2023;13(1):2199. doi:10.1038/s41598-023-28270-3
8. Huang L, Lin J, Song Y. Surveillance of bacterial resistance in Tongling City, Anhui Province from 2016 to 2018. Chinese J Antibiotics. 2022;(3):295–303.
9. Deng J, Yang J, Kang M. Analysis of bacterial resistance monitoring data in a comprehensive hospital in 2019. Chinese J Antibiotics. 2022;(4):405–411.
10. Fisher K, Phillips C. The ecology, epidemiology and virulence of Enterococcus. Microbiology. 2009;155(Pt 6):1749–1757. doi:10.1099/mic.0.026385-0
11. Tien BYQ, Goh HMS, Chong KKL, et al. Enterococcus faecalis promotes innate immune suppression and polymicrobial catheter-associated urinary tract infection. Infect Immun. 2017;85(12). doi:10.1128/IAI.00378-17
12. European Centre for Disease Prevention and Control. Surveillance Atlas of Infectious Diseases. 2023.
13. Peleg AY, Miyakis S, Ward DV, et al. Whole genome characterization of the mechanisms of daptomycin resistance in clinical and laboratory derived isolates of Staphylococcus aureus. PLoS One. 2012;7(1):e28316. doi:10.1371/journal.pone.0028316
14. Faron ML, Ledeboer NA, Buchan BW, Kraft CS. Resistance mechanisms, epidemiology, and approaches to screening for vancomycin-resistant enterococcus in the health care setting. J Clin Microbiol. 2016;54(10):2436–2447. doi:10.1128/JCM.00211-16
15. O’Driscoll T, Crank CW. Vancomycin-resistant enterococcal infections: epidemiology, clinical manifestations, and optimal management. Infect Drug Resist. 2015;8:217–230. doi:10.2147/IDR.S54125
16. Dubin KA, Mathur D, McKenney PT, et al. Diversification and evolution of vancomycin-resistant enterococcus faecium during intestinal domination. Infect Immun. 2019;87(7). doi:10.1128/IAI.00102-19
17. Eichel VM, Last K, Bruhwasser C, et al. Epidemiology and outcomes of vancomycin-resistant enterococcus infections: a systematic review and meta-analysis. J Hosp Infect. 2023;141:119–128. doi:10.1016/j.jhin.2023.09.008
18. Tortorano AM, Prigitano A, Morroni G, Brescini L, Barchiesi F. Candidemia: evolution of drug resistance and novel therapeutic approaches. Infect Drug Resist. 2021;14:5543–5553. doi:10.2147/IDR.S274872
19. Pfaller MA, Diekema DJ, Turnidge JD, Castanheira M, Jones RN. Twenty years of the SENTRY antifungal surveillance program: results for candida species from 1997-2016. Open Forum Infect Dis. 2019;6(Suppl 1):S79–S94. doi:10.1093/ofid/ofy358
20. Humphries R, Bobenchik AM, Hindler JA, Schuetz AN, McAdam AJ. Overview of changes to the clinical and laboratory standards institute performance standards for antimicrobial susceptibility testing M100, 31st edition. J Clin Microbiol. 2021;59(12):e0021321. doi:10.1128/JCM.00213-21
21. Yan XU, Yuexia ZHOU, Guocang L. Exploring and researching the positive rates of microbiological tests of different clinical specimens. China Foreign Med Treatment. 2021;(20):185–187.
22. Qian W. The influence of the difference of clinical samples on the positive results of microbiological test. China Prac Med. 2021;(17):210–212.
23. Kaini C, Cailian P, Pin W, Minjuan L. Time to positivity, distribution and drug resistance of pathogenic bacteria in blood culture. Henan Med Res. 2021;(32):6097–6100.
24. Ting C, Qin L, Wen-jun X, Li Y, Xiao-mei C, Tian-ying Z. Positive report time, distribution and antimicrobial resistance of pathogens from blood culture at a maternity and child health care hospital. Chin J Infect Control. 2015;14(11):735–739.
25. Ke-feng L, Hai-yang M, Xian-chun M, et al. Distribution and drug resistance of clinical pathogens in a tertiary hospital in Henan Province from 2010 to 2020. The Chinese J Clin Pharmacol. 2023;(14):2084–2088.
26. Xiaoyan Y, Lili L. Surveillance and analysis of multidrug-resistant bacteria and infection situations in a hospital from 2020 to 2022. Chinese J Disinfection. 2023;(09):716–718.
27. Mei-yun H, Si-jun X. Targeted monitoring analysis of multidrug resistant organism sinalevel-A tertiary hospital from 2020 to 2021. 2022:525–529.
28. Yinmei L, Lu W. Resistance trends among five important clinical pathogens in a tertiary general hospital from 2012 to 2019. World Clinical Drugs. 2021;(02):127–134.
29. Jun W, Tai-gui C, Shi-jie P, Kaijing Z. Distribution and drug resistance analysis of pathogenic bacteria in intensive care unit blood stream infection in a hospital. 2023:2227–2231+2237.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




