Back to Journals » Journal of Pain Research » Volume 18
“Do Doctors and Patients Have Different Understandings of Pain?” – A Pilot Study of Different Perspectives and Understandings of Pain in Clinical Pain Research
Authors Gormsen LK
Received 23 November 2024
Accepted for publication 30 April 2025
Published 24 May 2025 Volume 2025:18 Pages 2651—2662
DOI https://doi.org/10.2147/JPR.S508125
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Giuliano Lo Bianco
Lise Kirstine Gormsen1,2
1Department of Functional Disorders, Aarhus University Hospital, Aarhus, Denmark; 2Department of Clinical Medicine, Faculty of Health, Aarhus University, Aarhus, Denmark
Correspondence: Lise Kirstine Gormsen, Department of Functional Disorders, Aarhus University Hospital and Department of Clinical Medicine, Faculty of Health, Aarhus University, Palle Juul-Jensens Boulevard 11, Aarhus, 8200, Denmark, Email [email protected]
Background and Objective: Ambiguous results on pain thresholds often occur from biomedical pain research. Although results and methods are frequently discussed, only few studies have investigated participants’ understanding and perspectives of pain in research settings. The aim of this qualitative pilot study was to explore different understandings of pain in a clinical pain research setting.
Methods: We briefly interviewed 25 subjects, including Danish pain doctors and psychiatrists as well as pain patients, depressed patients, and healthy controls (five in each group) about their understanding of pain.
Results: Laymen seem less inclined to verbalize pain than professionals. In addition, they may embrace a concept of suffering that goes beyond the traditional body–mind dichotomy. Since suffering may be part of the pain experience, this difference in the understanding of pain may be at the core of the often ambiguous results when doctors and other health professionals study pain.
Conclusion: The results emphasize the need for supporting the ongoing process of integrating broad perspectives on pain in clinical pain research, including the concept of suffering. More research and resources are needed in this particular area of pain medicine.
Keywords: pain, suffering, concepts of pain, clinical pain research, pain thresholds
Introduction
Over the years, a number of studies have shown ambiguous results regarding pain complaints and pain thresholds in patients with depression and/or chronic pain. While depressed patients often complain of pain,1–7 studies examining pain thresholds in depressed patients show either higher (mechanical and thermal stimuli),8–11 unchanged,12,13 or lower14,15 thresholds to mechanical stimuli during depression, and women seem to tolerate less pain than men when pain thresholds are tested.6,15,16 Using the cold pressor test in depressed patients, pain tolerance thresholds were found to be either higher,17 unchanged,16 or lower18 when compared with controls. In general, chronic pain patients with, for example, fibromyalgia have lower pain thresholds compared with healthy controls;19–22 however, unchanged thresholds have been found in a population-based study.23
Results and methods are often discussed in the scientific literature. However, few studies have investigated participants’ understanding and perspectives of pain in clinical pain research settings. An exception is a study from 201824 in which chronic pain patients and healthy volunteers expressed difficulties and variability in rating experimental pain. However, to the author’s knowledge, no study has so far investigated the differences in doctors’ and patients’ understanding of pain in a biomedical clinical pain research setting, including also depressed patients.
In connection with the author’s clinical research project on pain and depression, published in the European Journal of Pain in 2004,13 the author became interested in understanding different perspectives of pain in clinical pain research settings. In the study,13 the author and colleagues examined pain thresholds to pressure and ice water in depressed patients and age- and gender-matched healthy participants during and after treatment for depression. The main findings showed that while treatment significantly improved depression, there was no significant change in pain thresholds during and after depression. As previously mentioned, this result is in contrast to clinical findings in depressed patients who complain more of pain when they are depressed. This generated a variety of questions concerning not only the bias and confounders but also more essential questions like “What do we mean when we talk about pain?” Is it possible that understandings of pain differ – especially between doctors and patients in research practice, and could this explain why the pain thresholds did not objectively change during major depression, which was in contrast to the subjective changes reported.
This question is important not only in the specific study on pain and depression13 but also in general when pain is studied in clinical pain research setting, because there might be a risk that we not fully capture the phenomena that we set out to study, which may lead to the wrong conclusions. An example could be that complaints of pain in depressed patients may deliberately be overheard because research results show no change in pain thresholds.
The aim of this pilot project was therefore to explore and develop an analytical model for the understanding of pain in biomedical clinical pain research.
Central Understandings of Pain in Pain Research
The concept of pain has developed from a simple physical phenomenon to a complex idea that combines theories within neurobiology, psychology, and sociology in understanding pain. Imbedded in this development is the change from understanding pain as a symptom to understanding pain as a disease in itself.25 This change has been initiated and promoted by the International Association for the Study of Pain (IASP) and has resulted in the development of multidisciplinary pain medicine as regards both the treatment and study of pain.26,27 To get a sense of the historical and organisational setting of clinical pain research, some core understandings of pain in pain research are shortly outlined. For a more comprehensive description, please see.28–31
According to the rope model developed by the French philosopher Descartes in 1664, pain is triggered when pulling a rope simultaneously activates a bell, thus illustrating the immediate connection between sensation and response.31
The Gate Control Theory of Pain developed by the psychologist Ronald Melzack and the anatomist Patrick Wall in 196532 views pain as regulated by a “gate” in the spinal cord, influenced by the brain and subjective factors like attention. Since then, our knowledge of the neurophysiology of pain has grown continuously. The latest edition of Wall and Melzack’s Textbook of Pain shows that the complex experience of pain is processed through multistringed systems.
The IASP definition of pain. In 1967, psychiatrist Harold Merskey defined pain as an “unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage”, which became widely used in pain research. The definition has since been updated and is today: “An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage”.33
The biopsychosocial view of pain expands the IASP pain definition by adding a social dimension,34,35 acknowledging that pain is influenced by psychological, social, and biological factors. This model, introduced by Engel in 1977,36 allows doctors to interpret patients’ pain through multiple lenses—psychological, social, and physical.37 This approach has been widely adopted and debated since the 1960s and 1970s. The cultural aspect of pain is often included in this model in relation to social aspects.
Although the understandings of pain presented here are chronological and separate, they are in some respects intertangled. For example, the Gate Control Theory has similarities with the rope model, although it is far more complex, and the biopsychosocial model has to some extent replaced the dichotomy of the body and mind of the IASP definition. Furthermore, today, the understanding of pain embeds many complex models.38
Materials and Methods
Methodological Considerations
In this pilot project, short interviews with patients and doctors were analyzed with qualitative techniques to get behind “the scene” with the aim of developing a model for analyzing different understandings of pain in clinical pain research. This provided a view into the participants’ understanding of pain and may inspire future research projects.
Setting
The interviews were made in a clinical pain research setting at the Danish Pain Research Center, Department of Clinical Medicine, Aarhus University. The Center has both laboratory and clinical research facilities and collaborates closely with Aarhus University Hospital in conducting research on chronic pain, pain treatment, and pain physiology. The aim is to understand the underlying mechanisms of chronic pain, in particular neuropathic pain, in order to improve treatment and to bridge the gap between pain physiology, experimental and clinical pain research.
Study Population
Twenty-five pain doctors, psychiatrists, pain patients, depressed patients, and healthy persons (five persons in each group) were interviewed on their view of pain. The patients were recruited for this study when they were enrolled in clinical pain research studies on pain and depression.13,19,39 The professionals were enrolled among the collaborators of the studies. Depressed patients aged 18–90 years admitted to the Psychiatric Hospital Risskov, Central Region Denmark, due to severe depression (according to ICD-10) and requiring ECT were invited to participate in the study provided that their score on the Hamilton Depression Scale (HDS-17) was >18. Only patients who did not take antidepressants the last week before ECT treatment or had relatively constant medication before, during, and after the study were included. Depressed patients with stroke, Alzheimer’s disease, polyneuropathy, Raynaud’s phenomenon, ischemic leg pain, serious danger of suicide, severe agitation, imminent delirium, or alcohol or drug dependence (ICD-10) were excluded before study start.
Furthermore, chronic neuropathic pain (NP) patients aged 18–75 years attending the Neuropathic Pain Clinic at Aarhus University Hospital, Aarhus, Denmark, and meeting the diagnostic criteria of peripheral NP40 or probable peripheral NP according to the grading system for NP41 were invited to participate in the study. Only patients with a mean weekly pain score ≥4 on an 11-point Likert scale and daily pain present ⩾6 months were included. Furthermore, treatment with antidepressants (TCAs, SSRIs, SNRIs, MAOIs, or others), antiepileptics (gabapentin, pregabalin, carbamazepine, or others), and other analgesics had to be stopped at least 2 weeks before study participation. Paracetamol (4 g per day) and aspirin (75 mg per day) were, however, permitted. Patients with stroke, Alzheimer’s disease, ischemic pain, Raynaud’s phenomenon, a previous diagnosis of mania, bipolar disorder, psychosis, severe agitation, imminent deliria, current suicide risk, or alcohol or drug dependence (ICD-10) were excluded before study start.
A group of healthy (no medical or psychiatric diagnosis) pain-free age- and gender-matched males and females served as healthy controls. They were not apparently clinically depressed or suffered from anxiety (Hamilton depression score < 6). No analgesic, monoaminergic, or antiepileptic intake was permitted in the control group.
The groups were representative of a typical clinical pain research setting at the Danish Pain Research Center as exemplified in the studies13,19,39 as concerns education, age, and gender distribution (Table 1). The educational level was the highest among the professionals who were all doctors, whereas it was mixed in the non-professional group (Table 1). Four of the pain doctors had a background in neurology and were 1–2 years into their speciality training, one was a consultant in anesthesiology, and all were at the time of the interview undertaking a PhD in pain medicine. The psychiatrists were all doctors and consultants in psychiatry working clinically in the psychiatric hospital setting.
 |
Table 1 Demographic Characteristics of Participants |
 |
Table 2 The Concept of Pain Among Patients and Doctors in a Clinical Research Setting |
Data Collection
Personal audiotaped interviews were conducted with the participants in their respective settings: doctors in their offices and patients in an experimental setup. It was an open and explorative interview. The aim of the interview was to get the participants to speak as openly as possible about their pain experience to clarify their understanding of pain. The opening and main question of the interview in all groups was: “What is pain? How would you describe pain to a person who does not know pain?” You are allowed to use words or a sentence. Furthermore, clarifying and encouraging questions were asked, for example, “you said that pain is….?” (repeating what the participant just said) or “are there more you want to say?” The interviews of about 20–50 minutes each were carried out by the author. The interviews were conducted, transcribed in Danish, and then translated into English by the author. QRS NVivo 7 was used for data processing.
Data Analysis
The interviews were analyzed according to the three techniques: condensation (i.e., the interview text is shortened so only the meaning is put forward); categorization (i.e., the text is analyzed in order to find out if a particular phenomenon is present) and interpretation (i.e., the text is critically analyzed and interpreted to find meaning)42 (see Figure 1). In the analyzing process, aspects and understandings of pain were looked for as described above but categories and concepts were also identified from the data analysis. For example, suffering as described by the doctor and philosopher Eric Cassell43 was not included in the first reading of the interviews; however, it was included later on as it seems present in the data. Furthermore, the linguistic characteristics were analyzed (e.g., scattered words or short sentences).
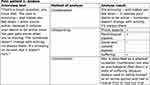 |
Figure 1 An example of the analysis of the interviews.42 |
Ethics
The study was exempt from ethical approval according to Danish legislation. However, the study complies with the Declaration of Helsinki. Written and oral informed consents were obtained from all participants including Demographic Characteristics. Furthermore, all participants were given fictitious names for the purpose of anonymity.
Results
An overview of the different models or concepts of pain among the participants in the study is given in Table 2.
Healthy Controls and Pain
The understanding of pain was described in two different ways in the group. Firstly, pain is described as a purely physical condition: Healthy control Anna said:
Pain is sticking, striking, burning, stinging, and pressing.
And the healthy control Ella said:
Pain feels like pressure, stinging, tension, something burning, pulling.
They tried to grasp the experience of pain as a physical sensation. This description of pain may be traced back to René Descartes’ rope model where pain is represented as a sensory area of the brain. Also, the pulling of a rope in the model was hinted at when Ella used the word pulling. However, words like burning, stinging, and pressing may also represent the sensory component of pain as framed by the McGill Pain Questionnaire, which was used in the research setting in this study. The McGill Pain Questionnaire is often used in clinical pain research settings and may reflect the Gate Control Theory of pain rather than the rope model.
Secondly, other healthy participants included a psychological aspect of pain. The psychological aspect is illustrated by the healthy control Berta’s answer:
Pain is a discomfort that is unbearable, e.g. drilling or sticking.
or the healthy control Emilia who said:
It hurts, it is a torment, it presses, it is sore, and it is simply awful.
It is the words unbearable and simply awful that go beyond the physical dimension.
Another element of pain is represented by the healthy control Camilla who said:
Pain is an undermining experience where one is not able to think logically. It can result in nausea and discomfort and it hurts.
This first aspect could be described as a psychological aspect of pain or even a concept that goes beyond the framework of dualism. Pain destroys Camilla’s ability to think logically, and aspects of her personality are thus damaged or lost. The American medical doctor and philosopher Eric Cassell described this as the concept of suffering (p. 43).43
The concept of suffering as described by Eric Cassell was one of the most interesting results that rose from the analysis. The author had not been aware of this concept, although suffering is often discussed in relation to pain. Cassell developed the concept of suffering in his book “The nature of suffering and the goals of medicine”,43 which was an attempt to go beyond the traditional way of thinking of body and mind in pain medicine. Cassell places suffering outside the framework of dualism by stating that suffering is present when aspects of the personality are damaged or lost (p. 43), which means that suffering can be caused by pain, but it is not a necessary condition. One could therefore suffer without having pain (p. 32). This is in contrast to his contemporary colleagues, and Cassell has over a number of years agitated for the importance of understanding suffering in medicine.
The healthy participants seemed one way or the other to have an experienced understanding of pain, a concept that had risen through their everyday life with pain. Furthermore, the participants hinted to elements of pain that involve what pain is doing to them as persons, and therefore suffering is integral in their understanding of pain. All participants in this group seem to be trying to verbalize their own experience of pain. However, the healthy control Ella is a trained nurse, and she might reproduce a professional, not personal, concept of pain, but her answers are still similar to those of other healthy controls. The healthy controls thus seem to have a concept of pain, which is achieved through their everyday life with pain and is therefore not a diagnostic or theoretical concept.
Pain Patients and Pain
The majority of the pain patients have a very broad understanding on pain. They describe pain as a physical, psychological, sociological, or suffering experience. The pain patient Danny illustrated this by saying:
Yes, but I will just say that it hurts and it burns. uhm. Like there is not enough space in the bone. Like it could burst. That is it. It is uncomfortable but one keeps quiet because it is no use in misery. It is not going to get better because of that. People cannot see that you are in pain. They do not understand. One keeps quiet.
The physical aspect is represented when he says: “... it hurts and it burns...” The psychological aspect or even suffering is verbalized when he talks about misery and the social when he talks about the interaction with others: “They do not understand.” Furthermore, his suffering consists of keeping quiet, which is an alteration of his personality. He would speak up if others would understand him. The pain patient Anders also illustrates suffering when he said that:
It is a difficult question - you know. The pain is annoying - and it makes you sad - when it is not possible to be active because it reduces your wish to be active because the pain increases when you are active.
Anders used to define himself as an active person and had to realise that he had lost that (Figure 1). On this basis, it seems that all the pain patients are not very verbalized about their pain, and furthermore that they all include a concept of suffering as described by Eric Cassell in his understanding of pain.
Depressed Patients and Pain
The depressed patients described pain with scattered words like the depressed patient Berit:
Pain is continuous, thumping, unbearable, and penetrating.
This means that the patients are not very articulate about their pain. Just as the healthy participants, they are trying to grasp the experience of pain. The depressed patients described a physical and psychological view of pain. Exemplified by the depressed patient Agnete who said:
Pain cuts, presses, it’s tense. It is a feeling of miserableness or of something tight, e.g. around the head. It can also be drilling.
Words as cuts, presses, and tense represent physical aspects of pain, and words as a feeling of miserableness represent a psychological aspect or even point to suffering. Other examples of suffering are Berit as quoted before and Eric:
Pain is something that hurts, something uncomfortable, something ugly.
The words unbearable, penetrating, and ugly indicate that the pain disturbs fundamental traits of the person. All the depressed patients seem in this way to imply suffering as a feature of pain. This analysis could be seen as an overinterpretation of the psychological and physical inhibition, which is seen in severely depressed patients. But from these simple sentences and from meeting the persons, a burden of suffering is sensed. Therefore, it seems that all the depressed patients hint to suffering as an element of pain.
Pain Doctors and Pain
All the pain doctors seemed to circle around IASP´s definition of pain “An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or defined in terms of such damage”. This definition that includes physical and psychological aspects could be described as a body-mind definition of pain. However, none of the doctors got the definition word by word. The pain doctor Bente said:
Pain is a subjective and objective feeling that is caused by possible or potential destruction of certain structures in the body where the pain originates from influenced by the subjective experience.
and pain doctor David said that:
Pain is an uncomfortable feeling that rises or that one feels rise because of something that can damage one’s tissue. An experience within the brain of the person in pain.
Only one of the pain doctors, Amalie, extended the definition with a sociological perspective and hereby employing a bio-psycho-social model of pain by saying:
… a feeling that influences the person's everyday life.
None of the pain doctors included or hinted to a concept of suffering in their definition of pain. They have a professional or theoretical view of pain exemplified with IASP's definition of pain and the neurobiological theory of pain that do not involve personal views on pain.
Psychiatrist and Pain
Psychiatrists have well-articulated definitions of pain that vary from the dualistic definition based on a body–mind dichotomy through a definition that also includes suffering to a broad definition of pain that includes physical, psychological, sociological, and cultural perspectives, as well as a component of suffering. The body–mind dichotomy is represented in the following quote by psychiatrist Abalone:
It is a feeling of physical or psychological discomfort. If it is physical, it is located to certain areas of the body, and if it is psychological, it is a more diffuse experience that can vary in intensity and have different characteristics.
The very complex notion of pain is represented by the psychiatrist Cecilie who also included a cultural aspect of pain by saying:
The explanation should be adapted to the person’s cultural background because understanding is in the language process. …. The metaphysical concept of pain, pain in a transferred sense, is used as a picture on mental states, and this concept again is dependent on the cultural background. …Some find it difficult to understand the phrases “life pain” or “wounds on the soul”, and may react (e.g., by wanting to be alone). They have difficulty expressing their feelings….
Psychiatrist Cecilie hints at the suffering aspect when she talks about “life pain” and “wounds on the soul”. These phrases are often used in Denmark to describe a dimension of pain that goes beyond the physical aspect. Eddy also hints to suffering when he said:
…it is an unpleasant sensation that is scaring, frightening, and leads to inactivation of the person.
Another perspective on pain, which is represented by the psychiatrists Cecilie, Daniel, and Eddy, is the influence of psychopathology on pain. An example is the psychiatrist Daniel who said:
…pain means a kind of discomfort. Now, I am already in doubt about the truth in what I just said because there are people who inflict pain on themselves or feel lust by hurting others or by being inflicted pain upon.
As shown, the psychiatrists have a very complex understanding of pain that also hints at a concept of suffering as a result of working with the complex field of psychiatry.
Professionals Versus Laymen
The analysis suggests that clinical doctors and researchers cannot assume that they have the same understanding of pain as their patients. The pain doctors talked around the body-mind definition of pain, whereas pain patients, depressed patients, and healthy participants talked from a body-mind definition that often hints to the concept of suffering. The psychiatrists also hinted at the concept of suffering in their definition of pain.
Furthermore, an interesting observation is that the experts of pain, the pain patients, often talk about pain briefly by only using a few sentences to describe their pain. They talk about a major handicap in their life in 3–5 transcribed lines, although they have the opportunity to speak at length. Furthermore, they describe their pain in broken sentences, taking a little break to gain time to express her-/himself more accurately, the pain patient Carl said:
Yes… it is many things. It is both the issue of... First of all it hurts right, but it can be many different types of pain ... forms of pain.
This is also a characteristic of depressed patients and healthy participants.
This suggests that lay people are not very articulate about their pain and instead try to capture the experience of pain with scattered words. A short form of talking about pain was to some extent shared by the pain doctors who all seemed to circle around IASP's definition of pain, although none of them used the exact words of the definition. In contrast, the psychiatrists had more well-articulated definitions of pain. It is interesting, but not surprising, that lay people seem to have an inside view of pain, while the professionals, especially pain doctors, have an external view of pain that circles around a definition.
Discussion
The findings in this study suggest that different concepts of pain are used in clinical pain research settings. Clinical doctors and researchers cannot assume that they have the same understanding of pain as their patients. The pain doctors talked around the body-mind definition of pain, whereas pain patients, depressed patients, and healthy participants talked from a body-mind definition that often hints to the concept of suffering. The psychiatrists also hinted at the concept of suffering in their definition of pain. This seems to be very appropriate as all depressed patients seem to imply this concept. However, some of the pain doctors and the psychiatrists may thus have difficulty discussing pain, especially with depressed patients and pain patients, but also with some of the healthy participants. It is well known that patients have different concepts of pain and are trying to come to terms with it.44,45 Furthermore, there are also studies that focus on the experiences of healthcare professionals who work with chronic pain patients.46 However, the focus of this study is the research setting and this perspective is to the author's knowledge new. An explanation of the observed diversity in this study is that laymen form their understanding of pain in a context that is different from that of medical professionals. Doctors and researchers focus on developing and sophisticating their understanding of pain for use in their biomedical clinical and research work, while laymen try to describe their personal experiences of pain. This means that medical professionals may have developed an understanding of pain without profoundly considering the concept developed by the carriers of the phenomenon.
We create concepts like pain through our language. The concept of physical objects like a cup is easier to define due to sensory input, such as its color and texture, while describing a mental phenomenon like pain requires comparisons to physical phenomena, like “it feels cold.” This process of specifying concepts helps communicate experiences, particularly in healthcare contexts where language is refined to discuss pain. However, this refinement may alter the concept and experience of pain. For example, patients may “cope” with pain, changing how they experience it, which is often the goal of psychological pain therapies.
Researchers, on the other hand, develop precise definitions of pain for study purposes. For instance, pain specialists often use the IASP definition of pain, which emphasizes the subjective and objective aspects of pain; however, they do not include personal concepts of pain, like in scientific fields, where the phenomena lack personal experience.
This is a general problem in medicine that has its roots in the research tradition of laboratory medicine in the 1800s.47 Laboratory medicine developed as an extension of physics and chemistry, and medicine developed from this natural-scientific method. This way of thinking is very useful in many forms of diseases (e.g., in diabetes where blood sugar levels are considered as an expression of the disease process). However, it is not suitable for chronic pain because there are no objective measures such as blood levels and other biological markers. In pain medicine, pain is primarily described by making the patients rate their pain on a visual analog scale from 0 (no pain) to 10 (worst thinkable pain). Since this is not an objective measure in the traditional biomedical sense, it is problematic to do pain research only by using the methods of biomedicine without taking into consideration the concept of pain created by the carriers of the phenomenon. This point is underpinned by Stussmann et al24 that advocate for researchers to incorporate the type of knowledge that includes difficulties and variability in rating experimental pain into the design and interpretation of pain research.
The laymen’s understanding of pain in this study may describe something basic about the essence of pain. However, laymen may, on the other hand, also be influenced by the understanding of pain from the pain profession when they explain pain. They may – as described before – not have studied the different ideas of pain directly, but they have been influenced through the public presence of the ideas. The reason is that the different understandings of pain have been promoted and communicated, e.g., through IASP or pain clinics or via the media from the professionals into society. The ideas may have influenced other institutions and patient organizations and merged into the view of pain shared by laymen. In this perspective, views of pain should be considered not only as maps of the world but also as maps for the world.49 This means that when a pain definition is presented in the professional pain world, it not only describes a disease, but it soon after becomes a map that “dictates” the communication, treatment, and further study of the condition.
This influence may be even clearer when pain patients are asked to talk about pain. They have in many cases been subject to treatment in multidisciplinary pain clinics, which often offer patients education in pain management from a biological, psychological, suffering, and sociological perspective, and they are therefore very influenced by these understandings of pain. However, the results suggest that suffering is not fully integrated because the majority of medical professionals do not include a concept of suffering in their understanding of pain. This is also underpinned by the author being blinded or overseeing the concept of suffering at the beginning of the study.
With regard to the presence of suffering in laymen’s definition of pain, it is difficult to say if it describes something essential about pain, or whether they have been influenced through society as described earlier, or they have as pain patients been introduced to the concept in connection with the treatment and rehabilitation in pain clinics. The answer is probably all three. Suffering is a central experience of living with chronic pain, but laymen are also exposed to the concept through the media and society, and pain patients are in particular exposed to the concept through the pain clinics.
The results suggest that the concept of suffering in relation to pain is present in a clinical pain research setting especially among laymen. It is therefore not only a useful but a crucial concept when trying to understand pain. If concepts like suffering are bypassed in methods and research projects in clinical pain research, the consequence will be that we do not fully capture the phenomena that we set out to study. As described in the beginning, an example is that depressed patients may understand pain as suffering when asked if they are in pain as opposed to when they participate in a research project where pain is referred to as the sensory experience represented by pain thresholds. This pinpoints the necessity of exploring the understanding of pain that is used among patients and professionals when the focus is doing research in clinical pain medicine.
Strengths and Limitations
This is one of the few studies that explores the understanding of pain among patients and professionals in a research setting. Although the analysis may appear somewhat simplistic, it identifies concepts that are circulated in clinical pain research settings that may be helpful to take into account when planning and doing research.
The quote “What you ask is what you get”48 applies to the question the participants were asked: “What is pain?” The issue is that the participants likely answered three different questions: A) What is the experience of pain like?, B) What causes pain?, and C) What are the effects of pain? Patients and laypeople mostly answered question A, while doctors focused on B and C. This distinction does not hinder the results. The key lies not only in the answers but also in how the questions were understood, and how they were distributed among the different groups.
Furthermore, the study only includes short interviews where more in-depth interviews would have been preferable. However, this is a pilot study that tries to get an overview and aims to inspire reflection on the clinical pain research setting and further research.
Conclusion
The results indicate that many concepts are used in a clinical pain research setting. Laymen are less inclined to verbalize and explain their pain than professionals, and furthermore – in contrast to professionals – tend to employ a concept of suffering that may go beyond the classical body-mind or bio-psycho-social pain definitions. From a clinical research point of view, the findings in this study are interesting because they could suggest that doctors and patients do not always talk about the same phenomenon when studying pain. This may be the core of well-known ambiguous results when doctors strive to study pain. Furthermore, the results show the need for supporting the ongoing integration of the concepts of suffering in clinical pain research. However, more research and further resources are needed in this particular area of pain medicine.
Acknowledgments
Firstly, we would like to thank the participants for their contribution. Secondly, Helle Obenhausen Andersen, who generously helped with language revision of the paper.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Corruble E, Guelfi JD. Pain complaints in depressed inpatients. Psychopathology. 2000;33(6):307–309. doi:10.1159/000029163
2. Roy R, Thomas M, Matas M. Chronic pain and depression: a review. Compr Psychiatry. 1984;25(1):96–105. doi:10.1016/0010-440X(84)90027-0
3. Gupta MA. Is chronic pain a variant of depressive illness? A critical review. Can J Psychiatry. 1986;31(3):241–248. doi:10.1177/070674378603100312
4. Romano JM, Turner JA. Chronic pain and depression: does the evidence support a relationship? Psychol Bull. 1985;97(1):18–34. doi:10.1037/0033-2909.97.1.18
5. Smith GR. The epidemiology and treatment of depression when it coexists with somatoform disorders, somatization, or pain. Gen Hosp Psychiatry. 1992;14(4):265–272. doi:10.1016/0163-8343(92)90097-T
6. Bair MJ, Robinson RL, Katon W, et al. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163(20):2433–2445. doi:10.1001/archinte.163.20.2433
7. Lépine JP, Briley M. The epidemiology of pain in depression. Hum Psychopharmacol. 2004;19(Suppl 1):S3–7. doi:10.1002/hup.618
8. Lautenbacher S, Krieg JC. Pain perception in psychiatric disorders: a review of the literature. J Psychiatr Res. 1994;28(2):109–122. doi:10.1016/0022-3956(94)90023-X
9. Lautenbacher S, Roscher S, Strian D, et al. Pain perception in depression: relationships to symptomatology and naloxone-sensitive mechanisms. Psychosom Med. 1994;56(4):345–352. doi:10.1097/00006842-199407000-00010
10. Dworkin RH, Clark WC, Lipsitz JD. Pain responsivity in major depression and bipolar disorder. Psychiatry Res. 1995;56(2):173–181. doi:10.1016/0165-1781(95)02501-7
11. Bär KJ, Brehm S, Boettger MK, et al. Pain perception in major depression depends on pain modality. Pain. 2005;117(1–2):97–103. doi:10.1016/j.pain.2005.05.016
12. Klauenberg S, Maier C, Assion H-J, et al. Depression and changed pain perception: hints for a central disinhibition mechanism. Pain. 2008;140(2):332–343. doi:10.1016/j.pain.2008.09.003
13. Gormsen L, Ribe AR, Raun P, et al. Pain thresholds during and after treatment of severe depression with electroconvulsive therapy. Eur J Pain. 2004;8(5):487–493. doi:10.1016/j.ejpain.2003.11.015
14. Schreiber S, Shmueli D, Grunhaus L, et al. The influence of electroconvulsive therapy on pain threshold and pain tolerance in major depression patients before, during and after treatment. Eur J Pain. 2003;7(5):419–424. doi:10.1016/S1090-3801(02)00146-5
15. Merskey H. The effect of chronic pain upon the response to noxious stimuli by psychiatric patients. J Psychosom Res. 1965;8:405–419. doi:10.1016/0022-3999(65)90083-8
16. Stengel E, Oldham AJ, Ehrenberg AS. Reactions to pain in various abnormal mental states. J Ment Sci. 1955;101(422):52–69. doi:10.1192/bjp.101.422.52
17. Lautenbacher S, Spernal J, Schreiber W, et al. Relationship between clinical pain complaints and pain sensitivity in patients with depression and panic disorder. Psychosom Med. 1999;61(6):822–827. doi:10.1097/00006842-199911000-00015
18. Ganchrow JR, Steiner JE, Kleiner M, et al. A multidisciplinary approach to the expression of pain in psychic depression. Percept Mot Skills. 1978;47(2):379–390. doi:10.2466/pms.1978.47.2.379
19. Gormsen L, Bach FW, Rosenberg R, et al. Differential pain modulation in patients with peripheral neuropathic pain and fibromyalgia. Scand J Pain. 2012;3(3):116–123. doi:10.1016/j.sjpain.2012.01.002
20. Desmeules JA, Cedraschi C, Rapiti E, et al. Neurophysiologic evidence for a central sensitization in patients with fibromyalgia. Arthritis Rheum. 2003;48(5):1420–1429. doi:10.1002/art.10893
21. Petzke F, Clauw DJ, Ambrose K, et al. Increased pain sensitivity in fibromyalgia: effects of stimulus type and mode of presentation. Pain. 2003;105(3):403–413. doi:10.1016/S0304-3959(03)00204-5
22. Jespersen A, Dreyer L, Kendall S, et al. Computerized cuff pressure algometry: a new method to assess deep-tissue hypersensitivity in fibromyalgia. Pain. 2007;131(1–2):57–62. doi:10.1016/j.pain.2006.12.012
23. Petersen MW, Skovbjerg S, Jensen JS, et al. Conditioned pain modulation and pain sensitivity in functional somatic disorders: the DanFunD study. Eur J Pain. 2022;26(1):154–166. doi:10.1002/ejp.1847
24. Stussman BJ, Nahin RL, Čeko M. Fibromyalgia patients and healthy volunteers express difficulties and variability in rating experimental pain: a qualitative study. Scand J Pain. 2018;18(4):657–666. doi:10.1515/sjpain-2018-0085
25. Raffaeli W, Arnaudo E. Pain as a disease: an overview. J Pain Res. 2017;10:2003–2008. doi:10.2147/JPR.S138864
26. Baszanger I. Inventing Pain Medicine: From the Laboratory to the Clinic. New Brunswick and London: Rutgers University Press; 1998.
27. Tompkins DA, Hobelmann JG, Compton P. Providing chronic pain management in the “Fifth Vital Sign” Era: historical and treatment perspectives on a modern-day medical dilemma. Drug Alcohol Depend. 2017;173(Suppl 1):S11–s21. doi:10.1016/j.drugalcdep.2016.12.002
28. Gatchel RJ, Peng YB, Peters ML, et al. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133(4):581–624. doi:10.1037/0033-2909.133.4.581
29. Perl ER. Ideas about pain, a historical view. Nat Rev Neurosci. 2007;8(1):71–80. doi:10.1038/nrn2042
30. Moayedi M, Davis KD. Theories of pain: from specificity to gate control. J Neurophysiol. 2013;109(1):5–12. doi:10.1152/jn.00457.2012
31. Wall PD. Pain: The Science of Suffering. Columbia University Press,; 2002.
32. Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150(3699):971–979. doi:10.1126/science.150.3699.971
33. Raja SN, Carr DB, Cohen M, et al. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain. 2020;161(9):1976–1982. doi:10.1097/j.pain.0000000000001939
34. Gatchel RJ, Turk DC. Criticisms of the biopsychosocial model in spine care: creating and then attacking a straw person. Spine. 2008;33(25):2831–2836. doi:10.1097/BRS.0b013e31817d24ad
35. Weiner BK. Spine update: the biopsychosocial model and spine care. Spine. 2008;33(2):219–223. doi:10.1097/BRS.0b013e3181604572
36. Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129–136. doi:10.1126/science.847460
37. Adams N, Poole H, Richardson C. Psychological approaches to chronic pain management: part 1. J Clin Nurs. 2006;15(3):290–300. doi:10.1111/j.1365-2702.2006.01304.x
38. Cohen SP, Vase L, Hooten WM. Chronic pain: an update on burden, best practices, and new advances. Lancet. 2021;397(10289):2082–2097. doi:10.1016/S0140-6736(21)00393-7
39. Gormsen L, Rosenberg R, Bach FW, et al. Depression, anxiety, health-related quality of life and pain in patients with chronic fibromyalgia and neuropathic pain. Eur J Pain. 2010;14(2):127.e1–8. doi:10.1016/j.ejpain.2009.03.010
40. Rasmussen PV, Sindrup SH, Jensen TS, et al. Symptoms and signs in patients with suspected neuropathic pain. Pain. 2004;110(1–2):461–469. doi:10.1016/j.pain.2004.04.034
41. Treede RD, Jensen TS, Campbell JN, et al. Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology. 2008;70(18):1630–1635. doi:10.1212/01.wnl.0000282763.29778.59
42. Kvale S. Inter Views: Learning the Craft of Qualitative Research Interviewing. SAGE Publications Inc; 2004.
43. Cassell E. The Nature of Suffering. New York: Oxford University Press; 1991.
44. van Rysewyk S, Blomkvist R, Chuter A, et al. Understanding the lived experience of chronic pain: a systematic review and synthesis of qualitative evidence syntheses. Br J Pain. 2023;17(6):592–605. doi:10.1177/20494637231196426
45. Toye F, Seers K, Allcock N, et al. Patients’ experiences of chronic non-malignant musculoskeletal pain: a qualitative systematic review. Br J Gen Pract. 2013;63(617):e829–41. doi:10.3399/bjgp13X675412
46. Toye F, Seers K, Barker KL. Meta-ethnography to understand healthcare professionals’ experience of treating adults with chronic non-malignant pain. BMJ Open. 2017;7(12):e018411. doi:10.1136/bmjopen-2017-018411
47. Porter R. The greatest benefit to Mankind: a medical history of humanity from antiquity to the present HarperCollins. 1997.
48. Babbie ER. The Practice of Social Research. 7th Edition, Wadsworth, Belmont, 1995.
49. Geertz C. The Interpretation of Cultures. Basic Books; 1973.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

